Abstract
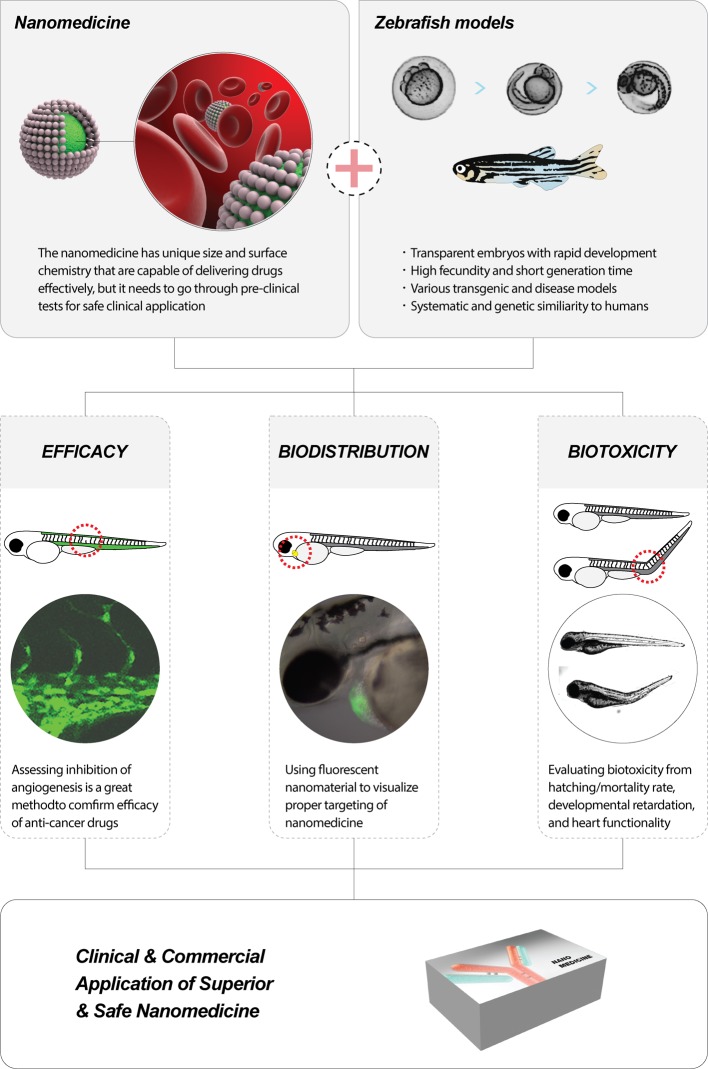
Preclinical screening with animal models is an important initial step in clinical translation of new drug delivery systems. However, establishing efficacy, biodistribution, and biotoxicity of complex, multicomponent systems in small animal models can be expensive and time-consuming. Zebrafish models represent an alternative for preclinical studies for nanoscale drug delivery systems. These models allow easy optical imaging, large sample size, and organ-specific studies, and hence an increasing number of preclinical studies are employing zebrafish models. In this review, we introduce various models and discuss recent studies of nanoscale drug delivery systems in zebrafish models. Also in the end, we proposed a guideline for the preclinical trials to accelerate the progress in this field.
Keywords: Biodistribution, Biotoxicity, Drug delivery system, Functional evaluation, Zebrafish model
Introduction
Relative to the dynamic research atmosphere in the development of nanoscale drug delivery systems, the number of consumer drugs that incorporate nanotechnology is very low. Countless nanoscale drug delivery system researches are focused on cancer treatments, and there are more than a dozen journals that concentrate on this particular topic; however, commercially and widely used FDA-approved nanomedicines are limited to a few, including Abraxane for metastatic breast cancer, Doxil for ovarian cancer and Emend for chemotherapy induced nausea [1,2]. This dissonance in research effort and clinical usage of nanomedicine is often attributed to the biological consequences of using nanomaterials. In the past, the unique physiochemical properties of particles combined with the ability to modify materials at molecular length scales promised to solve many of the problems in drug delivery and improve clinical outcomes [3–10]. However, the issues involving the biological consequences of using nanomaterials caused the current complications in nanoscale drug delivery systems. Validating efficacy and establishing that there is no biotoxicity during drug design and development have been extremely challenging. This has been compounded by the fact that the research has been largely empirical and without the development of design rules, to slow down clinical applications of nanomedicine.
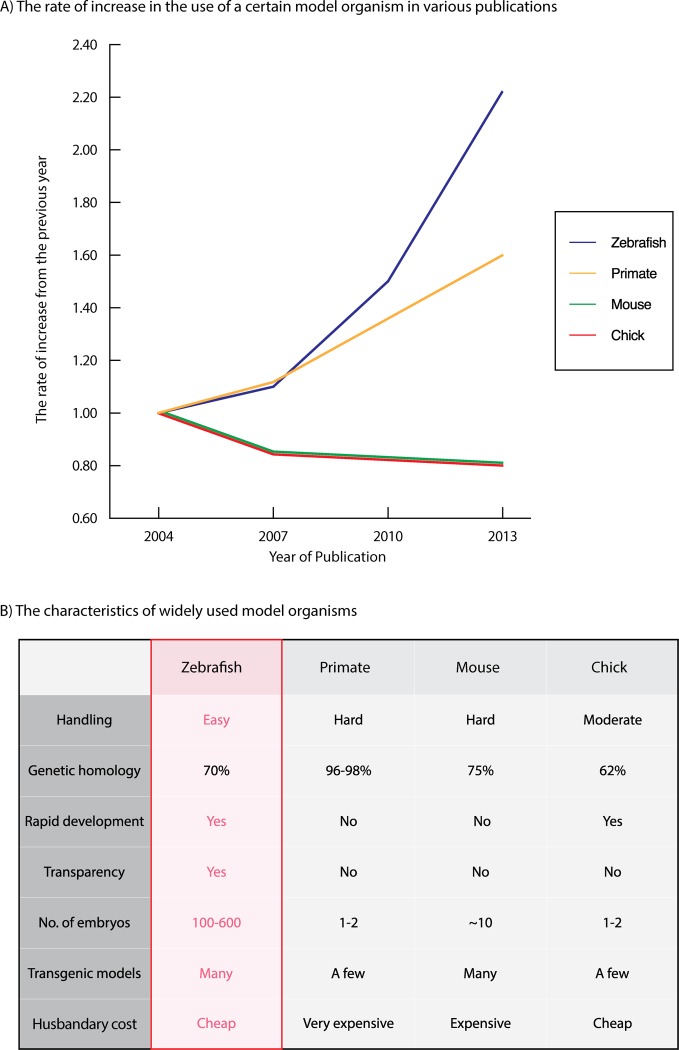
In designing and developing a new medicine for human, preclinical screenings with animal models are an essential part of gaining insight into the efficacy, biodistribution, and biotoxicity of nanomaterials [12–14]. Commonly, mouse models are used; however, preclinical screenings with animal models generally involve a large number of animals and hence can be expensive and time-consuming with mouse models (Figure 1B) [2,15–19]. Biological homologous to humans, primate models will provide the most reliable data [2,20–22]. However, experiments with baboons or chimpanzees are even more expensive and time-consuming (Figure 1B). Due to such high demand of money and time, many tend to refrain from including preclinical screenings with animal models during the development of new nanoscale drug delivery systems, and compromise with the less demanding in vitro assays.
Figure 1. Comparison of the zebrafish with other in-vivo model organisms employed in biomedical-nano researches.
(A) The prevalence of animal models in biomedical research. The normalized number of publications that employed zebrafish, primate, mouse, and chick models since 2004. The rapid growth of the zebrafish model highlights the benefits in preclinical studies. (B) The characteristics of widely used model organisms. Zebrafish, primate, mouse, and chick models are evaluated on important factors in preclinical studies. Apart from the genetic homology to humans, the zebrafish model has many advantages. The genetic homology of the animal model was obtained from Ensembl database browser analysis [11].
The zebrafish model is an alternative animal model that can resolve the issue (Figure 1A) [2]. Zebrafish models are inexpensive, amenable to modifications, and optically transparent, and hence have many advantages over other animal models (Figure 1B) [2,6,13,16,23–43]. With zebrafish models, we can easily incorporate sophisticated preclinical screenings during the nanoscale delivery system development [13,23,24,30–32,34,38,44]. This review highlights the characteristics and uses of zebrafish models for the researchers who are not accustomed to experiment with them. Also, in order to guide them through toward adopting preclinical screenings with zebrafish models during their research and eventually to foster clinical application of nanoscale drug delivery system, we included a suggested guideline.
Benefits and drawbacks of zebrafish models in preclinical studies of nanoscale drug delivery systems
Benefits
Optical transparency
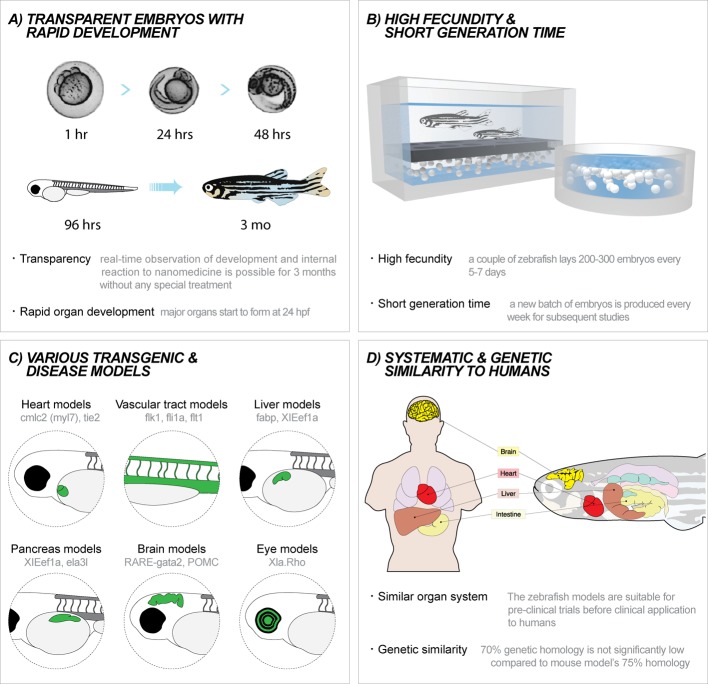
Zebrafish embryos retain optical transparency until approximately 60 h post fertilization (hpf), when the pigmentation process starts (Figure 2A) [24,45]. To keep the optical transparency beyond that point, transgenic models such as casper, which lacks pigments in its skin and scales, can be employed, or zebrafish embryos can be treated with 1-phenyl 2-thiourea (PTU) to inhibit pigmentation [24,46]. The transparency of zebrafish embryos offers unique opportunity to observe the events happening inside the body such as tumor development, vessel growth, organ development, and dispersion of nanomaterials. Such observations can be made after 96 hpf when major organs complete their development [24]. Due to relatively fast development as compared with other model organisms, preclinical screenings with zebrafish models can take less time because waiting period to notice significant changes in zebrafish’s behavior and morphology is shortened (Figure 2A) [31,32,45]. There are a wide range of transgenic zebrafish models with fluorescent organs that can help us to observe organ-specific reaction to nanomaterials through their clear body (Figure 2C) [34,44,46–49].
Figure 2. Characteristics of zebrafish models.
(A) Zebrafish are transparent and develop rapidly. Zebrafish embryos start forming major organs at 24 hpf. The transparency of zebrafish embryos is sustained until 96 hpf. Phenotypic changes upon exposure to drug delivery systems can be easily observed. (B) High fecundity and short generation time. A fertile zebrafish lays approximately 200–300 embryos every 5–7 days. Due to the high fecundity and short generation time, preclinical studies with zebrafish embryos can use large sample sizes, are cost-effective and can be conducted in a relative short time. (C) Numerous transgenic and disease models. Various models with fluorescent protein expressing organs are commercially available. Disease and knockdown models can be tailored for specific applications. (D) Systematic and genetic similarity to humans. Zebrafish models are phenotypically and genotypically similar to humans and hence suitable for prestudies. They have 70% genetic homology to humans, not significantly lower than widely used mouse models.
Statistical reliability
A fertile female zebrafish lays approximately 200–300 embryos every 5–7 days (Figure 2B) [30,31,50]. The high fecundity of zebrafish translates into statistical reliability, by providing large numbers of affordable subjects for preclinical studies. The development of new drug delivery systems requires extensive preclinical studies to support their efficacy and safety. This is particularly challenging with nanoscale delivery systems, which have been addressed with an issue in their safety. The productivity and relatively inexpensive price of zebrafish models enable us to design powerful preclinical studies with numerous experimental groups and large sample sizes, which can substantiate the capabilities and safety of a new nanoscale drug delivery system.
Feasibility for modification
In designing a powerful preclinical experiment, finding a suitable model can be extremely challenging. With zebrafish models, a large library of transgenic lines is commercially available. Most commonly adopted lines express fluorescent proteins on the surface of specific organs to facilitate the tracking of nanoscale drug delivery systems or examination of phenotypic changes upon exposure to them (Figure 2C). Moreover, zebrafish models can also be tailored at needs through genetic engineering, xenotransplanting, and injecting bacilli [34,45,46,51,52].
Regulation
The regulation of animal use in research is becoming more stringent [53,54]. For example, in Europe, animals cannot be tested after 7 days post-fertilization. Zebrafish embryos start forming major organs within 24 hpf, which allows researchers to observe biodistribution and biotoxicity early in development (Figure 2D) [24].
Drawbacks
There have been factors that limited the use of zebrafish models. First, compared with other animal models such as mouse, it lacks an established protocol, which is a fact that significantly limits the ability to make meaningful comparisons and draw significant conclusions amongst different studies [55]. We hope that our suggested guideline can contribute to encourage the community to agree upon an established protocol for zebrafish models. Second, it is widely misunderstood that zebrafish’s low relevance to humans is not high enough for preclinical screenings of nanoscale drug delivery systems. However, in reality, zebrafish have similar organs and gene composition as humans. While mouse models have 75% genetic similarity to humans, zebrafish models have approximately 70% similarity [56].
Functional screening of nanoscale drug delivery systems with zebrafish models
Nanomaterials’ versatility allowed the development of nanoscale drug delivery systems with ingenuous functionalities such as targetting ability and light/heat-reactive releasing capability of loads [57–60]. However, until those capabilities are proven to perfectly work in in vivo settings, the nanomedicine cannot be clinically adopted [61]. In functional screening of nanoscale drug delivery systems, researchers can choose from various transgenic and disease models of zebrafish to design a powerful tool to verify the efficacy and capabilities of their nanoscale drug delivery system.
Transgenic models
Angiogenesis and anticancer drugs
As mentioned above, zebrafish models have transparent body to allow researchers to observe their blood vessels (BVs) and learn about the distribution and functionalities of nanoscale drug delivery systems [33]. Especially, because tumor development involves neovasculature, angiogenesis is an important indicator of tumor growth. Conversely, we can test the efficacy of our cancer treating nanoscale drug delivery systems by observing the inhibition of angiogenesis (Table 1) [62–66]. The BVs of zebrafish are readily observable by introducing fluorescent dyes [67,68]. Alkaline phosphate is the most widely used dye for staining the zebrafish embryos’ BVs [69,70]. This method has been used to observe the down-regulation of angiogenesis upon injection of an oncogenic signal pathway inhibitor (Table 1) [71]. If the dyeing process is too cumbersome, transgenic zebrafish lines with fluorescent BVs such as Tg(flk1:EGFP) [33,72] and Tg(flk1:mCherry) can be purchased (Table 1) [73].
Table 1. Preclinical studies of nanoscale drug delivery systems in the BVs of zebrafish models.
| Purpose | Drug delivery system | Vascular model | Cargo | Treatment method | Treatment time | Observation time | Ref. |
|---|---|---|---|---|---|---|---|
| Inhibition of angiogenesis | Polymeric micelle | Tg(flk1:mCherry) | Curcumin | Direct injection | 48 hpf | 10, 20, 40, 60 mpi | [73] |
| Tg(flk1:EGFP) | Quecertin | Direct incubation | 15 hpf; 54 hpf; | 15 hpi; 48 hpi; | [74] | ||
| WT | PI3K pathway inhibitor | Direct injection | 48 hpf | 48 hpi | [71] | ||
| Tg(flk1:EGFP) | Curcumin | Direct incubation | 48 hpf | 120 hpf | [75] | ||
| Tracking of nanomaterial | Polymeric micelle | Tg(flk1:EGFP) | Doxorubucin | Direct injection | 70 hpf | 6 hpi | [76] |
| Lipid nanodroplet | Tg(fli1:EGFP) | Cyanine dye | Direct injection | 72 hpf | 5–1 hpi | [77] |
Organ models and organ-specific drugs
Transgenic models of zebrafish with fluorescent organs are readily available for tracking labeled nanoscale drug delivery systems or for testing their efficacy [34,44,78–81]. Tg(BMP4:EGFP) is a model with green fluorescent myocardium, that has been used for functional screening of common cardioactive and cardiotoxic drugs (epinephrine, doxazosin, esmolol, and doxorubicin). With more advanced imaging tools, pseudodynamic 3D images of the beating zebrafish heart were used to analyze changes in heart function following drug delivery [82]. Likewise, various organ models of zebrafish, for example those with fluorescent liver, brain, or pancreas, can be used to monitor organ-specific response to different nanomaterials (Figure 2C).
Disease models
Although they have only been introduced to us a few decades ago, zebrafish models are starting to provide important insights into human disease because approximately 70% of zebrafish disease genes functionally match that of humans [66,83,84]. The most prevalent disease model is cancer model [69,71,74,85,86]. Moreover, various genetic engineering techniques or the uptake of bacilli can also induce various diseases in zebrafish models (Table 2) [87–92].
Table 2. Inducing disease in zebrafish models by injecting a xenograft or bacteria.
| Zebrafish model | Disease/cancer type | Method | Ref. |
|---|---|---|---|
| Tg(flk1:EGFP) | B16-F10 melanoma cells labeled with CM-DiI | Xenograft injection at 48 hpf | [74] |
| Tg(fli1:EGFP); Tg(mpeg1:mCherry); Tg(lyz;DsRed) | Mycobacterium marium (fish tuberculosis agent) with bacilli labeled with DsRed | Bacterial injection at 48–52 hpf | [87] |
| WT | MDA-MB-231/GFP; B16-F10 cells labeled with the QTracker Red kit | Xenograft injection at 48 hpf | [71] |
| WT | Methicillin-resistant strain of Staphylococcus aureus | Bacterial injection | [88] |
| rag2E450fs mutant (casper) | GFP-labeled BRAFV600E | Xenograft injection at 3 months | [93] |
Cancer models
There are several ways to produce cancer zebrafish models: chemical treatment, genetic technology, and xenotransplantation, the introduction of foreign tumor cells [66,84]. Exposure to dimethylbenzanthracene can induce intestinal cancer, and overexpression of Myc gene will cause T-cell leukemia in zebrafish [66]. Xenotransplantation can produce more various types of cancers compared with the other two methods [66,84]. The transplantation of human B16-F10 melanoma cells labeled with Qtracker red has been used to simulate human melanoma in zebrafish embryos (Table 2) [71]. Xenografts with fluorescent labels can be monitored after injection of nanoscale drug delivery system. Moreover, researchers could learn about metastasis by imaging in xenotransplanted zebrafish models by counting the number of circulating tumor cells, which is a good indicator for metastasis (Table 2) [74]. The growth of a transplanted GFP-labeled BRAFV600E xenograft and subsequent vascularization around it were observed using flk1:mCherry; rag2E450fs zebrafish models [93]. In addition, tumor heterogeneity can be investigated by distinguishing tumor cells by labeling with different fluorescent tags based on differentiation status. Similarly, crestin:EGFP zebrafish have been used to melanoma since crestin, which is expressed embryonically in neural crest progenitor cells, is re-expressed in melanoma [94]. They could observe the development of BRAFV600E by tracking the expression of crestin over 40 days with p53/BRAF/crestin:EGFP zebrafish [94].
Other disease models
Our knowledge about zebrafish genome sequence allowed us to produce various disease models of it [83,92]. For example, metabolic diseases such as obesity, type 2 diabetes, and atherosclerosis can now be produced through genetic engineering, while in the past, we relied on less objective diet control methods. Moreover, because zebrafish share much of human brain’s circuitry [92], brain disorder studies with zebrafish models are also an emerging field [95]. Anxiety, depression, cognitive disorder, social disorder, ADHD, neurodegeneration, serotonin syndrome, eating disorders, and sleep disorders are common human brain disorders that can be studied through biobehavioral assays with zebrafish models, such as counting zebrafish subjects with lackluster locomotion [83,95].
Recently, transgenic zebrafish lines with fluorescent leukocytes, along with the discovery of reporter for the macrophage lineage, fostered the study of macrophage–pathogen interactions with zebrafish models. A team found their drug delivery system designed to treat tuberculosis was found to colocalize within the bacilli of macrophages by using Tg(mpeg1:mCherry) model with fluorescent macrophages [87]. The types of bacteria used for infecting zebrafish include Salmonella typhimurium, Vibrio anguillarum, Bacillus subtilis, Listeria monocytogenes, Mycobacterium marinum, Burkholderia cenocepacia, S. aureus, Shigella flexneri, and Candida albicans (Table 2) [91,96].
Toxicity screening for nanoscale drug delivery systems with zebrafish models
Any new drug delivery system is of no use if it is not safe. Therefore, many successfully funded nanoscale drug delivery system development processes often include exhaustive toxicity screening with mouse models. However, preclinical studies with mouse models can be extremely time and labor consuming, and moreover, expensive for most research labs. In vitro toxicity assessments, which they often compromise for testing the safety of their nanoscale drug delivery systems, cannot mimic the exposure in human body (Table 5). By adopting toxicity screening with less demanding zebrafish models, we can foster the community to produce more biosafe nanoscale drug delivery systems (Figure 3) [2].
Table 5. Models and methods used for toxicity screening in nanoscale drug delivery system research with zebrafish models.
| Model | Method | Drug delivery system/nanomaterial | Drug/cargo | Ref. |
|---|---|---|---|---|
| Zebrafish embryos | Direct incubation | Ag nanoparticles | N/A | [101] |
| Au nanoparticles | N/A | [98] | ||
| Mesoporous silica nanoparticles capped with β-cyclodextrin | N/A | [99] | ||
| Hydroxyapatite nanoparticles | N/A | [100] | ||
| Au nanoparticles | 6-mercaptopurine | [97] | ||
| Graphene nanoparticles | Curcumin | [103] | ||
| Direct injection | Ag nanoshell | N/A | [104] | |
| Graphene nanoparticles | N/A | [105] | ||
| Lipid nanodroplet | Cyanine dye | [77] | ||
| Polymer nanoparticles | LY294002 | [72] | ||
| Cells | MTT assay | Polymicelles | Curcumin | [75] |
| Polymicelles | Doxorubicin | [76] | ||
| ZnO micronanostructures | N/A | [106] | ||
| Lipid nanodroplet | Cyanine dye | [77] | ||
| Graphene nanoparticles | Curcumin | [103] | ||
| Polymer nanoparticles | LY294002 | [71] | ||
| PEG PCL nanoparticles | Quecertin | [74] | ||
| N/A | Graphene nanoparticles | GFP | [107] | |
| Silica-based colloidosomes | All trans-retinoic acid | [108] | ||
| Iron oxide nanoparticles | Cisplatin | [109] | ||
| Copolymer micelles | Curcumin | [73] |
Only some studies that used zebrafish models for studying efficacy and biodistribution kept the same model for toxicity screenings. A few studies used in vitro model, and few omitted the toxicity screening. Bold: Subjectts of toxicity screening
Figure 3. Zebrafish models for preclinical studies of nanoscale drug delivery systems.
(A) Therapeutic biology researches to study efficacy of anticancer treatments using zebrafish. (B) Biodistribution researches to study through tracking and imaging with fluorescent nanomaterials using transparent zebrafish embryos. (C) Biotoxicity researches within the zebrafish to evaluate and resolve concerns regarding toxicity of nanomaterials.
Zebrafish is an ideal model for the study of toxicity screening because a zebrafish embryo mimics the complexity of interactions in the human body. With a high degree of homology to human genome and biological systems, zebrafish embryos can be used to monitor the phenotypic and genotypic abnormalities upon exposure to nanomaterials. Observing change in the size and shape of organs during development is simple yet valuable indicators of biotoxicity. Low husbandry cost, rapid development, and ease in handling allow rapid high throughput and cost-effective preclinical screenings [2,97].
Unfortunately, even among the nanoscale delivery system studies that used zebrafish as animal models, only a few of them included the toxicity screening with zebrafish models. (Table 5). Most commonly, the embryos’ hatching rates and survival rates were observed at 72 hpf. Phenotypic deformations were monitored after 4 h post-incubation with different concentrations of nanomaterials in 24-wells. The aberrations in tail length, poor pigmentation, tail bending, and organ defects at higher concentrations represented phenotypic deformities due to drug delivery systems [97–100]. Nadrah et al. [99] applied additional assessments during 24 hpf through 47 hpf, which included observing characteristics such as egg coagulation, missing heartbeat, missing somites, missing tail detachment from the yolk sac, no eye and body pigmentation, missing blood flow, spine deformation, yolk sac edema, and incomplete eye and ear development. Uniquely, Daniel et al. [101] fed chironoma incubated with silver nanoparticles to study toxic effects and biodistribution of silver nanoparticles. Also by using whole body X-ray and UV-Visible fluorescence spectrum, they demonstrated that the silver nanoparticles penetrated the blood–brain barrier to reach the brain.
Investigating intracellular fate of nanomaterials in zebrafish can be done via TEM analysis of ultrathin sections of zebrafish subjects (Table 3) [26,66,102]. He et al. used the micrographs ultrathin sections of muscle cell to observe the intracellular deposits of S-TiO2 nanoparticles [26] The micrographs showed both lysosome and endosome formation, which indicated that the nanoparticles were introduced through receptor-mediated mechanism rather than simple diffusion [26]. Muth-Kohne et al. [66] also confirmed the cellular uptake of Ag nanoparticles by the lumen of developing gut and erythrocytes through TEM analysis. Sectioning specific organs such as kidney can offer insights into bioaccumulation and toxicity at specific organs as well. TEM analysis can be used to confirm the uptake of drug delivery systems and their uptake mechanisms.
Table 3. TEM analysis of zebrafish models.
Inductively coupled plasma MS (ICP-MS) is another way to confirm and quantitate the uptake of nanoscale drug delivery system by zebrafish embryos (Table 4) [83,92,95,96]. Elemental contents of the zebrafish embryos are analyzed by fixing and dissolving the embryos in a solution. For example, Zarco-Fernandez et al. [83] monitored Cd concentration in the embryos to quantitate quantum dot uptake.
Table 4. ICP-MS analysis of zebrafish models.
A guideline for preclinical screenings of nanoscale drug delivery system with zebrafish models
We compiled a list of toxicity screening methods employed by papers that used zebrafish models for testing capabilities of their respective nanomaterials (Table 6). It was frustrating to notice that more than half of the papers did not perform the toxicity assessments on zebrafish models despite their knowledge about it. In order to foster future papers to include simple yet powerful assays to confirm the safety of their nanoscale drug delivery systems on a living organism, we benchmarked different papers to suggest various toxicity screening assays using zebrafish embryos (Table 6).
Table 6. Proposed recommendations for preclinical studies of nanoscale drug delivery systems with zebrafish models.
| Direct incubation | Direct injection | |
|---|---|---|
| Treatment time point | 6 hpf | 48 hpf |
| Observation time point | 48, 72, 96, 168 hpf | 1, 24, 48, 72, 96, 120 hpi |
| Hatching/mortality rate observation time point | 72 hpf | |
| Heartbeat observation time point | 48, 72, 96 hpf | |
| Biodistribution observation | TEM analysis | |
| Nanomaterials uptake quantitation | ICP-MS analysis |
Bold: the time points for certain actions in preclinical studies
Abbreviation: hpi, h post injection.
In direct incubation method, the zebrafish embryos were exposed to the solutions of nanomaterials at 6 hpf [68,110–112]. Upon incubation, the biodistribution and efficacy of nanoscale drug delivery systems can be monitored at 48, 72, 96, and 168 hpf. For direct injection method, nanomaterials can be injected to the embryos at 48 hpf, after completing vascular development [68,113]. First observation can be made at 1 h post injection, and subsequent observations can be made at 24-h intervals for long-term effects.
The mortality and hatching rates of zebrafish embryos are the most commonly and conveniently monitored indicators of the biotoxicity. Both factors are measured at 72 hpf when the embryos normally hatch [110–112,114]. Milder toxic effects are usually reflected through heart defects, which can be assessed by monitoring the heart rate [24,45,110–112]. We recommend counting heartbeats for a 30-s period at 48, 72, and 96 hpf when the heart is fully developed. Additionally, liver, the site of nanomaterial accumulation, can be monitored from 96 hpf with 24-h intervals.
Conclusion
Functional and toxicological screenings of nanomaterials are essential for successful development of nanoscale drug delivery system, especially when the safety of nanomedicine is continuously questioned. However, many related studies fail to include preclinical studies with animal models because they normally cost considerable labor, money, and time. Zebrafish is a great alternative animal model, wrongly perceived to have poor homology to humans. However as mentioned above, zebrafish share most of disease genes and biological systems with humans. Moreover, the advantages of zebrafish model make it a versatile animal model for nanomedicine research.
Last, recent studies with zebrafish models are performed under a wide range of experimental conditions making comparison and benchmarking almost impossible. Therefore, we included a guideline for people who want to adopt zebrafish models into their research. We hope that in the future, a protocol for zebrafish will be established to accelerate the clinical use of nanoscale drug delivery systems.
Acknowledgments
We thank the Korea Zebrafish Resource Bank and appreciate Mr Su Chang Mun for his graphical artworks.
Abbreviations
- BV
blood vessel
- hpf
h post fertilization
- ICP-MS
inductively coupled plasma MS
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This work was supported by the Korea Health Technology R&D Project of Korea Health Industry Development Institute (KHIDI) [grant number HI15C3078]; the NRF Bio & Medical Technology Development Program by the Korean Government [grant number NRF-2015M3A9E2029265]; the TRC (Translational Research Center) project of KIST [grant number 2V05420]; and the Ministry of Health and Welfare, Republic of Korea [grant number HI15C3078].
References
- 1.Liu L., Ye Q., Lu M., Lo Y.C., Hsu Y.H., Wei M.C. et al. (2015) A new approach to reduce toxicities and to improve bioavailabilities of platinum-containing anti-cancer nanodrugs. Sci. Rep. 5, 10881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chakraborty C., Sharma A.R., Sharma G. and Lee S.S. (2016) Zebrafish: A complete animal model to enumerate the nanoparticle toxicity. J. Nanobiotechnology 14, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagarwal R.C., Kant S., Singh P.N., Maiti P. and Pandit J.K. (2009) Polymeric nanoparticulate system: a potential approach for ocular drug delivery. J. Control. Release 136, 2–13 [DOI] [PubMed] [Google Scholar]
- 4.Galloway J.F., Winter A., Lee K.H., Park J.H., Dvoracek C.M., Devreotes P. et al. (2012) Quantitative characterization of the lipid encapsulation of quantum dots for biomedical applications. Nanomedicine 8, 1190–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee K.H., Galloway J.F., Park J., Dvoracek C.M., Dallas M., Konstantopoulos K. et al. (2012) Quantitative molecular profiling of biomarkers for pancreatic cancer with functionalized quantum dots. Nanomedicine 8, 1043–1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jang G.H., Hwang M.P., Kim S.Y., Jang H.S. and Lee K.H. (2014) A systematic in-vivo toxicity evaluation of nanophosphor particles via zebrafish models. Biomaterials 35, 440–449 [DOI] [PubMed] [Google Scholar]
- 7.Park H., Hwang M.P., Lee J.W., Choi J. and Lee K.H. (2013) Harnessing immunomagnetic separation and quantum dot-based quantification capacities for the enumeration of absolute levels of biomarker. Nanotechnology 24, 285103. [DOI] [PubMed] [Google Scholar]
- 8.Hwang M.P., Lee J.W., Lee K.E. and Lee K.H. (2013) Think modular: a simple apoferritin-based platform for the multifaceted detection of pancreatic cancer. ACS Nano 7, 8167–8174 [DOI] [PubMed] [Google Scholar]
- 9.Dawidczyk C.M., Kim C., Park J.H., Russell L.M., Lee K.H., Pomper M.G. et al. (2014) State-of-the-art in design rules for drug delivery platforms: lessons learned from FDA-approved nanomedicines. J. Control. Release 187, 133–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeun M., Park S., Jang G.H. and Lee K.H. (2014) Tailoring MgxMn1-xFe2O4 superparamagnetic nanoferrites for magnetic fluid hyperthermia applications. ACS Appl. Mater. Interfaces 6, 16487–16492 [DOI] [PubMed] [Google Scholar]
- 11.Flicek P., Amode M.R., Barrell D., Beal K., Billis K., Brent S. et al. (2014) Ensembl 2014. Nucleic Acids Res. 42, D749–D755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jang H.J., Ahn J., Kim M.G., Shin Y.B., Jeun M., Cho W.J. et al. (2014) Electrical signaling of enzyme-linked immunosorbent assays with an ion-sensitive field-effect transistor. Biosens. Bioelectron. 64, 318–323 [DOI] [PubMed] [Google Scholar]
- 13.Kim K.-T. and Tanguay R.L. (2013) Integrating zebrafish toxicology and nanoscience for safer product development. Green Chem. 15, 872–880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grainger D.W. (2013) Connecting drug delivery reality to smart materials design. Int. J. Pharm. 454, 521–524 [DOI] [PubMed] [Google Scholar]
- 15.Veldman M.B. and Lin S. (2008) Zebrafish as a developmental model organism for pediatric research. Pediatr. Res. 64, 470–476 [DOI] [PubMed] [Google Scholar]
- 16.Bilotta J., Saszik S., DeLorenzo A.S. and Hardesty H.R. (1999) Establishing and maintaining a low-cost zebrafish breeding and behavioral research facility. Behav. Res. Methods Instrum. Comput. 31, 178–184 [DOI] [PubMed] [Google Scholar]
- 17.Macrae I.M. (2011) Preclinical stroke research–advantages and disadvantages of the most common rodent models of focal ischaemia. Br. J. Pharmacol. 164, 1062–1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chatzigeorgiou A., Halapas A., Kalafatakis K. and Kamper E. (2009) The use of animal models in the study of diabetes mellitus. In Vivo 23, 245–258 [PubMed] [Google Scholar]
- 19.Chong A.S., Alegre M.-L., Miller M.L. and Fairchild R.L. (2013) Lessons and limits of mouse models. Cold Spring Harb. Perspect. Med. 3, a015495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mathis C.A., Wang Y., Holt D.P., Huang G.-F., Debnath M.L. and Klunk W.E. (2003) Synthesis and evaluation of 11C-labeled 6-substituted 2-arylbenzothiazoles as amyloid imaging agents. J. Med. Chem. 46, 2740–2754 [DOI] [PubMed] [Google Scholar]
- 21.Devine S.M., Cobbs C., Jennings M., Bartholomew A. and Hoffman R. (2003) Mesenchymal stem cells distribute to a wide range of tissues following systemic infusion into nonhuman primates. Blood 101, 2999–3001 [DOI] [PubMed] [Google Scholar]
- 22.Chimpanzee Sequencing and Analysis Consortium (2005) Initial sequence of the chimpanzee genome and comparison with the human genome. Nature 437, 69–87 [DOI] [PubMed] [Google Scholar]
- 23.Fako V.E. and Furgeson D.Y. (2009) Zebrafish as a correlative and predictive model for assessing biomaterial nanotoxicity. Adv. Drug Deliv. Rev. 61, 478–486 [DOI] [PubMed] [Google Scholar]
- 24.McGrath P. and Li C.-Q. (2008) Zebrafish: a predictive model for assessing drug-induced toxicity. Drug Discov. Today 13, 394–401 [DOI] [PubMed] [Google Scholar]
- 25.Lee K.J., Nallathamby P.D., Browning L.M., Osgood C.J. and Xu X.H. (2007) In vivo imaging of transport and biocompatibility of single silver nanoparticles in early development of zebrafish embryos. ACS Nano 1, 133–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He X., Aker W.G. and Hwang H.M. (2014) An in vivo study on the photo-enhanced toxicities of S-doped TiO nanoparticles to zebrafish embryos (Danio rerio) in terms of malformation, mortality, rheotaxis dysfunction, and DNA damage. Nanotoxicology 8, 185–195 [DOI] [PubMed] [Google Scholar]
- 27.Ozel R.E., Hayat A., Wallace K.N. and Andreescu S. (2013) Effect of cerium oxide nanoparticles on intestinal serotonin in zebrafish. RSC Adv. 3, 15298–15309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.George S., Lin S., Ji Z., Thomas C.R., Li L.J, Mecklenburg M. et al. (2012) Surface defects on plate-shaped silver nanoparticles contribute to its hazard potential in a fish gill cell line and zebrafish embryos. ACS Nano 6, 3745–3759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones C.F., Campbell R.A., Brooks A.E., Assemi S., Tadjiki S., Thiagarajan G. et al. (2012) Cationic PAMAM dendrimers aggressively initiate blood clot formation. ACS Nano 6, 9900–9910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zon L.I. and Peterson R.T. (2005) In vivo drug discovery in the zebrafish. Nat. Rev. Drug Discov. 4, 35–44 [DOI] [PubMed] [Google Scholar]
- 31.Lawrence C. (2007) The husbandry of zebrafish (Danio rerio): a review. Aquaculture 269, 1–20 [Google Scholar]
- 32.Berghmans S., Jette C., Langenau D., Hsu K., Stewart R., Look T. et al. (2005) Making waves in cancer research: new models in the zebrafish. Biotechniques 39, 227–237 [DOI] [PubMed] [Google Scholar]
- 33.Stoletov K., Montel V., Lester R.D., Gonias S.L. and Klemke R. (2007) High-resolution imaging of the dynamic tumor cell vascular interface in transparent zebrafish. Proc. Natl. Acad. Sci. U.S.A. 104, 17406–17411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dooley K. and Zon L.I. (2000) Zebrafish: a model system for the study of human disease. Curr. Opin. Genet. Dev. 10, 252–256 [DOI] [PubMed] [Google Scholar]
- 35.Liu S. and Leach S.D. (2011) Zebrafish models for cancer. Annu. Rev. Pathol. 6, 71–93 [DOI] [PubMed] [Google Scholar]
- 36.Asnani A. and Peterson R.T. (2014) The zebrafish as a tool to identify novel therapies for human cardiovascular disease. Dis. Model. Mech. 7, 763–767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Newman M., Ebrahimie E. and Lardelli M. (2014) Using the zebrafish model for Alzheimer’s disease research. Front. Genet. 5, 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parng C., Seng W.L., Semino C. and McGrath P. (2002) Zebrafish: a preclinical model for drug screening. Assay Drug Dev. Technol. 1, 41–48 [DOI] [PubMed] [Google Scholar]
- 39.Kelsh R.N., Brand M., Jiang Y.J., Heisenberg C.P., Lin S., Haffter P. et al. (1996) Zebrafish pigmentation mutations and the processes of neural crest development. Development 123, 369–389 [DOI] [PubMed] [Google Scholar]
- 40.Dai Y.J., Jia Y.F., Chen N., Bian W.P., Li Q.K., Ma Y.B. et al. (2014) Zebrafish as a model system to study toxicology. Environ. Toxicol. Chem. 33, 11–17 [DOI] [PubMed] [Google Scholar]
- 41.Vacaru A.M., Unlu G., Spitzner M., Mione M., Knapik E.W. and Sadler K.C. (2014) In vivo cell biology in zebrafish - providing insights into vertebrate development and disease. J. Cell Sci. 127, 485–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jegstrup I.M. and Rosenkilde P. (2003) Regulation of post-larval development in the European eel: thyroid hormone level, progress of pigmentation and changes in behaviour. J. Fish Biol. 63, 168–175 [Google Scholar]
- 43.Alestrom P., Holter J.L. and Nourizadeh-Lillabadi R. (2006) Zebrafish in functional genomics and aquatic biomedicine. Trends Biotechnol. 24, 15–21 [DOI] [PubMed] [Google Scholar]
- 44.Lieschke G.J. and Currie P.D. (2007) Animal models of human disease: zebrafish swim into view. Nat. Rev. Genet. 8, 353–367 [DOI] [PubMed] [Google Scholar]
- 45.Briggs J.P. (2002) The zebrafish: a new model organism for integrative physiology. Am. J. Physiol. Regul. Integr. Comp. Physiol. 282, R3–R9 [DOI] [PubMed] [Google Scholar]
- 46.White R.M., Sessa A., Burke C., Bowman T., LeBlanc J., Ceol C. et al. (2008) Transparent adult zebrafish as a tool for in vivo transplantation analysis. Cell Stem Cell 2, 183–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang C.J., Tu C.T., Hsiao C.D., Hsieh F.J. and Tsai H.J. (2003) Germ‐line transmission of a myocardium‐specific GFP transgene reveals critical regulatory elements in the cardiac myosin light chain 2 promoter of zebrafish. Dev. Dyn. 228, 30–40 [DOI] [PubMed] [Google Scholar]
- 48.Burns C.G., Milan D.J., Grande E.J., Rottbauer W., MacRae C.A. and Fishman M.C. (2005) High-throughput assay for small molecules that modulate zebrafish embryonic heart rate. Nat. Chem. Biol. 1, 263–264 [DOI] [PubMed] [Google Scholar]
- 49.Ju B., Xu Y., He J., Liao J., Yan T., Hew C.L. et al. (1999) Faithful expression of green fluorescent protein(GFP) in transgenic zebrafish embryos under control of zebrafish gene promoters. Dev. Genet. 25, 158–167 [DOI] [PubMed] [Google Scholar]
- 50.Segner H. (2009) Zebrafish (Danio rerio) as a model organism for investigating endocrine disruption. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 149, 187–195 [DOI] [PubMed] [Google Scholar]
- 51.Staton C.A., Stribbling S.M., Tazzyman S., Hughes R., Brown N.J. and Lewis C.E. (2004) Current methods for assaying angiogenesis in vitro and in vivo. Int. J. Exp. Pathol. 85, 233–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kari G., Rodeck U. and Dicker A.P. (2007) Zebrafish: an emerging model system for human disease and drug discovery. Clin. Pharmacol. Ther. 82, 70–80 [DOI] [PubMed] [Google Scholar]
- 53.Bovenkerk B. and Kaldewaij F. (2015) The use of animal models in behavioural neuroscience research. Curr. Top. Behav. Neurosci., 19 17–46 [DOI] [PubMed] [Google Scholar]
- 54.McGrath J.C., Drummond G.B., McLachlan E.M., Kilkenny C. and Wainwright C.L. (2010) Guidelines for reporting experiments involving animals: the ARRIVE guidelines. Br. J. Pharmacol. 160, 1573–1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katt M.E., Placone A.L., Wong A.D., Xu Z.S. and Searson P.C. (2016) In vitro tumor models: advantages, disadvantages, variables, and selecting the right platform. Front. Bioeng. Biotechnol. 4, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barbazuk W.B., Korf I., Kadavi C., Heyen J., Tate S., Wun E. et al. (2000) The syntenic relationship of the zebrafish and human genomes. Genome Res. 10, 1351–1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang Y., Nayak T.R., Hong H. and Cai W. (2012) Graphene: a versatile nanoplatform for biomedical applications. Nanoscale 4, 3833–3842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McCarthy J.R. and Weissleder R. (2008) Multifunctional magnetic nanoparticles for targeted imaging and therapy. Adv. Drug. Deliv. Rev. 60, 1241–1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huang X., El-Sayed I.H., Qian W. and El-Sayed M.A. (2006) Cancer cell imaging and photothermal therapy in the near-infrared region by using gold nanorods. J. Am. Chem. Soc. 128, 2115–2120 [DOI] [PubMed] [Google Scholar]
- 60.Kim J., Piao Y. and Hyeon T. (2009) Multifunctional nanostructured materials for multimodal imaging, and simultaneous imaging and therapy. Chem. Soc. Rev. 38, 372–390 [DOI] [PubMed] [Google Scholar]
- 61.Nijhara R. and Balakrishnan K. (2006) Bringing nanomedicines to market: regulatory challenges, opportunities, and uncertainties. Nanomed. Nanotechnol. Biol. Med. 2, 127–136 [DOI] [PubMed] [Google Scholar]
- 62.Haldi M., Ton C., Seng W.L. and McGrath P. (2006) Human melanoma cells transplanted into zebrafish proliferate, migrate, produce melanin, form masses and stimulate angiogenesis in zebrafish. Angiogenesis 9, 139–151 [DOI] [PubMed] [Google Scholar]
- 63.Stern H.M. and Zon L.I. (2003) Cancer genetics and drug discovery in the zebrafish. Nat. Rev. Cancer 3, 533–539 [DOI] [PubMed] [Google Scholar]
- 64.Amatruda J.F., Shepard J.L., Stern H.M. and Zon L.I. (2002) Zebrafish as a cancer model system. Cancer Cell 1, 229–231 [DOI] [PubMed] [Google Scholar]
- 65.Stoletov K. and Klemke R. (2008) Catch of the day: zebrafish as a human cancer model. Oncogene 27, 4509–4520 [DOI] [PubMed] [Google Scholar]
- 66.Muth-Kohne E., Sonnack L., Schlich K., Hischen F., Baumgartner W., Hund-Rinke K. et al. (2013) The toxicity of silver nanoparticles to zebrafish embryos increases through sewage treatment processes. Ecotoxicology 22, 1264–1277 [DOI] [PubMed] [Google Scholar]
- 67.Jin S.-W., Beis D., Mitchell T., Chen J.-N. and Stainier D.Y. (2005) Cellular and molecular analyses of vascular tube and lumen formation in zebrafish. Development 132, 5199–5209 [DOI] [PubMed] [Google Scholar]
- 68.Lawson N.D. and Weinstein B.M. (2002) In vivo imaging of embryonic vascular development using transgenic zebrafish. Dev. Biol. 248, 307–318 [DOI] [PubMed] [Google Scholar]
- 69.Nicoli S., Ribatti D., Cotelli F. and Presta M. (2007) Mammalian tumor xenografts induce neovascularization in zebrafish embryos. Cancer Res. 67, 2927–2931 [DOI] [PubMed] [Google Scholar]
- 70.Habeck H., Odenthal J., Walderich B., Maischein H.-M. and Schulte-Merker S. (2002) Analysis of a zebrafish VEGF receptor mutant reveals specific disruption of angiogenesis. Curr. Biol. 12, 1405–1412 [DOI] [PubMed] [Google Scholar]
- 71.Harfouche R., Basu S., Soni S., Hentschel D.M., Mashelkar R.A. and Sengupta S. (2009) Nanoparticle-mediated targeting of phosphatidylinositol-3-kinase signaling inhibits angiogenesis. Angiogenesis 12, 325–338 [DOI] [PubMed] [Google Scholar]
- 72.Blum Y., Belting H.-G., Ellertsdottir E., Herwig L., Lüders F. and Affolter M. (2008) Complex cell rearrangements during intersegmental vessel sprouting and vessel fusion in the zebrafish embryo. Dev. Biol. 316, 312–322 [DOI] [PubMed] [Google Scholar]
- 73.Gao X., Zheng F., Guo G., Liu X., Fan R., Z-y Qian et al. (2013) Improving the anti-colon cancer activity of curcumin with biodegradable nano-micelles. J. Mater. Chem. B 1, 5778–5790 [DOI] [PubMed] [Google Scholar]
- 74.Wu Q., Deng S., Li L., Sun L., Yang X., Liu X. et al. (2013) Biodegradable polymeric micelle-encapsulated quercetin suppresses tumor growth and metastasis in both transgenic zebrafish and mouse models. Nanoscale 5, 12480–12493 [DOI] [PubMed] [Google Scholar]
- 75.Gou M., Men K., Shi H., Xiang M., Zhang J., Song J. et al. (2011) Curcumin-loaded biodegradable polymeric micelles for colon cancer therapy in vitro and in vivo. Nanoscale 3, 1558–1567 [DOI] [PubMed] [Google Scholar]
- 76.Gou M., Shi H., Guo G., Men K., Zhang J., Zheng L. et al. (2011) Improving anticancer activity and reducing systemic toxicity of doxorubicin by self-assembled polymeric micelles. Nanotechnology 22, 095102. [DOI] [PubMed] [Google Scholar]
- 77.Kilin V.N., Anton H., Anton N., Steed E., Vermot J., Vandamme T.F. et al. (2014) Counterion-enhanced cyanine dye loading into lipid nano-droplets for single-particle tracking in zebrafish. Biomaterials 35, 4950–4957 [DOI] [PubMed] [Google Scholar]
- 78.Korzh S., Pan X., Garcia-Lecea M., Winata C.L., Pan X., Wohland T. et al. (2008) Requirement of vasculogenesis and blood circulation in late stages of liver growth in zebrafish. BMC Dev. Biol 8, 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Huang H., Vogel S.S., Liu N., Melton D.A. and Lin S. (2001) Analysis of pancreatic development in living transgenic zebrafish embryos. Mol. Cell Endocrinol. 177, 117–124 [DOI] [PubMed] [Google Scholar]
- 80.Higashijima S.-I., Okamoto H., Ueno N., Hotta Y. and Eguchi G. (1997) High-frequency generation of transgenic zebrafish which reliably express GFP in whole muscles or the whole body by using promoters of zebrafish origin. Dev. Biol. 192, 289–299 [DOI] [PubMed] [Google Scholar]
- 81.Park H.-C., Kim C.-H., Bae Y.-K., Yeo S.-Y., Kim S.-H., Hong S.-K. et al. (2000) Analysis of upstream elements in the HuC promoter leads to the establishment of transgenic zebrafish with fluorescent neurons. Dev. Biol. 227, 279–293 [DOI] [PubMed] [Google Scholar]
- 82.Lin K.-Y., Chang W.-T., Lai Y.-C. and Liau I. (2014) Toward functional screening of cardioactive and cardiotoxic drugs with zebrafish in vivo using pseudodynamic three-dimensional imaging. Anal. Chem. 86, 2213–2220 [DOI] [PubMed] [Google Scholar]
- 83.Zarco-Fernandez S., Coto-Garcia A.M., Munoz-Olivas R., Sanz-Landaluze J., Rainieri S. and Camara C. (2016) Bioconcentration of ionic cadmium and cadmium selenide quantum dots in zebrafish larvae. Chemosphere 148, 328–335 [DOI] [PubMed] [Google Scholar]
- 84.White R., Rose K. and Zon L. (2013) Zebrafish cancer: the state of the art and the path forward. Nat. Rev. Cancer 13, 624–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nicoli S. and Presta M. (2007) The zebrafish/tumor xenograft angiogenesis assay. Nat. Protoc. 2, 2918–2923 [DOI] [PubMed] [Google Scholar]
- 86.Konantz M., Balci T.B., Hartwig U.F., Dellaire G., André M.C., Berman J.N. et al. (2012) Zebrafish xenografts as a tool for in vivo studies on human cancer. Ann. N. Y. Acad. Sci. 1266, 124–137 [DOI] [PubMed] [Google Scholar]
- 87.Fenaroli F., Westmoreland D., Benjaminsen J., Kolstad T., Skjeldal F.M., Meijer A.H. et al. (2014) Nanoparticles as drug delivery system against tuberculosis in zebrafish embryos: direct visualization and treatment. ACS Nano 8, 7014–7026 [DOI] [PubMed] [Google Scholar]
- 88.Xiong M.H., Li Y.J., Bao Y., Yang X.Z., Hu B. and Wang J. (2012) Bacteria‐responsive multifunctional nanogel for targeted antibiotic delivery. Adv. Mater. 24, 6175–6180 [DOI] [PubMed] [Google Scholar]
- 89.Astrofsky K.M., Schrenzel M.D., Bullis R.A., Smolowitz R.M. and Fox J.G. (2000) Diagnosis and management of atypical Mycobacterium spp. infections in established laboratory zebrafish (Brachydanio rerio) facilities. Comp. Med. 50, 666–672 [PubMed] [Google Scholar]
- 90.Cao Y., He S., Zhou Z., Zhang M., Mao W., Zhang H. et al. (2012) Orally administered thermostable N-acyl homoserine lactonase from Bacillus sp. strain AI96 attenuates Aeromonas hydrophila infection in zebrafish. Appl. Environ. Microbiol. 78, 1899–1908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.van der Sar A.M., Appelmelk B.J., Vandenbroucke-Grauls C.M. and Bitter W. (2004) A star with stripes: zebrafish as an infection model. Trends Microbiol. 12, 451–457 [DOI] [PubMed] [Google Scholar]
- 92.Bohme S., Stark H.J., Kuhnel D. and Reemtsma T. (2015) Exploring LA-ICP-MS as a quantitative imaging technique to study nanoparticle uptake in Daphnia magna and zebrafish (Danio rerio) embryos. Anal. Bioanal. Chem. 407, 5477–5485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tang Q., Moore J.C., Ignatius M.S., Tenente I.M., Hayes M.N., Garcia E.G. et al. (2016) Imaging tumour cell heterogeneity following cell transplantation into optically clear immune-deficient zebrafish. Nat. Commun. 7, 10358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kaufman C.K., Mosimann C., Fan Z.P., Yang S., Thomas A.J., Ablain J. et al. (2016) A zebrafish melanoma model reveals emergence of neural crest identity during melanoma initiation. Science 351, aad2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lin S., Taylor A.A., Ji Z., Chang C.H., Kinsinger N.M., Ueng W. et al. (2015) Understanding the transformation, speciation, and hazard potential of copper particles in a model septic tank system using zebrafish to monitor the effluent. ACS Nano 9, 2038–2048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gao J., Sepulveda M.S., Klinkhamer C., Wei A., Gao Y. and Mahapatra C.T. (2015) Nanosilver-coated socks and their toxicity to zebrafish (Danio rerio) embryos. Chemosphere 119, 948–952 [DOI] [PubMed] [Google Scholar]
- 97.Ganeshkumar M., Sastry T.P., Kumar M.S., Dinesh M.G., Kannappan S. and Suguna L. (2012) Sun light mediated synthesis of gold nanoparticles as carrier for 6-mercaptopurine: preparation, characterization and toxicity studies in zebrafish embryo model. Mater. Res. Bull. 47, 2113–2119 [Google Scholar]
- 98.Ganeshkumar M., Ponrasu T., Raja M.D., Subamekala M.K. and Suguna L. (2014) Green synthesis of pullulan stabilized gold nanoparticles for cancer targeted drug delivery. Spectrochim. Acta A Mol. Biomol. Spectrosc. 130, 64–71 [DOI] [PubMed] [Google Scholar]
- 99.Nadrah P., Maver U., Jemec A., Tišler T., Bele M., Dražić G. et al. (2013) Hindered disulfide bonds to regulate release rate of model drug from mesoporous silica. ACS Appl. Mater. Interfaces 5, 3908–3915 [DOI] [PubMed] [Google Scholar]
- 100.Zhao X., Ong K.J., Ede J.D., Stafford J.L., Ng K.W., Goss G.G. et al. (2013) Evaluating the toxicity of hydroxyapatite nanoparticles in catfish cells and zebrafish embryos. Small 9, 1734–1741 [DOI] [PubMed] [Google Scholar]
- 101.Daniel K., Kumar R., Sathish V., Sivakumar M., Sunitha S. and Sironmani T.A. (2011) Green synthesis (Ocimum tenuiflorum) of silver nanoparticles and toxicity studies in zebra fish (Danio rerio) model. Int. J. Nano Sci. Nanotechnol. 2, 103–117 [Google Scholar]
- 102.Jang G.H., Lee K.Y., Choi J., Kim S.H. and Lee K.H. (2016) Multifaceted toxicity assessment of catalyst composites in transgenic zebrafish embryos. Environ. Pollut. 216, 755–763 [DOI] [PubMed] [Google Scholar]
- 103.Liu C.-W., Xiong F., Jia H.-Z., Wang X.-L., Cheng H., Sun Y.-H. et al. (2013) Graphene-based anticancer nanosystem and its biosafety evaluation using a zebrafish model. Biomacromolecules 14, 358–366 [DOI] [PubMed] [Google Scholar]
- 104.Lukianova-Hleb E., Santiago C., Wagner D.S., Hafner J. and Lapotko D.O. (2010) Generation and detection of plasmonic nanobubbles in zebrafish. Nanotechnology 21, 225102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gollavelli G. and Ling Y.-C. (2012) Multi-functional graphene as an in vitro and in vivo imaging probe. Biomaterials 33, 2532–2545 [DOI] [PubMed] [Google Scholar]
- 106.Mishra Y.K., Adelung R., Röhl C., Shukla D., Spors F. and Tiwari V. (2011) Virostatic potential of micro-nano filopodia-like ZnO structures against herpes simplex virus-1. Antiviral Res. 92, 305–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhou X., Laroche F., Lamers G.E., Torraca V., Voskamp P., Lu T. et al. (2012) Ultra-small graphene oxide functionalized with polyethylenimine (PEI) for very efficient gene delivery in cell and zebrafish embryos. Nano Res. 5, 703–709 [Google Scholar]
- 108.Porta F. and Kros A. (2013) Colloidosomes as single implantable beads for the in vivo delivery of hydrophobic drugs. Part. Part. Syst. Charact. 30, 606–613 [Google Scholar]
- 109.Wang J., Wang X., Song Y., Zhu C., Wang J., Wang K. et al. (2013) Detecting and delivering platinum anticancer drugs using fluorescent maghemite nanoparticles. Chem. Commun. (Camb.) 49, 2786–2788 [DOI] [PubMed] [Google Scholar]
- 110.Kimmel C.B., Kane D.A., Walker C., Warga R.M. and Rothman M.B. (1989) A mutation that changes cell movement and cell fate in the zebrafish embryo. Nature 337, 358–362 [DOI] [PubMed] [Google Scholar]
- 111.Grandel H., Kaslin J., Ganz J., Wenzel I. and Brand M. (2006) Neural stem cells and neurogenesis in the adult zebrafish brain: origin, proliferation dynamics, migration and cell fate. Dev. Biol. 295, 263–277 [DOI] [PubMed] [Google Scholar]
- 112.Kozlowski D.J., Murakami T., Ho R.K. and Weinberg E.S. (1997) Regional cell movement and tissue patterning in the zebrafish theirembryo revealed by fate mapping with caged fluorescein. Biochem. Cell. Biol. 75, 551–562 [PubMed] [Google Scholar]
- 113.Isogai S., Horiguchi M. and Weinstein B.M. (2001) The vascular anatomy of the developing zebrafish: an atlas of embryonic and early larval development. Dev. Biol. 230, 278–301 [DOI] [PubMed] [Google Scholar]
- 114.Karlsson J., von Hofsten J. and Olsson P.-E. (2001) Generating transparent zebrafish: a refined method to improve detection of gene expression during embryonic development. Mar. Biotechnol. (N Y) 3, 522–527 [DOI] [PubMed] [Google Scholar]