Abstract
Objectives
To assess knowledge of HPV and attitudes towards HPV vaccination among the general female population, government officials, and healthcare providers in China to assist the development of an effective national HPV vaccination program.
Methods
A cross-sectional epidemiologic survey was conducted across 21 urban and rural sites in China using a short questionnaire. 763 government officials, 760 healthcare providers, and 11,681 women aged 15–59 years were included in the final analysis. Data were analyzed using standard descriptive statistics and logistic regression.
Results
Knowledge of HPV among the general female population was low; only 24% had heard of HPV. Less than 20% of healthcare providers recognized sexually naive women as the most appropriate population for HPV vaccination. There was high acceptance of the HPV vaccine for all categories of respondents. Only 6% of women were willing to pay more than US $300 for the vaccine.
Conclusions
Aggressive education is necessary to increase knowledge of HPV and its vaccine. Further proof of vaccine safety and efficacy and government subsidies combined with increased awareness could facilitate development and implementation of HPV vaccination in China.
Keywords: Cervical cancer, China, human papillomavirus, HPV vaccine, knowledge
Introduction
Cervical cancer is the second most common cancer among women worldwide, with an estimated 529,000 new cases and 275,000 deaths occurring every year (Ferlay et al., 2010). Over 85% of the cases occur in developing countries like China, where it accounts for 13% of female cancers (Ferlay et al., 2010). In China, wide disparities in cervical cancer incidence and mortality are mainly attributable to irregular education and economic development across the country, as well as a lack of a nationwide cervical cancer screening program (Shi et al., 2008; Zhang et al., 2010). Seventy percent of squamous cervical cancers worldwide are caused by human papillomavirus (HPV) strains 16 and 18 (Muñoz et al., 2003; Walboomers et al., 1999), and in China the percent is significantly higher at 84.5% (Chen et al., 2009). The recent development of two prophylactic vaccines against these strains, Gardasil®, Merck & Co Inc., and Cervarix®, GlaxoSmithKline Biologicals, holds the potential to drastically reduce the world burden of cervical cancer, and could have particular impact in China (Koutsky et al., 2002; Villa et al., 2005).
Both vaccines have been approved in more than 100 countries around the world, and Chinese government approval will likely be forthcoming after the completion of ongoing clinical trials. The HPV vaccines have potential for higher-than-average impact in China since cervical cancer mortality among young urban females has been recently increasing by 4.1% per year (Yang et al., 2003; Zhao et al., 2010). In order to develop an effective vaccination program, it is crucial to understand the population’s knowledge of HPV and attitudes towards HPV vaccination, as they will ultimately make the decision for or against vaccination for themselves and their children. It is essential to examine socioeconomic and demographic factors, since some such as education and familiarity with the healthcare system, are more associated with HPV knowledge and vaccine receptivity than others (Brewer and Fazekas, 2007).
There has been only one study on this topic to date in mainland China, which reported that 15% of women in the general population had previously heard of HPV and that nearly 85% were willing to be vaccinated, but these statistics varied with education and region (urban versus rural) (Li et al., 2009). However, this study did not solicit information from healthcare providers or government officials, whose knowledge and attitudes are equally as important to understand, as they will be instrumental in vaccination program development and implementation. The only other Chinese studies in this area were conducted in Hong Kong (Lee et al., 2007; Kwan et al., 2008; Kwan et al., 2009), where differing societal and economic factors make the findings less applicable to mainland China. In this article, we report the results of a multi-center survey assessing knowledge of HPV and attitudes towards HPV vaccination among Chinese government officials and medical personnel as well as women from the general population in order to facilitate the development of a Chinese HPV vaccination strategy.
Materials and Methods
Study population and sampling method
This multi-center, cross-sectional, epidemiologic study included three categories of respondents drawn from multiple urban and rural regions of China: women from the general population, government officials, providers. For the general population category, the large national census and unbalanced economic development necessitated four-stage sampling to obtain a representative study population from seven different geographic regions of China, each of which was stratifiedinto rural or urban based on economic development and population density. One urban site was selected from each geographic region from the 23 provincial general and women and children’s hospitals that had participated in a previous cervical cancer study through the National Cervical Cancer Consortium of China. Two rural sites were selected from each geographic region from the 43 county hospitals enrolled in a national rural cervical cancer screening project supported by the Ministries of Finance and Health (MOF/H). In total, this study included seven urban and fourteen rural sites. In urban areas, subjects were selected by systematic sampling using a pre-assigned sampling interval from outpatients, inpatients, and their female relatives who were physically present at a study hospital on the day of the study. In rural areas, subjects aged 30–59 years were systematically selected from the MOF/H registry in each of the 14 counties using a pre-assigned sampling interval. Subjects aged 15–29 years were selected from the same counties as their older counterparts using cluster sampling; villages within each county were randomly selected, and then every woman between the ages of 15 and 29 years in the village was asked to participate in the study. Surveys were discontinued in each age group when the target sample size was reached. The ratio of urban to rural women and the proportion of subjects per age group approximated the Chinese female population aged 15–59 years in the year 2000 (Ministry of Health, 2007), which had an urban: rural ratio of 2:3 with 12.5% aged 15–19 years, 11.6% aged 20–24 years, 14.3% aged 25–29 years, 15.4% aged 30–34 years, 13.2% aged 35–39 years, 9.7% aged 40–44 years, 10.3% aged 45–49 years, 7.6% aged 50–54 years and 5.5% aged 55–59 years.
Government officials were stratified into two groups, those working in Culture, Education, and/or Health, and those working in Agriculture, Industry, Transportation, or other departments and were drawn from the same urban and rural areas selected for the general population. In rural areas, officials were stratifed by level of government (county, commune, or village) and selected by cluster sampling, while in urban areas, convenience sampling was used due to the large number of government officials from which to select. All government officials were selected from officials who were either hospital inpatients, outpatients, or visiting another patient in the hospital. Healthcare providers were also drawn from the same urban and rural areas as the women from the general population and government officials and stratified sampling was used to select participants for the study. In urban areas, subjects were stratifiedby profession: gynecologists/obstetricians, pediatricians, and others, and then randomly selected. In rural areas, most doctors were general practitioners, so they were stratifiedby the level of their home community (county, commune, or village) and randomly selected.
Informed Consent
Before enrollment, all participants were given and information about the objectives of the study, benefits and risks associated with participation, and assurance of the confidentiality of the information provided. All participants were given the opportunity to ask questions and receive answers. All participants signed an informed consent form and the study was approved by the Institutional Review Board of the Cancer Institute, Chinese Academy of Medical Sciences (CICAMS).
Data Collection
Local interviewers were trained to orally administer a questionnaire to survey demographic characteristics and knowledge and attitudes about HPV and the HPV vaccine. All women from the general population were interviewed by a trained interviewer in a private area to avoid interruptions, and the survey information was recorded anonymously to encourage openness and honesty. The questionnaire used has been validated in several previous studies in China (Rong et al., 2002; Li et al., 2009). Questions were originally written in Mandarin Chinese in simple and clear language and knowledge of HPV and cervical cancer was assessed before further questions were asked on these topics. Many questions were multiple choice, and respondents could pick one or multiple answers. The survey for the general population also assessed sexual debut age and sexual behaviors, data from which are being published elsewhere (Zhao et al., 2012). The questionnaires for government officials and healthcare providers used many of the same questions as the general population survey but also included some questions specific to their profession, such as asking about the cervical screening techniques they recommended to patients or what venue they considered best for a future vaccination program. Some government officials and healthcare providers received the questionnaire to complete themselves, while others were interviewed by trained interviewers. All completed questionnaires underwent regular quality control to check for missing or invalid responses. If data were found missing, the respondant was asked to answer the missing questions again when the respondant had not left the survey place, otherwise, the respondant could not be included in the analysis when the relative question was analyzed.
Data Management and Analysis
Two local staff members separately entered survey information into an electronic database that was periodically sent to the data manager at CICAMS in Beijing. The data were double-checked so that both sets of data agreed. Contingency tables using Pearson Chi-squared or Fisher’s exact tests and tests of trend were used to establish crude associations of socio-demographic and behavior measures. There were five interview questions in all three surveys which directly measured knowledge of HPV and cervical cancer, and eight correct answers (two questions had multiple correct answers). A “knowledge score” on a scale from 1 to 8 was assigned to each respondent corresponding with the number of correct answers they selected. Analyses stratified by the three surveyed population categories and geographic region were used to identify independent determinants of HPV knowledge, with the knowledge score dichotomized at the halfway mark, with higher knowledge considered as 4 or more points on the knowledge scale. Multivariable logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) adjusted for relevant parameters as identifiedby preliminary analysis, which included demographic variables, genital infection history, knowledge to vaccines, anxiety on cervical cancer, acceptance of the vaccine for her daughter or herself and so on. Age was analyzed using ordinal regression analysis. Some data were analyzed using only descriptive statistics and were stratified by population and geographic region. Statisticians at CICAMS analyzed the data using the Statistical Package for the Social Sciences (SPSS) version 13.0 (SPSS, Chicago, IL).
Results
This study was carried out from May to December 2009 with a total of 13,375 people surveyed. For the general female population, 11,852 women were interviewed from seven urban and 14 rural areas of China and 171 ineligible cases were excluded (four were less than 15 years old, and 167 lived outside the selected study sites), for a total of 11,681 women (98.6%) aged 15 to 59 years in the final analysis. 763 government officials and 760 healthcare providers were also interviewed for this study from across the country. Characteristics of the study population are shown in Table 1. The vast majority of those surveyed were Han Chinese.
Table 1.
Sociodemographic Information of Survey Participant
| Characteristics | Urban | Rural | Total | Statistics, P |
|---|---|---|---|---|
| General Female Population, number | 4,761 | 6,920 | 11,681 | |
| Age (years, mean ± SD) | 33.9±11.6 | 34.0±11.9 | 34.0±11.8 | t=−0.59, P=0.559 |
| Marital status (number, %) | ||||
| Married | 3,317 (69.7) | 5,403 (78.1) | 8,720 (74.7) | χ2=105.0, P<0.0001 |
| Unmarried/Divorced/Widowed/Other | 1,444 (30.3) | 1,517 (21.9) | 2,961 (25.3) | |
| Level of education (number, %) | ||||
| Primary School and Below | 159 (3.3) | 2,353 (34.0) | 2,512 (21.5) | χ2=0.465E+4, P<0.0001 |
| Middle School | 645(13.5) | 2,814 (40.7) | 3,459 (29.6) | |
| High School | 1,555 (32.7) | 1,439 (20.8) | 2,994 (25.6) | |
| College and above | 2,402 (50.5) | 314 (4.5) | 2,716 (23.3) | |
| Occupation (number, %) | ||||
| Students | 773 (16.2) | 959 (13.9) | 1,732 (14.8) | χ2=0.432E+4, P<0.0001 |
| Farmers | 155 (3.3) | 3,987 (57.6) | 4,142 (35.5) | |
| Government/medical/clerks | 1,328 (27.9) | 172 (2.5) | 1,500 (12.8) | |
| Workers/operators/service industry | 1,262 (26.5) | 862 (12.5) | 2,124 (18.2) | |
| Unemployed/Free-lance/Others | 1,243 (26.1) | 940 (13.6) | 2,183 (18.7) | |
| Healthcare Providers, number | 354 | 406 | 760 | |
| Gender (number, %) | ||||
| Female | 273 (72.2) | 276 (68.0) | 549 (72.2) | χ2=7.87, P=0.005 |
| Male | 81 (27.8) | 130 (32.0) | 211 (27.8) | |
| Level of education (number, %) | ||||
| High school or below | 10 (2.8) | 190 (46.8) | 200 (26.3) | χ2=188.6, P<0.0001 |
| College and above | 344 (97.2) | 216 (53.2) | 560 (73.7) | |
| Specialty (number, %) | ||||
| Obstetrics/gynecology | 159 (44.9) | 119 (29.4) | 278 (36.6) | χ2=19.6, P<0.0001 |
| Other | 195 (55.1) | 286 (70.6) | 481 (63.4) | |
| Position (number, %) | ||||
| Chief/associate chief doctor | 93 (26.3) | 33 (8.1) | 126 (16.6) | χ2=46.8, P<0.0001 |
| Attending doctor | 71 (20.1) | 120 (29.6) | 191 (25.1) | |
| Resident/Intern/other | 190 (53.6) | 253 (62.3) | 443 (58.3) | |
| a Unit level (number, %) | ||||
| 1st | 245 (69.2) | 146 (36.0) | ------------- | ------------- |
| 2nd | 83 (23.5) | 166 (40.9) | ------------- | ------------- |
| 3rd | 26 (7.3) | 94 (23.2) | ------------- | ------------- |
| Government Officials, number | 352 | 411 | 763 | |
| Gender (number, %) | ||||
| Female | 249 (70.7) | 289 (70.3) | 538 (70.5) | χ2=0.163E-1, P=0.899 |
| Male | 103 (29.3) | 122 (29.7) | 225 (29.5) | |
| Level of education (number, %) | ||||
| High school or below | 41 (11.7) | 128 (31.1) | 169 (22.1) | χ2=41.8, P<0.0001 |
| College and above | 311 (88.4) | 283 (68.9) | 594 (77.9) | |
| Department | ||||
| Culture, education, and health | 172 (48.9) | 222 (54.0) | 394 (51.6) | χ2=2.01, P=0.156 |
| Other | 180 (51.1) | 189 (46.0) | 369 (48.4) | |
| a Unit level (number, %) | ||||
| 1st | 72 (20.5) | 242 (58.9) | ------------- | ------------- |
| 2nd | 121 (34.4) | 132 (32.1) | ------------- | ------------- |
| 3rd | 159 (45.2) | 37 (9.0) | ------------- | ------------- |
Unit levels : for Urban areas : 1st – Province, 2nd – City, 3rd – District ; for Rural areas : 1st – County, 2nd – Commune, 3rd – Village
HPV Knowledge
Only 3% of the general female population correctly answered all five knowledge questions for 8 points, while the majority of women scored 2 out of 8 points. Thirty-four percent of urban women and 16% of rural women had previously heard of HPV, and numbers were similar for having heard of the HPV vaccine. Almost 91% of urban and 84% of rural women had heard of cervical cancer. Table 2 shows a multivariate logistic regression analysis of sociodemographic variables and their association with HPV knowledge and vaccine acceptance. Compared to women with less education, women with at least a senior high education were significantly more likely to have an HPV knowledge score of 4 or higher (OR: 1.84, 95% CI: 1.63–2.08). The age of the women was subjected to an ordinal regression analysis, and each successively older age group was found to have a statistically significant higher likelihood of having higher HPV knowledge than the next younger age group (OR: 1.12, 95% CI:1.1–1.2).
Table 2.
Factors Affecting HPV Knowledge and Willingness for HPV Vaccination among the General Female Population
| HPV knowledge score ≥ 4, N (%) | HPV knowledge score < 4, N (%) | OR* (95% CI) | Willing to be vaccinated, N (%) | Not willing to be vaccinated, N (%) | OR* (95% CI) | |
|---|---|---|---|---|---|---|
| aAge | 2686 (23.0) | 8995 (77.0) | 1.12 (1.07–1.18) | 9019 (77.2) | 2662 (22.8) | 0.88 (0.84–0.93) |
| Marriage status | ||||||
| Not married | 774 (26.1) | 2187 (73.9) | 1 | 2190 (74.0) | 771 (26.0) | 1 |
| Married | 1912 (21.9) | 6808 (78.1) | 0.75 (0.63–0.91) | 6829 (78.3) | 1891 (21.7) | 1.21 (1.00–1.46) |
| Education | ||||||
| < Junior high school | 785 (13.1) | 5186 (86.9) | 1 | 4561 (76.4) | 1410 (23.6) | 1 |
| ≥ Senior high school | 1901 (33.3) | 3809 (66.7) | 1.84 (1.63–2.08) | 4458 (78.1) | 1252 (21.9) | 0.94 (0.83–1.06) |
| Occupation | ||||||
| Unemployed | 633 (29.0) | 1550 (71.0) | 1 | 1688 (77.3) | 495 (22.7) | 1 |
| Government/medical/clerking | 625 (41.7) | 875 (58.3) | 1.19 (1.02–1.38) | 1209 (80.6) | 291 (19.4) | 0.98 (0.82–1.17) |
| Farmers | 436 (10.5) | 3706 (89.5) | 0.51 (0.43–0.60) | 3168 (76.5) | 974 (23.5) | 1.27 (1.10–1.48) |
| Total family income | ||||||
| < 30,000 RMB/year | 1620 (19.8) | 6544 (80.2) | 1 | 4269 (74.5) | 1463 (25.5) | 1 |
| ≥ 30,000 RMB/year | 1066 (30.3) | 2451 (69.7) | 1.30 (1.16–1.45) | 4750 (79.8) | 1199 (20.2) | 1.30 (1.17–1.45) |
| Gynecological exam frequency | ||||||
| Infrequent (< annually) | 1620 (19.8) | 6544 (80.2) | 1 | 6161 (75.5) | 2003 (24.5) | 1 |
| Annually | 1066 (30.3) | 2451 (69.7) | 1.47 (1.33–1.63) | 2858 (81.3) | 659 (18.7) | 1.12 (1.01–1.25) |
| Genital infection history | ||||||
| No history | 1543 (20.1) | 6150 (79.9) | 1 | 5723 (74.4) | 1970 (25.6) | 1 |
| Positive history | 1143 (28.7) | 2845 (71.3) | 1.47 (1.32–1.63) | 3296 (82.6) | 692 (17.4) | 1.35 (1.21–1.50) |
| NIP vaccine knowledge | ||||||
| None | 120 (10.0) | 1082 (90.0) | 1 | 873 (72.6) | 329 (27.4) | 1 |
| Yes but not vaccinated | 719 (18.2) | 3233 (81.8) | 1.50 (1.19–1.90) | 2972 (75.2) | 980 (24.8) | 1.01 (0.86–1.20) |
| Yes and vaccinated | 1847 (28.3) | 4680 (71.7) | 1.54 (1.22–1.93) | 5174 (79.3) | 1353 (20.7) | 1.22 (1.03–1.45) |
| Non-NIP vaccine knowledge | ||||||
| None | 172 (8.9) | 1762 (91.1) | 1 | 1401 (72.4) | 533 (27.6) | 1 |
| Yes but not vaccinated | 1647 (23.0) | 5508 (77.0) | 1.64 (1.36–1.98) | 5503 (76.9) | 1652 (23.1) | 1.07 (0.93–1.23) |
| Yes and vaccinated | 867 (33.4) | 1725 (66.6) | 2.32 (1.89–2.85) | 2115 (81.6) | 477 (18.4) | 1.31 (1.11–1.56) |
| Cervical cancer anxiety | ||||||
| No | 609 (18.0) | 2770 (82.0) | 1 | 2204 (65.2) | 1175 (34.8) | 1 |
| Yes | 2077 (25.0) | 6225 (75.0) | 1.45 (1.30–1.62) | 6815 (82.1) | 1487 (17.9) | 2.23 (2.02–2.45) |
| HPV vaccine acceptance for herself | ||||||
| No | 318 (11.9) | 2344 (88.1) | 1 | ------------- | ------------- | ------------- |
| Yes | 2368 (26.3) | 6651 (73.7) | 2.26 (1.94–2.63) | ------------- | ------------- | ------------- |
| HPV knowledge score | ||||||
| <4 points on 1–8 scale | ------------- | -------------------------- | 6651 (73.9) | 2344 (26.1) | 1 | |
| ≥4 points on 1–8 scale | ------------- | -------------------------- | 2368 (88.2) | 318 (11.8) | 2.31 (2.02–2.64) | |
OR, Odds Ratio; CI, Confidence Interval;
Age of participants was subjected to an ordinal regression analysis with the following age groups: 15–19 years, 20–29 years, 30–39 years, 40–49 years, and 50–59 years;
Variables in Table 2, besides sexual active status, were included in the multivariate logistic regression analyses. The acceptance of the vaccine for a daughter was also included in the model of HPV knowledge. Sexual active status and the acceptance of the vaccine for a daughter were not statistically significant
Among government officials, 7% scored the maximum 8 points on the HPV knowledge scale, and the majority scored 2 out of 8 points. Approximately 44% of all officials had heard of HPV before the survey, 95% had heard of cervical cancer, and 33% had heard of the HPV vaccine. Healthcare providers scored the highest on the HPV knowledge scale, with at least 20% of both urban and rural practitioners scoring the maximum 8 points. The majority of urban providers scored 7 out of 8 points, and the majority of rural providers scored 6 out of 8 points. 96% and 80% of urban and rural providers, respectively, had heard of HPV, 95% and 89% associated it with cervical cancer, and 68% and 58% had heard of the vaccine. Gender, geographic level of the hospital, and experience level were not associated with their HPV knowledge level. The survey for healthcare providers also included several additional questions concerning high risk HPV types; over 68% of all providers were aware of the difference between high and low risk HPV. Tables 3 and 4 show the multivariate logistic regression for government officials and healthcare providers, respectively.
Table 3.
Factors Affecting HPV Knowledge and Willingness for HPV Vaccination among Government Officials
| HPV knowledge score ≥4, N (%) | HPV knowledge score < 4, N (%) | OR* (95% CI) | Willing to be vaccinated, N (%) | Not willing to be vaccinated, N (%) | OR* (95% CI) | |
|---|---|---|---|---|---|---|
| Age | ||||||
| < 35 years | 123 (42.1) | 169 (57.9) | 1 | 249 (85.3) | 43 (14.7) | 1 |
| ≥35 years | 188 (39.9) | 283 (60.1) | 1.07 (0.77–1.49) | 403 (85.6) | 68 (14.4) | 1.08 (0.69–1.70) |
| Gender | ||||||
| Male | 74 (32.9) | 151 (67.1) | 1 | 184 (81.8) | 41 (18.2) | 1 |
| Female | 237 (44.1) | 301 (55.9) | 1.47 (1.03–2.10) | 468 (87.0) | 70 (13.0) | 1.23 (0.78–1.95) |
| Education | ||||||
| ≤ Senior high school | 59 (34.9) | 110 (65.1) | 1 | 145 (85.8) | 24 (14.2) | 1 |
| ≥ College | 252 (42.4) | 342 (57.6) | 1.48 (0.98–2.25) | 507 (85.4) | 87 (14.6) | 0.97 (0.56–1.70) |
| Department | ||||||
| Other | 223 (37.2) | 376 (62.8) | 1 | 517 (86.3) | 82 (13.7) | 1 |
| Health | 88 (53.7) | 76 (46.3) | 2.12 (1.43–3.14) | 135 (82.3) | 29 (17.7) | 0.55 (0.32–0.92) |
| Type of government | ||||||
| Others | 100 (38.9) | 157 (61.1) | 1 | 222 (86.4) | 35 (13.6) | 1 |
| Communist party officials | 44 (39.3) | 68 (60.7) | 1.10 (0.67–1.82) | 95 (84.8) | 17 (15.2) | 0.96 (0.49–1.89) |
| Executive officials | 167 (42.4) | 227 (57.6) | 1.07 (0.74–1.53) | 335 (85.0) | 59 (15.0) | 0.82 (0.50–1.34) |
| Unit level | ||||||
| Commune/village | 86 (48.0) | 93 (52.0) | 1 | 161 (89.9) | 18 (10.1) | 1 |
| County | 148 (38.6) | 235 (61.4) | 0.52 (0.34–0.79) | 328 (85.6) | 55 (14.4) | 0.63 (0.34–1.19) |
| City | 46 (35.7) | 83 (64.3) | 0.58 (0.34–0.99) | 104 (80.6) | 25 (19.4) | 0.44 (0.21–0.92) |
| Central/provincial | 31 (43.1) | 41 (56.9) | 0.68 (0.37–1.27) | 59 (81.9) | 13 (18.1) | 0.49 (0.21–1.14) |
| NIP vaccine knowledge | ||||||
| None | 9 (31.0) | 20 (69.0) | 1 | 25 (86.2) | 4 (13.8) | 1 |
| Yes but not vaccinated | 74 (33.6) | 146 (66.4) | 1.22 (0.46–3.19) | 177 (80.5) | 43 (19.5) | 0.64 (0.18–2.28) |
| Yes and vaccinated | 228 (44.4) | 286 (55.6) | 1.53 (0.59–3.98) | 450 (87.5) | 64 (12.5) | 0.95 (0.27–3.36) |
| Non-NIP vaccine knowledge | ||||||
| None | 12 (25.5) | 35 (74.5) | 1 | 41 (87.2) | 6 (12.8) | 1 |
| Yes but not vaccinated | 160 (35.2) | 295 (64.8) | 1.32 (0.60–2.89) | 375 (82.4) | 80 (17.6) | 0.67 (0.24–1.81) |
| Yes and vaccinated | 139 (53.3) | 122 (46.7) | 2.30 (1.02–5.19) | 236 (90.4) | 25 (9.6) | 1.14 (0.39–3.35) |
| Cervical cancer anxiety | ||||||
| No | 50 (26.0) | 142 (74.0) | 1 | 139 (72.4) | 53 (27.6) | 1 |
| Yes | 261 (45.7) | 310 (54.3) | 1.91 (1.29–2.82) | 513 (89.8) | 58 (10.2) | 2.96 (1.90–4.60) |
| HPV vaccine acceptance for daughter | ||||||
| No | 34 (21.0) | 128 (79.0) | 1 | ------------- | -------------------------- | |
| Yes | 277 (46.1) | 324 (53.9) | 2.70 (1.69–4.32) | ------------- | -------------------------- | |
| HPV knowledge score | ||||||
| <4 points on 1–8 scale | ------------- | -------------------------- | 369 (81.6) | 83 (18.4) | 1 | |
| ≥4 points on 1–8 scale | ------------- | -------------------------- | 283 (91.0) | 28 (9.0) | 1.76 (1.08–2.89) | |
OR, Odds Ratio; CI, Confidence Interval;
Variables in Table 3 were included in the multivariate logistic regression analyses. The acceptance of the vaccine for government officials was also included in the model of HPV knowledge, but was not statistically significant
Table 4.
Factors Affecting HPV Knowledge and Willingness for HPV Vaccination among Healthcare Providers
| HPV knowledge score ≥4, N (%) | HPV knowledge score < 4, N (%) | OR* (95% CI) | Willing to be vaccinated, N | Not willing to be (%) vaccinated, N (%) | OR* (95% CI) | |
|---|---|---|---|---|---|---|
| Age | ||||||
| < 35 years | 337 (88.5) | 44 (11.5) | 1 | 318 (83.5) | 63 (16.5) | 1 |
| ≥35 years | 322 (85.0) | 57 (15.0) | 0.90 (0.53–1.52) | 304 (80.2) | 75 (19.8) | 1.31 (0.79–2.16) |
| Gender | ||||||
| Male | 174 (82.5) | 37 (17.5) | 1 | 171 (81.0) | 40 (19.0) | 1 |
| Female | 485 (88.3) | 64 (11.7) | 1.02 (0.54–1.95) | 451 (82.1) | 98 (17.9) | 0.44 (0.26–0.76) |
| Education | ||||||
| ≤ Senior high school | 145 (72.5) | 55 (27.5) | 1 | 161 (80.5) | 39 (19.5) | 1 |
| College | 368 (90.4) | 39 (9.6) | 2.98 (1.67–5.31) | 339 (83.3) | 68 (16.7) | 1.67 (0.89–3.12) |
| ≥ Graduate study | 146 (95.4) | 7 (4.6) | 3.50 (1.17–10.4) | 122 (79.7) | 31 (20.3) | 1.44 (0.62–3.36) |
| Department | ||||||
| Other | 387 (80.5) | 94 (19.5) | 1 | 385 (80.0) | 96 (20.0) | 1 |
| Obstetrics/gynecology | 271 (97.5) | 7 (2.5) | 7.78 (3.39–17.8) | 236 (84.9) | 42 (15.1) | 1.32 (0.82–2.12) |
| Experience | ||||||
| Junior doctors | 544 (85.8) | 90 (14.2) | 1 | 537 (84.7) | 97 (15.3) | 1 |
| Professors | 115 (91.3) | 11 (8.7) | 1.65 (0.70–3.90) | 85 (67.5) | 41 (32.5) | 0.36 (0.19–0.66) |
| Unit level | ||||||
| County/village/other | 210 (79.5) | 54 (20.5) | 1 | 230 (87.1) | 34 (12.9) | 1 |
| District | 139 (84.2) | 26 (15.8) | 0.84 (0.45–1.57) | 128 (77.6) | 37 (22.4) | 0.42 (0.23–0.79) |
| City | 77 (88.5) | 10 (11.5) | 0.88 (0.34–2.25) | 66 (75.9) | 21 (24.1) | 0.33 (0.14–0.76) |
| Central/provincial | 233 (95.5) | 11 (4.5) | 2.04 (0.84–4.96) | 198 (81.1) | 46 (18.9) | 0.41 (0.20–0.85) |
| NIP vaccine knowledge | ||||||
| None | 9 (100.0) | 0 (0.0) | ------------- | 8 (88.9) | 1 (11.1) | 1 |
| Yes but not vaccinated | 89 (75.4) | 29 (24.6) | ------------- | 73 (61.9) | 45 (38.1) | 0.28 (0.03–2.68) |
| Yes and vaccinated | 561 (88.6) | 72 (11.4) | ------------- | 541 (85.5) | 92 (14.5) | 0.87 (0.09–8.45) |
| Non-NIP vaccine knowledge | ||||||
| None | 23 (79.3) | 6 (20.7) | 1 | 15 (51.7) | 14 (48.3) | 1 |
| Yes but not vaccinated | 357 (85.8) | 59 (14.2) | 0.52 (0.17–1.62) | 336 (80.8) | 80 (19.2) | 2.67 (1.09–6.51) |
| Yes and vaccinated | 279 (88.6) | 36 (11.4) | 0.85 (0.26–2.76) | 271 (86.0) | 44 (14.0) | 3.60 (1.41–9.19) |
| Cervical cancer anxiety | ||||||
| No | 305 (85.9) | 50 (14.1) | 1 | 268 (75.5) | 87 (24.5) | 1 |
| Yes | 353 (87.4) | 51 (12.6) | 0.88 (0.47–1.63) | 353 (87.4) | 51 (12.6) | 3.34 (2.07–5.37) |
| HPV vaccine acceptance for herself | ||||||
| No | 104 (75.4) | 34 (24.6) | 1 | ------------- | ------------- | ------------- |
| Yes | 555 (89.2) | 67 (10.8) | 2.85 (1.48–5.48) | ------------- | ------------- | ------------- |
| HPV knowledge score | ||||||
| <4 points on 1–8 scale | ------------- | ------------- | ------------- | 67 (66.3) | 34 (33.7) | 1 |
| ≥ 4 points on 1–8 scale | ------------- | ------------- | ------------- | 555 (84.2) | 104 (15.8) | 2.86 (1.63–5.01) |
OR, Odds Ratio; CI, Confidence Interval;
Variables in Table 4 were included in the multivariate logistic regression analyses. The acceptance of the vaccine for a daughter was also included in the model of HPV knowledge, but was not statistically significant
Receptivity to the HPV Vaccince
The majority of those surveyed in all categories were willing to be vaccinated for HPV (77% of the general female population, 85% of government officials, and 82% of medical personnel), and the proportions were essentially equal in urban and rural areas. A similarly high porportion of all categories were willing for their daughter to be vaccinated (78% of the general female population, 79% of government officials, and 74% of healthcare providers). Multivariate logistic regression analysis showed that similar factors were associated with willingness to accept the vaccine as were associated with HPV knowledge, with several exceptions (Table 2, 3, 4). An ordinal regression analysis on age showed that as women from the general population increased in age, they became less likely to accept HPV vaccination (OR: 0.88, 95% CI: 0.84–0.93). Government officials with knowledge scores of 4 or above were significantly more likely to accept HPV vaccination for themselves than those with lower knowledge scores (OR: 1.76, 95% CI: 1.08–2.89). Among healthcare providers, associate professors and full professors were less likely to consent to vaccination than providers further down the career ladder (OR: 0.36, 95% CI: 0.19–0.66).
Table 5 presents reasons cited by respondents for and against vaccination. In both urban and rural areas, health benefits and fear of suffering from cervical cancer were cited as the top reasons for getting the vaccine among the general population. Rationales against HPV vaccination varied by geographic area and type of respondent. The majority of both urban and rural medical and government personnel were worried about the safety of the vaccine. Approximately 89% of all medical personnel would have recommended the HPV vaccine to their patients, and more than 70% of all healthcare providers thought the vaccine should be available in China. 76% of government officials thought the HPV vaccine should be included in the National Immunization Program.
Table 5.
Reasons for and against HPV vaccination
| General Female Population
|
Healthcare Providers
|
Government Officials
|
||||
|---|---|---|---|---|---|---|
| Urban | Rural | Urban | Rural | Urban | Rural | |
| Reasons for willingness to be vaccinated, multiple answers allowed (number, %) | ||||||
| N=3,661 | N=5,358 | N=284 | N=338 | N=280 | N=372 | |
| Self-benefit | 2,678 (73.1) | 4,165 (77.7) | 235 (82.7) | 273 (80.8) | 213 (76.1) | 283 (76.1) |
| Benefit to other youth | 542 (14.8) | 912 (17.0) | 24 (8.5) | 67 (19.8) | 55 (19.6) | 100 (26.9) |
| Fear of cervical cancer | 1,992 (54.4) | 3,503 (65.4) | 171 (60.2) | 228 (67.5) | 163 (58.2) | 247 (66.4) |
| Fear of genital warts | 483 (13.2) | 944 (17.6) | 69 (24.3) | 111 (32.8) | 48 (17.1) | 93 (25.0) |
| Fear of HPV infection | 1,383 (37.8) | 1,590 (29.7) | 142 (50.0) | 173 (51.2) | 120 (42.9) | 163 (43.8) |
| Fear of having been infected with HPV | 272 (7.4) | 290 (5.4) | 31 (10.9) | 59 (17.5) | 33 (11.8) | 35 (9.4) |
|
| ||||||
| Reasons against willingness to be vaccinated, multiple answers allowed (number, %) | ||||||
| N=1,100 | N=1,561 | N=70 | N=68 | N=72 | N=39 | |
| Belief in low self-risk | 302 (27.5) | 598 (38.3) | 23 (32.9) | 14 (20.6) | 17 (23.6) | 14 (35.9) |
| Limited usage to date | 434 (39.5) | 353 (22.6) | 31 (44.3) | 32 (47.1) | 21 (29.2) | 14 (35.9) |
| Belief that vaccination is risky | 563 (51.2) | 489 (31.3) | 49 (70.0) | 42 (61.8) | 52 (72.2) | 26 (66.7) |
| Doubt of vaccine efficacy | 365 (33.2) | 326 (20.9) | 39 (55.7) | 37 (54.4) | 32 (44.4) | 17 (43.6) |
| Doubt of source of vaccine | 164 (14.9) | 160 (10.2) | 12 (17.1) | 10 (14.7) | 14 (19.4) | 3 (7.7) |
| Expense of vaccine | 226 (20.5) | 579 (37.1) | 9 (12.9) | 14 (20.6) | 9 (12.5) | 8 (20.5) |
| Other | 87 (7.9) | 144 (9.2) | 2 ( 2.9) | 2 (2.9) | 0 (0.0) | 0 (0.0) |
Other Factors Important for Vaccine Program Implementation
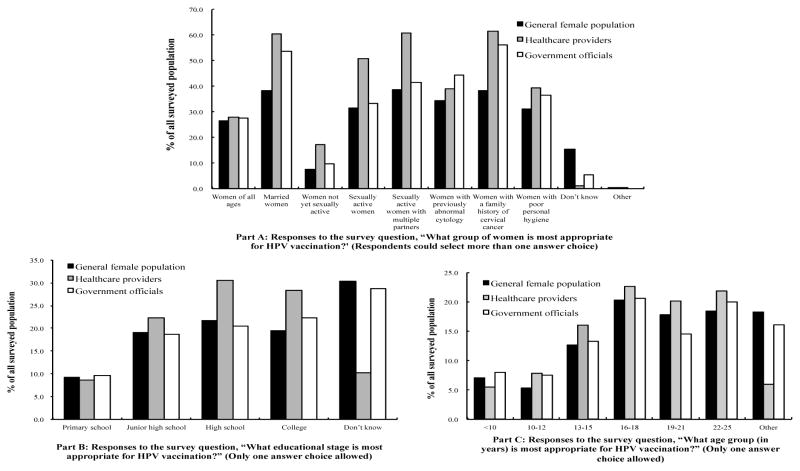
All respondent categories in both urban and rural areas cited Disease Prevention and Control Centers, followed by Maternal and Child Care Hospitals, as the optimal venues for HPV vaccination. Multiple survey questions assessed who respondents felt was the appropriate population for vaccination. Figure 1 shows the answers to several of these questions broken down by respondent type; urban and rural values were similar in all categories and are not shown. Less than 10% of both the general female population and government officials and less than 20% of healthcare providers selected ‘females not yet sexually active’ as an appropriate population for vaccination. When asked about the appropriate age for HPV vaccination, all categories of respondents focused on 16–18 and 22–25 year-old women, with less than 30% of any respondent group selecting females younger than 16 years of age. When directly asked whether before or after sexual debut was the best time for vaccination, the majority of the general population and government officials answered ‘Don’t know’, and 55% of doctors answered ‘before sexual debut’. (data for the latter question not shown).
Figure 1.
Opinions on the Appropriate Population to Receive HPV Vaccination
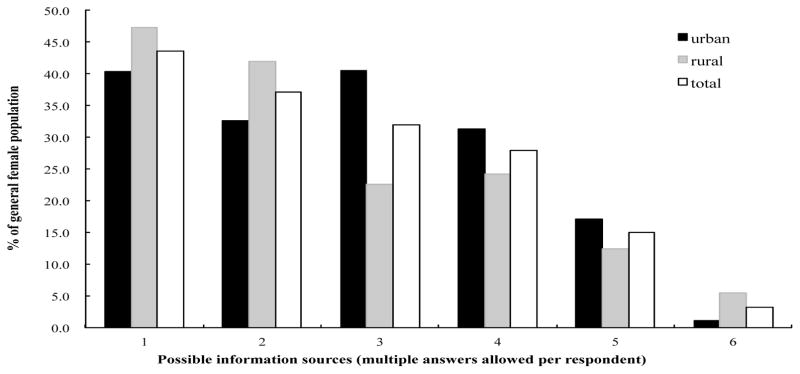
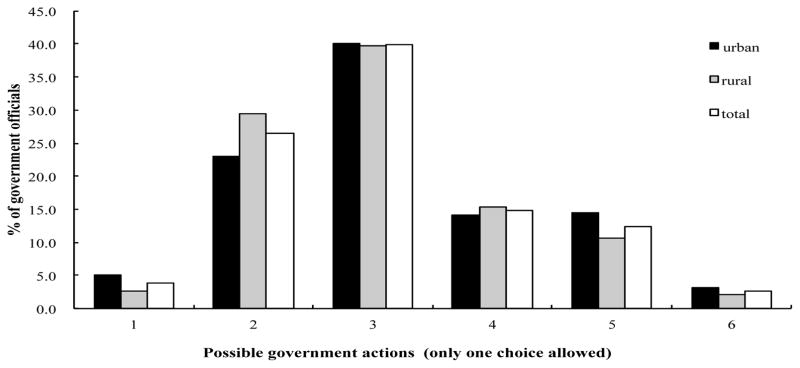
Figure 2 shows the sources of information used by the general population to learn about the HPV vaccine. The most trusted information source for all women was doctors or nurses. In addition, 68% of females surveyed from the general population were willing to pay up to 500 RMB for the HPV vaccine. Very few (6%) were willing to pay more than 2000 RMB (~$300 USD) for an imported HPV vaccine. When asked who should assume financial responsibility for the vaccine, 44% of government officials felt that the government and individuals should share the cost of HPV vaccination. Both doctors and government officials emphasized the importance of educational campaigns when asked to choose the best method for nationwide vaccination. Figure 3 shows government officials’ responses when asked how the government should react to the appearance of HPV vaccine on the market. To government officials, possible barriers to widespread vaccination included lack of understanding by women, cost, and unclear vaccine longterm safety and efficacy.
Figure 2. Responses of the General Female Population to the Survey Question, “What are your sources for HPV vaccine information?”.
1= Doctors or nurses; 2Media (broadcasting/TV/newspaper/magazines/websites); 3=Public lectures in hospitals/schools; 4=Social benefit programs; 5= Family members or friends; 6=Other
Figure 3. Responses of Government Officials to the Question, “What is the appropriate action of the Chinese government when the HPV vaccine appear on the market?”.
1=No direct government intervention; 2=Encouragement plus subsidization; 3=Active education campaigns; 4=Encouragement of vaccination for women in high-risk areas; 5=Wait-and-see due to unclear long-term safety and efficacy; 6=Mandate all eligible women get vaccinated
Discussion
To our knowledge, this is the first study to evaluate HPV knowledge and attitudes towards HPV vaccination among government officials and medical personnel, in addition to women from the general population, in mainland China. Although mainland and Hong Kong Chinese populations are not necessarily comparable, the low levels of HPV knowledge found in our study among the general female population were consistent with the knowledge levels found in the studies from Hong Kong (Lee et al., 2007; Kwan et al., 2008; Kwan et al., 2009), as well as with low knowledge levels noted in a review of 28 vaccine acceptability studies in the U.S. (Brewer and Fazekas, 2007).
Although higher than among the general female population, the relatively low knowledge level of government officials and medical personnel found in our study is troubling. Many surveyed healthcare providers did not recognize that HPV vaccination should occur before sexual debut, after which the risk of infection with HPV increases dramatically (Panatto et al., 2009). The majority of all healthcare providers selected females older than age 16 years as prime targets for vaccination, when in fact a recent study on the sexual debut age in China suggests that girls should be vaccinated for HPV between the ages of 13–15 years, before the conclusion of mandatory schooling (Zhao et al., 2012). Lower knowledge levels among rural healthcare providers compared to urban providers highlights the importance of focusing education efforts for healthcare professionals in less populated areas. Non-obstetrician/gynecologists should also be targets of increased education, as specialists in this field were 8.8 times more likely to have higher knowledge of HPV than other types of providers. In addition, education of government officials should target the higher levels (county and city officials) since they had less HPV knowledge than more local officials but will have more oversight over HPV vaccination programs.
The factors found in logistic regression analysis to be associated with willingness to be vaccinated against HPV or consent for vaccination of their daughters are important to consider. First and foremost, women with higher levels of HPV knowledge were significantly more open to vaccination for both themselves and their daughters than women with knowledge scores under 4 out of 8 on the knowledge scale. This finding reinforces the importance of public education in the success of a HPV vaccination program. In addition, many of the other factors which were associated with openness to HPV vaccination, such as exposure to other vaccines and frequent gynecological exams, all represent contact with the medical system in some way. Further education of providers will likely influence even more women to get the vaccine. It is unclear why professors and associate professors of medicine were significantly less likely to consent to HPV vaccination for their daughters than lower levels of providers; one possible explanation is that professors are more removed from clinical work than residents and attendings, and thus have less exposure to new clinical guildelines than their younger colleagues.
Despite low HPV knowledge levels, the strong approval for HPV vaccination for both themselves and their daughters among the general population is consistent with that recently found in China (Li et al., 2009) as well as in other countries (Brabin et al., 2006; Woodhall et al., 2007). The most common arguments against vaccination in our study included worries about the safety of the vaccine and low perceived personal risk of cervical cancer, attitudes which should both be responsive to education efforts. The HPV vaccine might be best introducted into China through government-sponsored programs to reassure people as to its safety, something also suggested by Li et al. (2009). For rural women, the cost of the vaccine was also a prominent barrier to vaccination, and indeed, the high cost (advertised retail price US $360 for the 3-shot series) bodes ill for its affordability to any Chinese women except the most wealthy. The fact that only 21% of rural women in our study were willing to pay more than RMB 500, or about US $80, for the entire series shows the need for drastic government subsidization of the vaccination program. Although many government officials cited worry about cost as a major concern for the success of HPV vaccination programs, the majority felt that the government should play some role in financing vaccinations, which is a positive indicator for future policies.
Women from the general population indicated high levels of trust in doctors and nurses as well as hospital lectures as their source of information about the HPV vaccine. This dependence on medical professionals and the healthcare delivery system stresses the importance of creating large numbers of healthcare providers in China who are well-informed about the benefits of the vaccine and the appropriate population who should be vaccinated. Doctors who feel more knowledgeable about the HPV vaccine have been shown to be more likely to recommend it to patients (Hopkins et al., 2009), and it seems likely that government officials with more education on the topic of HPV will more strongly support government vaccination campaigns as well (Dempsey and Davis, 2006).
Strengths of this study include that it surveyed a large population from different areas of China and specifically targeted medical and governmental personnel. The majority of the survey questions had been used several times before in China (Rong et al., 2002; Li et al., 2009), and the new questions made it possible to gather unique, invaluable information. Limitations include the cross-sectional nature of the study which did not allow for the determination of causal relationships, and the risk of selection bias because of the voluntary study population. However, this risk was low since a very high proportion of potential respondents agreed to be interviewed. Furthermore, among the professional respondents, some were interviewed orally and some took the survey in written form, raising the question of social desirability bias among those interviewed, but the use of trusted local interviewers decreases the weight of this limitation. The women from the general population were all interviewed in person due to concerns about literacy, and while it is true that HPV brings up sensitive sexual issues which could have interfered with genuine responses, the conduction of the study in a clinical setting and the use of trusted local interviewers likely minimized this complication as well. Doubtless there is also some residual confounding from unmeasured factors in the analysis, but an attempt was made to include all factors shown in previous studies to play a role in HPV knowledge or vaccine acceptability that were applicable to China (Brewer et al., 2007; Li et al., 2009).
In sum, awareness of HPV and its connections to cervical cancer is low among the general female population in China, and lower than expected among government and medical personnel, despite its strong connection with cervical cancer. Potential obstacles to the development of a widespread HPV vaccination program include low knowledge levels, high vaccine cost, and doubts as to the safety and longterm efficacy of the vaccine. However, widespread uptake of HPV vaccination in China is possible with aggressive public education campaigns, targeted education for medical and governmental personnel, further publicized scientific proof of vaccine safety and efficacy, and the development of a reasonable cost-sharing mechanism between the government and vaccine-eligible women. Increased public and professional education about HPV and prevention strategies could also have implications for other sexually transmitted diseases and vaccination campaigns in China.
Acknowledgments
This project was made possible by the efforts of twenty-one collaborative hospitals and by the participation of women, doctors, and government officials from Beijing, Nanjing, Xinjiang, Liaoning, Tianjin, Shanxi, Inner Mongolia, Shandong, Hunan, Henan, Fujian, Guangdong, Jiangxi, Yunnan, Chongqing, and Gansu. This work was partially supported by the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental & Craniofacial Research, National Institute on Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases Health, and NIH Office of Women’s Health and Research through the International Clinical Research Scholars and Fellows Program at Vanderbilt University (R24 TW007988) and the American Relief and Recovery Act.
References
- Brabin L, Roberts SA, Farzaneh F, Kitchener HC. Futureacceptance of adolescent human papillomavirus vaccination: A survey of parental attitudes. Vaccine. 2006;24:3087–94. doi: 10.1016/j.vaccine.2006.01.048. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev Med. 2007;45:107–14. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Chen W, Zhang X, Molijn A, et al. Human papillomavirustype-distribution in cervical cancer in China : the importance of HPV 16 and 18. Cancer Causes Control. 2009;20:1705–13. doi: 10.1007/s10552-009-9422-z. [DOI] [PubMed] [Google Scholar]
- Dempsey AF, Davis MM. Overcoming barriers to adherence to HPV vaccination recommendations. The Am J Manag Care. 2006;12(17 Suppl):S484–91. [PubMed] [Google Scholar]
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- Hopkins TG, Wood NJ, West RM, Darling JC. UK health professionals attitudes and knowledge regarding Human Papillomavirus (HPV) vaccination: a West Yorkshire Study. J Paediatr Child Health. 2009;45:652–5. doi: 10.1111/j.1440-1754.2009.01589.x. [DOI] [PubMed] [Google Scholar]
- Koutsky LA, Ault KA, Wheeler CM, et al. A controlledtrial of a human papillomavirus type 16 vaccine. NEJM. 2002;347:1645–51. doi: 10.1056/NEJMoa020586. [DOI] [PubMed] [Google Scholar]
- Kwan TTC, Chan KKL, Yip AMW, et al. Barriers and facilitators to human papillomavirus vaccination among Chinese adolescent girls in Hong Kong : a qualitative – quantitative study. Sex Transm Infect. 2008;84:227–32. doi: 10.1136/sti.2007.029363. [DOI] [PubMed] [Google Scholar]
- Kwan TTC, Chan KKL, Yip AMW, et al. Acceptability of human papillomavirus vaccination among Chinese women : concerns and implications. BJOG. 2009;116:501–10. doi: 10.1111/j.1471-0528.2008.01988.x. [DOI] [PubMed] [Google Scholar]
- Lee PWH, Kwan TTC, Fai K, et al. Beliefs about cervicalcancer and human papillomavirus (HPV) and acceptability of HPV vaccination among Chinese women in Hong Kong. Prev Med. 2007;45:130–4. doi: 10.1016/j.ypmed.2007.07.013. [DOI] [PubMed] [Google Scholar]
- Li J, Li LK, Ma JF, et al. Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China. Vaccine. 2009;27:1210–5. doi: 10.1016/j.vaccine.2008.12.020. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Ministry of Health (MOH) Chinese Health Statistics Yearbook. Beijing, China: Peking Union Medical Press; 2007. p. 337. [Google Scholar]
- Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. NEJM. 2003;348:518–27. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- Panatto D, Amicizia D, Lugarini J, et al. Sexual behaviour in Ligurian (Northern Italy) adolescents and young people: suggestions for HPV vaccination policies. Vaccine. 2009;27(Suppl 1):A6–10. doi: 10.1016/j.vaccine.2008.10.057. [DOI] [PubMed] [Google Scholar]
- Rong S, Chen W, Wu L, et al. Analysis of risk factorsfor cervical cancer in Xiangyuan County, Shanxi Province. Zhonghua Yu Fang Yi Xue Za Zhi. 2002;36:41–3. [PubMed] [Google Scholar]
- Shi JF, Qiao YL, Smith JS, et al. Epidemiology and prevention of human papillomavirus and cervical cancer in China and Mongolia. Vaccine. 2008;26(Suppl 1):M53–9. doi: 10.1016/j.vaccine.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Villa L, Costa R, Petta C, et al. Prophylactic quadrivalenthuman papillomavirus (types 6, 11, 16, and 18) L1 virus-like particle vaccine in young women: a randomised double-blind placebo-controlled multicentre phase II efficacy trial. Lancet Oncol. 2005;6:271–8. doi: 10.1016/S1470-2045(05)70101-7. [DOI] [PubMed] [Google Scholar]
- Walboomers JMM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–9. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- Woodhall SC, Lehtinen M, Verho T, et al. Anticipatedacceptance of HPV vaccination at the baseline of implementation: a survey of parental and adolescent knowledge and attitudes in Finland. JAH. 2007;40:466–9. doi: 10.1016/j.jadohealth.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Yang L, Parkin DM, Li L, Chen Y. Time trends in cancer mortality in China: 1987–1999. Int J Cancer. 2003;106:771–83. doi: 10.1002/ijc.11300. [DOI] [PubMed] [Google Scholar]
- Zhang YZ, Ma JF, Zhao FH, et al. Three-year follow-up results of visual inspection with acetic acid/Lugol’s iodine (VIA/VILI) used as an alternative screening method for cervical cancer in rural areas. Chin J Cancer. 2010;29:4–8. doi: 10.5732/cjc.009.10687. (in Chinese) [DOI] [PubMed] [Google Scholar]
- Zhao FH, Hu SY, Zhang SW, Chen WQ, Qiao YL. Cervical cancer mortality in 2004 – 2005 and changes during last 30 years in China. Chin J Prev Med. 2010;44:408–12. [PubMed] [Google Scholar]
- Zhao FH, Tiggelaar S, Hu SY, et al. A multi-center survey of age of sexual debut and sexual behavior in Chinese women: suggestions for optimal age of human papillomavirus vaccination in China. Cancer Epidemiol. 2012;36:384–90. doi: 10.1016/j.canep.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]