Abstract
Background:
Female sexual dysfunction (FSD) is a highly prevalent and often underestimated problem. However, large-scale, population-based epidemiological surveys of FSD are scarce in China. The present study was conducted to evaluate the prevalence and the potential risk factors of FSD across a selection of social groups in Beijing, China, based on the Female Sexual Function Index (FSFI).
Methods:
A cross-sectional study based on the multiple-stage cluster sampling was performed with adult women throughout the Dongcheng and Shunyi districts of Beijing. The Chinese version of FSFI was used, as well as questions on demographic characteristics, the disease-related context, and social relationships.
Results:
A total of 6000 consecutive women entered this study, with an actual response from 5024 women, corresponding to a response rate of 83.7%. A total of 4697 (78.3%) questionnaires were effective. The prevalence of adult FSD in Beijing was 2973 (63.3%) using a score of 26.55 as the boundary value, whereas the total mean FSFI score was 23.92 ± 6.37. However, 1423 (30.3%) women did not seek help. By multivariate logistic regression analysis, the possible potential risk factors included age (odds ratio [OR] = 1.051), dissatisfaction with the spouse's sexual ability (OR = 3.520), poor marital affection (OR = 2.087), spouse sexual difficulties (OR = 1.720), dissatisfaction with married life (OR = 1.476), living in a rural area (OR = 1.292), chronic pelvic pain (OR = 1.261), chronic disease (OR = 1.534), previous pelvic surgery (OR = 1.605), vaginal delivery (OR = 2.285), lower education (OR = 3.449) and postmenopausal (OR = 3.183).
Conclusions:
As suggested by the FSFI scores, female sexual problems are highly prevalent in Beijing. Dissatisfaction with the spouse's sexual ability, poor marital affection, sexual difficulties of the spouse, dissatisfaction with the marriage, rural life, CPP, and postmenopausal were conceivable risk factors for FSD in Beijing women.
Keywords: Beijing, Female Sexual Dysfunction, Female Sexual Function Index, Potential Risk Factors, Prevalence
Introduction
Sexuality is the foundation of not only human survival, but also reproduction, and has deep spiritual and cultural connotations. Sexual dysfunction is defined by the World Health Organization as “disturbance in sexual desire and in the psycho-physiological changes that characterize the sexual response cycle and which results in marked distress and interpersonal difficulty”.[1] Female sexual dysfunction (FSD) is a highly prevalent and often underestimated problem.[2] Epidemiological data, derived from surveys based on the current and internationally recognized diagnostic and validated self-administered questionnaire, the Female Sexual Function Index (FSFI),[3,4] have shown that the estimated prevalence of FSD may be 30–63%.[5,6,7] Epidemiological investigations from the United States and Europe have reported FSD prevalence of about 19–50%.[2,3,8] In the Middle East, the prevalence of sexual disorders was 31.5%.[8] In Japan, Hisasue et al.[3] reported that the prevalence of arousal disorder in women aged 30 years was 29.7%. Scientifically, the etiology of sexual dysfunction is frequently multifactorial as it relates to age, social strata, education level, employment, and religion as well as biological, medical, and psychological factors.[3,9] However, because of social customs and culture, patients and their clinicians often avoid discussing this topic. Large-scale, population-based epidemiological surveys of FSD are scarce in China. In addition, most prior studies evaluating sexual function in Chinese women were clinic based, with variations and inconsistency in the way FSD was measured, and did not use validated, condition-specific questionnaires.
The FSFI is a brief, multidimensional scale for assessing FSD. The professional FSFI questionnaire was designed in 2000.[10] Sun et al.[11] translated the FSFI into Chinese and demonstrated that the Chinese version of the FSFI is a reliable and valid questionnaire for assessing FSD in Chinese women. This study selected a well-developed city based on the economy, culture, and education level, with Beijing as the gold standard survey unit, to investigate the current sex life of apparently healthy women and identify the prevalence and factors associated with FSD in Chinese women. The long-term goals of this study included guidance for clients and health-care providers about sexuality and sexual dysfunction, screening for sexual disorders, and initiating dialog with professionals who could help recognize, treat, and eventually decrease the prevalence of sexual disorders and suffering.
Methods
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Review Committee of Peking Union Medical College Hospital, Chinese Academy of Medical Sciences.
All participants provided written informed consent prior to their enrollment in this study; however, a few participants were not willing or able to read the informed consent. Peking Union Medical College considered the informed consent consistent with ethical requests, on July 20, 2011. All the study data were kept confidential.
Study population
From July to December 2011, a population-based cross-sectional study was performed based on the feasibility, economic effectiveness, and representative principles of multiple-stage cluster sampling in Beijing. The respondents were female residents who had lived locally for >5 years. Additional inclusion criteria were that the women had to be aged ≥20 years, conscious and able to understand and participate in the survey, and asexually active during the prior 4-week period. Postpartum respondents who got pregnant <3.5 months were excluded from the study.
The health bureau of Dongcheng and Shunyi districts, which are owned by the Beijing city government, assisted with the study. The health bureau encouraged the women's participation. Every local family received a notice during the household health interview by the community doctors or community workers. The notice indicated the time and place that the questionnaire would be administered. The participants were provided with information on public hygiene and given basic education regarding gynecology and obstetrics on the same day. The health bureaus of the Dongcheng and Shunyi districts organized the administration of the questionnaire. Researchers approached participants in the local community health service center, an office block that provides general information to local residents and communication space for the researchers.
For poorly educated participants, an experienced interviewer explained the study. Verbal informed consent was provided simultaneously to ensure that all participants understood the study. All participants completed the questionnaire voluntarily, anonymously, and independently to ensure the confidentiality of the survey.
The sample content was analyzed according to a simple random sampling, minimum sample formula: N = uα2 × prevalence (1 − prevalence)/δ2. The prevalence was estimated as 40% according to the literature; the evaluated error, δ was 4%; and the minimum sample content was n1= (1.962 × 0.40 × 0.60)/0.042 = 576. A total of 315,000 female residents lived in the Dongcheng district in 2009, with women aged ≥20 years comprising 86% (270,900 women) of this population. We randomly sampled 1.0% of the female residents, a total of 2709 women. Shunyi district had 291,000 female residents aged ≥20 years, and we sampled 2505 women from this district. A total of 5214 participants were included in the survey. The sample size was expanded by 15%, and rounded to 6000; 3000 women from each of the two districts.
Considering the sensitivity of sexual problems, transportation convenience, and the logistics of the investigation, the study randomly sampled two districts of Beijing as the survey unit, including the high-level economic and culturally educated Dongcheng district and the medium-level economic and culturally educated Shunyi district.
Questionnaire
The questionnaire consisted of two parts: a general questionnaire and a professional questionnaire. The general questionnaire was designed on the basis of the potential risk factors for FSD and included detailed personal information such as demographic characteristics (age, education level, occupation, income level, and living environment), menstrual and childbearing history (menstrual status, marital status, active sex life expectancy, birth control, pregnancies, the number of children, and the mode of delivery), disease status (chronic pelvic pain [CPP], urinary incontinence, pelvic organ prolapse, gynecological disease, chronic disease, and surgical history), and social and sexual relationship status (work and life burden, marital affection, satisfaction/dissatisfaction with the marriage, appreciable sexual difficulties of the spouse, satisfaction/dissatisfaction with the spouse's sexual ability, and the method of help).
This study used the FSFI to evaluate the sexual dysfunction of women enrolled in this study. The FSFI is a brief, 19-item questionnaire that assesses self-reported female sexual function during the past 4 weeks and is organized into a 6-domain structure that includes desire (two questions), arousal (four questions), lubrication (four questions), orgasm (three questions), satisfaction (three questions), and pain (three questions). The optimal cutoff score of the FSFI was 26.55, which was confirmed in 2005 to identify FSD.[10]
Statistical analysis
All data were collected, and an EpiData database was established. Data were double entered and strictly checked to eliminate logic errors. All statistical analyses were performed using Statistical Package for Social Sciences, version 13.0 (SPSS Inc., Chicago, IL, USA). Enumeration data were analyzed using the Chi-square test, and the logistic regression multivariate analysis model was well suited for the single- or multi-potential risk factors for FSD such as dysaphrodisia, arousal difficulties, vaginal lubrication problems, orgasmic dysfunction, sexual satisfaction disorders, and dyspareunia. Odds ratios (ORs) and 95% confidence intervals were calculated. All tests were two sided, with a P < 0.05 considered statistically significant.
Results
A total of 6000 consecutive women entered this study, with an actual response from 5024 women, corresponding to a response rate of 83.7%. A total of 4697 (78.3%) questionnaires were effective. Participants’ ages ranged from 20 years to 60 years. All participants had completed 6 years of compulsory education; 618 (13.2%) had completed secondary school, 1057 (22.5%) had completed senior high school, 1190 (25.3%) had completed junior college, 1539 (32.8%) had completed college/university, and 239 (5.1%) were postgraduate students. Of the participants, 2069 (44.0%) engaged in intellectual occupations, 719 (15.3%) engaged in physical work, 1528 (32.5%) engaged in work that was both physical and intellectual, and 381 (8.1%) were homemakers. Family income was <RMB 2000 Yuan/month for 982 (20.9%) participants; RMB 2001–5000 Yuan/month for 2107 (44.9%); RMB 5001–10,000 Yuan/month for 1190 (25.3%), and >RMB 10,000 Yuan/month for 418 (8.9%) participants. Those living in urban areas accounted for 3754 (79.9%) participants, and 943 (20.1%) participants lived in rural areas [Table 1]. Menstrual status was regular for 3374 (71.8%) participants, irregular for 811 (17.3%), and 512 (10.9%) participants were postmenopausal; 760 (16.2%) participants had chronic disease and 267 (5.7%) had a history of pelvic surgery. Of the participants, 2840 (60.5%) had CPP, 344 (7.3%) had urinary incontinence, 62 (1.3%) had pelvic organ prolapse, and 1746 (37.5%) had gynecological disease. The participants’ marriage status and birth conditions are shown in Table 2.
Table 1.
The participants’ epidemiological profile in this study (n = 4697)
| Epidemiological characteristics | Values, n (%) |
|---|---|
| Age | |
| 20–29 years | 2066 (44.0) |
| 30–39 years | 681 (14.5) |
| 40–49 years | 1634 (34.8) |
| 50–60 years | 316 (6.3) |
| Education level | |
| Primary school | 45 (1.0) |
| Secondary school | 618 (13.2) |
| Senior high school | 1057 (22.5) |
| Junior college | 1190 (25.3) |
| College school | 1539 (32.8) |
| Postgraduate | 239 (5.1) |
| Occupation | |
| Brainwork | 2069 (44.0) |
| Physical work | 719 (15.3) |
| Brain and physical | 1528 (32.5) |
| Homemaker | 381 (8.1) |
| Family income | |
| ≤RNB 2000 Yuan/month | 982 (20.9) |
| RMB 2001–5000 Yuan/month | 2107 (44.9) |
| RMB 5001–10,000 Yuan/month | 1190 (25.3) |
| >RMB 10,000 Yuan/month | 418 (8.9) |
| Living environment | |
| Urban | 3754 (79.9) |
| Rural | 943 (20.1) |
| Chronic pelvic pain | |
| No | 1857 (39.5) |
| Yes | 2840 (60.5) |
| Gynecological disease | |
| No | 2951 (62.8) |
| Yes | 1746 (37.2) |
| Chronic disease | |
| No | 3937 (83.8) |
| Yes | 760 (16.2) |
| Pelvic surgery | |
| No | 4430 (94.3) |
| Yes | 267 (5.7) |
Table 2.
The participants’ marriage status and birth conditions in this study (n = 4697)
| Epidemiological characteristics | Values, n (%) |
|---|---|
| Menstrual status | |
| Regular pattern | 3374 (71.8) |
| Irregular | 811 (17.3) |
| Postmenopausal | 512 (10.9) |
| Marital status | |
| Married | 4478 (95.3) |
| Single | 77 (1.6) |
| Divorced | 49 (1.0) |
| Remarried | 26 (0.6) |
| Widowed | 67 (1.4) |
| Mode of delivery | |
| Nonparous | 706 (15.0) |
| Vaginal delivery | 2657 (56.6) |
| Cesarean section | 1334 (28.4) |
| Marital affection | |
| Very bad | 0 (0.0) |
| Relatively bad | 292 (6.2) |
| Common | 994 (21.2) |
| Relatively good | 1990 (42.4) |
| Very good | 1421 (30.3) |
| Marriage satisfaction | |
| Fairly satisfied | 1319 (28.1) |
| Satisfied | 2556 (54.4) |
| Common | 587 (12.5) |
| Dissatisfied | 146 (3.1) |
| Extremely disappointed | 89 (1.9) |
| Sexual difficulties of spouse | |
| Erectile dysfunction | 136 (2.9) |
| Rapid ejaculation | 189 (4.0) |
| Anaphrodisia | 586 (12.5) |
| None of the above | 3786 (80.6) |
| Satisfaction with spouse's sexual ability | |
| Fairly satisfied | 828 (17.6) |
| Satisfied | 2807 (60.0) |
| Common | 745 (15.9) |
| Dissatisfied | 211 (4.5) |
| Severely dissatisfied | 106 (2.3) |
The prevalence of adult FSD in Beijing was 2973 (63.3%) using a score of 26.55 as the boundary value, whereas the total mean FSFI score was 23.92 ± 6.37. The prevalence of adult female dysaphrodisia, arousal difficulties, vaginal lubrication problems, orgasmic dysfunction, sexual satisfaction disorders, and dyspareunia was 46.5%, 80.1%, 32.4%, 29.9%, 30.3%, and 31.6%, respectively [Figure 1]. Among women with FSD, 1423 (30.3%) never sought help, 1339 (28.5%) considered looking for information on the Internet or in books, and 1066 (22.7%) had visited a doctor.
Figure 1.
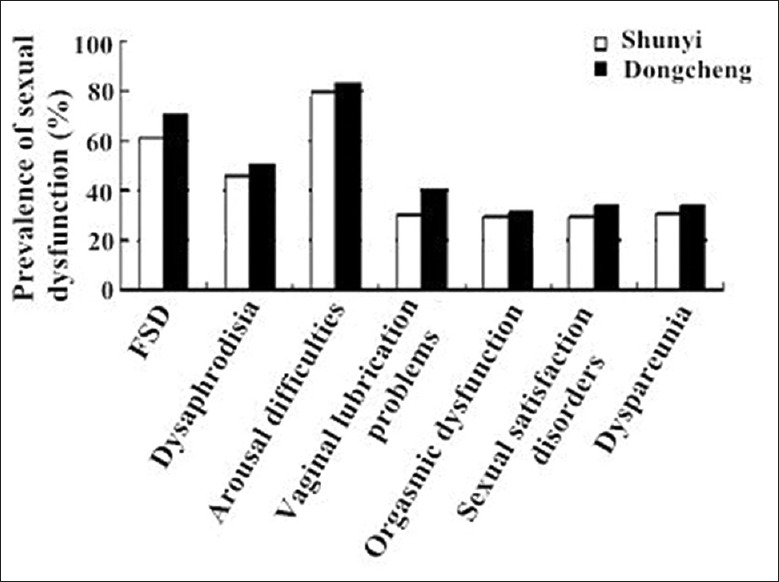
Prevalence of sexual dysfunction among women in Shunyi and Dongcheng districts of Beijing, China.
Multivariate logistic regression analysis was used for primary screening followed by multivariate logistic regression analysis of the potential factors for FSD. Age and sex life expectancy had significant colinearity (Spearman's index 0.794). By multivariate logistic regression analysis, the possible potential risk factors included age (OR = 1.051), dissatisfaction with the spouse's sexual ability (OR = 3.520), poor marital affection (OR = 2.087), spouse sexual difficulties (OR = 1.720), dissatisfaction with married life (OR = 1.476), living in a rural area (OR = 1.292), chronic pelvic pain (OR = 1.261), chronic disease (OR = 1.534), previous pelvic surgery (OR = 1.605), vaginal delivery (OR = 2.285), lower education (OR = 3.499), and postmenopausal (OR = 3.183). The sexual ability of the spouse, poor marital affection, postmenopausal, lower education, and spouse's sexual difficulties were the most probable and important factors [Table 3].
Table 3.
Multinomial logistic regression analysis of potential risk factors for female sexual dysfunction
| Variables | P | OR | 95% CI | |
|---|---|---|---|---|
| Lower boundary | Upper boundary | |||
| Age | 0.008 | 1.051 | 1.038 | 1.064 |
| Postmenopausal | 0.000 | 3.183 | 2.289 | 4.428 |
| Living in a rural area | 0.021 | 1.292 | 1.039 | 1.607 |
| Chronic pelvic pain | 0.002 | 1.261 | 1.087 | 1.464 |
| Chronic disease | 0.000 | 1.534 | 1.236 | 1.903 |
| Previous pelvic surgery | 0.010 | 1.605 | 1.120 | 2.299 |
| Vaginal delivery | 0.000 | 2.285 | 1.873 | 2.788 |
| Lower education | 0.012 | 3.449 | 1.308 | 9.099 |
| Poor marital affection | 0.000 | 2.087 | 1.663 | 2.620 |
| Marriage dissatisfaction | 0.011 | 1.476 | 1.092 | 1.994 |
| Sexual difficulties of spouse | 0.000 | 1.720 | 1.312 | 2.255 |
| Dissatisfaction with spouse's sexual ability | 0.000 | 3.520 | 2.656 | 4.666 |
OR: Odds ratio; CI: Confidence interval.
Discussion
Sexuality is a socially sensitive problem all over the world and has deep roots in many complicated health-related factors such as cultural, religious, and ethical social factors. The prevalence of FSD and effect factors was different between countries and different areas. The clinical diagnosis of FSD should be comprehensive and include a medical history, physical examination, psychological assessment, and diagnostic tests. No unified, objective, or quantifiable indicators are available. Almost all epidemiological surveys of FSD have been in questionnaire form. The FSFI questionnaire created in 2000 was developed as a brief, general, diagnostic epidemiological survey method for use all over the world.[10] A population-based sample study involved 5463 women aged 18–49 years in Finland in 2008 and found that 34.4% of women had sexual dysfunction (cutoff score ≤26.55).[12] In 2010, Echeverry et al.[13] reported the prevalence of FSD in sexually active women aged 18–40 years in Medellín, Colombia, as 30% (cutoff score ≤26.55). A self-administered questionnaire survey in 1580 female employees of two hospitals in South Taiwan, China reported that 43.8% had sexual difficulties in one or more domains (cutoff score ≤26.55).[13]
Although the population of China is approximately 1,300,000,000, no large-scale, population-based epidemiological survey of FSD has been conducted previously. In 2010, Sun et al.[11] completed the validation of the Chinese version of the FSFI. The present survey included 6000 women aged 20–66 years in Beijing using a self-reported questionnaire. Usually, an effective rate of ≥70% indicates the authenticity and effectiveness of a survey. We diagnosed FSD when the overall FSFI score was <26.55. Using the predetermined cutoff scores, the prevalence of adult female FSD in Beijing was 63.3%, higher than that of Europe, the US, and some Asian countries. The results of this survey reflected the real situation of adult FSD in Beijing and were closely related to the social and cultural background and sexual traditions in China.
The potential risk factors for FSD embodied a range of issues, but generally they could be classified into three categories: biological factors (e.g., age, hormone level, pelvic floor disease, and pelvic surgery), psychological factors (e.g., mood, affection for the spouse, and marital relationship), and social factors (e.g., education, economic level, social status, traditional culture, and religion). The effects of factors varied according to the different types of FSD. Satisfaction/dissatisfaction with the spouse's sexual ability and marital affection deserved more attention. A self-administered FSD questionnaire by Safarinejad[8] in Iran in 2006 showed that, among the women interviewed, 82% thought that their spouse's erectile dysfunction was significantly associated with their FSD and 72.3% attributed it to poor marital affection. A national survey of Swedes[14] found that appreciable erectile dysfunction or abnormal ejaculation increased the incidence of FSD. A research in Taiwan, China in 2009[15] showed that appreciable erectile dysfunction in the spouse caused female arousal, orgasmic dysfunction, and induced sexual dissatisfaction, and abnormal ejaculation might cause female sexual satisfaction disorder. The present study found that appreciable sexual difficulties of the spouse were potential risk factors for FSD. Male hypaphrodisia seemed to be the greatest factor influencing FSD, with a 7.1-increased incidence risk, followed by erectile dysfunction. Dissatisfaction with the spouse's sexual ability also increased the risk of FSD by approximately 6.94 times; therefore, this was another potential risk factor for FSD. The results of this study were practical and realistic and truthfully present issues. One plausible explanation was that, because of traditional Chinese culture, it is easier for Chinese women to point out sexual dysfunctions and dissatisfaction in themselves, but more difficult to admit the sexual problems of their spouse, such as erectile dysfunction. The results of this study also found that female affection toward the spouse strongly affected a woman's sexual function, even exceeding the influence of hormones.
In 1953, Kinsey et al.[16] proposed the theory that female sexual function changed with age and showed a declining trend with age. Safarinejad[8] used a FSFI questionnaire to survey 2626 Iranian women aged 20–60 years in 2006 and found that the prevalence of FSD increased with age. The same results were reported in Aslan et al.'s study[17] involving 1009 women in the outpatient clinic of a university hospital in Istanbul in 2008, Jiann et al.'s study in Taiwan, China in 2009,[15] and Ishak et al.'s study in Malaysia in 2010.[18]
The current research findings showed the increased prevalence with age. Our results also revealed that postmenopausal women had approximately 3 times higher risk of FSD than premenopausal ones. A decline in estrogen-induced vaginal dryness and increased intercourse pain might explain this phenomenon. The influence was progressive and a feature of the aging population.
Currently, data show that reproductive organ inflammation, myoma of the uterus; adenomyosis, cervical lesions, urinary incontinence, and other dysfunctions are rarely the cause of FSD. The present study found that the prevalence of FSD in healthy women was significantly lower than that among those who have gynecological diseases, indicating that gynecological disease was a risk factor for FSD. We also found that women with CPP were significantly more prone to FSD than women without CPP, indicating CPP as another risk factor for FSD. Pelvic surgery can cause FSD due to injury to the pelvic nerves or vessels during the procedure, inflammation and fibrosis after the surgery, and mental disorders caused. This study showed that both chronic disease and previous pelvic surgery are risk factors for FSD. Therefore, more attention must be paid to the disease during clinical treatment and management and how it impacts FSD.
This study also showed that the prevalence was significantly greater among women who had undergone a cesarean section compared with nulliparous women, but was significantly lower than that of the vaginal delivery group. Injury to pelvic floor organization and nerves by pregnancy and childbirth might cause an increased incidence of sexual dysfunction. Other vaginal delivery modes, such as vaginal dystocia, and vaginal birth were not classified in detail. Thus, additional studies on cesarean section and vaginal delivery and their influence on female sexuality are needed.
A survey in the US by Laumann et al.[6] in 1999 found that low economic social status and low education level were risk factors for FSD. Cayan et al.'s survey[19] in Turkey in 2004 showed that the prevalence of FSD among women with a university degree or higher was 29.1%, whereas the prevalence among women with a high school education or less was 70.9%. In 2006, Safarinejad et al.'s survey[8] in Iran revealed that women with a junior high school or high school level of education had a 1.3 and 1.5 times greater risk of FSD than women with university educations. Our investigation found that, as the education level increased, various types of FSD decreased in prevalence, indicating that higher education was a protective factor. Better-educated women pay more attention to sexual consciousness and property rights and are more able to express their appeal and dissatisfaction.
In human society, sex is closely related to marriage, emotions, and reproduction, but these cannot be completely equated. Emotion is the spiritual resonance, and marriage is a social contract. China implements a monogamous marriage system. Including marital and premarital sexual relationships, 95.7% of the respondents in our study were married, meaning that most of the respondents were in a stable partnership. Our data showed that women with fair marriage satisfaction experienced FSD less often than women who had more obstacles to marriage satisfaction, indicating that marriage dissatisfaction was a protective factor, reasonably.
In conclusion, female sexual problems are highly prevalent in Beijing. Dissatisfaction with the spouse's sexual ability, poor marital affection, sexual difficulties of the spouse, dissatisfaction with the marriage, rural life, CPP, and postmenopausal were conceivable risk factors for FSD in Beijing women. The sexual ability of the spouse, marital affection, postmenopausal, and spouse's sexual difficulties were the most probable and important factors. More research in different areas is essential for further understanding of FSD in China.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Xin Chen
References
- 1.Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008;77:635–42. doi: 10.1186/1471-2296-9-18. [PubMed] [Google Scholar]
- 2.Raina R, Pahlajani G, Khan S, Gupta S, Agarwal A, Zippe CD. Female sexual dysfunction: Classification, pathophysiology, and management. Fertil Steril. 2007;88:1273–84. doi: 10.1016/j.fertnstert.2007.09.012. doi: 10.1016/j.fertnstert.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Hisasue S, Kumamoto Y, Sato Y, Masumori N, Horita H, Kato R, et al. Prevalence of female sexual dysfunction symptoms and its relationship to quality of life: A Japanese female cohort study. Urology. 2005;65:143–8. doi: 10.1016/j.urology.2004.08.003. doi: 10.1016/j.urology.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Laumann EO, Glasser DB, Neves RC, Moreira ED., Jr GSSAB Investigators’ Group. A population-based survey of sexual activity, sexual problems and associated help-seeking behavior patterns in mature adults in the United States of America. Int J Impot Res. 2009;21:171–8. doi: 10.1038/ijir.2009.7. doi: 10.1038/ijir.2009.7. [DOI] [PubMed] [Google Scholar]
- 5.Hisasue S, Kumamoto Y, Sato Y, Masumori N, Horita H, Kato R, et al. Prevalence of female sexual dysfunction symptoms and its relationship to quality of life: A Japanese female cohort study. Urology. 2005;65:143–8. doi: 10.1016/j.urology.2004.08.003. doi: 10.1016/j.urology.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: Prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 7.Jones LR. The use of validated questionnaires to assess female sexual dysfunction. World J Urol. 2002;20:89–92. doi: 10.1007/s00345-002-0268-1. doi: 10.1007/s00345-002-0268-1. [DOI] [PubMed] [Google Scholar]
- 8.Safarinejad MR. Female sexual dysfunction in a population-based study in Iran: Prevalence and associated risk factors. Int J Impot Res. 2006;18:382–95. doi: 10.1038/sj.ijir.3901440. doi: 10.1038/sj.ijir.3901440. [DOI] [PubMed] [Google Scholar]
- 9.Parish WL, Laumann EO, Pan S, Hao Y. Sexual dysfunctions in urban china: A population-based national survey of men and women. J Sex Med. 2007;4:1559–74. doi: 10.1111/j.1743-6109.2007.00596.x. doi: 10.1111/j.1743-6109.2007.00596.x. [DOI] [PubMed] [Google Scholar]
- 10.Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): Cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 11.Sun X, Li C, Jin L, Fan Y, Wang D. Development and validation of Chinese version of Female Sexual Function Index in a Chinese population-a pilot study. J Sex Med. 2011;8:1101–11. doi: 10.1111/j.1743-6109.2010.02171.x. doi: 10.1111/j.1743-6109.2010.02171.x. [DOI] [PubMed] [Google Scholar]
- 12.Witting K, Santtila P, Varjonen M, Jern P, Johansson A, von der Pahlen B, et al. Female sexual dysfunction, sexual distress, and compatibility with partner. J Sex Med. 2008;5:2587–99. doi: 10.1111/j.1743-6109.2008.00984.x. doi: 10.1111/j.1743-6109.2008.00984.x. [DOI] [PubMed] [Google Scholar]
- 13.Echeverry MC, Arango A, Castro B, Raigosa G. Study of the prevalence of female sexual dysfunction in sexually active women 18 to 40 years of age in Medellín, Colombia. J Sex Med. 2010;7:2663–9. doi: 10.1111/j.1743-6109.2009.01695.x. doi: 10.1111/j.1743-6109.2009.01695.x. [DOI] [PubMed] [Google Scholar]
- 14.Fugl-Meyer AR, Fugl-Meyer K. Sexual disabilities, problems and satisfaction in 18-74-year-old Swedes. Scand J Sex. 1999;2:79–105. [Google Scholar]
- 15.Jiann BP, Su CC, Yu CC, Wu TT, Huang JK. Risk factors for individual domains of female sexual function. J Sex Med. 2009;6:3364–75. doi: 10.1111/j.1743-6109.2009.01494.x. doi: 10.1111/j.1743-6109.2009.01494.x. [DOI] [PubMed] [Google Scholar]
- 16.Kinsey AC, Pomeroy WB, Martin CE, Gebhard PH. Sexual behavior in the human female. Science. 1947;119:622–3. doi: 10.1126/science.119.3096.601. [Google Scholar]
- 17.Aslan E, Beji NK, Gungor I, Kadioglu A, Dikencik BK. Prevalence and risk factors for low sexual function in women: A study of 1,009 women in an outpatient clinic of a university hospital in Istanbul. J Sex Med. 2008;5:2044–52. doi: 10.1111/j.1743-6109.2008.00873.x. doi: 10.1111/j.1743-6109.2008.00873.x. [DOI] [PubMed] [Google Scholar]
- 18.Ishak IH, Low WY, Othman S. Prevalence, risk factors, and predictors of female sexual dysfunction in a primary care setting: A survey finding. J Sex Med. 2010;7:3080–7. doi: 10.1111/j.1743-6109.2010.01848.x. doi: 10.1111/j.1743-6109.2010.01848.x. [DOI] [PubMed] [Google Scholar]
- 19.Cayan S, Akbay E, Bozlu M, Canpolat B, Acar D, Ulusoy E. The prevalence of female sexual dysfunction and potential risk factors that may impair sexual function in Turkish women. Urol Int. 2004;72:52–7. doi: 10.1159/000075273. doi: 10.1159/000075273. [DOI] [PubMed] [Google Scholar]


