Abstract
Evidence suggests that living in a socioeconomically deprived neighborhood is associated with worse health. Yet most research relies on cross-sectional data, which implicitly ignore variation in longer-term exposure that may be more consequential for health. Using data from the 1970 to 2011 waves of the Panel Study of Income Dynamics merged with census data on respondents’ neighborhoods (N = 1,757), this study estimates a marginal structural model with inverse probability of treatment and censoring weights to examine: (1) whether cumulative exposure to neighborhood disadvantage from birth through age 17 affects self-rated health in early adulthood, and (2) the extent to which variation in such exposure helps to explain racial disparities therein. Findings reveal that prolonged exposure to neighborhood disadvantage throughout childhood and adolescence is strikingly more common among nonwhite versus white respondents and is associated with significantly greater odds of experiencing an incidence of fair or poor health in early adulthood.
Keywords: cumulative inequality, disadvantage, health, health disparities, life course, marginal structural model, neighborhood
Evidence that individual characteristics alone cannot explain population patterns of health and disease has contributed to a surge in research investigating whether and how broader contextual factors, such as the neighborhood environment, further shape the health of individual residents. Studies have found relationships between neighborhood characteristics, particularly concentrated poverty and other forms of socioeconomic disadvantage, and premature death (Doubeni et al. 2012), poor self-rated health (Tomey et al. 2013), depression and other mental health problems (Ahern and Galea 2011; Gapen et al. 2011), health-risk behaviors (Jackson, Knight, and Rafferty 2010), and various chronic conditions such as obesity, diabetes, cardiovascular disease, and certain cancers, even after adjustment for individual-level factors (Auchincloss et al. 2008; Diez Roux et al. 2001; Mujahid et al. 2008).
In addition, research documents that exposure to such adverse neighborhood conditions is unequally distributed both in the population and across the life course. People of color not only are more likely than their white counterparts to reside in a disadvantaged neighborhood in any single year but are also more likely to remain in such areas for repeated or prolonged periods of time (Quillian 2003; Sharkey 2013; Timberlake 2007). These findings point to the importance of considering both the occurrence and duration of exposure to neighborhood disadvantage, especially when assessing the contribution of neighborhood conditions to racial inequality.
Until recently, however, the majority of scholarship in this area measured neighborhood characteristics only once or over just a short window of observation, conflating persons who were recently exposed with those who have experienced more sustained residential adversity. Such a conceptualization is inconsistent with most theories of neighborhood effects, which tend to specify mechanisms that imply persistent exposure (Wodtke, Harding, and Elwert 2011), as well as with a life course perspective, in which experiences earlier in life are posited to have formative and enduring impacts on future outcomes, even when controlling for more contemporaneous determinants (Elder, Johnson, and Crosnoe 2003). Among the comparatively small but growing number of neighborhood-level studies that have employed longitudinal designs, few measure residential conditions regularly across childhood and adolescence, and even fewer examine subsequent effects on future health.
Using data from the 1970 to 2011 waves of the Panel Study of Income Dynamics (PSID) merged with census data on respondents’ neighborhoods, this study examines: (1) whether cumulative exposure to varying levels of neighborhood disadvantage from birth through age 17 affects self-rated health in early adulthood, and (2) the extent to which variation in the duration of such exposure helps to explain racial disparities therein. Neighborhood disadvantage is assessed once per year, every year throughout childhood and adolescence to better capture both change and persistence in residential conditions during this time (i.e., children can move into and out of different neighborhoods or they can remain in areas that may or may not change around them). In addition, this study employs a statistical method that accounts for neighborhood selection bias without controlling away the indirect pathways through which neighborhood effects may operate. As such, these findings provide a more comprehensive assessment of the young adult health consequences of exposure to neighborhood disadvantage that accumulates across the entire child and adolescent life course.
BACKGROUND
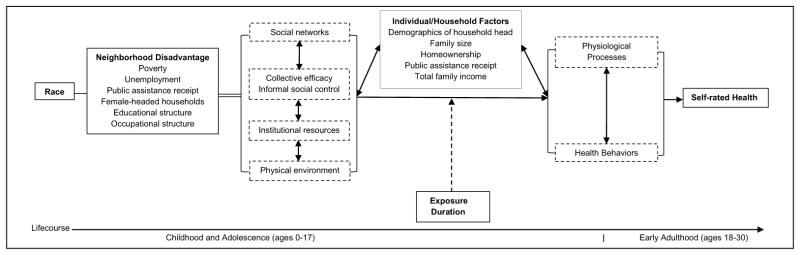
This study draws on the conceptual model depicted in Figure 1. In this model, race is a fundamental determinant of the level of neighborhood disadvantage into which a child is born as well as his or her likelihood of remaining in or moving out of similar residential environments over time. Neighborhood disadvantage is operationalized as the spatial clustering of poverty, unemployment, female-headed households, public assistance receipt, and educational and occupational marginalization. The assumption is that such composite neighborhood characteristics are concomitant to social processes and structural conditions that can directly, and in conjunction with individual- and household-level covariates, be salutogenic or pathogenic via their effects on more proximal behavioral and physiological determinants of health.
Figure 1.
Conceptual Model of the Effects of Exposure to Neighborhood Disadvantage throughout Childhood and Adolescence on Self-rated Health in Early Adulthood.
A life course perspective adds a temporal dimension to this model. Residing in a disadvantaged neighborhood for a moment in time can be hazardous, but it is less likely to dramatically impact one’s long-term health if surrounded by years of otherwise salutogenic residential exposures. On the other hand, experiencing similar adverse conditions repeatedly over time is more likely to have a compounding influence on future health. The various components of this model are discussed below.
Race and Residence in Separate and Unequal Spaces
Discriminatory housing policies and practices—including restrictive covenants, redlining, and residential steering as well as differentials in interest rates, subprime loans, and foreclosures—helped produce and continue to perpetuate the distinctive separation of whites and nonwhites in residential space (Peterson and Krivo 2010; Rugh, Albright, and Massey 2015). Of particular consequence is the inequality that often comes with such separation. Residential segregation concentrates advantage and power derived from a racialized social hierarchy within predominantly white neighborhoods, while disadvantage and marginalization are disproportionately concentrated in predominantly nonwhite neighborhoods (Logan 2011; Peterson and Krivo 2010). Given enduring constraints on residential mobility coupled with race-specific preferences for in-group and out-group neighbors (Sampson and Sharkey 2008), inter-neighborhood migration does little to alter such racial-spatial patterns of inequality (Crowder, Pais, and South 2012; Logan 2011; Sharkey 2013).
Social Processes and Structural Conditions Linking Neighborhoods and Health
Theory and previous research suggest at least four possible social and structural mechanisms through which the collective characteristics of places, and inequalities therein, operate to affect individual-level health (mental and physical) and health-risk behavior (e.g., violence, crime, substance use, and risky sexual activity) (Browning, Cagney, and Boettner 2016; Galster 2012; Sampson, Morenoff, and Gannon-Rowley 2002). First, neighborhood effects may be channeled through the resources within social networks. Neighbor A carries out a favor for Neighbor B (e.g., watching his or her children or providing advice about childrearing), trusting that the favor will be reciprocated at some later date. As favors multiply and are progressively exchanged across the network, a norm of reciprocity conducive to health and well-being is established (Kawachi 2010). In neighborhoods characterized by greater disadvantage, however, in which residents may be in greater need of support, the frequency of reciprocity exchanges can become burdensome and a hindrance to health and well-being, even when favors are likely to be returned (Gaumer, Jacobowitz, and Brooks-Gunn 2014; Newman and Chen 2007). Neighborhood networks can also facilitate the diffusion of health-related advice and other salutary information regarding housing, schooling, transportation, and employment. Nonetheless, Wilson (1987) argues that social ties among residents of disadvantaged neighborhoods tend to be more insular and to lack important connections that can transmit health-relevant information and services from the outside into the local network (Burt 2009; Granovetter 1995).
A second and related pathway through which neighborhood characteristics influence health is via collective efficacy, defined as mutual trust among residents as well as shared expectations and capacities for informal social control and collective action in relation to common objectives (Sampson 2012; Sampson, Morenoff, and Earls 1999). Robust inverse associations have been found between collective efficacy and violence, as residents are less likely to feel empowered to intervene when local norms are ambiguous and they mistrust or fear one another (Sampson, Raudenbush, and Earls 1997). Violence, in turn, not only threatens the health of those individuals directly involved, but also other residents who witness such incidents (Dupéré, Leventhal, and Vitaro 2012). Research has linked lower levels of collective efficacy to perceptions of danger and subsequent reductions in outdoor play and other forms of physical activity as well as with related increases in overweight/obesity and other stress-related conditions, such as depression, asthma, and cardiovascular disease (Burdette and Needham 2012; Cagney and Browning 2004). Theory and prior scholarship imply similar regulatory effects of collective efficacy on other problem behaviors, including illicit substance use, alcohol abuse, child neglect and abuse, and delinquency (Browning and Cagney 2002; Molnar et al. 2008; Simons et al. 2005). Moreover, collective efficacy can influence residents’ willingness and ability to mobilize and extract resources, for example, to protest the closure of a local hospital or clinic, to advocate for passage of a local ordinance to restrict smoking in public places, or to use zoning restrictions to prevent the citing of toxic waste, fast food, or alcohol outlets in the neighborhood (Bell and Rubin 2007; Kawachi 2010).
Third, neighborhood-health effects may operate through institutional resources. Disadvantaged neighborhoods often lack important health-promoting services (Bell and Rubin 2007). Medical institutions are an obvious example; however, persistent challenges to care often exist for residents of disadvantaged neighborhoods beyond their availability, including transportation difficulties, insensitive or culturally inappropriate treatment, long waiting room times, inadequately stocked pharmacies, and lack of multilingual staff (Sue and Zane 2009). Prior research further documents that supermarkets have sharply declined in low-income, predominantly nonwhite neighborhoods, forcing many residents to rely on convenience and other small stores with more limited, calorie-dense, and often higher-priced food selections (Liu et al. 2007; U.S. House Select Committee on Hunger 1990). These areas are also more likely to include a disproportionate share of fast food and alcohol outlets and associated advertising, which have been linked to poor diet, excessive alcohol consumption, and related harms, including chronic disease and injury (Campbell et al. 2009; Fuzhong et al. 2009). Moreover, because public school funding is often geographically determined, the schools in disadvantaged neighborhoods tend to have more dilapidated buildings, fewer qualified teachers, more limited curricula and academic counseling, fewer connections with colleges and employers, and higher levels of teen pregnancy. Such conditions may lead in turn to peer pressure against academic achievement and in support of health-compromising norms and behaviors (Williams 2003).
Finally, neighborhood characteristics may influence health through the physical environment—that is, patterns of regional design, growth, and change (Jackson 2003). Research has shown that high-poverty neighborhoods and neighborhoods of color are disproportionately located near major freeways, ports, and other industrial sources of diesel and air pollution (Lee 2002; Pais, Crowder, and Downey 2014), which may trigger asthma attacks and other respiratory problems, especially among children and other vulnerable populations (Clougherty et al. 2007; Delfino et al. 2009). The availability of sidewalks and safe, well-maintained streets and parks with adequate lighting can also influence health via opportunities for health-promoting activities, such as exercise and social interaction (Renalds, Smith, and Hale 2010). Moreover, patterns of suburban sprawl and systematic disinvestment in particular neighborhoods can also play a critical role in health by contributing to visual cues of neighborhood disorder (e.g., abandoned buildings, brownfields, graffiti, persistently broken windows), which have been shown in turn to affect social network ties and collective efficacy (Sampson and Raudenbush 1999).
Life Course Perspectives on Neighborhoods and Health
Neighborhoods are unlikely to have instantaneous or independent effects across the life course. A central theme of the life course perspective generally, and life course epidemiology more specifically, is the idea that exposures are linked to other exposures as well as outcomes in relation to time (Kuh et al. 2003; Lynch and Smith 2005). In particular, the effects of neighborhood disadvantage and the relative absence of concomitant social and structural resources and opportunities are thought to cluster, accumulate, and compound over time (in this case, across childhood and adolescence) such that future (young adult) health worsens as the duration of such exposure increases. This conceptualization has been broadly referenced as an accumulation model and more specifically, as a chain of risk model wherein a sequence of linked exposures raise the risk of poor health because one adverse exposure tends to be associated with another and so on; each of which can have both independent and cumulative effects on subsequent health (Kuh et al. 2003). Capturing the impact of such processes requires longitudinal study designs in which the temporal ordering of exposures and their interrelationships across time are explicit.
Existing Research on Neighborhoods and Health
The vast majority of extant research on neighborhoods and health has relied on cross-sectional data sets. Findings from this body of work are mixed. A wealth of studies document significant effects of neighborhood disadvantage, over and above individual-level factors, on various outcomes that are linked to self-rated health (Auchincloss et al. 2013; Brennan and Turrell 2012; Ding and Gebel 2012; Gidlow et al. 2010; Karasek, Ahern, and Galea 2012; Kawachi, Kennedy, and Glass 1999; Moore et al. 2009; Poortinga, Dunstan, and Fone 2008). Several studies, however, found significant effects of neighborhood affluence, but not neighborhood disadvantage (Browning and Cagney 2002, 2003; Wen, Browning, and Cagney 2003). Moreover, a few studies found no significant effects of neighborhood disadvantage on health after controlling for individual-level socioeconomic status, attributing contextual effects instead to the concentration of poor people in such areas (Duncan, Jones, and Moon 1993, 1995; Sloggett and Joshi 1994). One reason for these latter findings, as well as the often modest neighborhood-level (versus individual-level) coefficients in those studies in which an association with health is observed, may be the inability to account for the duration of exposure to health-relevant neighborhood characteristics.
The growing number of studies in which individuals’ residential environments have been assessed longitudinally show a more consistent and often larger effect on health. For example, in a pioneering study investigating the influence of current and prior neighborhoods on mental health using panel data that collected information across three waves, Wheaton and Clark (2003) found that childhood neighborhood has a lagged and cumulative effect on both externalizing and internalizing problems in early adulthood. Johnson and colleagues (2012) further examined the relationship between neighborhood characteristics in young adulthood (ages 20–30) and self-rated health in mid-to late life (age ≥ 35) using data on individuals who were followed for up to 38 years. Results suggest that young adult neighborhood characteristics, particularly concentrated poverty, account for up to 20% of the variation in health status in mid-to late life, even in the presence of a reasonably large amount of unobserved confounding due to individual- and household-level factors.
Moreover, Clarke and colleagues (2014) investigated changes in health status using a cumulative measure of exposure to neighborhood disadvantage among young adults (age ≥ 25) over 15 years and four waves of observation. Their findings document a significant cumulative effect of neighborhood disadvantage on changes in health status such that longer-term exposure is associated with 20% and 40% higher odds of functional decline and death, respectively, controlling for individual-level factors. Together, these results emphasize the potentially critical role not only of residential exposures at some earlier point in time, but of the accumulation of those past exposures for more precisely capturing neighborhood effects on health.
This study contributes to this emerging literature in at least two important ways. First, it explores the young adult health consequences of past residential exposures when neighborhood characteristics are measured regularly throughout the child and adolescent life course, from birth through age 17, rather than at only a few discrete points during this time or at already more advanced ages. Second, this study addresses the potential for bias due to the differential selection of individuals into or out of different neighborhoods using statistical methods that do not control away the indirect effects of neighborhoods which may operate through time-varying individual- and household-level factors, as is the case in conventional regression-based approaches.
To be sure, research focusing on outcomes other than health (Crowder and South 2011; Sampson, Sharkey, and Raudenbush 2008; Sharkey and Elwert 2011; Wodtke 2013; Wodtke et al. 2011), as well as an increasing number of social epidemiological studies (Cerda et al. 2010; Do, Wang, and Elliott 2013; Glymour et al. 2010; Kravitz-Wirtz 2016; Nandi et al. 2010; Oakes et al. 2015), have embraced this temporal turn in the neighborhood effects literature and have engaged explicitly with issues related to causality and time-varying confounding, although the focus with respect to health has generally been on exposures in adulthood. This study builds on such research to help clarify the effects of cumulative exposure to neighborhood disadvantage earlier in life, throughout childhood and adolescence, on self-rated health in early adulthood.
DATA AND METHODS
Data for this study were drawn from the PSID, a large, longitudinal survey of U.S. residents and their families conducted annually between 1968 and 1997, and every two years thereafter. The PSID has several strengths that made it particularly well suited for this study. First, it contained an oversam-ple of low-income families, as well as a wealth of information on a variety of individual- and household-level health-risk and protective factors. Second, the residential location of individual respondents at each interview could be linked to their corresponding census tract identifiers using the PSID’s supplemental, restricted-use Geospatial Match Files. These identifiers made it possible to characterize neighborhood disadvantage for prolonged intervals as well as to account for the potential mobility of respondents into and out of different neighborhoods. Third, the longitudinal design of the PSID made it possible to adjust for the temporal sequencing and compounding influence of individual, household, and neighborhood characteristics across time.
Sample Selection
The analytic sample for this study consisted of the 4,523 individuals born into PSID families between 1970 and 1980.1 Data on individual respondents were collected annually from birth until 2011 or until they were lost to follow-up. Given the focus on exposure to adverse neighborhood conditions throughout the entire child and adolescent life course, individuals were dropped if they were not continuously present in the survey for every year from ages 0 to 17 (N = 4,523 − 1,881 = 2,642). Of those, an additional 885 individuals did not respond to any questions about self-rated health in early adulthood and were excluded from analyses. The final sample included 1,757 individuals: 1,123 are classified as white and 634 are classified as non-white, of which the vast majority (94%) were black. Members of racial groups other than black were not represented in sufficient numbers to disaggregate the nonwhite category but were retained to maximize sample size.2
Dependent Variable
The dependent variable was self-rated health, which has shown high predictive validity for mortality, independent of other medical, behavioral, and psychosocial risk factors, as well as for future morbidity, healthcare utilization, and hospitalization (Idler and Angel 1990; Idler and Benyamini 1997). Self-rated health was assessed in the PSID at every wave since 1984, using the question, “Would you say your health in general is excellent, very good, good, fair, or poor?” Responses were dichotomized such that ‘0’ = “excellent, very good, or good” and ‘1’ = “fair or poor.” Given respondents’ relatively young age and thus lower likelihood of ill health, as well as this study’s focus on the incidence of poor health in early adulthood, the outcome of interest was any self-report of fair/poor health between ages 18 and 30.
Main Independent Variable
Census tracts were used to approximate neighborhood boundaries. Although there are limitations to this definition (Matthews 2011), there is broad consensus that census data at the tract level not only provide convenient access to considerable information over time, but also for most practical purposes, serve as a reasonable proxy for, or are at least highly correlated with, the causally relevant definition of a neighborhood (Crowder and Downey 2010; Diez Roux and Mair 2010; Sampson 2013). Information on census tracts in 1970, 1980, 1990, and 2000 came from the Neighborhood Change Database (NCDB; Geolytics 2012), in which data for all four decades had been normalized to 2000 tract boundaries and could therefore be compared across years without having to adjust for potential changes in boundary definitions over time. Data for intercensal years were imputed using linear interpolation.3
This study characterized neighborhood disadvantage in terms of the following census tract items thought to engender the social and structural mechanisms described previously: (1) proportion of residents below the poverty line, (2) proportion of residents (age ≥ 16) in the civilian labor force and unemployed, (3) proportion of households receiving public assistance, (4) proportion of female-headed households with children, (5) proportion of residents (age ≥ 25) with less than a high school diploma, (6) proportion of residents (age ≥ 25) with a bachelors/graduate/professional degree, and (7) proportion of residents (age ≥ 16) employed in managerial/professional/technical occupations.
Consistent with prior research (Messer et al. 2006; Stafford et al. 2005; Wodtke et al. 2011), Principal Components Analysis (PCA) was used to transform these seven items into a composite index of neighborhood disadvantage reflected by the first principal component. Each item’s loading on this component was used to weight its contribution to a neighborhood disadvantage score, which was calculated for every census tract at every year.4 The resulting scores were then divided into quintiles ranging from the least (level 1) to the most (level 5) disadvantaged based on the distribution of all tract-year observations in the NCDB between 1970 and 2000.
This contextual information was merged with the individual-level data such that each respondent received 18 different measurements of exposure to neighborhood disadvantage, 1 for every year from birth to age 17. Respondents’ cumulative exposure to neighborhood disadvantage throughout childhood and adolescence was calculated as the average of all the neighborhood disadvantage quintiles to which they were exposed from ages 1 to 17.5 While the same average value could be achieved for different patterns of exposure to neighborhood disadvantage, an exploratory latent class growth analysis showed that few respondents experienced upward or downward mobility, suggesting that an average measure of exposure to neighborhood disadvantage was a reasonable reflection of the cumulative experience of respondents in this study.
Covariates
Individual- and household-level variables were included in analyses as either time-invariant or time-varying. Time-invariant covariates included respondents’ race, gender, birth weight, and mother’s age and marital status, and the household head’s educational attainment at birth.6 Time-varying covariates, measured at each wave between ages 0 and 17, included the household head’s marital status, employment status and work hours, family size, homeownership, public assistance receipt, and total household income, standardized using the Consumer Price Index (CPI) to 1985 dollars.
Statistical Analysis
Initial analyses investigated the basic associations among race, neighborhood disadvantage, and self-rated health using conventional logistic regression models. The final analysis specified a marginal structural logistic regression model in which the parameters were estimated using Inverse Probability of Treatment (IPT) weights. The rationale behind this approach has to do with the failure of conventional regression models to take proper account of time-varying covariates that might be simultaneously confounders for the effects of future exposures and mediators for the effects of past exposures on future outcomes (Robins, Hernan, and Brumback 2000).
For instance, a family’s income directly influences both the type of neighborhood they can afford to live in and the health of its members. If a researcher does not control for family income when modeling the effects of neighborhood characteristics on health, she may overstate (or spuriously induce) the neighborhood–health relationship. Conversely, if she controls for family income, she removes from the final estimate the indirect effects of residential conditions that operate on health through family income (Kain 2004).
In longitudinal studies, this dilemma is compounded across time: family income, measured at any one wave, is a function of past income and past neighborhood conditions, as well as a determinant of future income, future neighborhood conditions, and future health. Controlling for family income and the other time-varying covariates all 18 times they are measured in this study would not only be cumbersome, but would wipe out the various indirect pathways through which neighborhood effects can transpire. Not controlling for such factors, however, could amount to neighborhood selection bias.
Marginal structural models using the IPT estimators were a means of incorporating the indirect effects of neighborhood disadvantage on health, while still adjusting for possible confounding (i.e., differential selection into and out of certain neighborhoods) by time-varying individual- and household-level covariates. This method proceeded in two steps. First, prior-year exposure to neighborhood disadvantage, time-invariant covariates, and both prior-year and concurrent time-varying covariates were used to predict respondents’ probability of exposure to each quintile of neighborhood disadvantage in each year. Respondents were then assigned a series of treatment weights based on the inverse of the predicted probability corresponding to the quintile of neighborhood disadvantage in which respondents were in fact observed (as opposed to the other four levels of disadvantage) in each year.
To obtain a more precise neighborhood effect estimate in the final marginal structural model, these weights were stabilized by multiplying each one by the same predicted probability as above, except time-varying covariates were excluded from the initial prediction model and the predicted probability was not inverted. The resulting series of stabilized treatment weights for each respondent at each age were then multiplied together to produce a single, summary weight reflecting the probability of exposure to that respondent’s actual sequence of neighborhood disadvantage quintiles throughout childhood and adolescence.
In the second step, a marginal structural logistic regression model estimating the effects of cumulative exposure to neighborhood disadvantage throughout childhood and adolescence on the probability of self-rated fair/poor health in early adulthood could be fit to a weighted pseudo-population generated using the stabilized treatment weights just described. Controlling for time-varying covariates was no longer necessary since their confounding effects on neighborhood selection had been accounted for through the weighting process. However, because time-invariant covariates were included in the regression models used to calculate both the numerator and denominator of the stabilized weights, they needed to still be controlled in the final model. Huber-White robust standard errors were used to account for the clustering of respondents within PSID households (Robins, Rotnitzky, and Scharfstein 2000; Wodtke et al. 2011).
To be unbiased and consistent, parameters estimated using IPT weights required several key assumptions, including no unmeasured confounding, no model misspecification, and positivity (Cole and Hernan 2008; Robins, Hernan, et al. 2000). Although this study adjusted for a wide array of among the most common predictors of both neighborhood selection and self-rated health, there was still the possibility that factors not measured in the PSID could upwardly bias the neighborhood effect estimate. Incorrectly specified models for selection into neighborhoods with varying levels of disadvantage could also bias the neighborhood effect estimate. However, other scholars utilizing the PSID and similar covariates have demonstrated that such estimates are relatively robust to a variety of model specifications (Wodtke 2013).
Finally, and perhaps most challenging in light of persistent racial-spatial inequalities, is the assumption of positivity, meaning that both nonwhites and whites must have a non-zero probability of exposure to every quintile of neighborhood disadvantage across all levels and combinations of measured covariates. Violations of the positivity assumption can result in weights that are unstable and sensitive to the presence of rare combinations of covariates. However, the IPT weights for this study displayed means reasonably close to one and small standard deviations, suggesting that the presence of rare combinations of covariates did not exert overt influence on the results. Although an argument in favor of weight truncation at the 1st and 99th or 5th and 95th percentiles could be justified on the basis of better behaved weights (mean = ‘1’, small range), substantive results based on these alternate specifications remain unchanged (see Appendix C in the online supplemental material, available at http://jhsb.sagepub.com/supplemental; Cole and Hernan 2008).
Sample Attrition
A considerable number of respondents were either lost to follow-up between birth and age 17 or did not respond to any self-rated health questions in early adulthood. This was not unexpected given the length of observation and stringent requirement that respondents be present at every wave of data collection from birth through age 17, plus at least 1 wave in early adulthood. To minimize the effects of biasing attrition, censoring weights were generated in the same manner as the stabilized treatment weights described above, except now the weights modeled the probability of remaining in the study for each respondent at each age, conditional on the same covariates as before.
More specifically, the age 1 censoring weights were generated by using what was known about respondents at birth (age 0), including levels of neighborhood disadvantage and both time-invariant and time-varying covariates, to predict the probability of remaining in (versus attriting from) the sample at age 1, and so on through age 17. By inverting this predicted probability, respondents who remained in the sample but who had characteristics more (or less) similar to those who attrited were given more (or less) weight. Again, these age-specific weights were stabilized and multiplied together to generate a summary censoring weight for each respondent. The weighted pseudo-population to which the final marginal structural model was fit, as described above, was actually constructed using the product of the stabilized IPT weight and the stabilized censoring weight for each respondent.
Missing Data
Missing data on all independent variables, including around 10% of observations for each time-invariant covariate (except race and gender, which were complete), 3% of observations for each time-varying covariate, and 18% of observations for neighborhood disadvantage, were multiply imputed using the twofold fully conditional specification algorithm (Welch, Bartlett, and Petersen 2014). The two-fold approach imputes missing values using chained equations at each time point, conditional on information at the same time point and user-specified adjacent time points. This study employed concurrent information plus or minus the two years adjacent to any missing values for the imputation. Findings were based on 10 multiple imputation data sets.
Due to computational constraints, missing data on the seven census tract items used to characterize neighborhood disadvantage were not imputed separately. Rather, only the summary score for neighborhood disadvantage generated through PCA based on those seven items was imputed. These imputed scores were then divided into quintiles using the preestablished cut points from the distribution of all (nonmissing) tract-year observations in the NCDB.
RESULTS
Sample Characteristics
Tables 1 and 2 display summary statistics for the time-invariant and time-varying characteristics, respectively, among respondents not lost to follow-up before age 18 and who answered at least one self-rated health question in early adulthood. A comparison by race reveals a pattern of notable differences. Nonwhite young adults were nearly two times more likely than their white counterparts to report fair/poor health at least once in early adulthood (27% versus 15%). As children, nonwhite respondents were also more likely to be born to an unmarried mother and into a household in which the head had less than a high school education. Moreover, they were nearly twice as likely as whites to be born low birth weight, a known risk factor for ongoing health problems.
Table 1.
Time-invariant sample characteristics
| Nonwhite | White | |
|---|---|---|
|
|
|
|
| (n=634) | (n=1123) | |
| Self-rated health in early adulthood, percent | ||
|
| ||
| Fair/poor health at least once between ages 18–30 | 26.66 | 14.69 |
| Excellent/very good/good health | 73.34 | 85.31 |
|
| ||
| Gender, percent | ||
|
| ||
| Female | 56.78 | 52.09 |
| Male | 43.22 | 47.91 |
|
| ||
| Birthweight, percent | ||
|
| ||
| Less than 88 ounces | 10.73 | 5.97 |
| 88 ounces or more | 89.27 | 94.03 |
|
| ||
| Mother’s marital status at birth, percent | ||
|
| ||
| Unmarried | 46.69 | 6.86 |
| Married | 53.31 | 93.14 |
|
| ||
| Household head’s educational attainment at birth, percent | ||
|
| ||
| Less than high school | 55.21 | 19.15 |
| High school graduate | 31.86 | 37.93 |
| At least some college | 12.93 | 42.92 |
|
| ||
| Mother’s age at birth, mean (SD) | 22.67 (5.17) | 25.45 (4.95) |
Note: Statistics reported for respondents not lost to follow -up before age 18 and w ho answ ered at least one self-rated health question in early adulthood (first of 10 imputation datasets); Differences by race are statistically significant at p<0.001
Table 2.
Time-varying sample characteristics
| Nonwhite (n=634) | White (n=1123) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Age 1 | Age 10 | Age 17 | Age 1 | Age 10 | Age 17 | |
| Neighborhood disadvantage quintile, percent | ||||||
| 1st quintile (least disadvantaged) | 2.05 | 3.47 | 5.52 | 14.43 | 18.97 | 21.73 |
| 2nd quintile | 2.84 | 5.52 | 8.04 | 20.75 | 18.79 | 21.73 |
| 3rd quintile | 6.15 | 6.78 | 9.78 | 22.97 | 25.73 | 25.65 |
| 4th quintile | 15.14 | 16.72 | 17.67 | 26.27 | 24.13 | 21.10 |
| 5th quintile (most disadvantaged) | 73.82 | 67.51 | 58.99 | 15.58 | 12.38 | 9.80 |
| Household head’s marital status, percent | ||||||
| Unmarried | 34.07 | 43.38 | 49.53 | 4.99 | 11.40 | 17.10 |
| Married | 65.93 | 56.62 | 50.47 | 95.01 | 88.60 | 82.90 |
| Household head’s employment status, percent | ||||||
| Unemployed | 28.86 | 33.60 | 29.81 | 7.93 | 10.15 | 9.17 |
| Employed | 71.14 | 66.40 | 70.19 | 92.07 | 89.85 | 90.83 |
| Public assistance receipt, percent | ||||||
| Received public assistance | 19.40 | 26.34 | 14.98 | 3.65 | 4.01 | 1.69 |
| Did not receive public assistance | 80.60 | 73.66 | 85.02 | 96.35 | 95.99 | 98.31 |
| Homeownership, percent | ||||||
| Does not own home | 64.98 | 57.26 | 49.05 | 38.74 | 23.06 | 19.95 |
| Owns home | 35.02 | 42.74 | 50.95 | 61.26 | 76.94 | 80.05 |
| Household income in (1985) $1,000s, mean (SD) | 15.41 (11.01) | 16.53 (13.83) | 18.06 (15.77) | 29.01 (16.85) | 25.69 (24.64) | 29.87 (31.82) |
| Household head’s work hours/week, mean (SD) | 27.92 (17.99) | 27.73 (19.90) | 29.59 (20.44) | 42.10 (15.02) | 41.51 (15.39) | 41.12 (15.75) |
| Family size, mean (SD) | 4.96 (2.64) | 4.74 (1.67) | 4.54 (1.62) | 3.91 (1.18) | 4.49 (1.04) | 4.09 (1.15) |
Note: Statistics reported for respondents not lost to follow -up before age 18 and w ho answ ered at least one self-rated health question in early adulthood (first of 10 imputation datasets); Within each age, differences by race are statistically significant at p<0.001
At various cross-sections throughout childhood and adolescence, nonwhite respondents also remained in households that were consistently more disadvantaged than white respondents with respect to the head’s marital and employment statuses, as well as income and hours worked per week, which were often close to half those of white household heads at ages 1, 10, and 17 (Table 2). The single most striking difference, however, was the inequality in exposure to neighborhood disadvantage highlighted at the top of Table 2. At age 1, for example, 74% of nonwhite children resided in the most disadvantaged neighborhood quintile compared to just 16% of white children. At the other end of the spectrum, only 2% of nonwhite versus 14% of white one-year-olds resided in neighborhoods characterized by the least disadvantage. This same general pattern of racial-spatial inequality persisted into adolescence, with 59% of nonwhites compared to 10% of whites residing in the most disadvantaged neighborhood quintile at age 17, while just 6% of nonwhites versus 22% of whites resided in the least disadvantaged quintile.
Cumulative Exposure to Neighborhood Disadvantage
Table 3 more explicitly quantifies racial differences in the duration of exposure to neighborhood disadvantage for nonwhite versus white children and youth from ages 1 through 17, documenting dramatic racial inequalities in both the average neighborhood disadvantage quintile to which children and youth were persistently exposed, as well as the proportion of time they resided in the most disadvantaged neighborhood quintile. In the top section of Table 3, higher values indicate more persistent exposure to neighborhood disadvantage. Consistent with but more pronounced than the racially disparate pattern of cross-sectional measures of neighborhood disadvantage presented previously, only 1% of nonwhite respondents were exposed to the least disadvantaged neighborhoods, on average, throughout childhood and adolescence whereas 61% grew up, on average, in the most disadvantaged neighborhood quintile. Conversely, most white respondents spent their youth in neighborhoods that were, on average, in the midrange of the disadvantage distribution. Only 7% resided in the most disadvantaged neighborhood quintile, while 13% experienced only the least disadvantaged neighborhoods before age 18, on average.7
Table 3.
Cumulative exposure to neighborhood disadvantage from ages one through 17
| Nonwhite | White | |
|---|---|---|
|
|
|
|
| (n=634) | (n=1123) | |
| Average neighborhood disadvantage quintile, percent | ||
|
| ||
| 1.0 to 1.4 (least disadvantaged) | 1.10 | 12.56 |
| 1.5 to 2.4 | 3.31 | 22.62 |
| 2.5 to 3.4 | 8.36 | 32.06 |
| 3.5 to 4.4 | 26.34 | 26.18 |
| 4.5 to 5.0 (most disadvantaged) | 60.88 | 6.59 |
|
| ||
| Proportion time in most disadvantaged quintile | ||
|
| ||
| Mean percent | 67.06 | 12.89 |
| Mean years | 11.4 | 2.19 |
Note: Statistics reported for respondents not lost to follow -up before age 18 and w ho answ ered at least one self-rated health question in early adulthood (first of 10 imputation datasets); Differences by race are statistically significant at p<0.001
The bottom section of Table 3 summarizes the proportion of time respondents spent in the most disadvantaged neighborhood quintile from ages 1 through 17. This measure helps operationalize variability in sustained exposure to the most extreme forms of neighborhood adversity. Again, dramatic racial disparities emerge that are more pronounced than at any single point in time. The average nonwhite respondent spent an overwhelming 67% of their youth in the most disadvantaged neighborhood quintile compared to 13% among the average white respondent. This translates to approximately 11 versus just 2 out of 17 years lived in neighborhoods characterized by the most disadvantage for nonwhite versus white respondents, respectively. Overall, these findings reiterate the persistence of racial residential segregation and prior research documenting the extremely “divergent social worlds” (Peterson and Krivo 2010), and thus health-relevant resources and opportunities, to which nonwhites and whites are persistently exposed over the course of childhood and adolescence.
Cumulative Neighborhood Effects on Self-rated Health Disparities
Table 4 shows unadjusted (Model 1), partially adjusted (Models 2–3), and marginal structural model (Model 4) estimates of the relationships among race, neighborhood disadvantage throughout childhood and adolescence, and self-rated health in early adulthood. The first model quantifies the statistically significant disparity in the probability of reporting fair/poor health at least once in early adulthood among nonwhite versus white respondents, without considering prior neighborhood exposures or individual- and household-level covariates. Results indicate that compared to whites, nonwhite respondents have over 2 times higher odds of experiencing fair/poor health at least once between ages 18 and 30 (exp [.75] = 2.12).
Table 4.
Effects of cumulative exposure to NH disadvantage from ages 0–17 on self-rated fair/poor health in early adulthood, n=1,757 (log odds ratios)
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | |||||
| Average NH disadvantage | 0.38 | 0.07 | *** | 0.38 | 0.08 | *** | 0.20 | 0.10 | * | |||
| Race (white) | ||||||||||||
| Nonwhite | 0.75 | 0.12 | *** | 0.23 | 0.15 | 0.26 | 0.68 | 0.34 | 0.20 | |||
| NH disadvantage X race | −0.01 | 0.16 | ||||||||||
| Gender (male) | ||||||||||||
| Female | 0.29 | 0.15 | ||||||||||
| Birthweight (88 ounces or more) | ||||||||||||
| Less than 88 ounces | −0.56 | 0.29 | ||||||||||
| Mother’s marital status at birth (married) | ||||||||||||
| Unmarried | −0.02 | 0.29 | ||||||||||
| HH’s education at birth (less than high school) | ||||||||||||
| High school graduate | −0.49 | 0.18 | ** | |||||||||
| At least some college | −0.66 | 0.25 | ** | |||||||||
| Mother’s age at birth | 0.03 | 0.02 | ||||||||||
| NH disadvantage at birth | 0.08 | 0.09 | ||||||||||
| HH’s marital status at birth (married) | ||||||||||||
| Unmarried | 0.33 | 0.31 | ||||||||||
| HH’s employment status at birth (employed) | ||||||||||||
| Unemployed | 0.13 | 0.26 | ||||||||||
| Homeownership at birth (owns home) | ||||||||||||
| Does not own home | 0.17 | 0.16 | ||||||||||
| Family size at birth | −0.04 | 0.04 | ||||||||||
| Public assistance receipt at birth (none) | ||||||||||||
| Received public assistance | 0.04 | 0.30 | ||||||||||
| Household income at birth | 0.21 | 0.13 | ||||||||||
| HH’s work hours per week at birth | 0.00 | 0.01 | ||||||||||
| Year born (1970–72) | ||||||||||||
| 1973–1975 | −0.14 | 0.21 | ||||||||||
| 1976–1978 | 0.06 | 0.20 | ||||||||||
| 1979–1980 | 0.11 | 0.23 | ||||||||||
Notes: Statistics reported for respondents not lost to follow-up before age 18 and who answered at least one self-rated health question in early adulthood; Coefficients are combined estimates from 10 multiple imputation datasets; NH=Neighborhood; HH=Household head;
p<0.05;
p<0.01;
p<0.001
Model 2 introduces a variable for cumulative exposure to neighborhood disadvantage, measured as the average of neighborhood disadvantage quin-tiles experienced by respondents every year from ages 1 through 17. Including this cumulative measure of neighborhood disadvantage, which is significantly associated with worse health, rendered the coefficient for race statistically nonsignificant, suggesting that race is no longer associated with self-rated health once neighborhood disadvantage is included in the model. As indicated by the non-significant interaction term added in Model 3, race also does not appear to moderate the association between cumulative neighborhood disadvantage and self-rated health. On the surface, these findings suggest not only that prior neighborhood conditions matter for future health but also that dramatic differences in the average level of neighborhood disadvantage to which nonwhite and white respondents are exposed during childhood and adolescence may account for a considerable share of the racial disparity in self-rated health in early adulthood.
Although instructive, the effect on young adult health of cumulative exposure to neighborhood disadvantage just described is likely intertwined with those of individual- and household-level characteristics that vary across childhood and adolescence in conjunction with variations in neighborhood conditions. To account for the potential confounding and mediating roles of such time-varying characteristics on the relationship between cumulative neighborhood disadvantage and self-rated health, Model 4 presents estimates from a marginal structural logistic regression analysis using stabilized IPT and censoring weights while also controlling for time-invariant characteristics.
These estimates indicate that residing in more disadvantaged neighborhoods throughout childhood and adolescence is associated with a statistically significant increase in the probability of reporting fair/poor health at least once between ages 18 and 30. Specifically, each unit (quintile) increase in cumulative neighborhood disadvantage from ages 1 through 17 is related to a 22% increase in the odds of experiencing an incidence of fair/poor health in early adulthood (exp [.20] = 1.22). By computational extension, respondents who were persistently exposed to neighborhoods in the most disadvantaged quintile from ages 1 through 17 (a majority of nonwhite respondents) had over two times higher odds of reporting fair/poor health at least once between ages 18 and 30 compared to (predominantly white) respondents who resided, on average, in the least disadvantaged neighborhood quintile (exp [(5–1) × .20] = 2.23).
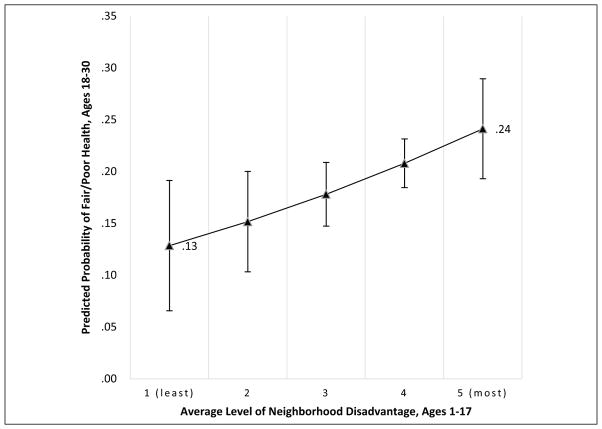
A visual representation of the effects of such neighborhood inequality on health is presented in Figure 2. It depicts predicted probabilities and their 95% confidence intervals of reporting fair/poor health in early adulthood by the average level of neighborhood disadvantage to which respondents were exposed as children and youth. All other baseline covariates are set to their sample means. As the figure indicates, if respondents had been persistently exposed to the least disadvantaged quintile of neighborhoods from ages 1 through 17, only about 1 in 10 (13%) would have reported an incidence of fair/poor health in early adulthood. Conversely, if the same respondents had been exposed, on average, to the fourth or fifth quintiles of neighborhood disadvantage as children and youth, approximately twice as many—that is, 1 in 5 (21%) or 1 in 4 (24%), respectively—would have reported an incidence of fair/poor health between ages 18 and 30. Given the links between self-rated health and concurrent and future physical and mental healthcare need and utilization, as well as comorbid conditions, such an increased incidence of fair/poor health among relatively young adults may represent a substantial added burden for this country’s most impoverished, underresourced, and racially segregated communities, as well as an important feedback mechanism through which neighborhood inequality is perpetuated.
Figure 2.
Predicted Probability of Self-rated Fair/Poor Health in Early Adulthood by Average Level of Neighborhood Disadvantage Experienced During Childhood and Adolescence, Panel Study of Income Dynamics, 1970–2011 (N = 1,757).
DISCUSSION
This study examined the effect of growing up in neighborhoods characterized by varying levels of disadvantage on self-rated health in early adulthood, utilizing the 1970 to 2011 waves of the PSID merged with census data on respondents’ neighborhoods. Findings show that more sustained exposure to neighborhood disadvantage throughout the child and adolescent life course has negative implications for self-rated health in early adulthood. In contrast to studies that have characterized the residential environment only once or over just a short window of observation, this study employed yearly measurements of respondents’ neighborhoods from birth through age 17, as well as a statistical method that accounts for dynamic individual- and household-level factors known to be predictive of future health but also related to the sorting of families into and out of neighborhoods over time. When such estimates are compared to those using more conventional regression-based techniques, which merely condition on time-varying covariates averaged across childhood and adolescence, the IPT-weighted neighborhood effect is slightly attenuated. This suggests, consistent with other work in this area (Jokela 2014), that respondents’ differential selection into more or less disadvantaged neighborhoods, as well as individual- and household-level factors, may account for some but not all of the neighborhood-health effect.
Moreover, while this study indicates that prolonged exposure to neighborhood disadvantage during childhood and adolescence is universally deleterious to young adult health, a more nuanced interpretation suggests that the adverse effects of neighborhood disadvantage are likely to be more concentrated among nonwhite children and youth. In keeping with other work on racial residential segregation and neighborhood stratification, results show that nonwhite children and youth are not only more likely than their white counterparts to be born into neighborhoods characterized by higher levels of disadvantage and thus fewer social and structural resources and opportunities, but to remain in similar types of health-compromising residential environments for the entirety of their pre-adult years. Thus, even as neighborhoods exert similar effects across racial groups, the separate and unequal residential contexts in which nonwhite versus white children and youth tend to persistently live, learn, and grow likely play a critical role in producing and perpetuating racial disparities in self-rated health in adulthood.
Limitations
Although this study uses panel data and unique statistical methods to address some of the most common challenges in neighborhood effects research, the results should be considered in the context of several remaining limitations. First, the absence of completely “tracted” land in 1970 and 1980 resulted in missing census data on neighborhood characteristics and necessitated imputation, which may have led to some misclassification of neighborhood disadvantage. Second, given the historical timing of this study, the sample is limited to white and predominantly black respondents. Future research examining health as a function of cumulative neighborhood effects among Asian and Latino populations is encouraged.
Third, although there appears to be sufficient overlap in the race-specific distributions of cumulative exposure to neighborhood disadvantage to generate stable IPT weights and thus to satisfy the positivity assumption on which the final analysis is based, it would be ideal (although perhaps not realistic) to find a sample in which neighborhood stratification is less pronounced in order to further disentangle the mechanisms behind the relationships among race, place, and health. Finally, this study did not assess the mechanisms thought to help explain how neighborhood-health effects transpire but rather the broader environment thought to engender such social processes and structural conditions. Longitudinal research able to more explicitly measure these potential mechanisms, including, for example, network ties, collective efficacy, social services, and environmental hazards, would be enlightening.
CONCLUSION
Findings from this study add to the growing body of evidence suggesting that place-based, developmentally appropriate, and ongoing investments in the social, economic, and structural aspects of underre-sourced neighborhoods and neighborhoods of color can have benefits for health and health equity that extend across the life course. On the one hand, a considerable body of prior scholarship has detailed the long arm of early-life individual- and family-level disadvantage on health in older ages, including the effects of family poverty in childhood (Brooks-Gunn and Duncan 1997) and early-life adversity and toxic stress (Felitti et al. 1998; Shonkoff et al. 2012; Shonkoff, Boyce, and McEwen 2009) on later-life physical and mental well-being and mortality. On the other hand, a related but often separate body of extensive research has shown that neighborhood-level disadvantage is associated with health in the cross-section and increasingly, over time. This study brings these two literatures into more explicit dialogue, empirically documenting the importance of child and adolescent neighborhood circumstances for later-life self-rated health.
Accordingly, in order to cultivate a more healthful and thus productive cadre of young adults, policies must strive to generate durable, place-based investments in children and youth (Bell and Rubin 2007; Sharkey 2013). Whereas prior neighborhood effects research based on cross-sectional data has often concluded with similar sentiments, the implementation of associated health policy and practice changes has generally been hampered by challenges to causal inference. Using longitudinal data and a statistical method that attempts to model the full data distribution (i.e., estimating each respondents’ level of self-rated health under each level of neighborhood disadvantage), this study provides strong evidence for the consequences of prolonged exposure to neighborhood disadvantage throughout childhood and adolescence on future (young adult) health, especially among nonwhite children and youth for whom such exposures tend to be more common and more persistent.
Supplementary Material
Biography
Nicole Kravitz-Wirtz is a postdoctoral fellow at the Population Studies Center at the University of Michigan. Her research focuses on the transmission of inequality within and between generations, particularly the effects of differences in exposure to household and neighborhood resources, hazards, and opportunity structures earlier in life on health and well-being later in life. She received her PhD in sociology with concentrations in health and social statistics from the University of Washington and her MPH with a concentration in epidemiology from the University of California, Los Angeles, Fielding School of Public Health.
Footnotes
Sample members were asked for their year of birth at multiple survey waves. If there were discrepancies across waves, the modal response was used.
The nonwhite category consists of 598 (94%) respondents who identified as black and 36 respondents (6%) who identified as a race other than white or black. Appendix A (in the online supplemental material, available at http://jhsb.sagepub.com/supplemental) details the composition of these nonwhite, nonblack respondents.
If decennial census tract data in 1970 or 1980 was missing and linear interpolation was impossible, data from 1980, 1990, and/or 2000 were used to extrapolate values for up to five years prior to the most recent value.
Only the first principal component was retained. Item loadings on this first component ranged from .341 for the proportion of female-headed households to .413 for the proportion of households receiving public assistance income (see Appendix B in the online supplemental material, available at http://jhsb.sagepub.com/supplemental).
Neighborhood disadvantage at birth is not included in this measure but rather as part of a vector of time-invariant covariates.
Household head’s educational attainment is treated as time-invariant and measured at respondents’ year of birth because the PSID does not measure parental education at regular intervals. If data at year of birth were missing, the most recent subsequent measurement was used, which for most respondents was within three years of birth.
Average neighborhood disadvantage is categorized and displayed as an ordinal variable in Table 3 for illustrative purposes. It is treated as a continuous variable in subsequent analyses.
The online appendices are available at http://jhsb.sagepub.com/supplemental.
References
- Ahern Jennifer, Galea Sandro. Collective Efficacy and Major Depression in Urban Neighborhoods. American Journal of Epidemiology. 2011;173(12):1453–62. doi: 10.1093/aje/kwr030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auchincloss Amy H, Diez Roux Ana V, Timothy Dvonch J, Brown Patrick L, Graham Barr R, Daviglus Martha L, Goff David C, Jr, Kaufman Joel D, O’Neill Marie S. Associations between Recent Exposure to Ambient Fine Particulate Matter and Blood Pressure in the Multi-ethnic Study of Atherosclerosis (MESA) Environmental Health Perspectives. 2008;116(4):486–91. doi: 10.1289/ehp.10899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auchincloss Amy H, Mujahid Mahasin S, Shen Mingwu, Michos Erin D, Whitt-Glover Melicia C, Diez Roux Ana V. Neighborhood Health-promoting Resources and Obesity Risk (the Multi-ethnic Study of Atherosclerosis) Obesity. 2013;21(3):621–28. doi: 10.1038/oby.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell Judith E, Rubin Victor. Why Place Matters: Building a Movement for Healthy Communities. Oakland, CA: PolicyLink; 2007. [Google Scholar]
- Brennan SL, Turrell G. Neighborhood Disadvantage, Individual-level Socioeconomic Position, and Self-reported Chronic Arthritis: A Cross-sectional Multilevel Study. Arthritis Care & Research. 2012;64(5):721–28. doi: 10.1002/acr.21590. [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn Jeanne, Duncan Greg J. The Effects of Poverty on Children. Future of Children. 1997;7(2):55–71. [PubMed] [Google Scholar]
- Browning Christopher R, Cagney Kathleen A. Neighborhood Structural Disadvantage, Collective Efficacy, and Self-rated Physical Health in an Urban Setting. Journal of Health and Social Behavior. 2002;43(4):383–99. [PubMed] [Google Scholar]
- Browning Christopher R, Cagney Kathleen A. Moving beyond Poverty: Neighborhood Structure, Social Processes, and Health. Journal of Health and Social Behavior. 2003;44(4):552–71. [PubMed] [Google Scholar]
- Browning Christopher R, Cagney Kathleen A, Boettner Bethany. Neighborhood, Place, and the Life Course. In: Shanahan JM, Jeylan Mortimer T, Johnson MK, editors. Handbook of the Life Course. Vol. 2. New York: Springer; 2016. pp. 597–620. [Google Scholar]
- Burdette Amy M, Needham Belinda L. Neighborhood Environment and Body Mass Index Trajectories from Adolescence to Adulthood. Journal of Adolescent Health. 2012;50(1):30–37. doi: 10.1016/j.jadohealth.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Burt Ronald S. Structural Holes: The Social Structure of Competition. Cambridge, MA: Harvard University Press; 2009. [Google Scholar]
- Cagney Kathleen A, Browning Christopher R. Exploring Neighborhood-level Variation in Asthma and Other Respiratory Diseases. Journal of General Internal Medicine. 2004;19(3):229–36. doi: 10.1111/j.1525-1497.2004.30359.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell Carla Alexia, Hahn Robert A, Elder Randy, Brewer Robert, Chattopadhyay Sajal, Fielding Jonathan, Naimi Timothy S, Toomey Traci, Lawrence Briana, Middleton Jennifer Cook. The Effectiveness of Limiting Alcohol Outlet Density as a Means of Reducing Excessive Alcohol Consumption and Alcohol-related Harms. American Journal of Preventive Medicine. 2009;37(6):556–69. doi: 10.1016/j.amepre.2009.09.028. [DOI] [PubMed] [Google Scholar]
- Cerda Magdalena, Diez Roux Ana V, Tchetgen Eric Tchetgen, Gordon-Larsen Penny, Kiefe Catarina. The Relationship between Neighborhood Poverty and Alcohol Use: Estimation by Marginal Structural Models. Epidemiology. 2010;21(4):482–89. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke Philippa, Morenoff Jeffrey, Debbink Michelle, Golberstein Ezra, Elliott Michael R, Lantz Paula M. Cumulative Exposure to Neighborhood Context: Consequences for Health Transitions over the Adult Life Course. Research on Aging. 2014;36(1):115–42. doi: 10.1177/0164027512470702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty Jane E, Levy Jonathan I, Kubzansky Laura D, Barry Ryan P, Suglia Shakira Franco, Canner Marina Jacobson, Wright Rosalind J. Synergistic Effects of Traffic-related Air Pollution and Exposure to Violence on Urban Asthma Etiology. Environmental Health Perspectives. 2007;115(8):1140–46. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole Stephen R, Hernan Miguel A. Constructing Inverse Probability Weights for Marginal Structural Models. American Journal of Epidemiology. 2008;168(6):656–64. doi: 10.1093/aje/kwn164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowder Kyle, Downey Liam C. Inter-neighborhood Migration, Race, and Environmental Hazards: Modeling Micro-level Processes of Environmental Inequality. American Journal of Sociology. 2010;115(4):1110–49. doi: 10.1086/649576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowder Kyle, Pais Jeremy, South Scott J. Neighborhood Diversity, Metropolitan Constraints, and Household Migration. American Sociological Review. 2012;77(3):325–53. doi: 10.1177/0003122412441791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowder Kyle, South Scott J. Spatial and Temporal Dimensions of Neighborhood Effects on High School Graduation. Social Science Research. 2011;40(1):87–106. doi: 10.1016/j.ssresearch.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino Ralph J, Chang Joyce, Wu Jun, Ren Cizao, Tjoa Thomas, Nickerson Bruce, Cooper Dan, Gillen Daniel L. Repeated Hospital Encounters for Asthma in Children and Exposure to Traffic-related Air Pollution Near the Home. Annals of Allergy, Asthma & Immunology. 2009;102(2):138–44. doi: 10.1016/S1081-1206(10)60244-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux Ana V, Mair Christina. Neighborhoods and Health. Annals of the New York Academy of Sciences. 2010;1186(1):125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Diez Roux Ana V, Merkin Sharon Stein, Arnett Donna, Chambless Lloyd, Massing Mark, Javier Nieto F, Sorlie Paul, Szklo Moyses, Tyroler Herman A, Watson Robert L. Neighborhood of Residence and Incidence of Coronary Heart Disease. New England Journal of Medicine. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Ding Ding, Gebel Klaus. Built Environment, Physical Activity, and Obesity: What Have We Learned from Reviewing the Literature? Health & Place. 2012;18(1):100–105. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Do D Phuong, Wang Lu, Elliott Michael R. Investigating the Relationship between Neighborhood Poverty and Mortality Risk: A Marginal Structural Modeling Approach. Social Science & Medicine. 2013;91:58–66. doi: 10.1016/j.socscimed.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doubeni Chyke A, Schootman Mario, Major Jacqueline M, Torres Stone Rosalie A, Laiyemo Adeyinka O, Park Yikyung, Lian Min, Messer Lynne, Graubard Barry I, Sinha Rashmi, Hollenbeck Albert R, Schatzkin Arthur. Health Status, Neighborhood Socioeconomic Context, and Premature Mortality in the United States: The National Institutes of Health–AARP Diet and Health Study. American Journal of Public Health. 2012;102(4):680–88. doi: 10.2105/AJPH.2011.300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan Craig, Jones Kelvyn, Moon Graham. Do Places Matter? A Multi-level Analysis of Regional Variations in Health-related Behaviour in Britain. Social Science & Medicine. 1993;37(6):725–33. doi: 10.1016/0277-9536(93)90366-c. [DOI] [PubMed] [Google Scholar]
- Duncan Craig, Jones Kelvyn, Moon Graham. Psychiatric Morbidity: A Multilevel Approach to Regional Variations in the UK. Journal of Epidemiology and Community Health. 1995;49(3):290–95. doi: 10.1136/jech.49.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupéré Véronique, Leventhal Tama, Vitaro Frank. Neighborhood Processes, Self-efficacy, and Adolescent Mental Health. Journal of Health and Social Behavior. 2012;53(2):183–98. doi: 10.1177/0022146512442676. [DOI] [PubMed] [Google Scholar]
- Elder Glen H, Jr, Johnson Monica Kirkpatrick, Crosnoe Robert. The Emergence and Development of Life Course Theory. In: Mortimer JT, Shanahan MJ, editors. Handbook of the Life Course. New York: Kluwer Academic/Plenum; 2003. pp. 3–19. [Google Scholar]
- Felitti Vincent J, Anda Robert F, Nordenberg Dale, Williamson David F, Spitz Alison M, Edwards Valerie, Koss Mary P, Marks James S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fuzhong Li, Harmer Peter, Cardinal Bradley J, Bosworth Mark, Johnson-Shelton Deb. Obesity and the Built Environment: Does the Density of Neighborhood Fast-food Outlets Matter? American Journal of Health Promotion. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galster George C. The Mechanism(s) of Neighbourhood Effects: Theory, Evidence, and Policy Implications. In: van Ham M, Manley D, Bailey N, Simpson L, Maclennan D, editors. Neighbourhood Effects Research: New Perspectives. Houton, Netherlands: Springer; 2012. pp. 23–56. [Google Scholar]
- Gapen Mark, Cross Dorthie, Ortigo Kile, Graham Allen, Johnson Eboni, Evces Mark, Ressler Kerry J, Bradley Bekh. Perceived Neighborhood Disorder, Community Cohesion, and PTSD Symptoms among Low-income African Americans in an Urban Health Setting. American Journal of Orthopsychiatry. 2011;81(1):31–37. doi: 10.1111/j.1939-0025.2010.01069.x. [DOI] [PubMed] [Google Scholar]
- Gaumer Elyzabeth, Jacobowitz Ahuva, Brooks-Gunn Jeanne. Building Ties: The Social Networks of Affordable-housing Residents. Cityscape: A Journal of Policy Development and Research. 2014;16(3):47–68. [Google Scholar]
- Geolytics. Neighborhood Change Database, 1970–2010. Somerville, NJ: Author; 2012. [Google Scholar]
- Gidlow Christopher, Cochrane Thomas, Davey Rachel C, Smith Graham, Fairburn Jon. Relative Importance of Physical and Social Aspects of Perceived Neighbourhood Environment for Self-reported Health. Preventive Medicine. 2010;51(2):157–63. doi: 10.1016/j.ypmed.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Glymour M Maria, Mujahid Mahasin, Wu Qiong, White Kellee, Tchetgen Tchetgen Eric J. Neighborhood Disadvantage and Self-assessed Health, Disability, and Depressive Symptoms: Longitudinal Results from the Health and Retirement Study. Annals of Epidemiology. 2010;20(11):856–61. doi: 10.1016/j.annepidem.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granovetter Mark. Getting a Job: A Study of Contacts and Careers. Chicago: University of Chicago Press; 1995. [Google Scholar]
- Idler Ellen L, Angel Ronald J. Self-rated Health and Mortality in the NHANES-I Epidemiologic Follow-up Study. American Journal of Public Health. 1990;80(4):446–52. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler Ellen L, Benyamini Yael. Self-rated Health and Mortality: A Review of Twenty-seven Community Studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Jackson James S, Knight Katherine M, Rafferty Jane A. Race and Unhealthy Behaviors: Chronic Stress, the HPA Axis, and Physical and Mental Health Disparities over the Life Course. American Journal of Public Health. 2010;100(5):933–39. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson Richard J. The Impact of the Built Environment on Health: An Emerging Field. American Journal of Public Health. 2003;93(9):1382–84. doi: 10.2105/ajph.93.9.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson Rucker C, Schoeni Robert F, Rogowski Jeannette A. Health Disparities in Mid-to-late Life: The Role of Earlier Life Family and Neighborhood Socioeconomic Conditions. Social Science & Medicine. 2012;74(4):625–36. doi: 10.1016/j.socscimed.2011.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokela Markus. Are Neighborhood Health Associations Causal? A 10-year Prospective Cohort Study with Repeated Measurements. American Journal of Epidemiology. 2014;180(8):776–84. doi: 10.1093/aje/kwu233. [DOI] [PubMed] [Google Scholar]
- Kain John F. A Pioneer’s Perspective on the Spatial Mismatch Literature. Urban Studies. 2004;41(1): 7–32. [Google Scholar]
- Karasek Deborah, Ahern Jennifer, Galea Sandro. Social Norms, Collective Efficacy, and Smoking Cessation in Urban Neighborhoods. American Journal of Public Health. 2012;102(2):343–51. doi: 10.2105/AJPH.2011.300364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi Ichiro. Social Capital and Health. In: Bird CE, Conrad P, Fremont AM, Timmermans S, editors. Handbook of Medical Sociology. Nashville, TN: Vanderbilt University Press; 2010. p. 18. [Google Scholar]
- Kawachi Ichiro, Kennedy Bruce P, Glass Roberta. Social Capital and Self-rated Health: a Contextual Analysis. American Journal of Public Health. 1999;89(8):1187–93. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz-Wirtz Nicole. A Discrete-time Analysis of the Effects of More Prolonged Exposure to Neighborhood Poverty on the Risk of Smoking Initiation by Age 25. Social Science & Medicine. 2016;148:79–92. doi: 10.1016/j.socscimed.2015.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life Course Epidemiology. Journal of Epidemiology and Community Health. 2003;57(10):778–83. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Charles. Environmental Justice: Building a Unified Vision of Health and the Environment. Environmental Health Perspectives. 2002;110(Suppl 2):141–44. doi: 10.1289/ehp.02110s2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Gilbert C, Wilson Jeffrey S, Qi Rong, Ying Jun. Green Neighborhoods, Food Retail and Childhood Overweight: Differences by Population Density. American Journal of Health Promotion. 2007;21(4s):317–25. doi: 10.4278/0890-1171-21.4s.317. [DOI] [PubMed] [Google Scholar]
- Logan John R. Project US2010 Report. New York: Russell Sage Foundation; 2011. Separate and Unequal: The Neighborhood Gap for Blacks, Hispanics and Asians in Metropolitan America; pp. 1–22. [Google Scholar]
- Lynch John, Smith George Davey. A Life Course Approach to Chronic Disease Epidemiology. Annual Review of Public Health. 2005;26(1):1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- Matthews Stephen A. Spatial Polygamy and the Heterogeneity of Place: Studying People and Place via Egocentric Methods. In: Burton LM, Kemp SP, Leung M, Matthews SA, Takeuchi DT, editors. Communities, Neighborhoods, and Health: Expanding the Boundaries of Place. New York: Springer; 2011. pp. 35–56. [Google Scholar]
- Messer Lynne C, Laraia Barbara A, Kaufman Jay S, Eyster Janet, Holzman Claudia, Culhane Jennifer, Elo Irma, Burke Jessica G, O’Campo Patricia. The Development of a Standardized Neighborhood Deprivation Index. Journal of Urban Health. 2006;83(6):1041–62. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar Beth E, Cerda Magdalena, Roberts Andrea L, Buka Stephen L. Effects of Neighborhood Resources on Aggressive and Delinquent Behaviors among Urban Youths. American Journal of Public Health. 2008;98(6):1086–93. doi: 10.2105/AJPH.2006.098913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore Latetia V, Diez Roux Ana V, Nettleton Jennifer A, Jacobs David R, Franco Manuel. Fast-food Consumption, Diet Quality, and Neighborhood Exposure to Fast Food: The Multi-ethnic Study of Atherosclerosis. American Journal of Epidemiology. 2009;170(1):29–36. doi: 10.1093/aje/kwp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujahid Mahasin S, Diez Roux Ana V, Shen Mingwu, Gowda Deepthiman, Sanchez Brisa, Shea Steven, Jacobs David R, Jackson Sharon A. Relation between Neighborhood Environments and Obesity in the Multi-ethnic Study of Atherosclerosis. American Journal of Epidemiology. 2008;167(11):1349–57. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- Nandi Arijit, Glass Thomas A, Cole Stephen R, Chu Haitao, Galea Sandro, Celentano David D, Kirk Gregory D, Vlahov David, Latimer William W, Mehta Shruti H. Neighborhood Poverty and Injection Cessation in a Sample of Injection Drug Users. American Journal of Epidemiology. 2010;171(4):391–98. doi: 10.1093/aje/kwp416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman Katherine S, Chen Victor Tan. The Missing Class: Portraits of the Near Poor in America. Boston: Beacon Press; 2007. [Google Scholar]
- Oakes J Michael, Andrade Kate E, Biyoow Ifrah M, Cowan Logan T. Twenty Years of Neighborhood Effect Research: An Assessment. Current Epidemiology Reports. 2015;2(1):80–87. doi: 10.1007/s40471-015-0035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pais Jeremy, Crowder Kyle, Downey Liam. Unequal Trajectories: Racial and Class Differences in Residential Exposure to Industrial Hazard. Social Forces. 2014;92(3):1189–215. doi: 10.1093/sf/sot099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson Ruth D, Krivo Lauren J. Divergent Social Worlds: Neighborhood Crime and the Racial-spatial Divide. New York: Russell Sage Foundation; 2010. [Google Scholar]
- Poortinga Wouter, Dunstan Frank D, Fone David L. Neighbourhood Deprivation and Self-rated Health: The Role of Perceptions of the Neighbourhood and of Housing Problems. Health & Place. 2008;14(3):562–75. doi: 10.1016/j.healthplace.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Quillian Lincoln. How Long Are Exposures to Poor Neighborhoods? The Long-term Dynamics of Entry and Exit from Poor Neighborhoods. Population Research and Policy Review. 2003;22(3): 221–49. [Google Scholar]
- Renalds Arlene, Smith Tracey H, Hale Patty J. A Systematic Review of Built Environment and Health. Family & Community Health. 2010;33(1): 68–78. doi: 10.1097/FCH.0b013e3181c4e2e5. [DOI] [PubMed] [Google Scholar]
- Robins James M, Rotnitzky Andrea, Scharfstein Daniel O. Sensitivity Analysis for Selection Bias and Unmeasured Confounding in Missing Data and Causal Inference Models. In: Halloran ME, Berry D, editors. Statistical Models in Epidemiology, the Environment, and Clinical Trials. New York: Springer; 2000. pp. 1–94. [Google Scholar]
- Robins James M, Hernan Miguel Angel, Brumback Babette. Marginal Structural Models and Causal Inference in Epidemiology. Epidemiology. 2000;11(5):550–60. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- Rugh Jacob S, Albright Len, Massey Douglas S. Race, Space, and Cumulative Disadvantage: A Case Study of the Subprime Lending Collapse. Social Problems. 2015;62:186–218. doi: 10.1093/socpro/spv002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson Robert J. Great American City: Chicago and the Enduring Neighborhood Effect. Chicago: University of Chicago Press; 2012. [Google Scholar]
- Sampson Robert J. The Place of Context: A Theory and Strategy for Criminology’s Hard Problems. Criminology. 2013;51(1):1–31. [Google Scholar]
- Sampson Robert J, Morenoff Jeff D, Earls Felton. Beyond Social Capital: Spatial Dynamics of Collective Efficacy for Children. American Sociological Review. 1999;64:633–60. [Google Scholar]
- Sampson Robert J, Morenoff Jeffrey D, Gannon-Rowley Thomas. Assessing ‘Neighborhood Effects’: Social Processes and New Directions in Research. Annual Review of Sociology. 2002;28:443–78. [Google Scholar]
- Sampson Robert J, Raudenbush Stephen W. Systematic Social Observation of Public Spaces: A New Look at Disorder in Urban Neighborhoods 1. American Journal of Sociology. 1999;105(3):603–51. [Google Scholar]
- Sampson Robert J, Raudenbush Stephen W, Earls Felton. Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy. Science. 1997;277(5328):918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sampson Robert J, Sharkey Patrick. Neighborhood Selection and the Social Reproduction of Concentrated Racial Inequality. Demography. 2008;45(1):1–29. doi: 10.1353/dem.2008.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson Robert J, Sharkey Patrick, Raudenbush Stephen W. Durable Effects of Concentrated Disadvantage on Verbal Ability among African-American Children. Proceedings of the National Academy of Sciences. 2008;105(3):845–52. doi: 10.1073/pnas.0710189104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey Patrick. Stuck in Place: Urban Neighborhoods and the End of Progress toward Racial Equality. Chicago: University of Chicago Press; 2013. [Google Scholar]
- Sharkey Patrick, Elwert Felix. The Legacy of Disadvantage: Multigenerational Neighborhood Effects on Cognitive Ability. American Journal of Sociology. 2011;116(6):1934–81. doi: 10.1086/660009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff Jack P, Thomas Boyce W, McEwen Bruce S. Neuroscience, Molecular Biology, and the Childhood Roots of Health Disparities. JAMA: The Journal of the American Medical Association. 2009;301(21):2252–59. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Shonkoff Jack P, Garner Andrew S, Siegel Benjamin S, Dobbins Mary I, Earls Marian F, McGuinn Laura, Pascoe John, Wood David L. The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics. 2012;129(1):e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Simons Ronald L, Simons Leslie Gordon, Burt Callie Harbin, Brody Gene H, Cutrona Carolyn. Collective Efficacy, Authoritative Parenting and Delinquency: A Longitudinal Test of a Model Integrating Community- and Family-level Processes. Criminology. 2005;43(4):989–1029. [Google Scholar]
- Sloggett Andrew, Joshi Heather. Higher Mortality in Deprived Areas: Community or Personal Disadvantage? BMJ. 1994;309(6967):1470–74. doi: 10.1136/bmj.309.6967.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford Mai, Cummins Steven, Macintyre Sally, Ellaway Anne, Marmot Michael. Gender Differences in the Associations between Health and Neighbourhood Environment. Social Science & Medicine. 2005;60(8):1681–92. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Sue Stanley, Zane Nolan. The Role of Culture and Cultural Techniques in Psychotherapy: A Critique and Reformulation. Asian American Journal of Psychology. 2009;S(1):3–14. doi: 10.1037//0003-066x.42.1.37. (The first author presented an earlier version of this article as an invited address at the Asian American Psychological Association Convention, August 1985, Los Angeles.) [DOI] [PubMed] [Google Scholar]
- Timberlake Jeffrey M. Racial and Ethnic Inequality in the Duration of Children’s Exposure to Neighborhood Poverty and Affluence. Social Problems. 2007;54(3):319–42. [Google Scholar]
- Tomey Kristin, Diez Roux Ana V, Clarke Philippa, Seeman Teresa. Associations between Neighborhood Characteristics and Self-rated Health: A Cross-sectional Investigation in the Multi-ethnic Study of Atherosclerosis (MESA) Cohort. Health & Place. 2013;24:267–74. doi: 10.1016/j.healthplace.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. House Select Committee on Hunger. Obtaining Food: Shopping Constraints of the Poor. Black Scholar. 1990;21(1):6–16. [Google Scholar]
- Welch Catherine, Bartlett Jonathan, Petersen Irene. Application of Multiple Imputation Using the Two-fold Fully Conditional Specification Algorithm in Longitudinal Clinical Data. Stata Journal. 2014;14(2):418–31. [PMC free article] [PubMed] [Google Scholar]
- Wen Ming, Browning Christopher R, Cagney Kathleen A. Poverty, Affluence, and Income Inequality: Neighborhood Economic Structure and Its Implications for Health. Social Science & Medicine. 2003;57(5):843–60. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- Wheaton Blair, Clarke Philippa. Space Meets Time: Integrating Temporal and Contextual Influences on Mental Health in Early Adulthood. American Sociological Review. 2003;68(5):680–706. [Google Scholar]
- Williams David R. The Health of Men: Structured Inequalities and Opportunities. American Journal of Public Health. 2003;93(5):724–31. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson William Julius. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago: University of Chicago Press; 1987. [Google Scholar]
- Wodtke Geoffrey T. Duration and Timing of Exposure to Neighborhood Poverty and the Risk of Adolescent Parenthood. Demography. 2013;50(5):1765–88. doi: 10.1007/s13524-013-0219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wodtke Geoffrey T, Harding David J, Elwert Felix. Neighborhood Effects in Temporal Perspective: The Impact of Long-term Exposure to Concentrated Disadvantage on High School Graduation. American Sociological Review. 2011;76(5):713–36. doi: 10.1177/0003122411420816. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.