Abstract
Objective:
Most patients admitted to Intensive Care Units (ICU) have problems in using oral medication or ingesting solid forms of drugs. Selecting the most suitable dosage form in such patients is a challenge. The current study was conducted to assess the frequency and types of errors of oral medication administration in patients with enteral feeding tubes or suffering swallowing problems.
Methods:
A cross-sectional study was performed in the ICU of Shahid Sadoughi Hospital, Yazd, Iran. Patients were assessed for the incidence and types of medication errors occurring in the process of preparation and administration of oral medicines.
Findings:
Ninety-four patients were involved in this study and 10,250 administrations were observed. Totally, 4753 errors occurred among the studied patients. The most commonly used drugs were pantoprazole tablet, piracetam syrup, and losartan tablet. A total of 128 different types of drugs and nine different oral pharmaceutical preparations were prescribed for the patients. Forty-one (35.34%) out of 116 different solid drugs (except effervescent tablets and powders) could be substituted by liquid or injectable forms. The most common error was the wrong time of administration. Errors of wrong dose preparation and administration accounted for 24.04% and 25.31% of all errors, respectively.
Conclusion:
In this study, at least three-fourth of the patients experienced medication errors. The occurrence of these errors can greatly impair the quality of the patients’ pharmacotherapy, and more attention should be paid to this issue.
KEYWORDS: Intensive Care Unit, medication errors, pharmaceutical preparations
INTRODUCTION
Critically ill patients in Intensive Care Units (ICUs) receive more drugs compared to patients of other wards. Thus, rates of medication errors are higher in these patients.[1] Most patients admitted to ICU have problems in using oral medication or ingesting solid forms of drugs.[2] Several medication errors can occur during enterally drug administration, including errors in dosage form selection, methods of oral medication administration, drug interactions, and incompatibility with nutrition formula.[3] Although enteral feeding tubes are not suitable for administration of oral drugs, receiving crushed tablets is common through these tubes and can result in tube obstruction, an increase in adverse drug reactions, reduction in drug effectiveness, or drug-enteral nutrition (EN) incompatibility. Crushing many drugs such as enteric coated tablets, controlled-release tablets, and mutagenic and teratogenic drugs can lead to a decrease in drugs effects, irritation of gastric mucosa, and harm to the nurse.[4] Selection of the most suitable dosage form in such patients is a challenge. Liquid dosage forms are the best choices if possible because of easy absorption and no tube obstruction.[5] Sometimes, other routes of administration exist for a drug and can be used as an alternative to solid forms.[6] However, the challenging issue is that there is no liquid or injection substitution for many of drugs, and the only solution is using mortar and pestle for crushing tablets or opening capsules which can alter pharmacokinetic profile of the drug.[7]
The aim of our study was to assess the frequency and types of errors of oral medication administration in patients with enteral feeding tubes or suffering from dysphagia who were admitted to the General ICU in Shahid Sadoughi Hospital (Yazd, Iran).
METHODS
A cross-sectional study was performed in the 16-bed ICU of the largest teaching hospital in Yazd, Iran, from January 2016 to April 2016. The study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences. ICU was selected because of high numbers of patients who cannot use solid forms of drugs or use EN. All patients with swallowing problems or feeding through nasogastric (NG) tube who were administered at least one oral drug were eligible to be enrolled in this study. All drugs were prepared and administered by nursing staff, and pharmacists had no intervention in this process. Nurses were not aware of the study's purpose and reason of pharmacist attendance as an observer. The needed information were collected including patient's age and gender, nurse's gender, type of disease, the length of hospital stay, number and frequency of oral drugs administered by enteral tube, and concomitant intravenous medications. Observations were performed during all work shifts and holidays. Oral pharmaceutical preparations that should not be crushed or administered through an enteral feeding tube were identified from the recommendations of the manufacturers and by reviewing articles and relevant references.[8] Furthermore, the availability of liquid formulation for each drug was assessed to know if liquid substitutions for the solid dosage forms exist.
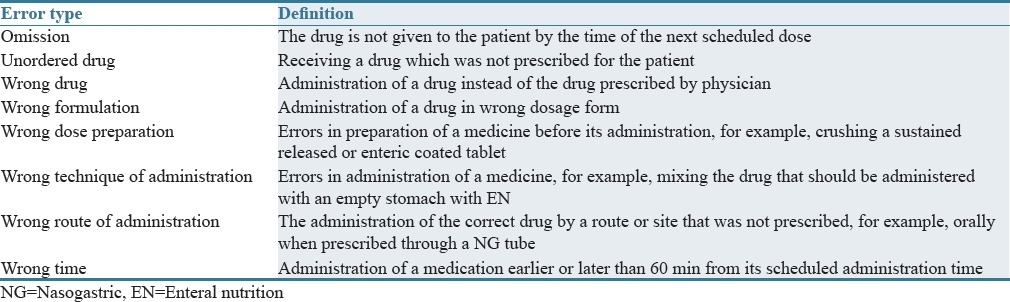
Then, the errors of drug administration through enteral tubes were evaluated and classified according to Table 1.[9] The data were analyzed using SPSS, V 16 (SPSS Inc., Chicago, IL, USA). The results were analyzed using descriptive statistics (frequency and percentage) and inferential statistics (Fisher's exact test and ANOVA). P< 0.05 was considered statistically significant.
Table 1.
Definition of errors
RESULTS
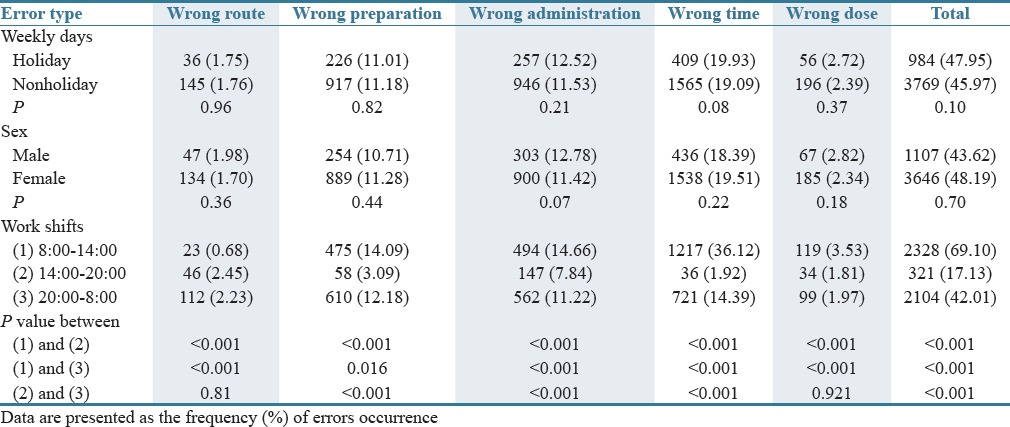
During the study period, a total of 94 patients with a mean ± standard deviation (SD) age of 58 ± 28.5 years (ranging from 2 months to 92 years) were evaluated. The main diagnoses were: cerebral (35.29%), respiratory (16.66%), and cardiovascular diseases (8.82%). The length of ICU stay varied from 2 to 57 days, with a mean ± SD of 11.6 ± 11 days. The length of tube feeding or having swallowing difficulty varied from 1 to 55 days, with a mean of 10.7 ± 10.49 days. Totally, 10,250 administrations were observed during the study period. The average of drug administration for every patient was 109.04 (from 2 to 832). Moreover, 128 different types of drugs were prescribed for the patients. Five of the most commonly used oral drugs during the study period were pantoprazole tablet, piracetam syrup, losartan tablet, lactulose syrup, and L-carnitine syrup. On average, every patient received 13.84 types of drugs, 5.84 types of oral drugs, and 4.7 types of solid drugs. Nine different oral pharmaceutical preparations were used, including tablets (51%), syrups (19%), coated tablets (11%), capsules (5%), oral suspensions (4%), effervescent tablets (3%), powders (3%), oral drops (3%), and oral solutions. In addition, 41 (35.34%) out of 116 different solid drugs (except effervescent tablets and powders) could be substituted by liquid or injectable forms. Preparation and administration errors occurred in 34 types of drugs while 76.59% of patients (72 patients) experienced these errors during their hospital stay. The most common error was the time error which included 19.25% of all administrations [Table 2]. The frequencies of wrong dose preparation and administration errors were about 11.15% and 11.73% of administrations, respectively. No omission, unordered drug, and wrong drug error was observed. The frequency of errors regarding the different work shifts, holiday and nonholiday shifts, and nurses’ gender are shown in Table 3. The differences reached statistical significance just for work shifts.
Table 2.
The twenty oral drugs most frequently prescribed which are non-crushable or can interact with enteral nutrition[6,8,11]
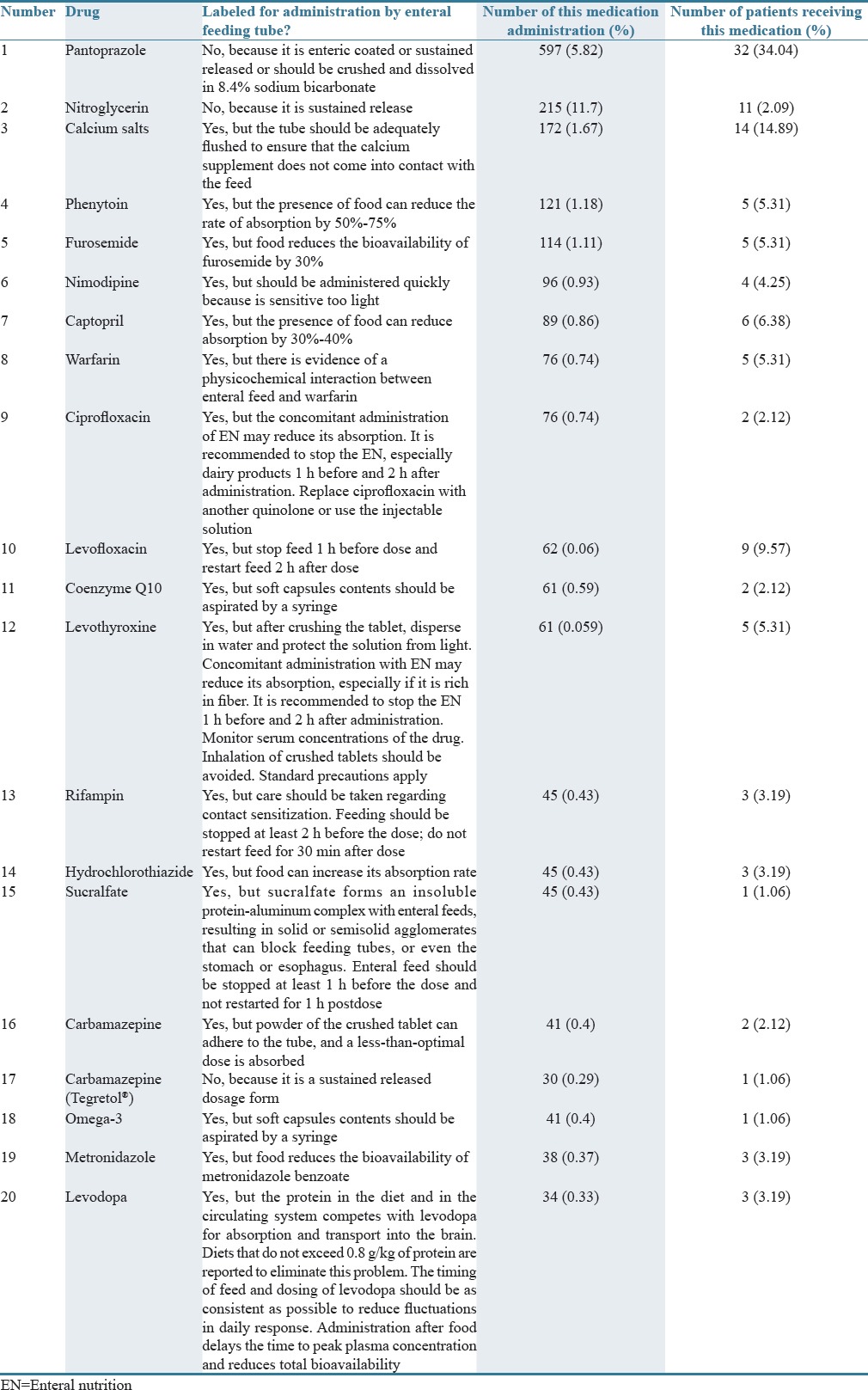
Table 3.
Correlation between the nurses’ demographic data and work shifts with the frequency of errors occurrence
DISCUSSION
In our study, it was found that most of the drugs were administered in solid dosage forms, and nearly 36% of them could be substituted by injection or oral liquid formulations. A study conducted by Barbosa et al. reported that 72.7% of studied cases were also receiving intravenous medications, and it was possible that some of the drugs could be substituted by intravenous formulations.[6] Silva et al. reached the conclusion that among 49 drugs prescribed in solid oral pharmaceutical forms, 17 (34.7%) were also available in oral liquid form, implying that at least 290 prescriptions (21.8%) could have reduced the risk of catheter obstruction.[10]
Among the administered medicines, pantoprazole was the most frequently prescribed and had the highest percent of wrong dose preparation. Pantoprazole is sensitive to gastric acid; therefore, crushing tablets and administering the pieces through NG tube have the possibility of degradation and therefore a decreased efficacy.[3] Our results are different from those of Barbosa et al., Presoti et al., and Silva et al. They reported that the most frequently used drug was captopril.[6,10,11] It seems that in these studies, proton-pump inhibitors are mostly used in their liquid dosage form (injectable dosage forms or oral suspensions), while in our country, oral suspension does not exist and only pantoprazole is used in injectable dosage form which is much more expensive compared to its oral dosage forms and its use is not cost-effective for hospitals.
Digoxin and phenytoin were administrated for 6.38% and 5.31% of patients. In another similar study conducted at a university hospital in Southern Brazil, the frequency of administrations of these two drugs was 9.8% and 6.3%, respectively.[12] These drugs, especially phenytoin, need exclusive care for administration. Enteral feeding can decrease phenytoin absorption and hence reduce its serum concentrations.[13] It is suggested that the serum concentrations of drugs with narrow therapeutic indices should be monitored regularly, especially when they are administered through a feeding tube.[8]
Crushing sodium valproate enteric coated tablets is considered as an error in some studies because valproate is irritant for gastric mucosa and can cause nausea and vomiting. Therefore, its tablets should not be crushed for use through NG tube.[3] We can use sodium valproate syrup instead of crushing tablets; however, using syrup will not solve the problem of nausea and vomiting. Thus, we did not consider crushing sodium valproate enteric coated tablets as an error in this study. For extended released products, it is recommended that doses be 8%–20% higher than non- extended release (ER) products; therefore, crushing them leads to a sudden release of high doses of valproate which can produce higher serum concentrations and effects than expected.[14]
Considering the work shifts, our data showed that the rate of medical errors was so high at 8:00 a.m. Furthermore, most of the administrations occurred in this work shift (nearly 23%). The high number of administrations and changes in the nurses’ shifts at this time plays an important role in errors occurrence. Indeed, 8:00 a.m. is the pick time for nursing distractions and lack of concentration due to telephone calls, educational rounds, physicians’ visits, higher nurse workloads, ordering necessary drugs to pharmacy center, and drug distribution from there leading to increased risk of errors.[15,16]
According to the UK standards for ICUs, a minimum nurse/patient ratio of 1:1 together with additional nurses according to patient needs, training requirements, the total number of beds, and the geographical arrangements within the unit should exist. Nonetheless, in this ward, every nurse is responsible for two patients and nursing workload is high. Thus, this ICU is particularly prone to medical errors and one solution for this problem is to employ more nurses.
In this ICU, medication preparation and administration are carried out by nurses and each nurse does it on the basis of their experience, habit, and personal information, not according to standard protocols. Unfortunately, no standard protocol was defined in this ICU. In-hospital education of nurses by clinical pharmacists can significantly increase their knowledge and profession in the aspects of medication preparation, tube flushing, recognizing drug-drug or drug-feed interactions, and recognizing dosage forms characteristics.[17] Pharmacists can help treatment team by providing useful information on selecting the correct drug, dosage form, and route of administration. Moreover, pharmacists are able to decrease some drug-drug interactions by administrating them separated by an appropriate time interval (generally 2–4 h).[18]
It is suggested that a routine checklist must be followed including: (1) never add medications directly to the enteral formula, (2) clean the enteral tube by flushing water under pressure, and (3) observe the patient for unexpected changes in clinical response and evolution.[12]
It was observed that most of the time all the drugs administered at the same time were crushed and mixed together which is completely wrong. Drugs should not be mixed together for administration through NG tube and each drug should be administrated separately; otherwise, physical and chemical incompatibility, tube occlusion, or changes in drug pharmacodynamics will possibly occur.[19]
Our study indicated that the frequency of drug administration and preparation errors in patients who cannot use solid forms of drugs in this ICU was high. Close cooperation between medical teams including pharmacists or pharmacotherapists, physicians, and nurses can result in administration of drugs through enteral catheters correctly.[17]
AUTHORS’ CONTRIBUTION
Dr. Seyed Mojtaba Sohrevardi contributed in study design and revising manuscript. Dr. Mohammad Hossein Jarahzadeh contributed as the head of the ICU and treating physician. Mahtabalsadat Mirjalili contributed in data gathering, manuscript writing and data analysis. Dr. Ehsan Mirzaei contributed in study idea and data gathering. Arefeh Dehghani Tafti contributed in data analysis. Dr. Behrooz Heydari contributed as scientific advisor and has revised the manuscript critically.
Financial support and sponsorship
The present article was extracted from the thesis written by Dr. Maryam Foroozmehr and was financially supported by SUMS (grant number: 93/1168).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the staff of Shahid Sadoughi Hospital (Yazd, Iran) for their support in collecting data. This article is extracted from a pharmacy student thesis.
REFERENCES
- 1.Papadopoulos J, Smithburger PL. Common drug interactions leading to adverse drug events in the Intensive Care Unit: Management and pharmacokinetic considerations. Crit Care Med. 2010;38(6 Suppl):S126–35. doi: 10.1097/CCM.0b013e3181de0acf. [DOI] [PubMed] [Google Scholar]
- 2.Cornish P. “Avoid the crush”: Hazards of medication administration in patients with dysphagia or a feeding tube. CMAJ. 2005;172:871–2. doi: 10.1503/cmaj.050176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emami S, Hamishehkar H, Mahmoodpoor A, Mashayekhi S, Asgharian P. Errors of oral medication administration in a patient with enteral feeding tube. J Res Pharm Pract. 2012;1:37–40. doi: 10.4103/2279-042X.99677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van den Bemt PM, Cusell MB, Overbeeke PW, Trommelen M, van Dooren D, Ophorst WR, et al. Quality improvement of oral medication administration in patients with enteral feeding tubes. Qual Saf Health Care. 2006;15:44–7. doi: 10.1136/qshc.2004.013524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomson F, Naysmith M, Lindsay A. Managing drug therapy in patients receiving enteral and parenteral nutrition. Hosp Pharm. 2000;7:164–6. [Google Scholar]
- 6.Barbosa AP, de Paula SL, Barbosa DS, da Cunha DF. Oral drug administration by enteral tube in adults at a tertiary teaching hospital. E SPEN J. 2012;7:e241–4. [Google Scholar]
- 7.Salmon D, Pont E, Chevallard H, Diouf E, Tall ML, Pivot C, et al. Pharmaceutical and safety considerations of tablet crushing in patients undergoing enteral intubation. Int J Pharm. 2013;443:146–53. doi: 10.1016/j.ijpharm.2012.12.038. [DOI] [PubMed] [Google Scholar]
- 8.White R, Bradnam V. Handbook of Drug Administration Via Enteral Feeding Tubes. London: Pharmaceutical Press; 2015. [Google Scholar]
- 9.Kelly J, Wright D, Wood J. Medicine administration errors in patients with dysphagia in secondary care: A multi-centre observational study. J Adv Nurs. 2011;67:2615–27. doi: 10.1111/j.1365-2648.2011.05700.x. [DOI] [PubMed] [Google Scholar]
- 10.Silva MJ, Cava CE, Pedroso PK, Futuro DO. Evaluation of the profile of drug therapy administered through enteral feeding tube in a general hospital in Rio de Janeiro. Braz J Pharm Sci. 2011;47:331–7. [Google Scholar]
- 11.Presoti AR, do Nascimento MM, Marques LA. Prescription of drugs to be administered through feeding tubes in a Brazilian hospital: Profile and qualification. J Gen Pract. 2013;1:112. [Google Scholar]
- 12.Heineck I, Bueno D, Heydrich J. Study on the use of drugs in patients with enteral feeding tubes. Pharm World Sci. 2009;31:145–8. doi: 10.1007/s11096-008-9268-6. [DOI] [PubMed] [Google Scholar]
- 13.Bauer LA. Interference of oral phenytoin absorption by continuous nasogastric feedings. Neurology. 1982;32:570–2. doi: 10.1212/wnl.32.5.570. [DOI] [PubMed] [Google Scholar]
- 14.McAuley JW, Lott RS, Alldredge BK. Seizure disorders. In: Alldredge BK, Corelli RL, Ernst ME, Guglielmo BJ, Jacobson PA, Koda-Kimble MA, et al., editors. Applied Therapeutics: The Clinical use of Drugs. Philadelphia, PA: Wolters Kluwer/Lipincot William and Wilkins; 2013. pp. 1387–418. [Google Scholar]
- 15.Tang FI, Sheu SJ, Yu S, Wei IL, Chen CH. Nurses relate the contributing factors involved in medication errors. J Clin Nurs. 2007;16:447–57. doi: 10.1111/j.1365-2702.2005.01540.x. [DOI] [PubMed] [Google Scholar]
- 16.Fahimi F, Ariapanah P, Faizi M, Shafaghi B, Namdar R, Ardakani MT. Errors in preparation and administration of intravenous medications in the intensive care unit of a teaching hospital: An observational study. Aust Crit Care. 2008;21:110–6. doi: 10.1016/j.aucc.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Dashti-Khavidaki S, Badri S, Eftekharzadeh SZ, Keshtkar A, Khalili H. The role of clinical pharmacist to improve medication administration through enteral feeding tubes by nurses. Int J Clin Pharm. 2012;34:757–64. doi: 10.1007/s11096-012-9673-8. [DOI] [PubMed] [Google Scholar]
- 18.Abbasinazari M, Zareh-Toranposhti S, Hassani A, Sistanizad M, Azizian H, Panahi Y. The effect of information provision on reduction of errors in intravenous drug preparation and administration by nurses in ICU and surgical wards. Acta Med Iran. 2012;50:771–7. [PubMed] [Google Scholar]
- 19.Bankhead R, Boullata J, Brantley S, Corkins M, Guenter P, Krenitsky J, et al. Enteral nutrition practice recommendations. J Parenter Enteral Nutr. 2009;33:122–67. doi: 10.1177/0148607108330314. [DOI] [PubMed] [Google Scholar]


