Abstract
Objective:
Antimicrobial prophylaxis has been demonstrated to lower the incidence of postoperative infection in nearly all types of surgery. The American Society of Health-System Pharmacists (ASHP) guideline summarizes current data on the appropriate use of antibiotic for surgical prophylaxis. The objective of this study was to assess and audit the use of antibiotics in a tertiary care center according to the recommendation of ASHP guideline.
Methods:
This cross-sectional study was performed using prospective data gathered from April to September 2015 in the surgical wards of Al Zahra Hospital, Isfahan, Iran. Antibiotic indication and choice, dose, dosing interval, route of administration, and timing of first administration and duration of prophylaxis were compared with the ASHP guideline recommendations.
Findings:
A total of 100 patients with the mean age of 49.8 ± 18.2 years were recruited for this study. About 22% of procedures had full compliance with all guideline recommendations. The most frequently encounter noncompliance type were the duration of prophylaxis (14%) and appropriate agent choice (35%). Timing of the initial dose was appropriate in most of the procedures (42%).
Conclusion:
This study revealed that most of the prescribed antibiotics for surgical prophylaxis are not in accordance with standard treatment guideline. The density of antimicrobial use for preoperative antimicrobial prophylaxis is very high. Furthermore, the hospital should develop a formal strategy, including a local guideline for antimicrobial prophylaxis in surgical procedures.
KEYWORDS: Antibiotic prophylaxis, guideline adherence, surgery
INTRODUCTION
The utilization of antimicrobial prophylaxis for chose surgical methodology is one of the measures used to keep the improvement of a surgical site infection (SSI).[1] SSIs altogether increment the length of hospital stay, morbidity, and mortality and along these lines deplete medicinal services framework assets.[2] Proper utilization of anti-infection agents can decrease the occurrence of SSI,[3] and the unsuitable use of antibiotics for prophylaxis increased drug toxicity and the emergence of antibiotic-resistant bacteria.[3]
In spite of the accessibility of universal and national rules for surgical prophylaxis, recent studies surveying the present routine of prophylaxis have demonstrated that overutilization of antimicrobial medications, unnecessary utilization of wide range antibacterial and wrong planning and span are still hazardous.[4,5,6,7,8,9,10] Although a few studies have reported abuse of anti-infection agents in Iranian healing facilities, there are insufficient studies about the quality and of surgical prophylaxis in Iran.[5,11,12,13,14,15] In this study, we used the guidelines of the American Society of Health-System Pharmacists (ASHP)[16] to assess the appropriateness of antibiotic prophylaxis for surgical procedures in the large teaching hospital affiliated with Isfahan University of Medical Sciences (IUMS) in Isfahan, Iran.
METHODS
A prospective audit was undertaken between April and September 2015 in “Alzahra” teaching hospital, Isfahan, Iran, which is a tertiary referral hospital with 850 beds. Services cover all the major specialties, including general medicine, surgery, obstetrics and gynecology, urology, psychiatry and orthopedics except of pediatrics. The Ethic Committee of IUMS approved the study protocol. All patients aged ≥18 years admitted for elective surgery were recruited during the study.
Data were collected prospectively from PATIENT’S chart and entered on the data collection forms. The following information was noted: patient demographic information, ward, type of surgery, wound class, antibiotic therapy received (agents, doses, dose intervals, and route of administration, the number of doses, initiation times, and duration of administration), outcome of prophylaxis and outcome of patients. Compliance with recommendations of ASHP guidelines was assessed for every aspect of antibiotic prophylaxis. Patients who received antibiotic treatment for infections were excluded, as were patients for whom it was not possible to determine whether the antibiotic was given as treatment or prophylaxis.
The American College of Surgeons determines four classes of surgical wound types based on the wound's level of contamination: clean, clean-contaminated, contaminated, and dirty-infected.[16] We determined type of wound based on the performed procedure.
The first criterion evaluated was preoperative antibiotic prophylaxis indication; if this criterion was assessed as inappropriate, the other criteria also considered as inappropriate. Antibiotic prophylaxis remedies considered as wrong if any of the surveyed criteria inappropriate (i.e., “inappropriate” indication or choice).
Each record's parameters were evaluated against following criteria: Indication for prophylaxis: according to ASHP guideline recommendations; choice of antibiotics: According to the ASHP guideline recommendations; time of administration of first preoperative dose(s): Proper-if given within 30–60 min before incision; duration of prophylaxis; dose and route of administration.
For patients who developed a wound infection during admission, only antibiotics prescribed before the onset of infection were enlisted; this was performed to separate prophylactic and treatment courses.
All statistical analyses were performed using SPSS version 20 (SPSS Inc., Chicago, IL, USA). Frequency and percentage were calculated and presented.
RESULTS
A total of 100 patients reviewed in this study (mean age 46.8 ± 18.2; male: 62). Patients ranged in age from 18 to 86 years. The types of surgery were as follows: Thorax (24%), general surgery (19%), orthopedic (18%) vascular surgery (14%), plastic surgery (13%), obstetrics-gynecologic (6%), and neurosurgical (6%). The most performed procedures are as follows: Thoracotomy (n = 7), rhinoplasty (n = 5) cholecystectomy (n = 4), femoral and hip fixation (n = 4) Endoscopic retrograde cholangiopancreatography (n = 3), dilation and curettage (n = 3), cesarean (n = 3), and open reduction internal fixation (n = 3). All of the reviewed procedures were elective. Most of the surgical wounds were clean (74%), or clean-contaminated (21%), and 5% were contaminated. Table 1 shows the proportion of procedures in which the antibiotic therapy prescribed agreed with the ASHP guideline recommendation for indications and regimens of antibiotic prophylaxis.
Table 1.
Compliance with the American Society of Health-System Pharmacists’ therapeutic guidelines on antimicrobial prophylaxis in surgery (n =100)
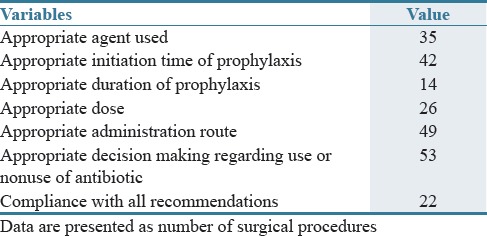
We found that antibiotic(s) were administered inappropriately for 47 procedures for which antibiotic prophylaxis was not indicated. The antibiotic used most frequently were cefazolin (in 66 procedures, 66%), metronidazole (in 18), ceftizoxime (in 14), clindamycin (in 13), ceftriaxone (in 11), vancomycin (in 10), and ceftazidime (in 9). Cefazolin was appropriately prescribed in 31 procedures. A total of 792 g of cefazolin was used for patients.
Of 36% of patients for whom a single antibiotic was indicated, 10% received two or more antibiotics. All the administration was consistent with the guideline recommendation in 35 procedures. The dose and dosing interval were appropriate for 43% of procedures. All the antibiotics were administered intravenously.
For 42 patients from 100 patients, antibiotic prophylaxis was started 30–60 min before induction of anesthesia. For five patients, prophylaxis was started >2 h after induction of anesthesia. The surgery duration was >3 h in nine patients; only two of them received an additional dose of antibiotic (cefazolin) during surgery.
The duration of prophylaxis was consistent with the guideline recommendation for 14 patients. The mean duration of prophylaxis for the remaining 37 patients was 6.7 ± 5.9 days (range, 2–25 days). For 27 of these patients, the duration of prophylaxis was >72 h. The mean length of hospital stay was 6.1 ± 5.9 (range, 1–32 days).
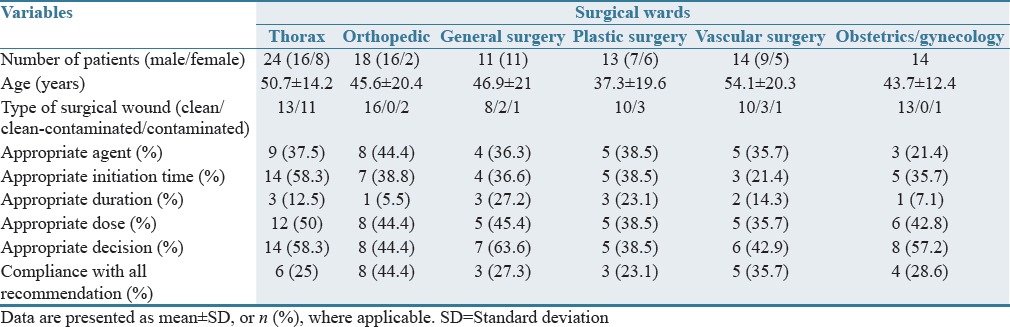
All of our patients stay alive and discharged from the hospital. Infection developed in eight of these patients despite the use of antibiotics for surgical prophylaxis. From these, only one patient received appropriate prophylaxis. Table 2 shows the patient characteristics and adherence to ASHP guideline recommendations in different surgical wards in our hospital. Different surgical wards had the most compliance with the guideline at the appropriate initiation time of prophylaxis and the least compliance with appropriate duration of prophylaxis. Orthopedic surgeons followed by vascular surgeon had the most overall compliance with all guideline recommendations (>90%).
Table 2.
Results of preoperative antimicrobial prophylaxis in different surgical wards
DISCUSSION
The results of this study demonstrate that about all of the patients got anti-microbial for surgical prophylaxis regarding the sort of surgical intercession. General consistency with the assessment criteria was accomplished in 22% of the procedures. These outcomes show that the surgical group knew about the estimation of antibiotics in counteracting SSI, additionally, exhibit a general absence of attention to international standards by human health care providers, and reflected the impact from an absence of clinical guidelines.
The ASHP recommends prophylaxis with cefazolin as first choice and single agent for most procedures (clean and clean-contaminated).[16] Only 35% of our patients received the appropriate agent; use of >1 drug without any indication for multidrug prophylaxis, and use of antibiotics not recommended for prophylaxis, such as third-generation cephalosporins, are the most common errors in antibiotic selection. This misuse and overuse of antibiotics are associated with the emergence of bacterial resistance and increase in health-associated costs. Inappropriate selection of antibiotics for prophylaxis has been shown in some studies such as Sudan (56.3%),[6] Iran (54%).[13] On the other hand, antibiotic choice for prophylaxis has been better (regarding appropriateness) in studies from the United States (95% of courses were appropriate),[17] Brazil (75%),[18] and China (95%).[19]
For the greater part of patients, the duration of prophylaxis was extended beyond single doses. Other studies reported the same problem.[5,6,7,8,9,10,11] Extended use of prophylactic antimicrobials has been linked with the appearance of bacterial resistance, the risk of superinfection and drug toxicity.[20] Prophylaxis was started at the right time in most of our procedures. None of our patients developed an infection during hospitalization possibly because of continuing prophylaxis beyond the recommended duration. Therefore, we couldn’t judge about the outcome of preoperative antibiotic prophylaxis.
The rate of the wrong indication for antibiotics was high among the general surgery and obstetrics/gynecology discipline. The possible reasons behind the higher rate of improper antibiotic use in these wards include distinctive of surgical systems, complex surgical methods, and higher surgery rates. Proper pharmacists’ specialists alongside strict supervision over surgeons at local hospitals might be valuable and helpful in the pattern of proper antibiotic utilization.
Although antimicrobial prophylaxis can decrease the incidence of SSI, this benefit must weigh against the risks of adverse drug reactions, the emergence of resistant bacteria and the direct monetary cost.[21] One potential strategy to enhance antimicrobial practice in hospitals is institutionalization, either by receiving an international guideline or by developing a local hospital guideline. Institutionalization efforts should be administered by a board of trustees that incorporates specialists, anesthesiologist, microbiologists, pharmacists, and infection control departments. Guidelines should be based on the hospital's specific bacterial epidemiology patterns, the best literature evidence, and surgeon favorite. The standardized protocol should then be provided to surgeons, in an effort to achieve consensus, before execution. A few studies have demonstrated that guidelines can enhance the quality of antibiotic use. Currently, there are no national standard or guideline about the preoperative antimicrobial prophylaxis in Iran. At our study setting, neither guideline nor consensuses are available. The poor practice documented by the present study could be enhanced with effective interventions.
Our study had some limitations. First, the results do not include microbiology outcome parameters and process parameters. Second, in some cases, the timing of antibiotic administration had not documented in the patient's hospital file; third the cost-effectiveness and feasibility of ASHP guidelines in our region has not been documented. We choose ASHP as an available and international guideline.
This study revealed that most of the prescribed antibiotics for surgical prophylaxis are not in accordance with standard treatment guideline. A preface of local prescribing guideline together with proper educational interventions is required to improve the excellence of preoperative antibiotic use.
AUTHORS’ CONTRIBUTION
Sarah Mousavi designed the study, analyzed the data and drafted the manuscript. Elham Zamani collected and interpreted the data and Faranak Bahrami revised the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Korol E, Johnston K, Waser N, Sifakis F, Jafri HS, Lo M, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS One. 2013;8:e83743. doi: 10.1371/journal.pone.0083743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coomer NM, Kandilov AM. Impact of hospital-acquired conditions on financial liabilities for medicare patients. Am J Infect Control. 2016;44:1326–34. doi: 10.1016/j.ajic.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 3.Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35:605–27. doi: 10.1086/676022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Momany NH, Al-Bakri AG, Makahleh ZM, Wazaify MM. Adherence to international antimicrobial prophylaxis guidelines in cardiac surgery: A Jordanian study demonstrates need for quality improvement. J Manag Care Pharm. 2009;15:262–71. doi: 10.18553/jmcp.2009.15.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Askarian M, Reza Moravveji A, Assadian O. Prescription of prophylactic antibiotics for neurosurgical procedures in teaching hospitals in Iran. Am J Infect Control. 2007;35:260–2. doi: 10.1016/j.ajic.2006.04.214. [DOI] [PubMed] [Google Scholar]
- 6.Elbur AI, Yousif MA, Elsayed AS, Abdel-Rahman ME. An audit of prophylactic surgical antibiotic use in a Sudanese Teaching Hospital. Int J Clin Pharm. 2013;35:149–53. doi: 10.1007/s11096-012-9719-y. [DOI] [PubMed] [Google Scholar]
- 7.Goede WJ, Lovely JK, Thompson RL, Cima RR. Assessment of prophylactic antibiotic use in patients with surgical site infections. Hosp Pharm. 2013;48:560–7. doi: 10.1310/hpj4807-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hohmann C, Eickhoff C, Radziwill R, Schulz M. Adherence to guidelines for antibiotic prophylaxis in surgery patients in German hospitals: A multicentre evaluation involving pharmacy interns. Infection. 2012;40:131–7. doi: 10.1007/s15010-011-0204-7. [DOI] [PubMed] [Google Scholar]
- 9.Durando P, Bassetti M, Orengo G, Crimi P, Battistini A, Bellina D, et al. Adherence to international and national recommendations for the prevention of surgical site infections in Italy: Results from an observational prospective study in elective surgery. Am J Infect Control. 2012;40:969–72. doi: 10.1016/j.ajic.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Ng RS, Chong CP. Surgeons’ adherence to guidelines for surgical antimicrobial prophylaxis – A review. Australas Med J. 2012;5:534–40. doi: 10.4066/AMJ.2012.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Afhami SH, Boujar Arani N, Sayadi L. Antibiotic prophylaxis before surgeries. Iran Surg J. 2011;19:28–35. [Google Scholar]
- 12.Askarian M, McLaws ML, Meylan M. Knowledge, attitude, and practices related to standard precautions of surgeons and physicians in university-affiliated hospitals of Shiraz, Iran. Int J Infect Dis. 2007;11:213–9. doi: 10.1016/j.ijid.2006.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Askarian M, Moravveji AR, Mirkhani H, Namazi S, Weed H. Adherence to American Society of Health-System Pharmacists surgical antibiotic prophylaxis guidelines in Iran. Infect Control Hosp Epidemiol. 2006;27:876–8. doi: 10.1086/506405. [DOI] [PubMed] [Google Scholar]
- 14.Mahdaviazad H, Masoompour SM, Askarian M. Iranian surgeons’ compliance with the American Society of Health-System Pharmacists guidelines: Antibiotic prophylaxis in private versus teaching hospitals in Shiraz, Iran. J Infect Public Health. 2011;4:253–9. doi: 10.1016/j.jiph.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Vessal G, Namazi S, Davarpanah MA, Foroughinia F. Evaluation of prophylactic antibiotic administration at the surgical ward of a major referral hospital, Islamic Republic of Iran. East Mediterr Health J. 2011;17:663–8. [PubMed] [Google Scholar]
- 16.Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195–283. doi: 10.2146/ajhp120568. [DOI] [PubMed] [Google Scholar]
- 17.Vaisbrud V, Raveh D, Schlesinger Y, Yinnon AM. Surveillance of antimicrobial prophylaxis for surgical procedures. Infect Control Hosp Epidemiol. 1999;20:610–3. doi: 10.1086/501680. [DOI] [PubMed] [Google Scholar]
- 18.Heineck I, Ferreira MB, Schenkel EP. Prescribing practice for antibiotic prophylaxis for 3 commonly performed surgeries in a teaching hospital in Brazil. Am J Infect Control. 1999;27:296–300. doi: 10.1053/ic.1999.v27.a96193. [DOI] [PubMed] [Google Scholar]
- 19.Ou Y, Jing BQ, Guo FF, Zhao L, Xie Q, Fang YL, et al. Audits of the quality of perioperative antibiotic prophylaxis in Shandong Province, China, 2006 to 2011. Am J Infect Control. 2014;42:516–20. doi: 10.1016/j.ajic.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Schonberger RB, Barash PG, Lagasse RS. The surgical care improvement project antibiotic guidelines: Should we expect more than good intentions? Anesth Analg. 2015;121:397–403. doi: 10.1213/ANE.0000000000000735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wick EC, Hobson DB, Bennett JL, Demski R, Maragakis L, Gearhart SL, et al. Implementation of a surgical comprehensive unit-based safety program to reduce surgical site infections. J Am Coll Surg. 2012;215:193–200. doi: 10.1016/j.jamcollsurg.2012.03.017. [DOI] [PubMed] [Google Scholar]


