Abstract
Objective:
Studies have demonstrated the direct relation between elevation in cardiac necrosis markers and increased risk of cardiovascular complications after percutaneous coronary intervention (PCI) in chronic kidney disease (CKD) patients. In this study, we sought to evaluate the effect of omega-3 on creatine kinase-MB (CK-MB) and troponin-I in CKD patients undergoing elective PCI.
Methods:
Eighty CKD patients, candidate for elective PCI, were randomly assigned into two groups: Group A – receiving omega-3 (2.5 g, 12 h before PCI) plus standard treatment (n = 37) and Group B – control group, receiving only standard therapy (aspirin 325 mg and clopidogrel 600 mg loading dose and weight-adjusted intravenous heparin) (n = 43). Blood samples were collected before and 24 h after PCI for measuring CK-MB and troponin-I. The primary endpoint was considered to be postprocedural variations of CK-MB and troponin-I levels in both groups. The secondary endpoint was the percentage of pre-procedural myocardial infarction (PMI) occurrence, defined as the elevation of post-PCI troponin-I, between study groups.
Findings:
Both the baseline and 24-h CK-MB were significantly higher in omega-3 group. Although 24-h troponin-I increased less in omega-3-treated arm compared to the control group, no statistically significant variation was observed between the two groups. With regard to PMI occurrence, no significant difference was detected among study groups.
Conclusion:
Despite the beneficial but nonsignificant effects of omega-3 on decreasing post-PCI elevation of troponin-I and PMI occurrence, further investigations with bigger study population, higher doses of omega-3 and longer duration of treatment, and long-term follow-up of patients are required to better test the potential effects of omega-3 in improving clinical outcomes in CKD patients undergoing PCI.
KEYWORDS: Chronic kidney disease, creatine kinase-MB, omega-3 fatty acids, percutaneous coronary intervention, preprocedural myocardial infarction, troponin-I
INTRODUCTION
Patients with chronic kidney disease (CKD) are more likely to develop cardiac diseases. Importantly, not only these patients are more susceptible to cardiac diseases but also they are more vulnerable to face with more severe cardiac complications. Meanwhile, coronary artery disease is the main cause of death in these patients, and it is estimated that 1-year mortality in CKD patients after myocardial infarction can get up to 59%.[1,2] Furthermore, in several recent studies, it has been shown that patients with CKD undergoing percutaneous coronary intervention (PCI) are also more prone to various post-PCI adverse effects such as unsuccessful intervention, increase in hospitalization time, higher rates of clinical and angiographic restenosis, more elevation in post-PCI cardiac biomarkers, and mortality, compared to non-CKD patients.[3,4] Recent investigations have demonstrated that elevation of cardiac necrosis markers, creatine kinase-MB (CK-MB), and troponin-I, after PCI is directly associated with short-, intermediate-, and long-term adverse outcomes, remarkably mortality after PCI.[5,6] Therefore, American College of Cardiology/American Heart Association (AHA) guidelines now recommend routine measurement of CK-MB and troponin, 8–12 h after PCI in all patients regardless of symptoms, for prognostic evaluation (Class 2A recommendation).[7]
It has been revealed that inadequate platelet inhibition at the time of PCI is associated with a higher risk of recurrent ischemic events after PCI; as a result, antiplatelet therapies have been introduced as a main treatment option before and after PCI.[8] Regarding the beneficial cardiac effects of omega-3 polyunsaturated fatty acids (PUFAs) as an antiplatelet agent and its improving effect on aspirin responsiveness, we as well as Gajos et al. previously investigated the effect of omega-3 on cardiac necrosis markers in patients with normal kidney function undergoing elective PCI.[9,10] In our previous study, it has been revealed that pretreatment with a loading dose of omega-3 could significantly decrease CK-MB elevation after PCI.[9] Therefore, in this study, we aimed to evaluate the effect of omega-3 on post-PCI cardiac necrosis markers, CK-MB, and troponin-I in patients with CKD. To the depth of our knowledge and available databases, this trial is the first one in evaluating the effect of omega-3 in CKD patients in this setting.
METHODS
This is a prospective and randomized clinical trial conducted in cardiac catheterization laboratory of two tertiary care centers affiliated to Shiraz University of Medical Sciences (SUMS), Shiraz, Iran. The study was carried out from January 2015 to January 2016 and was approved by the Ethical Committee of SUMS. The identifier code of Iranian Registry of Clinical Trials (IRCT) is IRCT2015040920441N2. As to the ethics, informed consent was obtained from all patients enrolled in the study.
Eighty patients admitted to two cardiac hospitals of SUMS for elective PCI were enrolled in the study. Inclusion criteria were the age range of 15–80 years, non-ST elevation acute coronary syndrome, candidates for elective PCI, treatment with aspirin at least 5 days preceding PCI, and estimated glomerular filtration rate (eGFR) between 30 and 60 cc/min. Exclusion criteria were cardiac bypass surgery in the previous 3 months, administration of bivalirudin and glycoprotein IIb/IIIa inhibitors during PCI, presence of active bleeding, platelet count <70 × 109/L, allergy to aspirin or clopidogrel or omega-3 PUFAs, and unsatisfactory PCI.
eGFR was calculated using Cockcroft-Gault equation: GFR = (140 − age) × body weight (kg)/72 × plasma creatinine (mg/dl) (×0.85 for female). Preprocedural creatinine, obtained at the nearest time before the PCI, was used for calculating eGFR.
Interventions were carried out using the standard technique with performing drug-eluting stents for all patients. Eligible patients were randomly divided into two groups through simple randomization method. The control group received merely pre-PCI standard therapy while omega-3 group received standard therapy plus omega-3.
According to the institutional protocol, all patients were pretreated with oral aspirin (325 mg loading then 80 mg/day lifelong) and clopidogrel (600 mg loading then 75 mg/day for at least 1-year post-PCI). In addition, all patients received weight-adjusted intravenous unfractionated heparin with a target activated clotting time of 250–350 s before the intervention.
Omega-3 pearls (Super Natural®; NutraLab, Canada) containing polyunsaturated fatty acids of 600 mg eicosapentaenoic acid (EPA) and 300 mg docosahexaenoic acid (DHA) were used. For all patients in omega-3 group, 2.5 g of omega-3 (2 pearls containing 1200 mg EPA and 600 mg DHA) were used 12 h preceding the PCI.
Blood samples were collected before (baseline) and 24 h after PCI for measuring CK-MB and troponin-I. The primary endpoint of this investigation was considered to be postprocedural variations of CK-MB and troponin-I levels in both groups. The secondary endpoint was the percentage of pre-procedural myocardial infarction (PMI) occurrence, defined as the elevation of post-PCI troponin-I more than 3 times of upper limit normal, between study groups.
Statistical analysis was performed using Statistical Package for Social Sciences software version 21.0 (SPSS, Inc., Chicago, IL, USA). The Mann–Whitney U-test was applied for statistical analysis of cardiac necrosis markers. Differences in proportions were tested by the Chi-square when assumptions were met; if not, the Fisher's exact test was used (if >25% of the categories has expected frequencies <5). The results were expressed as median (interquartile range) or mean ± standard deviation (SD). P<0.05 was considered statistically significant.
RESULTS
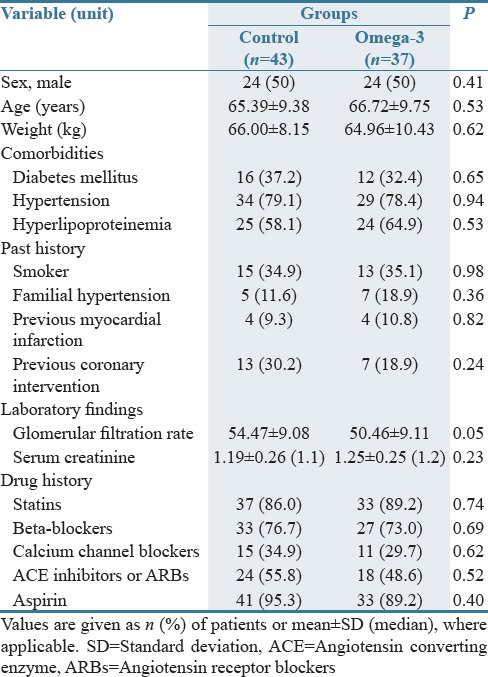
The CONSORT diagram of the clinical trial is showed in Figure 1. Thirty-seven participants were assigned in the omega-3 group and 43 participants in the control group. No statistically significant differences were observed between study groups with regard to basic clinical characteristics, medical and drug history. Patients’ demographic data are presented in Table 1.
Figure 1.
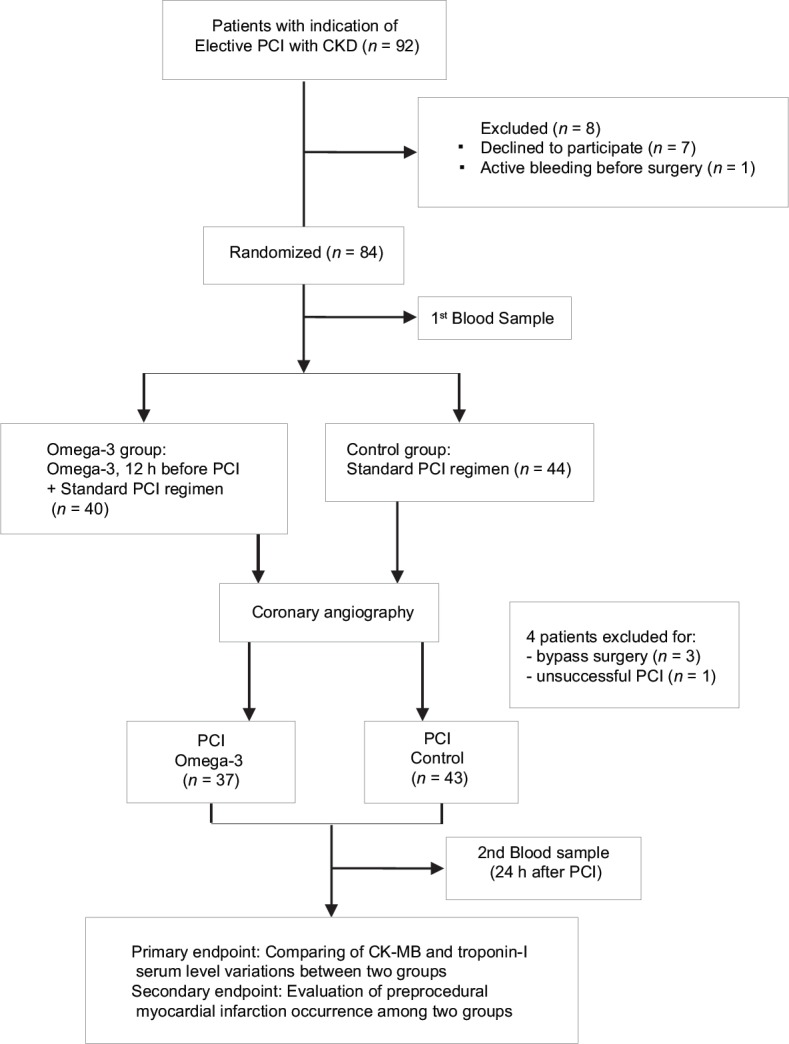
CONSORT flow diagram of the clinical trial
Table 1.
Demographic information and clinical features in the omega-3 and control groups
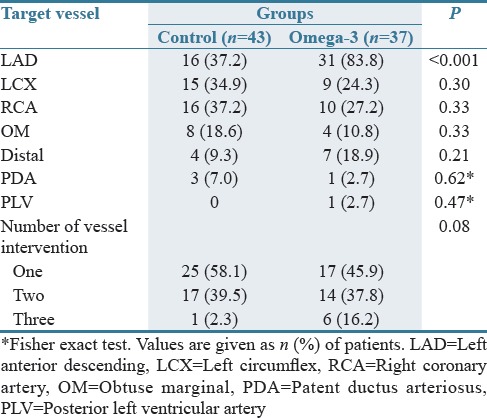
Procedural features with regard to the type and number of target vessels in the study groups are reported in Table 2. No statistically significant difference was seen between two groups except with left anterior descending (LAD) vessel distribution that was significantly more involved in omega-3 arm.
Table 2.
Type and number of vessels undergoing intervention in the omega-3 and control groups
The change in CK-MB and troponin-I in both groups is summarized in Table 3. CK-MB levels were reported as median (interquartile range). As shown, the baseline CK-MB was significantly higher in omega-3 group compared to control (P = 0.030). Although rising in 24-h CK-MB level was seen in both arms of the study, the CK-MB was also significantly higher in omega-3-treated patients after the procedure (P = 0.045). Comparing the differences between baseline and 24-h CK-MB between two groups, no significant difference was detected.
Table 3.
Creatine kinase-MB levels (U/L) and troponin-I levels (ng/mL) at baseline and 24 h after percutaneous coronary intervention in the omega-3 and control groups
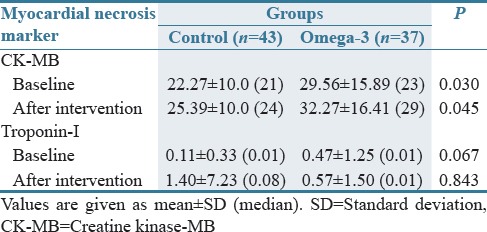
Results of troponin-I were presented as mean ± SD. No statistically significant variation was detected in baseline levels between both groups. Although 24-h troponin-I increased less in omega-3-treated arm compared to the control group, no statistically significant difference was revealed between groups.
Despite PMI was more occurred in control arm, no significant difference was detected between omega-3 (24.3%) and control (27.9%) groups with regard to the rate of PMI occurrence (P = 0.717).
By following patients for adverse effects of therapy, no major bleeding (e.g., gastrointestinal bleeding, intracranial hemorrhage) was observed in study groups.
DISCUSSION
This trial is a randomized trial evaluating the impact of pretreatment with a loading dose of omega-3 on myocardial necrosis markers, CK-MB, and troponin-I, in CKD patients undergoing elective PCI. Based on the available literature, no previous study has assessed the efficacy of omega-3 fatty acids on these biomarkers in CKD in this setting.
The main findings of this trial were as follows: (1) less increasing trend in the level of post-PCI troponin-I was seen in omega-3 group comparing control group; however, this difference could not reach the significance level; (2) statistically significant differences were detected with regard to both baseline and 24-h CK-MB among study groups. However, the difference between baseline and 24-h CK-MB was not significant between two groups; (3) PMI occurrence was not significantly different between two groups.
Recent investigations have demonstrated the direct association between elevation of cardiac necrosis markers, CK-MB, and troponin-I, and increased risk of major adverse cardiovascular events (MACE) such as MI, target vessel revascularization, and mortality.[5,11,12] It is also indicated that CK-MB and troponin-I levels are of importance in the evaluation of prognosis after PCI intervention.[13] It has been revealed that elevation in post-PCI levels of these markers is associated with short-, intermediate-, and long-term adverse outcomes following PCI.[5,6] In addition, several investigations have reported that CKD by itself is directly associated with increased risks of post-PCI adverse cardiac events and mortality.[14,15] Meanwhile, it has been revealed that troponin-I is a highly specific marker for myocardial damage in patients with CKD, unlike CK-MB which may also be elevated in the absence of myocardial injury in patients with CKD.[16]
In recent years, several trials have investigated different therapeutic strategies for preventing the rise in these cardiac markers after PCI and subsequent myocardial necrosis, mainly focusing on agents enhancing antiplatelet effect at the time of intervention.[17] Studies have shown the antiplatelet effect of omega-3 PUFAs when used alone[18] or in combination with aspirin.[19] In addition, the potential effect of omega-3 PUFAs in increasing platelet responsiveness to dual antiplatelet therapy (aspirin plus clopidogrel) has been previously reported in stable coronary artery disease patients undergoing PCI.[10] In our previous study investigating the effect of pretreatment with loading dose of omega-3 on cardiac necrosis markers (troponin-I and CK-MB) in normal kidney patients undergoing PCI, omega-3 could significantly decrease CK-MB elevation at both 8 and 24 h after PCI. Although less increasing trend in 24-h troponin-I was reported in omega-3 group, there was no statistically significant difference between omega-3 and control groups.[9] Our results were similar to the reports of this study with regard to troponin-I. In contrast, in this study, 24-h CK-MB was significantly higher in omega-3 arm compared to control group. Several factors may lead to this difference. One could be the significant higher baseline CK-MB in omega-3-treated patients. Therefore, to decrease the confounding effect of baseline CK-MB, differences between baseline and 24-h CK-MB were compared among two groups. However, no statistically significant difference was detected between study groups.
The elevated LAD involvement in omega-3 group could be another confounding factor which is a reflection of more severe atherosclerotic vessel involvement in this group. As a result, we reanalyzed the data separating those with LAD involvement from those without. However, no significant variation was detected in differences between pre- and post-PCI CK-MB in patients with LAD involvement among study groups. Furthermore, no difference was seen in those patients with or without LAD disease in omega-3 group. Therefore, after decreasing the confounding effects of higher baseline CK-MB and more LAD involvement in the intervention group, omega-3 was still unable to significantly decrease cardiac necrosis markers in CKD patients doing PCI.
In addition, one of the leading causes of PCI-attributable morbidity and mortality is myocardial necrosis and infarction defined as the elevation of cardiac biomarkers (CK-MB and troponin-I) between 1 and 3 times upper limit normal for myocardial necrosis and more than 3 times upper limit normal for myocardial infarction by AHA.[20] According to such definitions, there are various reports for the incidence of post-PCI myocardial damage in the literature ranging from 3.6% to 48.8%. Furthermore, this incidence was associated with a number of factors categorized as patient-, lesion-, and procedure-related factors.[21,22] According to the result of this study, 27.9% in control and 24.3% in omega-3 groups experienced PMI (based on troponin-I). Despite the lower prevalence of PMI in omega-3-treated patients, no statistically significant difference was seen among the study groups. Remarkably higher levels of pre-PCI CK-MB and higher involvement of LAD vessel in omega-3 arm may have contributed to this finding. Low sample size and using just 2.5 g single dose of omega-3 might have been the other reasons.
Our study has several limitations. First, a small number of patients were included in our study (due to financial shortage), which might have led to the insignificant effect of omega-3 on troponin-I. Second, it was not feasible to measure the baseline cardiac biomarkers during the study period; therefore, despite randomization, we are not able to distribute patients insignificantly with regard to these biomarkers between study groups. Third, we did not follow the patients for evaluating the long-term MACE as omega-3 may profit beneficial effect on long-term outcomes rather than in short terms such as PMI. Fourth, a single 2.5 g dose of omega-3 was used in this pilot study. Higher doses of omega-3 and longer duration of treatment may be more beneficial.
Despite the beneficial but nonsignificant effects of omega-3 on decreasing post-PCI elevation of troponin-I and PMI occurrence, further investigations with higher study population, higher doses of omega-3 and longer duration of treatment, and long-term follow-up of patients are required to better test the potential effects of omega-3 in improving the short- and long-term clinical outcomes in CKD patients undergoing PCI.
AUTHORS’ CONTRIBUTION
Farzaneh Foroughinia had contributed in concept/design, data analysis/interpretation, drafting article, critical revision of article, approval of article, statistics, funding secured by, and data collection. Maryam Foroozmehr had participated in concept/design, data analysis/interpretation, drafting article, approval of article, statistic, and data collection.
Financial support and sponsorship
The present article was extracted from the thesis written by Dr. Maryam Foroozmehr and was financially supported by SUMS (grant number: 93/1168).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Center for Development of Clinical Research of Nemazee Hospital for statistical analysis, Dr. Elham Nasiri for editorial assistance, and also personnels of Kowsar and Alzahra Hospitals.
REFERENCES
- 1.Coats WC, Dellsperger KC. Advances in percutaneous coronary intervention in patients with chronic kidney disease. Adv Perit Dial. 2010;26:42–6. [PubMed] [Google Scholar]
- 2.Edwards NC, Steeds RP, Ferro CJ, Townend JN. The treatment of coronary artery disease in patients with chronic kidney disease. QJM. 2006;99:723–36. doi: 10.1093/qjmed/hcl101. [DOI] [PubMed] [Google Scholar]
- 3.Gruberg L, Mehran R, Waksman R, Dangas G, Fuchs S, Wu H, et al. Creatine kinase-MB fraction elevation after percutaneous coronary intervention in patients with chronic renal failure. Am J Cardiol. 2001;87:1356–60. doi: 10.1016/s0002-9149(01)01552-1. [DOI] [PubMed] [Google Scholar]
- 4.Jeong YH, Hong MK, Lee CW, Park DW, Kim YH, Kim JJ, et al. Impact of significant chronic kidney disease on long-term clinical outcomes after drug-eluting stent versus bare metal stent implantation. Int J Cardiol. 2008;125:36–40. doi: 10.1016/j.ijcard.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 5.Selvanayagam JB, Porto I, Channon K, Petersen SE, Francis JM, Neubauer S, et al. Troponin elevation after percutaneous coronary intervention directly represents the extent of irreversible myocardial injury: Insights from cardiovascular magnetic resonance imaging. Circulation. 2005;111:1027–32. doi: 10.1161/01.CIR.0000156328.28485.AD. [DOI] [PubMed] [Google Scholar]
- 6.Brener SJ, Lytle BW, Schneider JP, Ellis SG, Topol EJ. Association between CK-MB elevation after percutaneous or surgical revascularization and three-year mortality. J Am Coll Cardiol. 2002;40:1961–7. doi: 10.1016/s0735-1097(02)02538-x. [DOI] [PubMed] [Google Scholar]
- 7.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, Jacobs AK, Kern MJ, King SB, 3rd, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention) J Am Coll Cardiol. 2006;47:e1–121. doi: 10.1016/j.jacc.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Wong YW, Prakash R, Chew DP. Antiplatelet therapy in percutaneous coronary intervention: Recent advances in oral antiplatelet agents. Curr Opin Cardiol. 2010;25:305–11. doi: 10.1097/HCO.0b013e328339f1aa. [DOI] [PubMed] [Google Scholar]
- 9.Foroughinia F, Salamzadeh J, Namazi MH. Protection from procedural myocardial injury by omega-3 polyunsaturated fatty acids (PUFAs): Is related with lower levels of creatine kinase-MB (CK-MB) and troponin I? Cardiovasc Ther. 2013;31:268–73. doi: 10.1111/1755-5922.12016. [DOI] [PubMed] [Google Scholar]
- 10.Gajos G, Rostoff P, Undas A, Piwowarska W. Effects of polyunsaturated omega-3 fatty acids on responsiveness to dual antiplatelet therapy in patients undergoing percutaneous coronary intervention: The OMEGA-PCI (OMEGA-3 fatty acids after pci to modify responsiveness to dual antiplatelet therapy) study. J Am Coll Cardiol. 2010;55:1671–8. doi: 10.1016/j.jacc.2009.11.080. [DOI] [PubMed] [Google Scholar]
- 11.Cavallini C, Savonitto S, Violini R, Arraiz G, Plebani M, Olivari Z, et al. Impact of the elevation of biochemical markers of myocardial damage on long-term mortality after percutaneous coronary intervention: Results of the CK-MB and PCI study. Eur Heart J. 2005;26:1494–8. doi: 10.1093/eurheartj/ehi173. [DOI] [PubMed] [Google Scholar]
- 12.Feldman DN, Kim L, Rene AG, Minutello RM, Bergman G, Wong SC. Prognostic value of cardiac troponin-I or troponin-T elevation following nonemergent percutaneous coronary intervention: A meta-analysis. Catheter Cardiovasc Interv. 2011;77:1020–30. doi: 10.1002/ccd.22962. [DOI] [PubMed] [Google Scholar]
- 13.Prasad A, Rihal CS, Lennon RJ, Singh M, Jaffe AS, Holmes DR., Jr Significance of periprocedural myonecrosis on outcomes after percutaneous coronary intervention: An analysis of preintervention and postintervention troponin T levels in 5487 patients. Circ Cardiovasc Interv. 2008;1:10–9. doi: 10.1161/CIRCINTERVENTIONS.108.765610. [DOI] [PubMed] [Google Scholar]
- 14.Szczech LA, Reddan DN, Owen WF, Califf R, Racz M, Jones RH, et al. Differential survival after coronary revascularization procedures among patients with renal insufficiency. Kidney Int. 2001;60:292–9. doi: 10.1046/j.1523-1755.2001.00799.x. [DOI] [PubMed] [Google Scholar]
- 15.Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation. 2002;106:2207–11. doi: 10.1161/01.cir.0000035248.71165.eb. [DOI] [PubMed] [Google Scholar]
- 16.Gruberg L, Fuchs S, Waksman R, Pichard AD, Kent KM, Laird JR, et al. Prognostic value of cardiac troponin I elevation after percutaneous coronary intervention in patients with chronic renal insufficiency: A 12-month outcome analysis. Catheter Cardiovasc Interv. 2002;55:174–9. doi: 10.1002/ccd.10081. [DOI] [PubMed] [Google Scholar]
- 17.Patti G, Colonna G, Pasceri V, Pepe LL, Montinaro A, Di Sciascio G. Randomized trial of high loading dose of clopidogrel for reduction of periprocedural myocardial infarction in patients undergoing coronary intervention: Results from the ARMYDA-2 (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2005;111:2099–106. doi: 10.1161/01.CIR.0000161383.06692.D4. [DOI] [PubMed] [Google Scholar]
- 18.Guillot N, Caillet E, Laville M, Calzada C, Lagarde M, Véricel E. Increasing intakes of the long-chain omega-3 docosahexaenoic acid: Effects on platelet functions and redox status in healthy men. FASEB J. 2009;23:2909–16. doi: 10.1096/fj.09-133421. [DOI] [PubMed] [Google Scholar]
- 19.Larson MK, Ashmore JH, Harris KA, Vogelaar JL, Pottala JV, Sprehe M, et al. Effects of omega-3 acid ethyl esters and aspirin, alone and in combination, on platelet function in healthy subjects. Thromb Haemost. 2008;100:634–41. [PubMed] [Google Scholar]
- 20.Thygesen K, Alpert JS, White HD. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–95. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Lansky AJ, Stone GW. Periprocedural myocardial infarction: Prevalence, prognosis, and prevention. Circ Cardiovasc Interv. 2010;3:602–10. doi: 10.1161/CIRCINTERVENTIONS.110.959080. [DOI] [PubMed] [Google Scholar]
- 22.Prasad A, Gersh BJ, Bertrand ME, Lincoff AM, Moses JW, Ohman EM, et al. Prognostic significance of periprocedural versus spontaneously occurring myocardial infarction after percutaneous coronary intervention in patients with acute coronary syndromes: An analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2009;54:477–86. doi: 10.1016/j.jacc.2009.03.063. [DOI] [PubMed] [Google Scholar]


