Abstract
Introduction:
The pain catastrophizing scale (PCS) is the most widely used tool to assess pain catastrophizing. The aim of this study was to translate, culturally adapt, and validate the PCS questionnaire in Arabic.
Methods:
A systematic translation process was used to translate the original English PCS into Arabic. After the pilot study, we validated our version among patients with chronic pain at two tertiary care centers. We tested the reliability of our version using internal consistency and test-retest reliability. We examined the validity by assessing construct validity, concurrent validity (by investigating the associations with Brief Pain Inventory [BPI]), and face validity.
Results:
A total of 113 subjects (50 men, 63 women) were included in the study. Cronbach's α was 0.94 (95% confidence interval [CI]: 0.92–0.96), and interclass correlation coefficients was 0.83 (95% CI: 0.77–0.89) for the total scale. There was no statistically significant difference in the total PCS scores between patients who reported experiencing current pain and those who did not. Among patients who reported having current pain, pain severity was weakly associated with the total PCS scores (r = 0.22, P = 0.03). PCS and its subscales were not statistically significantly associated with any of the BPI items. Nonetheless, patients who were diagnosed with neuropathic pain had statistically significantly higher scores on the total PCS, rumination, and helplessness subscales. Most patients found the PCS questions to be clear and easy to understand, and thought the questionnaire items covered all their problem areas regarding their pain catastrophizing.
Conclusion:
Our translated version of PCS is reliable and valid for use among Arabic-speaking patients.
Keywords: Anesthesia, Arabic, chronic pain, pain catastrophizing scale, reliability, validity
Introduction
Pain is one of the most common complaints in everyday clinical practice. As pain is a subjective symptom, the description of pain may vary across patients, which may result in large variations in self-report pain scores among patients suffering from similar ailments. As it is possible that patients who tend to catastrophize their pain are likely to report having more severe pain, the variability in pain scores may also be affected by patients’ tendency to catastrophize.[1]
Pain catastrophizing may be broadly defined as a cognitive process involving an exaggerated negative inclination towards pain experiences. Although there remains no consensus regarding the defining criteria of pain catastrophizing, investigators generally agree that pain catastrophizing may have a negative effect toward pain experience.[1] Three elements have been identified to be essential for the process of catastrophizing; magnification (exaggeration of the threatening properties of pain), rumination (inability to stop thinking about the pain), and helplessness (inability to do anything to influence pain). Nonetheless, which of these components is the primary element for pain catastrophizing remains debatable.[1]
From a clinical perspective, the pain catastrophizing scale (PCS) may help identify patients who are susceptible to heightened distress responses to aversive procedures, such as chemotherapy. Knowing individuals’ levels of catastrophizing may facilitate the application of interventions that aid in coping with or recovery from these procedures. For example, Heyneman et al.[2] suggested that strategies such as positive self-instruction are more likely to be effective in reducing distress than distraction strategies. However, tailoring pain management for chronic pain patients is even more difficult. Recent guidelines highlights the need to assess levels of pain catastrophizing when studying chronic postsurgical pain, among which the PCS is the most commonly used instrument to measure pain catastrophizing in chronic pain studies.[3]
Although the validity and reliability of PCS questionnaire has been evaluated in many studies and it has been translated into many languages across the world, an Arabic translation of the PCS is not available. The aim of this study is to translate, culturally adapt, and validate PCS questionnaire into Arabic language.
Methods
A repeated measures study was conducted between September 2014 and December 2016 in two tertiary hospitals in Riyadh – Saudi Arabia: King Faisal Specialized Hospital (KFSH) (Institutional Review Board [IRB] Approval No. 2141 101) and King Fahad Medical City (KFMC) (IRB Approval No. 14-107). An electronic data-capturing template was made to standardize the data collection process and maintain quality.
Translation and cultural adaptation
Initial translation (forward translation)
Five bilingual translators, from five Arabic countries (Syria, Saudi Arabia, Yemen, Sudan and Egypt) with different dialects, were assigned. All translators spoke Arabic as their mother language. Two of them were naive translators with no prior knowledge of the concepts being quantified, and they were not from the medical field. Each translator produced a written report of the translation that they completed, after which all the translators met to discuss the translation and came to a consensus of the translated version of the instrument.
Backward translation
Two translators who were totally blind to the original (English) questionnaires were assigned to translate the final Arabic version back into the English language. This is a process of validity check to make sure that the translated version reflects the same item content as the original version. English (the source language) was the mother tongue for these two translators, and they were not aware of the concepts being explored.
An expert committee
An expert committee was composed of a methodologist, health professionals, and language professionals. The expert committee's role was to consolidate all the versions of the questionnaire and develop the prefinal version of the questionnaire for field-testing. The committee eventually reviewed all the translations and reached consensus on any discrepancy.
Measures
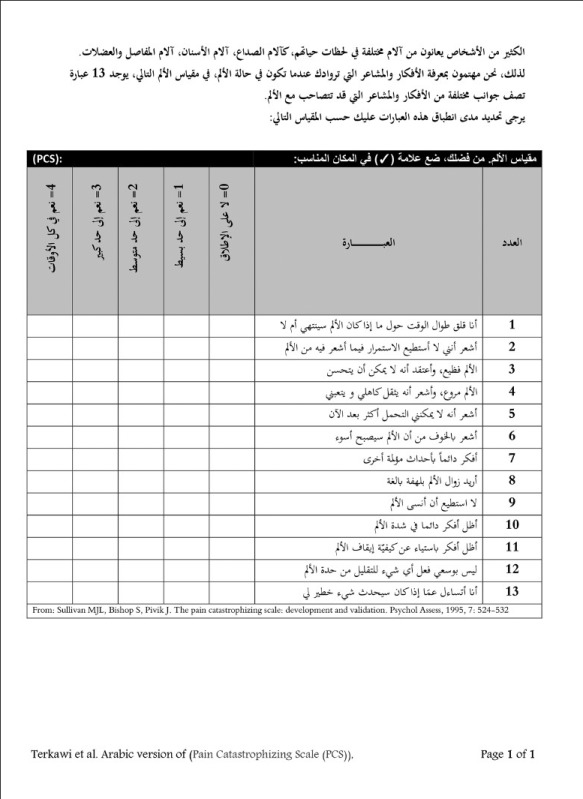
Pain catastrophizing scale
The PCS includes 13 items assessing the thoughts and feelings associated with pain.[4] The PCS assesses three dimensions of pain catastrophizing: Rumination (4 items; Questions 8, 9, 10, and 11), magnification (3 items; Questions 6, 7, and 13), and helplessness (6 items; Questions 1, 2, 3, 4, 5, and 12). Patients rate on a 5-point Likert-type scale (0 = not at all, 1 = to a slight degree, 2 = to a moderate degree, 3 = to a great degree, 4 = all the time) the degree to which they have the described thoughts and feelings when they are experiencing pain. A total PCS score can be computed by summing the score on all the items, with higher scores indicating a higher tendency of pain catastrophizing. The scores for the three PCS subscales can be obtained in a similar manner. In the original study, a PCS total score of ≥30 was considered to be indicative of a clinically relevant level of catastrophizing. Although, the author in a more recent study found a cutoff score ≥24 might be a more evidence-based cut score.[5]
Numerical rating scale
Numerical rating scale (NRS) is 11-point (0–10) pain intensity score that assesses current overall pain intensity (from 0= “no pain” to 10= “pain as bad as you can imagine”).[6]
Brief Pain Inventory
The Brief Pain Inventory (BPI) is commonly used to assess patients’ pain in clinical settings. Two domains of pain are assessed with the BPI – pain severity and pain interference. Pain severity is measured with four items, assessing pain at its “worst,” “least,” “average,” and “now” (current pain). The intensity of pain is rated from 0 (no pain) to 10 (pain as bad as you can imagine). Pain interference is measured with seven items, assessing the extent to which pain has interfered with seven daily activities (general activity, walking, work, mood, enjoyment of life, relations with others, and sleep). Patients rated, from 0 (does not interfere) to 10 (completely interferes), how pain has interfered with their functioning.[7] We used the MD Anderson Cancer Center Arabic BPI-Short Form version, a previously translated and validated version.[8] In the current study, Cronbach's alpha (α) was 0.83 and 0.88 for pain severity and pain interference, respectively.
Study protocol
An Arabic version of the PCS questionnaire was administered twice among chronic pain (more than 3 months) patients in the pain clinic. This questionnaire was part of a package that contained the BPI questionnaire and NRS as validating questionnaires (all in Arabic). Eligible patients were between 17 and 80 years old and reported chronic pain of at least 3 months’ duration. Exclusion criteria included psychosis, significant visual impairment, physical disability, or patient's refusal to participate in the study. The patients completed the questionnaire for the first time (Time 1) in the clinic, after the researcher explained the purpose of the study, obtained a verbal consent, and answered all queries. The questionnaire was completed the second time (Time 2) by telephone interview after an average of 7 days.
Pilot study
The prefinal version was pilot tested on a group of 34 patients (19 males and 15 females). The pilot data are not shown here for space consideration. Both interviews (Time 1 and Time 2) were completed in person, after which the participants were asked about their experience and thoughts about the current version. No specific feedback was received. The committee met at this point and approved the prefinal version as final [the final Arabic version is presented in the Appendix 1]. No changes were implemented to the prefinal version.
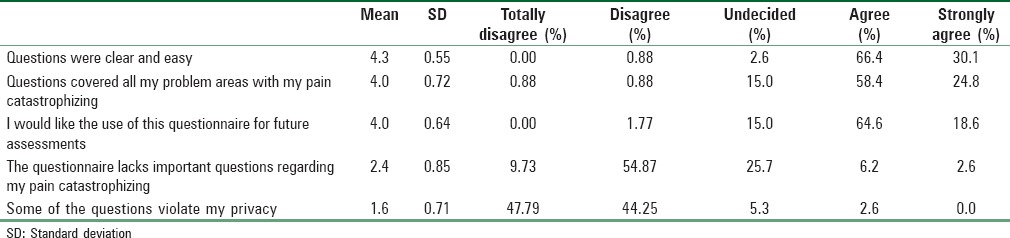
Assessing face validity
After completing the PCS at Time 1, patients responded to five statements regarding the PCS items on a 5-point Likert type scale: 1 = totally disagree, 2 = disagree, 3 = undecided, 4 = agree, and 5 = strongly agree. The five statements were: (1) Questions were clear and easy; (2) questions covered all your problem areas with your pain catastrophizing; (3) you would like the use of this questionnaire for future assessments; (4) the questionnaire lacks important questions regarding your pain catastrophizing; (5) any of the questions violate your privacy.
Statistical analysis
All data analyses were performed in R version 3.3.2 (2016-10-31). Descriptive statistics (mean [M], standard deviation [SD], minimum, maximum)[9] were presented for the PCS items, subscale and total scores, BPI items and composite score.
Reliability
The internal consistency of the PCS was examined using Cronbach's α. Cronbach's α ranges from 0 (no internal consistency; none of the items are correlated with each other) to 1 (perfect internal consistency; all of the items are perfectly correlated with each other). Cronbach's α was computed for the total PCS scale (all 13 items), as well as the rumination (4 items), magnification (3 items), and helplessness (6 items) subscales. An instrument with α ≥0.70 is typically considered to have adequate internal consistency.[10] As α is a function of the questionnaire's length, α is expected to be lower for the subscales than for the total scale.
Test-retest reliability was assessed by a second administration (Time 2) of the PCS, after at least 72 h of the first administration (Time 1). The stability of the individuals’ responses was estimated using the Pearson's correlation coefficients (r) between their responses in the two administrations. Pearson correlation coefficient (r) between the two assessments was computed for the PCS subscale and total pain scores. Test-retest reliability was considered to be weak if r < 0.3, moderate if 0.3 ≥ r < 0.5, and strong if r ≥ 0.5. Intraclass correlation coefficients (ICCs) were also computed, with ICC ≥0.70 indicating good test-retest reliability.[11]
Validity
Construct validity of the PCS was examined by investigating the association between the PCS subscale and total scores and the numerical pain scale. To establish concurrent validity of the PCS, the extent to which the PCS is correlated with another validated measure of pain, the BPI. Pearson's correlation coefficient (r) was used to evaluate the strength of the associations; r < 0.3 was considered to be weak, moderate if 0.3 ≥ r < 0.5, and strong if r ≥ 0.5.
Results
A total of 113 patients (50 men, 63 women) participated in the validation study of the PCS questionnaire. The average age was 52 (SD = 17), with average BMI of 33 (SD = 8). Most patients had university-level education (39%), with fewer proportions having received some high school (36%), less than high school (14%), or no education (11%). The majority of these patients were married (87%), whereas 8% were single, <2% were divorced, and 4% were widowed. Of the enrolled patients, 29% were rated as 1, 54% were rated as 2, and 16% were rated as 3 on the American Society of Anaesthesiologists (ASA) score. Eighty six (76%) patients were from KFSH, and 27 (24%) from KFMC. Most patients (90%) reported having current pain.
Chronic pain diagnoses were as follows: 54 (47.8%) radiculopathy, 10 (8.8%) musculoskeletal, 9 (8.0%) osteoarthritis, 8 (7.1%) mechanical low back pain, 5 (4.4%) failed back surgery syndrome, 3 (2.7%) nerve injury/trauma, 3 (2.7%) sacroiliitis, 3 (2.7%) spinal stenosis, 2 (1.8%) carpal tunnel syndrome, 2 (1.8%) complex regional pain syndrome, 2 (1.8%) mechanical neck pain, 2 (1.8%) spondylolisthesis, 2 (1.8%) trigeminal neuralgia, 1 (0.9%) chronic headache, 1 (0.9%) fibromyalgia, 1 (0.9%) occipital neuralgia, 1 (0.9%) rotator cuff tear, 1 (0.9%) spinal cord injury, 1 (0.9%) spondylosis, 1 (0.9%) meralgia paresthetica, and 1 (0.9%) unknown cause.
On average, the patients were contacted for the second interview 8 (SD = 7) days after their initial participation. The majority of the patients (93%) completed the second interview within 10 days after the initial interview.
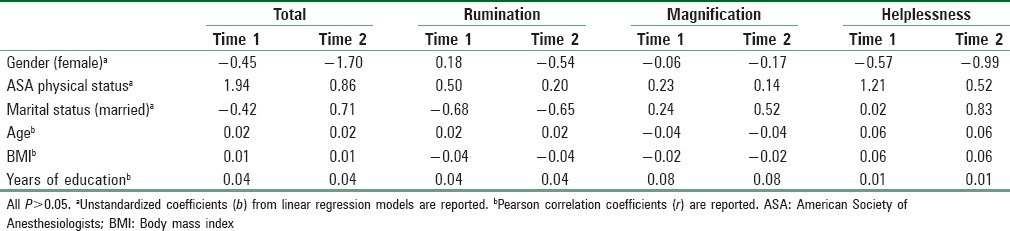
The descriptive statistics of the PCS and BPI at Time 1 and Time 2 are presented in Table 1. Patients’ scores on the PCS total and subscales were not correlated with their demographic characteristics [Table 2].
Table 1.
Descriptive statistics of the pain catastrophizing scale, Brief Pain Inventory, and numerical rating scale for chronic pain patients
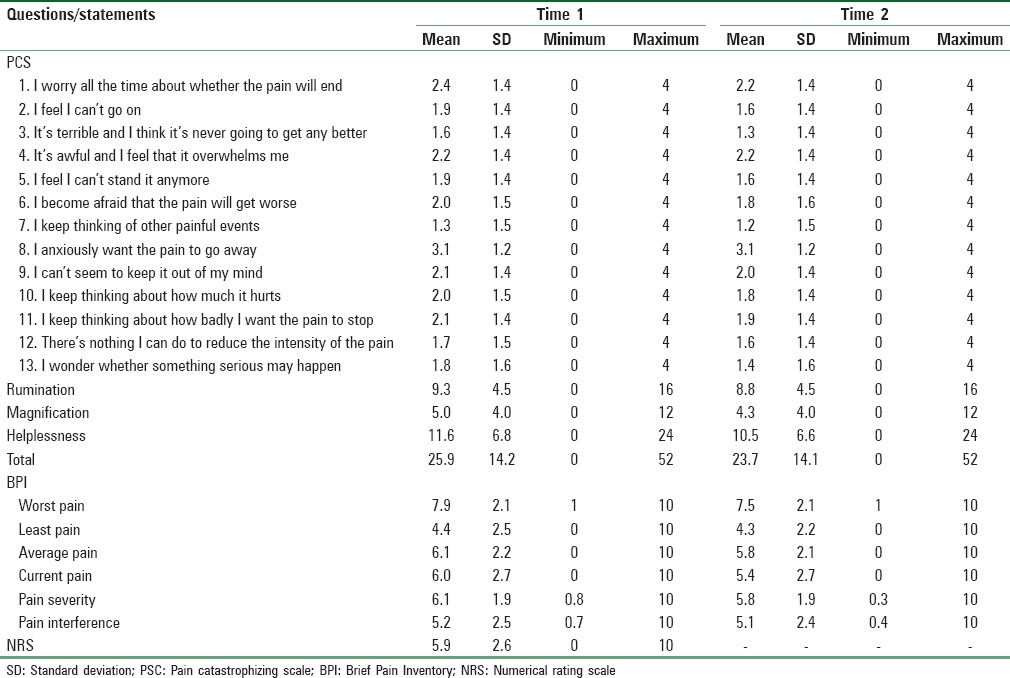
Table 2.
Associations between demographic characteristics and pain catastrophizing
Reliability
Cronbach's α's for the PCS total scale and subscales are shown in Table 3. Results showed excellent internal consistency for the 13-item PCS. The internal consistencies for the three subscales were good, albeit slightly lower, as to be expected given the subscales consist of fewer items.
Table 3.
Cronbach's alpha for the Pain Catastrophizing Scale
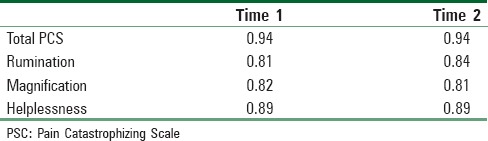
Test-retest reliability was computed using all patients with complete PCS data for both interviews; none of the patients had missing data on the PCS. The correlation coefficients (rs) between the two interviews were 0.84 (95% confidence interval [CI]: 0.77–0.89), 0.83 (95% CI: 0.76–0.88), 0.81 (95% CI: 0.73–0.86), and 0.8 (95% CI: 0.72–0.86) for the total PCS, rumination, magnification, and helplessness subscales, respectively. ICCs were 0.83 (95% CI: 0.77–0.89), 0.82 (95% CI: 0.76–0.88), 0.8 (95% CI: 0.73–0.86), and 0.79 (95% CI: 0.72–0.86) for the total PCS, rumination, magnification, and helplessness subscales, respectively. Results suggested good test-retest reliability for the overall PCS and its three dimensions.
Validity
The construct validity of the PCS was assessed by examining the correlations between the PCS and patients’ self-reported current pain on the NRS. Results from linear regression showed that there was no statistically significant difference in the total PCS scores between patients who reported having current pain and those who reported having no current pain (b = 2.64, standard error [SE] =4.53, P = 0.56). Among the 102 patients who reported having current pain, the severity of the reported pain on the NRS was weakly associated with their PCS scores (r = 0.22, P = 0.03). Results suggested that patients who reported more severe pain were slightly more likely to have higher scores on the PCS.
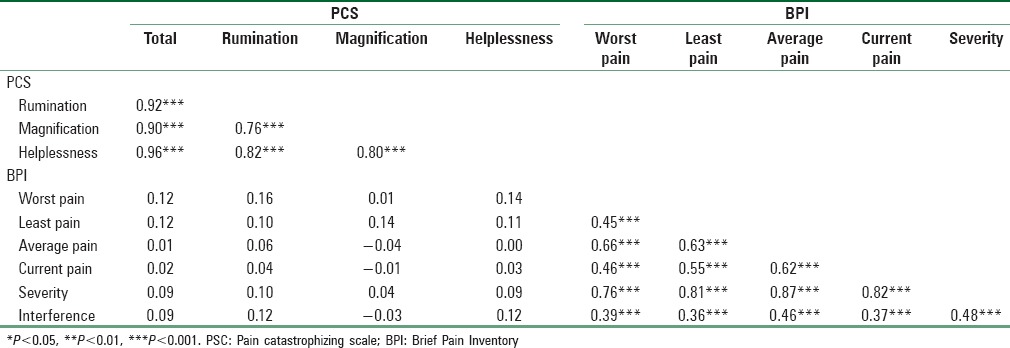
To investigate the concurrent validity of the PCS, the extent to which the PCS was associated with the BPI was examined. As shown in Table 4, PCS and its subscales were not statistically significantly associated with any of the BPI items (rs = −0.04–0.16, all Ps >0.05). Results suggested that pain catastrophizing was not correlated with pain assessed with the BPI.
Table 4.
Pearson correlation coefficients between Pain Catastrophizing Scale and Brief Pain Inventory among patients
Among the 113 patients in this study, 74 (65.5%) were diagnosed with neuropathic pain. We compared PCS scores between patients who were and were not diagnosed with neuropathic pain using linear regression models. Results showed that patients who were diagnosed with neuropathic pain had statistically significantly higher scores on the PCS total scale (b = 6.51, SE = 2.76, P = 0.02), the rumination (b = 2.13, SE = 0.86, P = 0.01) and helplessness (b = 3.20, SE = 1.32, P = 0.02) subscales than patients who were not diagnosed with neuropathic pain. There were no statistically significant differences between the two groups of patients on the PCS magnification (b = 1.18, SE = 0.78, P = 0.14) subscale.
Face validity
Patients’ responses to the five questions assessing the face validity of the PCS are presented in Table 5. The majority of the patients endorsed agree or strongly agree for the first three questions assessing face validity. Results showed that most patients found the PCS questions to be clear and easy to understand, the questionnaire items covered all their problem areas regarding their pain catastrophizing, and that most would like to use the PCS for their long-term follow-up assessment. Most patients disagreed that the PCS lacks important questions regarding their pain catastrophizing, suggesting that the PCS addressed most, if not all, of the important issues associated with pain catastrophizing. Finally, most patients felt that the PCS questions did not violate their privacy.
Table 5.
Descriptive statistics for face validity
Discussion
Pain catastrophizing is characterized by the tendency to magnify the threat value of a pain stimulus, to feel helpless in the presence of pain, as well as by a relative inability to prevent or inhibit pain-related thoughts in anticipation of, during, or following a painful event. The PCS is one of the most widely used questionnaires to assess pain catastrophizing. It is also available in 20 other languages, including Brazilian,[12] Chinese,[13] Hindi,[14] Norwegian,[15] and South African.[16]
To the best of our knowledge, this is the first study to translate, culturally adapt, and validate the PCS questionnaire in Arabic. Our Arabic version of the PCS showed excellent internal consistency and test-retest reliability. Among patients who reported experiencing current pain, PCS scores were positively associated the severity of pain, suggesting that pain catastrophizing may be associated with the intensity of distress caused by pain. In the current study, most patients found the PCS questions to be easy to understand and cover all areas relevant to their pain catastrophizing. Such findings indicated that the translated PCS version can be easily administrated among Arabic-speaking patients.
Patients’ demographic characteristics (gender, age, years of education, or marital status) and health status (ASA score) were not associated with the PCS total or subscale scores. In a previous study, Osman et al.[17] found a significant difference in PCS scores between men and women. Compared to men, women were reported to have higher PCS scores on the rumination and helplessness subscales, as well as the total PCS scale. On the contrary, no statistically significant gender difference was observed in the PCS total or subscales among patients in our study. Future studies should examine whether there exists cross-cultural differences in the construct of pain catastrophizing among similar types of patients. However, we found patients who were diagnosed with neuropathic pain had higher scores on the PCS total scale, the rumination and helplessness subscales than patients who were not diagnosed with neuropathic pain. Our findings echoes Cory et al. findings, as they found women with features of neuropathic pain have worse pain catastrophizing than those without features of neuropathic pain.[18]
The current study found that the PCS scores were not associated with the presence or absence of current pain. In addition, the PCS total and subscale scores were not correlated with pain assessed with the BPI. These results suggested that pain catastrophizing, as assessed with the PCS, may not be associated with the subjective perspective of pain, pain intensity, or pain interference. It is possible that pain catastrophizing may be considered to be characteristics of personality traits or cognitive processes, which may not be necessarily related with the construct of pain itself.
Conclusion
The results of our study suggested that Arabic version of PCS is a valid and reliable tool to gauge the catastrophizing of pain among chronic pain Arabic-speaking patients. Our findings also suggested that pain catastrophizing is not associated with demographic characteristics or other subjective pain assessments among Arabic-speaking patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Appendix 1: Arabic version of the pain catastrophizing scale questionnaire
References
- 1.Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: A critical review. Expert Rev Neurother. 2009;9:745–58. doi: 10.1586/ERN.09.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heyneman NE, Fremouw WJ, Gano D, Kirkland F, Heiden L. Individual differences and the effectiveness of different coping strategies for pain. Cognit Ther Res. 1990;14:63–77. [Google Scholar]
- 3.VanDenKerkhof EG, Peters ML, Bruce J. Chronic pain after surgery: Time for standardization? A framework to establish core risk factor and outcome domains for epidemiological studies. Clin J Pain. 2013;29:2–8. doi: 10.1097/AJP.0b013e31824730c2. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychol Assess. 1995;7:524–32. [Google Scholar]
- 5.Scott W, Wideman TH, Sullivan MJ. Clinically meaningful scores on pain catastrophizing before and after multidisciplinary rehabilitation: A prospective study of individuals with subacute pain after whiplash injury. Clin J Pain. 2014;30:183–90. doi: 10.1097/AJP.0b013e31828eee6c. [DOI] [PubMed] [Google Scholar]
- 6.Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. New York: The Guilford Press; 2001. pp. 15–34. [Google Scholar]
- 7.Cleeland CS, Ryan KM. Pain assessment: Global use of the brief pain inventory. Ann Acad Med Singapore. 1994;23:129–38. [PubMed] [Google Scholar]
- 8. [Last accessed on 2017 Jan 07]. Available from: https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI-SF_English-24h_Original_SAMPLE.pdf .
- 9.Caret: Classification and Regression Training. [Computer Program]. Version R Package Version 6.0-732016 [Google Scholar]
- 10.Nunnally J. Psychometric Theory. New York: McGraw-Hill; 1978. [Google Scholar]
- 11.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York: McGraw-Hill; 1994. [Google Scholar]
- 12.Sehn F, Chachamovich E, Vidor LP, Dall-Agnol L, de Souza IC, Torres IL, et al. Cross-cultural adaptation and validation of the Brazilian Portuguese version of the pain catastrophizing scale. Pain Med. 2012;13:1425–35. doi: 10.1111/j.1526-4637.2012.01492.x. [DOI] [PubMed] [Google Scholar]
- 13.Xu X, Wei X, Wang F, Liu J, Chen H, Xiong Y, et al. Validation of a simplified Chinese version of the pain catastrophizing scale and an exploration of the factors predicting catastrophizing in pain clinic patients. Pain Physician. 2015;18:E1059–72. [PubMed] [Google Scholar]
- 14.Bansal D, Gudala K, Lavudiya S, Ghai B, Arora P. Translation, adaptation, and validation of Hindi version of the pain catastrophizing scale in patients with chronic low back pain for use in India. Pain Med. 2016;17:1848–58. doi: 10.1093/pm/pnv103. [DOI] [PubMed] [Google Scholar]
- 15.Fernandes L, Storheim K, Lochting I, Grotle M. Cross-cultural adaptation and validation of the Norwegian pain catastrophizing scale in patients with low back pain. BMC Musculoskelet Disord. 2012;13:111. doi: 10.1186/1471-2474-13-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris LD, Grimmer-Somers KA, Louw QA, Sullivan MJ. Cross-cultural adaptation and validation of the South African pain catastrophizing scale (SA-PCS) among patients with fibromyalgia. Health Qual Life Outcomes. 2012;10:137. doi: 10.1186/1477-7525-10-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the pain catastrophizing scale. J Behav Med. 1997;20:589–605. doi: 10.1023/a:1025570508954. [DOI] [PubMed] [Google Scholar]
- 18.Cory L, Harvie HS, Northington G, Malykhina A, Whitmore K, Arya L. Association of neuropathic pain with bladder, bowel and catastrophizing symptoms in women with bladder pain syndrome. J Urol. 2012;187:503–7. doi: 10.1016/j.juro.2011.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]


