ABSTRACT
Background: Heart Failure (HF) is a progressive epidemic associated with considerable morbidity and mortality. Self-reported data from the National Health and Nutrition Examination Survey (NHANES) provides a unique representation of individuals suffering from HF. The purpose of this study is to analyze updated NHANES 2013-2014 data to identify any changes in the prevalence and current risk factors of HF, especially given the novel lifestyles and increased medical awareness of current generations.
Methods: NHANES uses a multistage probability sampling design under the Centers for Disease Control and Prevention (CDC). The Student's t-test and Chi-square test/ Fisher's exact test was used for analysis of variables. A multiple logistic regression model was used to identify statistically significant risk factors for HF. Analyses were performed with the use of SAS software, version 9.4.
Results: Based on our analysis, the primary risk factor was coronary artery disease followed by hypertension, diabetes mellitus, age ≥ 65 years, and obesity.
Conclusion: The findings revealed that despite improved population awareness and advancements in diagnostics and therapeutics, the same risk factors continue to persist. This provided an insight into the path towards which our resources need to be directed, so as to effectively tackle the aforementioned risk factors.
KEYWORDS: Congestive heart failure, NHANES, risk factors, epidemiology
1. Introduction
Heart failure (HF) is a progressive epidemic associated with considerable mortality and morbidity as well as immense healthcare costs. HF was established as an epidemic in the latter half of the 20th century, with a progressive increase in prevalence and hospitalizations related to HF noted especially in the elderly [1,2]. HF hospitalizations and readmissions continue to rise due to many factors including increased prevalence of the disease, lack of guideline directed therapy, and lack of patient adherence. Heart failure is difficult to define as a separate entity, as its features comprise of a constellation of signs and symptoms. Due to the nature of the disease process, multiple diagnostic criteria have arisen, the most notable being those based on the Framingham Heart Study [3]. Other noteworthy criteria include those based on the Cardiovascular Health Study (CHS) or the European Society of Cardiology [4].
Regardless of criterion used, HF has shown a progressive rise in prevalence over the past few decades, attributable to both increased efficacy of treatment methods and increased age of the population. The prevalence of HF is estimated to be greater than 5.8 million in the United States and approximately more than 23 million around the world. Lifetime risk of developing HF is high (approximately one in five people) [5–7]. Self-reported studies, most notably the National Health and Nutrition Examination Survey (NHANES), provide a unique representation of individuals suffering from HF, allowing comparison of risk factors amongst the population. Given advancements in the prevention and management of HF in recent decades, it is not implausible to expect a shift in the types of risk factors implicated in its pathogenesis. Due to this reason, frequent analyses of self-reported surveys should provide an updated outlook of risk factors, especially due to novel lifestyles and the increased medical awareness of current generations. The purpose of this study is to review the updated NHANES data in order to identify any changes in the prevalence and current risk factors of HF based on self-reported data, or the lack thereof.
2. Methods
2.1. Survey design
The NHANES survey is conducted by the Centers for Disease Control and Prevention (CDC) along with the National Center for Health Statistics (NCHS). It is a review of population nutrition and general health. Survey findings provide information regarding prevalence of multiple diseases as well as associated risk factors and exposures. The survey comprises of multiple steps including household interviews and physical examinations. The sample population represents the general, non-institutionalized United States population using a sophisticated cluster survey design. Several groups of individuals such as Hispanics, African Americans, and individuals aged 60 years and older are over-represented to ensure proper sample size and reflection of the representative population. The year in focus for the purpose of this analysis was from 2013 to 2014. A total of 5761 individuals were included in the survey during this time period.
2.2. Definition of variables
Interviewers of the NHANES survey are adequately trained prior to the conduction of interviews. Presence of HF was defined based on the subject’s response to two main questions: ‘Have you ever been told by a physician that you had heart failure?’ and ‘What was your age when you were told you have heart failure?’ Major risk factors were determined by questions regarding the presence of coronary artery disease (CAD), diabetes mellitus, and obesity. Additional variables included age, sex, ethnicity, BMI, and smoking status.
3. Statistical analysis
NHANES uses a complex multi-stage probability sampling design [8]. We reported continuous variables as mean and standard deviation. The categorical variables were reported as number and percent. We used the Student’s t-test to analyze between-group differences for continuous variables, and Chi-square test or Fisher’s exact test for categorical variables. A multiple logistic regression model was used to identify significant predictors for CHF. All analyses were performed with the use of SAS software, version 9.4 (SAS Institute, Cary NC). A p-value of less than 0.05 was considered to indicate statistical significance.
4. Results
Among the 5761 individuals chosen as representative of the US general population in the NHANES Survey, 182 reported the presence of heart failure. Comparison of the individuals with HF and those without allowed determination of certain statistically significant exposures and risk factors (Table 1).
Table 1.
Demographics and risk factors based on NHANES data 2013–2014.
| CHF | Non-CHF | p-Value | |
|---|---|---|---|
| Total number of estimated population | 182 | 5579 | |
| Age at screening – mean | 66.29 | 48.52 | <0.0001 |
| Female – no.% | 95 (52.19%) | 2913 (52.21%) | 0.9966 |
| Black – no.% | 44 (24.18%) | 1129 (20.24%) | 0.1940 |
| Less than high school education – no.% | 51 (28.02%) | 1189 (21.31%) | 0.0302 |
| Current cigarette smoking (everyday/some days) – no. % | 31 (17.03%) | 1161 (20.81%) | 0.2158 |
| Abnormal alcohol consumption – no.% | |||
| Female: two or more drinks everyday | 17 (17.89%) | 896 (30.76%) | 0.0073 |
| Male: three or more drinks everyday | 8 (9.20%) | 816 (30.61%) | <0.0001 |
| NOT participate in moderate physical activity – no.% | 142 (78.02%) | 3753 (67.27%) | 0.0023 |
| Hypertension – no. % | 149 (81.87%) | 1989 (35.65%) | <0.0001 |
| High cholesterol level – no.% | 120 (65.93%) | 1884 (33.77%) | <0.0001 |
| BMI (Body mass index), means ±SD | 32.75 (9.83) | 28.99 (7.03) | <0.0001 |
| Overweight (BMI 15–29.9) – no.% | 39 (21.43%) | 1727 (30.96%) | 0.0061 |
| Obese (BMI ≥30) – no.% | 89 (48.90%) | 1991 (35.69%) | 0.0003 |
| Self-reported diabetes, % | 73 (40.11%) | 645 (11.56%) | <0.0001 |
| Coronary artery disease, % | 70 (38.46%) | 161 (2.89%) | <0.0001 |
Multiple regression models determined the top risk factors that had a statistically significant association with HF (Table 2 and Figures 1, 2). The primary risk factor was coronary artery disease (OR 8.87, 95% CI 6.14–12.81, p-value <0.0001) followed by hypertension (OR 3.38, 95% CI 2.22–5.14, p-value <0.0001). Subsequent risk factors in order of odds ratios include diabetes mellitus, age ≥65, and obesity (BMI >30). Coronary artery disease and hypertension continue to be the top two risk factors, which correlate with the results of previous studies.
Table 2.
Multiple logistic regressions on risk factors for HF patients.
| |
|
95% Confidence interval |
|
|
|---|---|---|---|---|
| Predictors | Odds ratio | Lower limits | Upper limits | p-Value |
| Coronary artery disease | 8.87 | 6.14 | 12.81 | <.0001 |
| Hypertension | 3.38 | 2.22 | 5.14 | <.0001 |
| Diabetes | 2.06 | 1.45 | 2.91 | <.0001 |
| Age 65 and older | 2.01 | 1.42 | 2.85 | <.0001 |
| Obesity (BMI 30 and above) | 1.45 | 1.04 | 2.01 | 0.0292 |
| High cholesterol | 1.42 | 1.00 | 2.02 | 0.0492 |
| NOT participate in moderate physical activity | 0.73 | 0.50 | 1.07 | 0.1032 |
| Abnormal alcohol consumption | 0.71 | 0.45 | 1.13 | 0.1479 |
| No high school education | 1.17 | 0.81 | 1.68 | 0.4036 |
Figure 1.
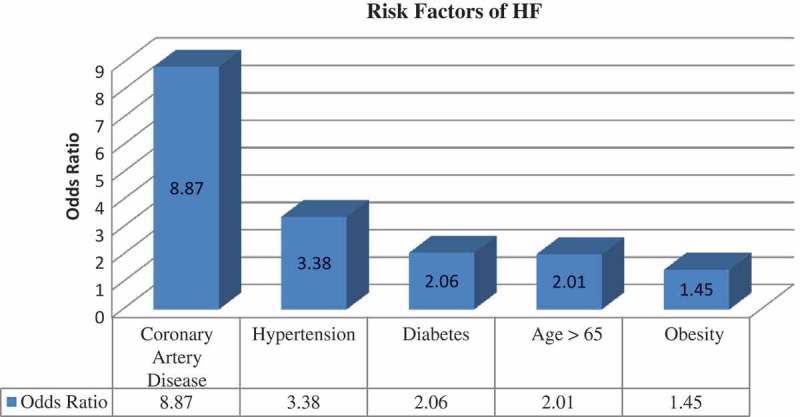
Bar diagram outlining results.
Figure 2.
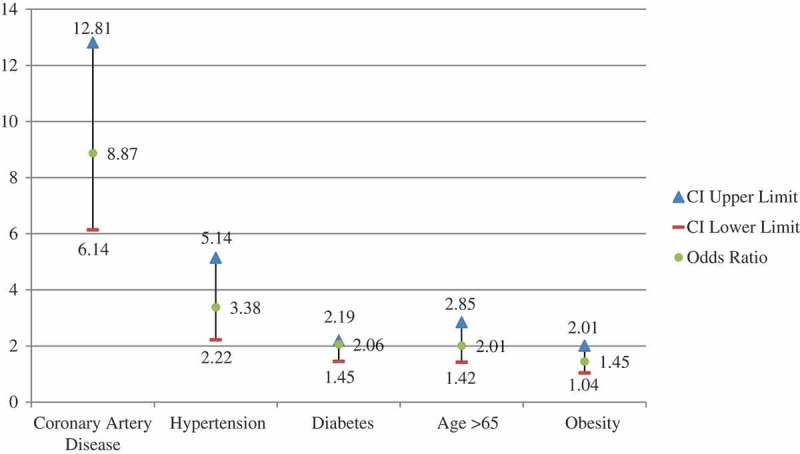
Graphical representation of results of current study with correlating Confidence Intervals (CI) and Odds Ratios(OR).
5. Discussion
Heart failure (HF) is now recognized as a progressing public health issue [9]. According to a study done by J.B. O’Connell in 1994, hospital charges for heart failure were approximately $10 000 per discharge, based on a mean length of stay of 6.3 to 7.7 days. A study of 29 000 patients with heart failure reported an average cost of almost $11 000 per patient per hospitalization in 1997 [10]. In spite of decreased incidence of HF, the prevalence of HF has increased substantially in the US over the past two decades [11–13]. Epidemiologic population-based data from the Framingham Study indicate that the incidence of HF increased precipitously with age in both genders, approximately doubling with each subsequent decade [14]. According to another study done using National Hospital Discharge Survey data from 1979 to 2004, the number of hospitalizations with the diagnosis of heart failure tripled from 1 274 000 in 1979 to 3 860 000 in 2004 [15]. These studies imply that the prevalence and costs of HF may continue to increase significantly in the future decades.
Our calculations estimated the prevalence of HF in the US as 1.9% (5 960 260 CHF patients in 311 204 216 total estimated populations) (Table 3). Prevalence of HF among men is 1.8%, which is slightly lower when compared to prevalence among women (2.0%). According to the CDC and the 2016 statistical update from American Heart Association, about 5.7 million adults in the US have heart failure, which correlates to approximately 1.77% of the United States population. A similar study done using NHANES I (1971 to 1975) data estimated the prevalence of HF in the US population as 1.1% [1]. This implies that the prevalence of the disease is increasing at a significant rate. This increase may be attributed to increased awareness among the population and advancements in diagnosis and treatment standards.
Table 3.
Extrapolation of NHANES demographic data to US population.
| Demographics | Number of HF patients estimated | Total estimated population | Prevalence rate per 100 000 people |
|---|---|---|---|
| Total | 5 960 260 | 311 204 216 | 1915 |
| Gender | |||
| Male | 2 775 492 | 152 055 444 | 1825 |
| Female | 3 184 768 | 159 148 772 | 2001 |
| Race | |||
| African Americans | 882 940 | 37 634 068 | 2346 |
The results of our study demonstrated that coronary artery disease (CAD) is the strongest and most important risk factor for the development of HF. Based on our study, the prevalence of CAD amongst the population with CHF is 38.46% (70 out of 182 with HF), with an odds ratio (OR) of 8.87 (95%CI: 6.14–12.81; P-value: <0.0001). In contrast, the prevalence of CAD among the non-HF population is a low 2.89%, highlighting the strong association between CAD and the development of HF. A prospective cohort study, based on the NHANES I survey conducted from 1971 to 1975, concluded that more than 60% of the HF cases in the study population were attributed to CAD [16]. In a major multicenter heart failure clinical trial involving 20 190 participants, CAD was the foremost cause of HF in 68% of patients, ultimately concluding that coronary artery disease had become the single most important cause of HF in Western countries [17].
Hypertension has also been viewed as a major factor in the progression of HF. The calculated prevalence of hypertension among our HF population was 81.87% (149 out of 182 with HF) with an odds ratio (OR) of 3.38 (95%CI: 2.22–5.14; P-value: <0.0001). This finding is in agreement with the cohort study in 1970 which assessed 5143 subjects from the original Framingham Heart Study and concluded that hypertension was the most common risk factor for HF. During approximately 20.1 years of follow-up, analysis of the study revealed that hypertension had a high attributable risk for HF, responsible for 59% of cases in women and 39% of cases in men [18]. Another prospective cohort study based on the NHANES I survey determined the relative risk (RR) of hypertension with respect to HF as 1.50 (95% CI: 1.34–1.68; P < .001) [16]. Ultimately, the results of our study based on the NHANES 2013–14 data are similar to the aforementioned studies, providing an insight into long-term risk for HF in hypertensive patients. This fact brings forward the predicament in treating hypertension adequately. The recent recommendations put forth by the Joint National Committee serve as current guidelines, however newer studies such as the SPRINT trial may trigger modifications in treatment standards.
Our analysis also supports that Diabetes Mellitus (DM) is an important risk factor in the development of HF. Based on our data, the self reported prevalence of diabetes among the HF population is 40.11% (73 out of 182) with an odds ratio (OR) of 2.06 (95%CI: 1.45–2.91; P-value: <0.0001). Prior research had also established diabetes as a notable risk factor for HF [19–26]. A 1997 study done using the electronic medical records of 9591 patients with type 2 DM derived that HF was prevalent in 11.8% of diabetic subjects compared to 4.5% of control subjects [27]. Several theories have been put forward to explain the pathophysiology behind the development of HF in the diabetic population, including metabolic disturbances, impaired dilatation of epicardial coronary arteries, impaired calcium homeostasis, apoptosis of myocardial cells, autonomic neuropathy, and insulin resistance [28]. Regardless of mechanism, diabetes has an undeniable association with cardiovascular mortality.
Obesity and age above 65 years are important risk factors HF. Data from our study suggested that – individuals 65 years and older had an odds ratio of 2.01(95%CI: 1.42–2.85; P-value: <0.0001) and obese individuals (BMI 30 and above) had an odds ratio of 1.45(95%CI: 1.04–2.01; P-value: <0.0292). These results are of particular interest because of the alarming rate of obesity trends in the U.S [29]. A study done in 2002 concluded that obesity alone is the risk factor in 11% of men and 14% of women with HF [30].
The major strength of our study is that it analyzes an established data set from the NHANES database, encompassing a large sample size, standardized questionnaires, and consistent data-reporting methods, thereby increasing the power of our study. Additionally, use of data from NHANES allows analysis of multiple risk factors amongst a common population, and therefore facilitates generalization reflective of the entire US population. Given that the data set is population-based, gender and racial differences are adequately studied as well.
The major limitation of this study is that it utilizes prevalence data from self-reported history, which increases the possibility of inaccurately estimating the prevalence of diseases, especially due to participant misconceptions regarding their level of health and the timing of risk-factor onset. Thus, as with most studies using questionnaires, recall bias is also a limitation in extrapolating data from this survey. Other limitations include absence of data regarding medication use or control of risk factors in individuals, such as insulin use, quantification of glucose control, optimization of BP control, etc. Moreover, the diagnosis of HF is not validated in this study, increasing the risk of observer bias.
In conclusion, our study re-established coronary artery disease and hypertension as the two foremost risk factors in the development of HF. Diabetes, age 65 years and older, and obesity are the other risk factors that play an important role as well. The results of our study are similar to the results of previous studies, revealing that despite improved population awareness and newer advancements in diagnostics and therapeutics, the same risk factors continue to persist. Extensive analysis of the NHANES 2013-14 data provided an insight into the path towards which our resources need to be directed, with a goal to more effectively tackle the aforementioned risk factors.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Schocken D, Arrieta M, Leaverton P, et al. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol. 1992;20(2):301–306. DOI: 10.1016/0735-1097(92)90094-4 [DOI] [PubMed] [Google Scholar]
- [2].Fang J, Mensha G, Croft J, et al. Heart failure related hospitalization in the U.S. J Am Coll Cardiol. 2008;52:428–434. DOI: 10.1016/j.jacc.2008.03.061 [DOI] [PubMed] [Google Scholar]
- [3].McKee P, Castelli W, McNamara P, et al. The natural history of congestive heart failure: the Framingham study. New England J Med. 1971;285(26):1441–1446. DOI: 10.1056/nejm197112232852601 [DOI] [PubMed] [Google Scholar]
- [4].Di Bari M, Pozzi C, Cavallini C.. The diagnosis of heart failure in the community comparative validation of four sets of criteria in unselected older adults: the ICARe Dicomano study. J Am Coll Cardiol. 2004;44(8):1601–1608. DOI: 10.1016/j.jacc.2004.07.022 [DOI] [PubMed] [Google Scholar]
- [5].Braunwald E. Cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. New England J Med. 1997;337(19):1360–1369. DOI: 10.1056/nejm199711063371906 [DOI] [PubMed] [Google Scholar]
- [6].Lloyd-Jones D, Adams R, Brown T, et al. Heart disease and stroke statistics–2010 update: a report from the American heart association. Circulation. 2009;121(7):e46–e215. DOI: 10.1161/circulationaha.109.192667 [DOI] [PubMed] [Google Scholar]
- [7].Levy D, Kenchaiah S, Larson M, et al. Long-term trends in the incidence of and survival with heart failure. New England J Med. 2002;347(18):1397–1402. DOI: 10.1056/nejmoa020265 [DOI] [PubMed] [Google Scholar]
- [8].NHANES I web tutorial: sample design in NHANES I: sample design. Cdcgov. 2016. [cited 2016 August 4]. Available from: https://www.cdc.gov/nchs/tutorials/NHANES/SurveyDesign/SampleDesign/Info1_I.htm
- [9].McMurray J. Heart failure: epidemiology, aetiology, and prognosis of heart failure. Heart. 2000;83(5):596–602. DOI: 10.1136/heart.83.5.596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].O’Connell J. The economic burden of heart failure. Clin Cardiol. 2000;23(S3):III6–III10. DOI: 10.1002/clc.4960231503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].National Center for Health Statistics. Health, United States. 1995. [cited 2016 August 4]. Available from: https://www.cdc.gov/nchs/data/hus/hus95.pdf [Google Scholar]
- [12].National Heart, Lung, and Blood Institute Morbidity and mortality chartbook on cardiovascular lung and blood diseases. Bethesda (MD): US Department of Health and Human Services, National Institutes of Health; 1996. [Google Scholar]
- [13].Gillum R. Epidemiology of heart failure in the United States. Am Heart J. 1993;126(4):1042–1047. DOI: 10.1016/0002-8703(93)90738-u [DOI] [PubMed] [Google Scholar]
- [14].Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5(2):167–173. DOI: 10.1023/a:1009884820941 [DOI] [PubMed] [Google Scholar]
- [15].Fang J, Mensah G, Croft J, et al. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol. 2008;52(6):428–434. DOI: 10.1016/j.jacc.2008.03.061 [DOI] [PubMed] [Google Scholar]
- [16].He J, Ogden L, Bazzano L, et al. Risk factors for congestive heart failure in US men and women. Arch Intern Med. 2001;161(7):996 DOI: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- [17].Gheorghiade M, Bonow R. Chronic heart failure in the United States: a manifestation of coronary artery disease. Circulation. 1998;97(3):282–289. DOI: 10.1161/01.cir.97.3.282 [DOI] [PubMed] [Google Scholar]
- [18].Levy D. The progression from hypertension to congestive heart failure. JAMA. 1996;275(20):1557 DOI: 10.1001/jama.1996.03530440037034 [DOI] [PubMed] [Google Scholar]
- [19].Ali A, Rybicki B, Alam M, et al. Clinical predictors of heart failure in patients with first acute myocardial infarction. Am Heart J. 1999;138(6):1133–1139. DOI: 10.1016/s0002-8703(99)70080-3 [DOI] [PubMed] [Google Scholar]
- [20].Mehta R, Ruane T, McCargar P, et al. The treatment of elderly diabetic patients with acute myocardial infarction. Arch Intern Med. 2000;160(9):1301 DOI: 10.1001/archinte.160.9.1301 [DOI] [PubMed] [Google Scholar]
- [21].Gottdiener J, Arnold A, Aurigemma G, et al. Predictors of congestive heart failure in the elderly: the cardiovascular health study. J Am Coll Cardiol. 2000;35(6):1628–1637. DOI: 10.1016/s0735-1097(00)00582-9 [DOI] [PubMed] [Google Scholar]
- [22].Kannel W. Vital epidemiologic clues in heart failure. J Clin Epidemiol. 2000;53(3):229–235. DOI: 10.1016/s0895-4356(99)00135-3 [DOI] [PubMed] [Google Scholar]
- [23].Capes S, Hunt D, Malmberg K, et al. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355(9206):773–778. DOI: 10.1016/s0140-6736(99)08415-9 [DOI] [PubMed] [Google Scholar]
- [24].Smith W. Epidemiology of congestive heart failure. Am J Cardiol. 1985;55(2):A3–A8. DOI: 10.1016/0002-9149(85)90789-1 [DOI] [PubMed] [Google Scholar]
- [25].Chen Y, Vaccarino V, Williams C, et al. Risk factors for heart failure in the elderly: a prospective community-based study. Am J Med. 1999;106(6):605–612. DOI: 10.1016/s0002-9343(99)00126-6 [DOI] [PubMed] [Google Scholar]
- [26].Aronow W, Ahn C, Kronzon I. Comparison of incidences of congestive heart failure in older African-Americans, Hispanics, and Whites. Am J Cardiol. 1999;84(5):611–612. DOI: 10.1016/s0002-9149(99)00392-6 [DOI] [PubMed] [Google Scholar]
- [27].Nichols G, Hillier T, Erbey J, et al. Congestive heart failure in type 2 diabetes: prevalence, incidence, and risk factors. Diabetes Care. 2001;24(9):1614–1619. DOI: 10.2337/diacare.24.9.1614 [DOI] [PubMed] [Google Scholar]
- [28].Kasznicki J, Drzewoski J. State of the art paper heart failure in the diabetic population – pathophysiology, diagnosis and management. Arch Med Sci. 2014;3:546–556. DOI: 10.5114/aoms.2014.43748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Executive summary of the clinical guidelines on the Identification, evaluation, and treatment of overweight and obesity in Adults. Arch Intern Med. 1998;158(17):1855 DOI: 10.1001/archinte.158.17.1855 [DOI] [PubMed] [Google Scholar]
- [30].Kenchaiah S, Evans J, Levy D, et al. Obesity and the risk of heart failure. New England J Med. 2002;347(5):305–313. DOI: 10.1056/nejmoa020245 [DOI] [PubMed] [Google Scholar]


