ABSTRACT
We present the case of an 83-year-old woman with a past medical history significant for schizoaffective disorder, presenting to our emergency department with the complaint of ‘pain’. Given the non-specific complaint and the limited history obtained, CT imaging was performed on her chest and abdomen which incidentally found a large duodenal diverticulum. This manuscript discusses the incidence of duodenal diverticula and the potential associated complications.
KEYWORDS: Duodenal diverticulum, complications
1. Background
Diverticula are sac-like protrusions of the bowel wall that occur throughout the small and large intestine. Diverticula of the small bowel are much less common and tend to be asymptomatic, and are found incidentally on routine imaging. According to Leivonen et al. [1], 2–5% of patients undergoing upper GI barium studies and 7% of patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) have been reported to have duodenal diverticula.[1]
In the small bowel, the most common location is that of the duodenum, more specifically near the papilla of Vater.[2] Most duodenal diverticula are extraluminal as this is secondary to herniation near the entrance of a large vessel,[1] while intraluminal ones tend to be congenital, secondary to incomplete canalization.[3]
As previously mentioned, approximately 90% of patients with duodenal diverticula are asymptomatic,[4] with the most common symptom being postprandial cramping epigastric pain.
Complications are rare in duodenal diverticulosis but have been reported, including but not limited to: small bowel obstruction (more common with intraluminal diverticula), diverticulitis, and gastrointestinal bleeding.
Duodenal diverticula are typically found on upper gastrointestinal series or abdominal CT, which usually shows a globular out-pouching (as seen in our case in Figure 1). The most accurate imaging modality is upper endoscopy but this is rarely performed given the benign nature of the disease.[5]
Figure 1.
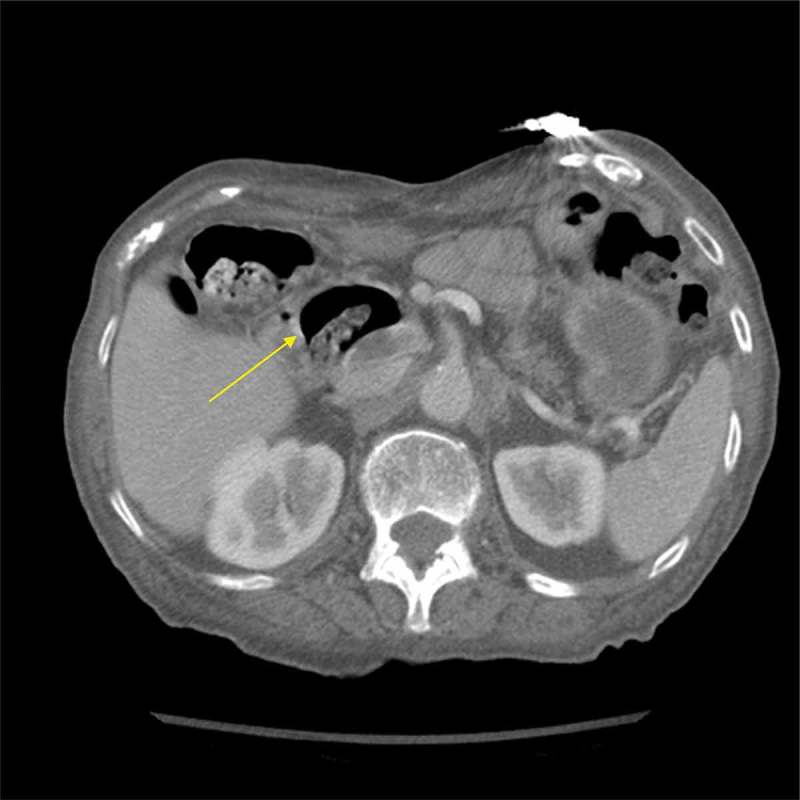
Abdominal CT with contrast showing the large out pouching of a duodenal diverticulum containing mostly gas and some ingested material.
2. Case report
We present the case of an 83-year-old woman with a past medical history significant for schizoaffective disorder, presenting to our emergency department with the complaint of ‘pain’. Taking her history was made challenging due to her underlying psychiatric disorder, as she could not elaborate on duration or even location of her pain. The limited information obtained indicated either chest or abdominal pain. The review of systems was unremarkable with the exception of early satiety. Other relevant medical history includes: atrial fibrillation, coronary artery disease and hypertension for which she takes carvedilol, furosemide, clopidogrel and warfarin. In addition, she has olanzapine and citalopram for her schizoaffective disorder.
The patient was afebrile and normotensive with tachypnea at 22 respirations and tachycardia of 102 bpm. The physical exam was unremarkable. Initial laboratory testing of CBC and BMP were within normal limits. Three sets of troponin were all negative for ischemia and the EKG was unremarkable save for the exception of some premature ventricular contractions. The urinalysis was not suggestive of a urinary tract infection.
The patient was started on omeprazole for presumed acid reflux causing the abdominal/chest pain but given her multiple cardiac risk factors, she was admitted to the hospital to rule out acute coronary syndrome.
As the patient had tachypnea with tachycardia, a chest CT was ordered which was negative for acute pulmonary embolism. Interestingly, the chest CT showed a potential ‘pancreatic mass’ and further evaluation was recommended. On day 2 of hospitalization, abdominal CT was ordered which did not show a pancreatic mass and instead a very large duodenal diverticulum.
3. Conclusion
Since most duodenal diverticula are asymptomatic and found incidentally, no treatment is indicated. Intervention is only required if the patient develops complications such as bowel obstruction, diverticulitis, GI bleeding, or small intestinal bacterial overgrowth. Surgical management is reserved for complicated diverticulitis involving bowel perforation, abscess, or fistula.[5]
Acute coronary syndrome was ruled out in our patient and the non-specific pain was likely secondary to acid reflux as the patient felt much improved 24 h after initiating the proton pump inhibitor. However, symptomatic duodenal diverticula could not be ruled out as we could not confirm the exact location or quality of pain. Regardless, our patient had no signs of bowel obstruction, diverticulitis, GI bleeding, or small intestinal bacterial overgrowth. Therefore, no further intervention was required and she was safely discharged to home on the second day of hospitalization.
It is important for healthcare providers to be aware of the complications associated with duodenal diverticulum as this is a relatively common incidental finding with a potential dangerous outcome if complications are not recognized early.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Leivonen MK, Halttunen JA, Kivilaakso EO.. Duodenal diverticulum at endoscopic retrograde cholangiopancreatography, analysis of 123 patients. Hepatogastroenterology. 1996;43(10):961–57. [PubMed] [Google Scholar]
- [2].Akhrass R, Yaffe MB, Fischer C, et al. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997;184(4):383–388. [PubMed] [Google Scholar]
- [3].Fleming CR, Newcomer AD, Stephens DH, et al. Intraluminal duodenal diverticulum. Report of two cases and review of the literature. Mayo Clin Proc. 1975;50(5):244–248. [PubMed] [Google Scholar]
- [4].Psathakis D, Utschakowski A, Müller G, et al. Clinical significance of duodenal diverticula. J Am Coll Surg. 1994;178(3):257–260. [PubMed] [Google Scholar]
- [5].Palder SB, Frey CB. Jejunal diverticulosis. Arch Surg. 1988;123(7):889–894. [DOI] [PubMed] [Google Scholar]


