Abstract
Background
There is a paucity of data on the use of alcohol in urban slums of southern India.
Methods
We screened 2811 men for alcohol use via a household-level census in an urban slum in Vellore, Tamil Nadu, and interviewed 220 age- and area-matched pairs of men drinkers and non-drinkers to examine factors associated with alcohol use. Alcohol Use Disorder Identification Test (AUDIT), a standard instrument, was used to assess risk levels of drinking of 354 drinkers. Prevalence rates were calculated using age-adjusted direct standardization. Odds ratios (ORs) of drinking status and higher-risk drinking were calculated using conditional logistic regression and ordinal logistic regression, respectively.
Results
Among all men, we estimated that 46.1% consumed alcohol and 31.4% were hazardous drinkers (19% increased-risk, 7.7% high-risk and 4.7% dependent drinkers). Factors associated with alcohol use were: manual labour occupations (OR 2.08); presence of a common mental disorder (OR 1.50) and smoking (OR 2.08); while Muslim religion was protective (OR 0.43). Factors associated with higher-risk alcohol use were: being reported as a non-drinker during the census (OR 3.96); presence of a common mental disorder (OR 3.83); smoking (OR 1.78); drinking before legal age of 21 years (OR 2.71); spending more than
 100 per day on alcohol (OR 6.17); and mainly drinking Indian-made foreign liquor (OR 5.45).
100 per day on alcohol (OR 6.17); and mainly drinking Indian-made foreign liquor (OR 5.45).
Conclusion
High prevalence of hazardous drinking and the factors associated with it suggest the need for population-wide interventions and further investigations to effectively reduce hazardous alcohol use and its harmful effects.
INTRODUCTION
Alcohol-related problems are rapidly becoming a major public health concern in India as a result of increased production, easy availability and changing values of society.1,2 It is estimated that 20%–40% of men between 15 and 60 years of age consume alcohol regularly or intermittently, and prevalence of alcohol use and hazardous use are trending upwards.3,4 Alcohol-related problems are attributable in over one-fifth of hospital admissions in India, but are under-recognized by physicians who treat such patients.5 Alcohol is involved in 15%–20% of traumatic brain injuries and 60% of all injuries reported to emergency rooms.5 Hazardous alcohol use is highly associated with oesophageal cancer, liver disease, duodenal ulcer, high-risk sexual behaviour, HIV infection, tuberculosis and suicide.5 A rapid increase in prevalence of hazardous alcohol use implies increased alcohol-related morbidity, which increases the cost of healthcare. Estimates from a study in Bengaluru show that Government of India spends about
 244 billion per year to manage the consequences of hazardous alcohol use, while it earns
244 billion per year to manage the consequences of hazardous alcohol use, while it earns
 216 billion annually from excise revenue of alcohol.3 Hence, hazardous alcohol use is a major issue for the country as well as for individuals.
216 billion annually from excise revenue of alcohol.3 Hence, hazardous alcohol use is a major issue for the country as well as for individuals.
Hazardous alcohol use, especially dependent drinking, also has serious consequences to those close to drinkers. Children of dependent drinkers are at increased risk of physical injuries and malnutrition.6 Domestic violence is significantly more among households with hazardous alcohol users.7 Wives of hazardous alcohol users are 2–3 times more likely to have mental disorders compared to wives of moderate- or non-drinkers.8 Clinicians often see women with depression, and occasionally signs of domestic violence, likely to be related to alcohol use by their spouses.
A previous study in rural Kaniyambadi block of Vellore has shown that the rates of alcohol use and hazardous use among men were 34.8% and 14.2%, respectively.9 The same study identified use of Indian-made foreign liquor (IMFL) and availability of illicitly brewed alcohol as risk factors of hazardous use, while education was deemed protective. A recent study in a slum community in Kolkata found that prevalence rates of alcohol use and hazardous use among men were 65.8% and 22%, respectively.10 A study in Bengaluru reported 31.1% prevalence of alcohol use among men in slum communities.3 A report from general practices in Goa estimated that 59% of men consumed alcohol, and 15% were hazardous drinkers.11 An alcohol prevalence study or a risk factor assessment in urban slum areas in southern India has not yet been reported.
We aimed to determine the nature, prevalence and factors associated with alcohol use and hazardous use among adult men in an urban slum community called Old Town in Vellore, Tamil Nadu, using a cross-sectional and matched case–control study design.
METHODS
Overview and setting
This study was conducted from December 2010 through May 2011 in a slum community called Old Town in Vellore, Tamil Nadu. Old Town is a geographically defined area of 0.3 km2 with a population of about 8900. The Low Cost Effective Care Unit (LCECU) of Christian Medical College (CMC), Vellore, has been working in the area for many years providing primary and secondary care services. The institutional review board of CMC approved this study.
The study has three sections: (i) cross-sectional survey of 2811 men in Old Town to assess alcohol use and factors associated with being reported as a drinker; (ii) analysis of 220 case–control pairs to further evaluate factors associated with drinking status; and (iii) assessment of 354 drinkers to determine risk factors of hazardous drinking. The details of the study are outlined below.
Census and alcohol use screening
We updated the census of Old Town, which was initially conducted from December 2008 through July 2009 by LCECU. The initial census data included household-level data (e.g. location, religion and socioeconomic class) and individual-level data (e.g. gender, occupation, marital status, education and year of birth). Socioeconomic class was assessed on a 5-point scale based on the Kuppuswamy scale, modified specifically for use in Vellore.12 Households were classified as low, middle or high socioeconomic classes.
Five trained field workers visited each household listed in the initial census, recorded any new members and those who were no longer in the household, and updated individual-level data. An additional field worker was responsible for surveying any new households not included in the initial census. The field workers interviewed adult household representatives who were considered the most knowledgeable about their household members.
To screen for alcohol use, we asked the representative if anyone in the household consumed any alcohol in the past 12 months. Those who had consumed alcohol in the past 12 months were listed as reported drinkers, and those who had not consumed alcohol were listed as reported non-drinkers.
If no one was available at a household on three separate visits (i.e. door-locked), the household was excluded from the census. We enumerated a total of 1902 households and excluded 5 door-locked households.
Case–control design
Due to limited resources, we designed a matched case–control study to identify risk factors of alcohol use. Among 2811 adult men identified in the census (year of birth ≤1992), we individually interviewed samples of drinkers (cases) and non-drinkers (controls). A schematic of sample selection is shown in Fig. 1.
Fig 1.
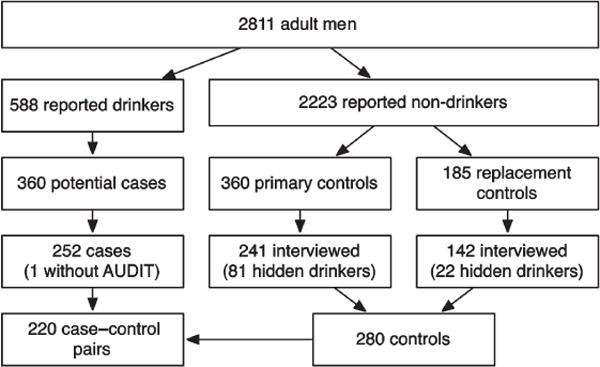
Flowchart of case–control sample selection
AUDIT Alcohol Use Disorder Identification Test
We randomly selected 360 potential cases from among the 588 reported drinkers, and then selected 360 primary controls from among 2223 reported non-drinkers (Fig. 1). The primary controls were pair-wise matched with each case based on year of birth (within 6 years) and area of residence. A matched case–control design allowed us to produce more accurate odds ratios (ORs) of drinking status by controlling for confounding factors related to age and area. We used area of residence as a matching criterion because Old Town consists of six contiguous areas that vary in general characteristics.
We excluded participants from the study if (i) they refused to be interviewed, (ii) they had moved out of residence recorded in the census, (iii) they had died since the time of the census, (iv) no one answered the door on three separate occasions (i.e. door-locked), or (v) they had been misclassified as potential cases or controls. When a primary control was excluded or was found to be a drinker during the private interview (i.e. hidden drinker), we selected a replacement control that met the same matching criteria. After exclusion, we recruited a total of 251 cases and 280 controls. Thirty-one cases and 60 controls did not have matching controls and cases, respectively, resulting in 220 matched pairs. We also recruited 103 hidden drinkers (81 from primary controls and 22 from replacement controls).
Assessments
For the private interviews, we developed a questionnaire, which included basic demographic information such as age and the number of years lived in the current residence, and the General Health Questionnaire 12 (GHQ-12).13,14 GHQ-12 is a 12-item questionnaire that is widely used in primary care settings to screen for common mental disorders (CMDs), namely depression and anxiety.15 A score ≥4 of 12 is considered a positive result and suggests the presence of a CMD. The Tamil version of GHQ-12 has been validated previously in a community study in Vellore.16
To confirm the drinking status reported in the census, and identify drinkers not reported in the census, we asked each participant about his alcohol use. If the participant reported use of alcohol in the past 12 months we used the Alcohol Use Disorder Identification Test (AUDIT)17 to assess their risk level of alcohol use. AUDIT is a simple, 10-item questionnaire used for screening and classifying alcohol drinkers. Drinkers were classified as low risk (scores 0–7), increased risk (scores 8–15), high risk (scores 16–19) and dependent drinker (scores 20–40).17 In this study and in general, ‘hazardous drinking’ or ‘hazardous use’ refers to AUDIT scores of ≥8. The Tamil version of the AUDIT has been utilized previously in Vellore.9
Alcohol was defined as beer, wine, IMFL (a category of hard liquor that emulates western-style drinks, such as brandy, rum, and whisky, with a maximum alcohol content of 42.8%),9 and illicitly distilled liquor called ‘pattai saarayam’. We defined a ‘drink’ based on standard bottle sizes of beer and IMFL. IMFL is available in three bottle sizes: quarter (180 ml; 4 drinks), half (360 ml; 8 drinks) and full (750 ml; 17 drinks). Beer is available in one bottle size (650 ml), but comes in two strengths: light (4%–5% alcohol; 2 drinks) and strong (6%–10% alcohol; 4 drinks).
Additionally, we asked the drinkers for the age when they first had alcohol, the age when they began consuming alcohol at their current frequency, how much money they typically spent on alcohol on a day that they consumed alcohol, and whether they usually drank alone or with others. We asked all participants whether they smoked any tobacco products, including beedi and cheroot. Interviews were conducted by three men field workers.
Statistical analysis
We categorized continuous variables (e.g. age, years of education, years lived in current residence, amount of money spent) into quartiles. We further dichotomized certain variables based on statistical significance using chi-square test (had ≥10 years of education; lived <15 years in current residence; started drinking at current frequency before age 27 years; and spent >
 100 per day on alcohol).
100 per day on alcohol).
Prevalence of alcohol use among all men was calculated using age-adjusted direct standardization method based on the prevalence of (i) reported drinkers among all men and (ii) hidden drinkers among the primary controls. Likewise, distribution of AUDIT classes among men was calculated using age-adjusted direct standardization method based on AUDIT class distribution of drinkers and hidden drinkers.
The census-wide cross-sectional analysis was done with unconditional logistic regression using reported drinking status as the outcome variable (n=2811). The following variables were tested for inclusion in this analysis: age, area, religion, marital status, education, socioeconomic class and occupation. We obtained ORs and 95% confidence intervals (95% CIs) from the logistic regression. Factors remained in the adjusted model if significant at p<0.20. These estimates were compared to a case–control analysis done on a smaller sample of the population to obtain more information and to further control for confounders using conditional logistic regression (n=440). Matched variables (age and area) were not tested for inclusion, but we tested for additional variables: years of residence, smoking status and GHQ-12 status.
The risk-level analysis was done among 251 cases and 103 hidden drinkers with an ordinal logistic regression using AUDIT class as the outcome variable (n=354). The following additional variables were tested for inclusion in this analysis: hidden drinking (i.e. being reported as a non-drinker in the census), drinking before age 21 years, drinking at current frequency before age 27 years, spending >
 100 on alcohol per day, preferring IMFL and usually drinking alone. Interaction between each variable and hidden drinking status was also tested. Factors remained in the adjusted model if significant at p<0.20 and their interaction with hidden drinking status remained if significant at p<0.10. The final model excluded 40 drinkers who did not report the amount of money spent on alcohol. We used chi-square test to compare the 40 excluded drinkers with those that were included in the analysis.
100 on alcohol per day, preferring IMFL and usually drinking alone. Interaction between each variable and hidden drinking status was also tested. Factors remained in the adjusted model if significant at p<0.20 and their interaction with hidden drinking status remained if significant at p<0.10. The final model excluded 40 drinkers who did not report the amount of money spent on alcohol. We used chi-square test to compare the 40 excluded drinkers with those that were included in the analysis.
RESULTS
Demographics
We screened 2811 men for alcohol use during the census. Their mean (SD) age was 36.2 (14.4) years (median 33, range 18–91) and the mean duration of schooling was 6.0 (4.4) years. The majority were married, from the low socioeconomic class, Hindu and unskilled labourers. Of the 220 case–control pairs, the mean age was 39.8 (12.5) years, mean duration of schooling was 5.5 (4.2) years, and mean duration of living in current residence was 26.4 (15.3) years (Table I). Fifty per cent were smokers and 23% were positive for a CMD.
Table I.
Demographic characteristics of all men by reported drinking status (n=2811) and case–control pairs (n=440)
| Variable | Reported non-drinkers (n=2223) |
Reported drinkers (n=588) |
Controls (n=220) |
Cases (n=220) |
|---|---|---|---|---|
|
| ||||
| n (%) | n (%) | n (%) | n (%) | |
| Age (years)* | ||||
| 18–24 | 678 (30.5) | 34 (5.8) | 18 (8.2) | 18 (8.2) |
| 25–32 | 525 (23.6) | 142 (24.1) | 57 (25.9) | 58 (26.4) |
| 33–45 | 499 (22.4) | 209 (35.5) | 79 (35.9) | 78 (35.5) |
| ≥46 | 521 (23.4) | 203 (34.5) | 66 (30.0) | 66 (30.0) |
| Area | ||||
| Uthramatha Koil | 558 (25.1) | 116 (19.7) | 46 (20.9) | 46 (20.9) |
| Filterbed Medu | 446 (20.1) | 169 (28.7) | 55 (25.0) | 55 (25.0) |
| Devaraj Nagar | 600 (27.0) | 81 (13.8) | 24 (10.9) | 24 (10.9) |
| SSK Maniyam | 255 (11.5) | 100 (17.0) | 40 (18.2) | 40 (18.2) |
| MGR Nagar | 186 (8.4) | 77 (13.1) | 36 (16.4) | 36 (16.4) |
| Bharathiyar Nagar | 178 (8.0) | 45 (7.7) | 19 (8.6) | 19 (8.6) |
| Marital status | ||||
| Single | 858 (38.6) | 63 (10.7) | 43 (19.5) | 30 (13.6) |
| Married | 1304 (58.7) | 513 (87.2) | 171 (77.7) | 189 (85.9) |
| Widowed | 49 (2.2) | 11 (1.9) | 5 (2.3) | 1 (0.5) |
| Divorced or separated | 12 (0.5) | 1 (0.2) | 1 (0.5) | 0 (0.0) |
| Education* | ||||
| No education | 518 (23.3) | 199 (33.8) | 56 (25.5) | 66 (30.0) |
| 1–5 years | 399 (17.9) | 145 (24.7) | 44 (20.0) | 56 (25.5) |
| 6–9 years | 671 (30.2) | 172 (29.3) | 63 (28.6) | 67 (30.5) |
| ≥10 years | 635 (28.6) | 72 (12.2) | 57 (25.9) | 31 (14.1) |
| Socioeconomic status | ||||
| Low | 1381 (62.1) | 439 (74.7) | 128 (58.2) | 167 (75.9) |
| Middle | 776 (34.9) | 145 (24.7) | 85 (38.6) | 51 (23.2) |
| High | 66 (3.0) | 4 (0.7) | 7 (3.2) | 2 (0.9) |
| Religion | ||||
| Hindu | 1568 (70.5) | 521 (88.6) | 172 (78.2) | 198 (90.0) |
| Christian | 184 (8.3) | 46 (7.8) | 22 (10.0) | 15 (6.8) |
| Muslim | 469 (21.1) | 21 (3.6) | 26 (11.8) | 7 (3.2) |
| Others | 2 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Occupation | ||||
| Unemployed | 384 (17.3) | 32 (5.4) | 35 (15.9) | 9 (4.1) |
| Unskilled labourer | 1362 (61.3) | 452 (76.9) | 137 (62.3) | 168 (76.4) |
| Skilled labourer | 367 (16.5) | 96 (16.3) | 37 (16.8) | 42 (19.1) |
| Service-related | 60 (2.7) | 4 (0.7) | 5 (2.3) | 0 (0.0) |
| Business | 44 (2.0) | 4 (0.7) | 6 (2.7) | 1 (0.5) |
| Agriculture-related | 3 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| High income/professional | 3 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Years in current residence* | ||||
| ≤15 | – | – | 41 (18.6) | 77 (35.0) |
| >15, ≤28 | – | – | 59 (26.8) | 57 (25.9) |
| >28, ≤38 | – | – | 57 (25.9) | 49 (22.3) |
| >38 | – | – | 63 (28.6) | 37 (16.8) |
| GHQ-12 positive | – | – | 25 (11.4) | 76 (34.5) |
| Smoker | – | – | 62 (28.2) | 158 (71.8) |
GHQ-12 General Heath Questionnaire (refer to text for definition)
categorized into quartiles among all men
Prevalence of alcohol use and AUDIT class
Of the 2811 men screened for alcohol use, 588 (20.9%) were reported as drinkers. Among the 241 primary controls that were interviewed 81 (33.6%) were found to be drinkers. Based on these prevalences, the age-adjusted overall prevalence (95% CI) of drinkers among men was 46.1% (39.7%–52.5%). Similarly, among all men in Old Town, 19% (15.3%–22.6%) were increased-risk drinkers, 7.7% (4.4%–11.1%) were high-risk drinkers and 4.7% (3.1%–6.3%) were dependent drinkers (Table II). Combined, an estimated 31.4% (27.5%–35.2%) of all men were hazardous drinkers (AUDIT score ≥8).
Table II.
Distribution of AUDIT (Alcohol Use Disorder Identification Test) class among cases, primary hidden drinkers among all men
| AUDIT class (score) | Cases (n=251) n (%) |
Hidden drinkers (n=81) n (%) |
All men (n=2811) Estimated % (95% CI)* |
|---|---|---|---|
| Low risk (0–7) | 84 (33.5) | 20 (24.1) | 14.8 (10.9–18.6) |
| Hazardous (8–40) | 167 (66.5) | 61 (75.3) | 31.4 (27.5–35.2) |
| Increased risk (8–15) | 104 (41.4) | 40 (48.2) | 19.0 (15.3–22.6) |
| High risk (16–19) | 33 (13.1) | 14 (16.9) | 7.7 (4.4–11.1) |
| Dependent (20–40) | 30 (12.0) | 9 (10.8) | 4.7 (3.1–6.3) |
age-adjusted direct standardization
Risk factors of alcohol use
Logistic regression of all men in Old Town identified the following factors to be associated with being a reported drinker: older age, being married, being of low socioeconomic class, being an unskilled labourer (i.e. watchman, manual labourer, porter, shop assistant and launderer) or a skilled labourer (i.e. barber, tailor, driver, carpenter, mason and painter). Certain areas within Old Town were associated with being a reported drinker. Having ≥10 years of education and Muslim religion were protective. Conditional logistic regression of 220 case–control pairs identified the following factors to be associated with drinking: being an unskilled labourer, presence of a CMD and smoking. Muslim religion was protective (Table III).
Table III.
Unadjusted and adjusted odds ratios for reported drinking status among all men (n=2811) and drinking status among case–control pairs (n=440)
| Variable | All men (n=2811)
|
Case–control pairs (n=440)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted
|
Adjusted
|
Unadjusted
|
Adjusted
|
|||||
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Age (years)* | ||||||||
| 18–24 | Reference category | Reference category | ||||||
| 25–32 | 5.39 (3.65–7.98) | <0.001 | 3.07 (1.97–4.76) | <0.001 | ||||
| 33–45 | 8.35 (5.71–12.22) | <0.001 | 3.98 (2.52–6.26) | <0.001 | ||||
| ≥46 | 7.77 (5.31–11.37) | <0.001 | 4.33 (2.74–6.84) | <0.001 | ||||
| Area | ||||||||
| Uthramatha Koil | Reference category | Reference category | ||||||
| Filterbed Medu | 1.82 (1.40–2.38) | <0.001 | 1.88 (1.40–2.54) | <0.001 | ||||
| Devaraj Nagar | 0.65 (0.48–0.88) | 0.006 | 1.27 (0.88–1.82) | 0.198 | ||||
| SSK Maniyam | 1.89 (1.39–2.56) | <0.001 | 1.56 (1.12–2.18) | 0.009 | ||||
| MGR Nagar | 1.99 (1.43–2.78) | <0.001 | 1.87 (1.30–2.68) | <0.001 | ||||
| Bharathiyar Nagar | 1.22 (0.83–1.78) | 0.317 | 1.00 (0.66–1.51) | 0.987 | ||||
| Married | 4.82 (3.73–6.23) | <0.001 | 2.26 (1.65–3.11) | <0.001 | 1.36 (0.93–1.98) | 0.117 | ||
| Ten years or more education† | 0.35 (0.27–0.45) | <0.001 | 0.58 (0.43–0.78) | <0.001 | 0.66 (0.45–0.96) | 0.030 | ||
| Low socioeconomic class | 1.80 (1.46–2.20) | <0.001 | 1.92 (1.51–2.43) | <0.001 | 1.55 (1.14–2.11) | 0.006 | 1.32 (0.97–1.81) | 0.081 |
| Religion | ||||||||
| Hindu | Reference category | Reference category | Reference category | Reference category | ||||
| Christian | 0.75 (0.54–1.06) | 0.099 | 0.70 (0.48–1.02) | 0.064 | 0.76 (0.45–1.28) | 0.300 | 0.84 (0.50–1.42) | 0.508 |
| Muslim | 0.14 (0.09–0.21) | <0.001 | 0.12 (0.07–0.19) | <0.001 | 0.40 (0.19–0.84) | 0.016 | 0.43 (0.20–0.91) | 0.028 |
| Others | – | – | – | – | ||||
| Occupation | ||||||||
| Unemployed | Reference category | Reference category | Reference category | Reference category | ||||
| Unskilled labourer | 3.98 (2.73–5.80) | <0.001 | 2.93 (1.95–4.42) | <0.001 | 2.69 (1.38–5.27) | 0.004 | 2.08 (1.05–4.13) | 0.035 |
| Skilled labourer | 3.14 (2.05–4.80) | <0.001 | 2.97 (1.85–4.77) | <0.001 | 2.60 (1.27–5.34) | 0.009 | 2.04 (0.98–4.28) | 0.058 |
| Service-related | 0.80 (0.27–2.34) | 0.684 | 1.06 (0.35–3.24) | 0.918 | – | – | – | – |
| Business | 1.09 (0.37–3.23) | 0.875 | 1.23 (0.39–3.86) | 0.728 | 0.70 (0.09–5.51) | 0.733 | 0.80 (0.10–6.35) | 0.836 |
| Agriculture-related | – | – | – | – | ||||
| High income/professionals | – | – | – | – | ||||
| Lived ≤15 years in current residence‡ | 1.47 (1.11–1.94) | 0.006 | ||||||
| GHQ-12 positive | 1.77 (1.34–2.34) | <0.001 | 1.50 (1.12–1.99) | 0.006 | ||||
| Smoking | 2.55 (1.90–3.42) | <0.001 | 2.15 (1.58–2.91) | <0.001 | ||||
GHQ-12 General Heath Questionnaire (refer to text for definition)
categorized into quartiles among all men
75th percentile used as cut-off
25th percentile used as cut-off
Final model adjusted for socioeconomic class, religion, occupation, GHQ-12 and smoking
Characteristics of drinkers
Of the 251 cases and 103 hidden drinkers, mean (SD) age at first drink was 22.3 (8.0) years, mean age to begin drinking at current frequency was 28.4 (8.3) years, and mean amount of money spent on alcohol on a typical day when drinking was
 148 (120). The majority of drinkers consumed IMFL as the main type of alcohol (Table IV).
148 (120). The majority of drinkers consumed IMFL as the main type of alcohol (Table IV).
Table IV.
Characteristics of cases (n=251) and hidden drinkers (n=103) by AUDIT class
| Variable | Cases
|
Hidden drinkers
|
||||||
|---|---|---|---|---|---|---|---|---|
| Low risk (n=84) |
Increased risk (n=104) |
High risk (n=33) |
Dependent (n=30) |
Low risk (n=23) |
Increased risk (n=43) |
High risk (n=19) |
Dependent (n=18) |
|
|
| ||||||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Age (years)* | ||||||||
| 18–24 | 8 (9.5) | 8 (7.7) | 1 (3.0) | 2 (6.7) | 3 (13.0) | 1 (2.3) | 1 (5.3) | 1 (5.6) |
| 25–32 | 21 (25.0) | 28 (26.9) | 8 (24.2) | 6 (20.0) | 7 (30.4) | 7 (16.3) | 4 (21.1) | 3 (16.7) |
| 33–45 | 30 (35.7) | 40 (38.5) | 6 (18.2) | 15 (50.0) | 7 (30.4) | 18 (41.9) | 7 (36.8) | 5 (27.8) |
| ≥46 | 25 (29.8) | 28 (26.9) | 18 (54.5) | 7 (23.3) | 6 (26.1) | 17 (39.5) | 7 (36.8) | 9 (50.0) |
| Area | ||||||||
| Uthramatha Koil | 18 (21.4) | 15 (14.4) | 9 (27.3) | 8 (26.7) | 1 (4.3) | 8 (18.6) | 4 (21.1) | 4 (22.2) |
| Filterbed Medu | 24 (28.6) | 34 (32.7) | 5 (15.2) | 4 (13.3) | 13 (56.5) | 14 (32.6) | 3 (15.8) | 3 (16.7) |
| Devaraj Nagar | 11 (13.1) | 11 (10.6) | 3 (9.1) | 2 (6.7) | 2 (8.7) | 4 (9.3) | 4 (21.1) | 1 (5.6) |
| SSK Maniyam | 11 (13.1) | 25 (24.0) | 6 (18.2) | 2 (6.7) | 0 (0.0) | 9 (20.9) | 5 (26.3) | 4 (22.2) |
| MGR Nagar | 10 (11.9) | 16 (15.4) | 7 (21.2) | 7 (23.3) | 4 (17.4) | 4 (9.3) | 1 (5.3) | 5 (27.8) |
| Bharathiyar Nagar | 10 (11.9) | 3 (2.9) | 3 (9.1) | 7 (23.3) | 3 (13.0) | 4 (9.3) | 2 (10.5) | 1 (5.6) |
| Marital status | ||||||||
| Single | 12 (14.3) | 15 (14.4) | 4 (12.1) | 2 (6.7) | 5 (21.7) | 4 (9.3) | 4 (21.1) | 3 (16.7) |
| Married | 71 (84.5) | 89 (85.6) | 29 (87.9) | 27 (90.0) | 18 (78.3) | 38 (88.4) | 15 (78.9) | 15 (83.3) |
| Widowed | 1 (1.2) | 0 (0.0) | 0 (0.0) | 1 (3.3) | 0 (0.0) | 1 (2.3) | 0 (0.0) | 0 (0.0) |
| Education* | ||||||||
| No education | 23 (27.4) | 36 (34.6) | 12 (36.4) | 9 (30.0) | 5 (21.7) | 8 (18.6) | 7 (36.8) | 8 (44.4) |
| 1–5 years | 19 (22.6) | 25 (24.0) | 11 (33.3) | 5 (16.7) | 5 (21.7) | 12 (27.9) | 3 (15.8) | 3 (16.7) |
| 6–9 years | 22 (26.2) | 33 (31.7) | 9 (27.3) | 13 (43.3) | 7 (30.4) | 15 (34.9) | 8 (42.1) | 6 (33.3) |
| 10 years or more | 20 (23.8) | 10 (9.6) | 1 (3.0) | 3 (10.0) | 6 (26.1) | 8 (18.6) | 1 (5.3) | 1 (5.6) |
| Socioeconomic class | ||||||||
| Low | 60 (71.4) | 79 (76.0) | 26 (78.8) | 20 (66.7) | 12 (52.2) | 29 (67.4) | 17 (89.5) | 14 (77.8) |
| Middle | 23 (27.4) | 25 (24.0) | 7 (21.2) | 9 (30.0) | 10 (43.5) | 14 (32.6) | 2 (10.5) | 4 (22.2) |
| High | 1 (1.2) | 0 (0.0) | 0 (0.0) | 1 (3.3) | 1 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Religion | ||||||||
| Hindu | 77 (91.7) | 89 (85.6) | 33 (100.0) | 28 (93.3) | 17 (73.9) | 34 (79.1) | 16 (84.2) | 14 (77.8) |
| Christian | 4 (4.8) | 13 (12.5) | 0 (0.0) | 0 (0.0) | 5 (21.7) | 6 (14.0) | 1 (5.3) | 2 (11.1) |
| Muslim | 3 (3.6) | 2 (1.9) | 0 (0.0) | 2 (6.7) | 1 (4.3) | 3 (7.0) | 2 (10.5) | 2 (11.1) |
| Occupation | ||||||||
| Unemployed | 3 (3.6) | 3 (2.9) | 2 (6.1) | 2 (6.7) | 3 (13.0) | 6 (14.0) | 3 (15.8) | 2 (11.1) |
| Unskilled labourer | 65 (77.4) | 79 (76.0) | 26 (78.8) | 25 (83.3) | 1 (4.3) | 1 (2.3) | 0 (0.0) | 1 (5.6) |
| Skilled labourer | 16 (19.0) | 21 (20.2) | 5 (15.2) | 3 (10.0) | 18 (78.3) | 30 (69.8) | 16 (84.2) | 15 (83.3) |
| Business | 0 (0.0) | 1 (1.0) | 0 (0.0) | 0 (0.0) | 1 (4.3) | 6 (14.0) | 0 (0.0) | 0 (0.0) |
| Years lived in current residence* | ||||||||
| ≤15 | 35 (41.7) | 34 (32.7) | 3 (9.1) | 15 (50.0) | 3 (13.0) | 7 (16.3) | 4 (21.1) | 4 (22.2) |
| >15, ≤28 | 19 (22.6) | 26 (25.0) | 13 (39.4) | 6 (20.0) | 7 (30.4) | 10 (23.3) | 4 (21.1) | 4 (22.2) |
| >28, ≤38 | 18 (21.4) | 20 (19.2) | 11 (33.3) | 5 (16.7) | 7 (30.4) | 14 (32.6) | 3 (15.8) | 3 (16.7) |
| >38 | 12 (14.3) | 24 (23.1) | 6 (18.2) | 4 (13.3) | 6 (26.1) | 12 (27.9) | 8 (42.1) | 7 (38.9) |
| GHQ-12 positive | 14 (16.7) | 38 (36.5) | 18 (54.5) | 17 (56.7) | 2 (8.7) | 6 (14.0) | 3 (15.8) | 8 (44.4) |
| Smoking | 49 (58.3) | 78 (75.0) | 24 (72.7) | 28 (93.3) | 9 (39.1) | 29 (67.4) | 12 (63.2) | 15 (83.3) |
| Money spent on alcohol on typical day | ||||||||
≤
 100 100 |
67 (79.8) | 58 (55.8) | 16 (48.5) | 6 (20.0) | 14 (60.9) | 21 (48.8) | 7 (36.8) | 6 (33.3) |
>
 100 100 |
8 (9.5) | 40 (38.5) | 16 (48.5) | 23 (76.7) | 4 (17.4) | 14 (32.6) | 8 (42.1) | 6 (33.3) |
| Declined to answer | 9 (10.7) | 6 (5.8) | 1 (3.0) | 1 (3.3) | 5 (21.7) | 8 (18.6) | 4 (21.1) | 6 (33.3) |
| Preferred type of alcohol | ||||||||
| IMFL | 75 (89.3) | 100 (96.2) | 33 (100.0) | 29 (96.7) | 18 (78.3) | 42 (97.7) | 19 (100.0) | 17 (94.4) |
| Beer | 9 (10.7) | 4 (3.8) | 0 (0.0) | 0 (0.0) | 5 (21.7) | 1 (2.3) | 0 (0.0) | 0 (0.0) |
| Illicitly distilled | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5.6) |
| Usually drinks alone | 40 (47.6) | 57 (54.8) | 19 (57.6) | 14 (46.7) | 10 (43.5) | 23 (53.5) | 11 (57.9) | 9 (50.0) |
| Mean (SD) age (years) at first drink | 25.5 (8.6) | 20.8 (7.9) | 18.8 (7.4) | 18.9 (5.4) | 22.8 (5.7) | 24.9 (7.9) | 22.7 (7.8) | 21.2 (7.1) |
| Mean (SD) age (years) when started drinking at current frequency | 29.6 (8.6) | 28.5 (8.5) | 27.9 (8.9) | 25.4 (8.4) | 26.9 (6.0) | 28.9 (7.7) | 26.5 (7.2) | 29.8 (10.0) |
Mean (SD) money spent (
 ) on alcohol in a typical day in the past 12 months ) on alcohol in a typical day in the past 12 months |
101 (73) | 161 (143) | 153 (106) | 214 (120) | 123 (104) | 131 (62) | 173 (143) | 224 (181) |
categorized into quartiles among all men
GHQ-12 General Heath Questionnaire (refer to text for definition)
IMFL Indian-made foreign liquor (refer to text for definition)
Risk factors of higher AUDIT class
Ordinal regression of 354 drinkers (251 cases and 103 hidden drinkers) identified the following factors to be associated with higher AUDIT class in the final adjusted model: being a hidden drinker, presence of a CMD, smoking, drinking before legal age of 21 years, spending >
 100 per day on alcohol and preferring IMFL. Living in one of the areas was found to be protective against higher AUDIT class. We also found a weak protective interaction between spending >
100 per day on alcohol and preferring IMFL. Living in one of the areas was found to be protective against higher AUDIT class. We also found a weak protective interaction between spending >
 100 and hidden drinking status. Those who did not report their spending were more likely to be a hidden drinker (p<0.001) and a non-smoker (p=0.001), but otherwise they were not statistically different from those who reported their spending (Table V).
100 and hidden drinking status. Those who did not report their spending were more likely to be a hidden drinker (p<0.001) and a non-smoker (p=0.001), but otherwise they were not statistically different from those who reported their spending (Table V).
Table V.
Unadjusted and adjusted odds ratios for higher AUDIT class among cases and hidden drinkers (n=354)
| Variable | Unadjusted
|
Adjusted (n=314)
|
||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Hidden drinker* | 1.69 (1.11–2.57) | 0.015 | 3.96 (2.04–7.68) | <0.001 |
| Age (years)† | ||||
| 18–24 | Reference category | |||
| 25–32 | 1.45 (0.63–3.33) | 0.379 | ||
| 33–45 | 1.72 (0.77–3.82) | 0.184 | ||
| ≥46 | 2.13 (0.95, –4.76) | 0.066 | ||
| Area | ||||
| Uthramatha Koil | Reference category | Reference category | ||
| Filterbed Medu | 0.48 (0.27–0.85) | 0.012 | 0.48 (0.25–0.93) | 0.029 |
| Devaraj Nagar | 0.63 (0.30–1.32) | 0.220 | 0.96 (0.41–2.26) | 0.931 |
| SSK Maniyam | 0.95 (0.51–1.79) | 0.883 | 1.06 (0.51–2.20) | 0.876 |
| MGR Nagar | 1.11 (0.58–2.13) | 0.759 | 1.09 (0.53–2.24) | 0.818 |
| Bharathiyar Nagar | 0.85 (0.40–1.82) | 0.679 | 0.93 (0.41–2.12) | 0.866 |
| Married | 1.19 (0.70–2.05) | 0.519 | ||
| Ten years or more education‡ | 0.33 (0.19–0.60) | <0.001 | ||
| Low socioeconomic class | 1.36 (0.89–2.09) | 0.161 | ||
| Low socioeconomic class × hidden drinker§ | 2.48 (0.97–6.32) | 0.057 | ||
| Religion | ||||
| Hindu | Reference category | |||
| Christian | 0.69 (0.35–1.37) | 0.291 | ||
| Muslim | 1.58 (0.62–4.04) | 0.343 | ||
| Occupation | ||||
| Unemployed | Reference category | |||
| Unskilled labourer | 0.99 (0.40–2.42) | 0.981 | ||
| Skilled labourer | 0.77 (0.29–2.08) | 0.611 | ||
| Business | 1.14 (0.16–8.29) | 0.900 | ||
| Lived ≤15 years in current residence‖ | 0.78 (0.51–1.19) | 0.250 | ||
| GHQ-12 positive | 2.97 (1.93–4.56) | <0.001 | 3.83 (2.34–6.28) | <0.001 |
| Smoking | 2.46 (1.60–3.77) | <0.001 | 1.78 (1.07–2.94) | 0.026 |
| Drink before 21** | 2.58 (1.73–3.82) | <0.001 | 2.71 (1.70–4.32) | <0.001 |
| Drinking current frequency before 27†† | 1.21 (0.83–1.77) | 0.328 | ||
Spend more than
 100/day†† 100/day††
|
4.63 (2.94–7.29) | <0.001 | 6.17 (3.48–10.92) | <0.001 |
Spend more than
 100/day × hidden drinker§ 100/day × hidden drinker§
|
0.38 (0.14–0.98) | 0.046 | 0.38 (0.14–1.04) | 0.059 |
| Mainly drinks IMFL | 4.88 (1.96–12.17) | <0.001 | 5.45 (1.86–15.99) | 0.002 |
| Usually drinks alone | 1.17 (0.80–1.71) | 0.431 | 1.44 (0.92–2.26) | 0.109 |
GHQ-12 General Heath Questionnaire (refer to text for definition)
IMFL Indian-made foreign liquor (refer to text for definition)
drinker who was initially not reported as a drinker during the census
categorized into quartiles among all men
75th percentile used as cut-off
adjusted for main effects of the two variables. Only interactions that were significant at p<0.10 are shown
25th percentile used as cut-off
legal drinking age in Tamil Nadu
median used as cut-off
Final model adjusted for hidden status, area, GHQ-12, smoking, underage drinking, money spent, money spent × hidden status, preferring IMFL, and drinking alone
DISCUSSION
We examined the use of alcohol in an urban slum community in Vellore, Tamil Nadu. The strengths of our study include the age-and area-matched sampling strategy, and the use of an objective, reliable and standard measure of alcohol use. We have identified a number of risk factors for alcohol use and hazardous use. To the best of our knowledge, this is the first study to describe the nature, prevalence and risk factors of alcohol use and hazardous use in an urban slum community in Tamil Nadu.
We found that half of the men in Old Town consumed alcohol, and that over one-third drank hazardously. These are much higher estimates compared to a previous study from rural Vellore.9 The prevalence of hazardous use was much higher than those reported in an urban slum in Kolkata and Goa, while prevalence of alcohol use was lower than both.10,11 This suggests an alarmingly high prevalence of hazardous use among drinkers in Old Town. With such a high prevalence of hazardous drinking, a community-wide intervention programme may be appropriate to raise awareness and to start counselling hazardous drinkers. Other slum communities in southern India may also have a higher prevalence of hazardous use, and further studies on alcohol use in southern India should be done.
We identified factors associated with alcohol use using two methods: a census-wide cross-sectional analysis and a matched case–control analysis. The census-wide analysis allowed us to examine the effect of age and area on drinking status, while the case–control analysis enabled us to investigate additional variables while reducing confounding associated with age and area. Almost all factors tested in the census-wide analysis were significant even in the adjusted model, while certain factors, namely marriage, education and socioeconomic class were not significant in the adjusted case–control model. The discrepancy may be due to the difference in the reporter (household representative v. self). Household representatives of men who are better educated or of higher socioeconomic class may under-report drinkers in their households due to a social desirability bias, while men who are married may be more likely to be reported as drinkers by their wives. Additionally, effects of religion and occupation remained significant in the case–control analysis, although they were attenuated due to a smaller sample size and power. The census-wide analysis does not account for hidden drinkers and grossly underestimates the prevalence of alcohol use, which indicates that future studies of alcohol use in similar populations should not rely solely on household-level surveys.
We also determined several important factors associated with higher-risk drinking in the urban slum community. We found that drinkers who were initially reported as non-drinkers during the census (i.e. hidden drinkers) were more likely to have higher AUDIT classifications than those who were initially reported as drinkers. This may reflect the population’s tendency to under-report harmful drinking, reinforcing the notion that household-level surveys on alcohol use may not be reliable.
Drinking before the legal age was associated with higher AUDIT class, suggesting a need for better enforcement of laws prohibiting alcohol access to underage drinkers. Preference of IMFL as a risk factor for hazardous use is consistent with the rural study in Vellore.9 Clearly there is a need for a population-based intervention and a more effective implementation of existing regulation to limit the availability of IMFL. However, since the government generates a large amount of revenue through taxation on IMFL, the politics of alcohol in India is very complex.18 Further studies are necessary to determine effective ways to reduce IMFL consumption and hazardous use.
Drinkers typically spend >
 100 on alcohol on days that they drink.
100 on alcohol on days that they drink.
 100 represents a major portion of the average daily wage in the community, and thus alcohol use makes an impact on household finances. As our study shows, a strong association between spending >
100 represents a major portion of the average daily wage in the community, and thus alcohol use makes an impact on household finances. As our study shows, a strong association between spending >
 100 per day on alcohol and hazardous drinking implies significant economic burden on households with hazardous drinkers. Reduction and prevention of hazardous drinking may alleviate some of the economic burden of these communities. The weak protective interaction between spending >
100 per day on alcohol and hazardous drinking implies significant economic burden on households with hazardous drinkers. Reduction and prevention of hazardous drinking may alleviate some of the economic burden of these communities. The weak protective interaction between spending >
 100 and being a hidden drinker may be due to under-reporting of the amount spent by hidden drinkers. This is consistent with the fact that a significantly higher proportion of hidden drinkers declined to answer how much they spent on alcohol.
100 and being a hidden drinker may be due to under-reporting of the amount spent by hidden drinkers. This is consistent with the fact that a significantly higher proportion of hidden drinkers declined to answer how much they spent on alcohol.
Additionally, the fact that CMD is a risk factor of higher AUDIT is consistent with a previous study from Goa.11 This implies the need for a thorough assessment of mental health issues for those who drink alcohol and seek medical attention. Furthermore, it suggests the need to decrease hazardous alcohol use to lower the incidence of CMDs.
There are several important limitations to our study. First, drinking status was self-reported. If the high prevalence of hidden drinkers were an indication, the overall prevalence of alcohol use may be underestimated. We were not able to consider any biological factors (e.g. genetic factor, family history and comorbid conditions). Finally, our study is limited by its cross-sectional nature and thus causality cannot be ascertained. A longitudinal cohort study would be needed to assess and confirm predictors of hazardous alcohol use in India.
Our study indicates an urgent need for a population-wide intervention programme that discourages under-aged men from drinking alcohol and regulates access to IMFL. Further studies are needed to determine effective approaches to reduce harmful effects of hazardous alcohol use.
Acknowledgments
We acknowledge and thank Dr Gagandeep Kang of Christian Medical College, Vellore, for her mentorship and guidance; Dr Florin Vaida of University of California, San Diego for his statistical expertise, and Dr Victoria Ojeda of University of California, San Diego for her feedback on the manuscript. We also thank all the staff and faculty at CMCs LCECU and Community Health and Development, including Rajiv Sarkar, Suresh Kumar, Augustine Franklin, Karthikeyan and Dr Ruby Karl, for helping with various aspects of this study. This work was supported by the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental and Craniofacial Research, National Institute on Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases, and National Institutes of Health Office of Women’s Health and Research through the Fogarty International Clinical Research Scholars and Fellows Program at Vanderbilt University (R24 TW007988) and the American Relief and Recovery Act.
Contributor Information
SUNMIN KIM, University of California, San Diego School of Medicine, La Jolla, CA 92092, USA.
SAMARA RIFKIN, Vanderbilt University School of Medicine, USA.
SUSHIL MATHEW JOHN, Christian Medical College, Vellore, Tamil Nadu, India - Low Cost Effective Care Unit.
K.S. JACOB, Department of Psychiatry
References
- 1.World Health Organization. Global status report on alcohol and health: India profile. Geneva: WHO; 2011. pp. 1–286. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/ind.pdf (accessed on 17 Aug 2012) [Google Scholar]
- 2.Das SK, Balakrishnan V, Vasudevan DM. Alcohol: Its health and social impact in India. Natl Med J India. 2006;19:94–9. [PubMed] [Google Scholar]
- 3.World Health Organization. Burden and socio-economic impact of alcohol: The Bangalore study. New Delhi: WHO, Regional Office for South-East Asia; 2006. p. 72. Available at http://www.searo.who.int/LinkFiles/Alcohol_and_Substance_abuse_Bangalore-Study.pdf (accessed on 17 Aug 2012) [Google Scholar]
- 4.Prasad R. Alcohol use on the rise in India. Lancet. 2009;373:17–18. doi: 10.1016/s0140-6736(08)61939-x. [DOI] [PubMed] [Google Scholar]
- 5.Obot IS, Room R. Alcohol, gender and drinking problems: Perspectives from low and middle income countries. Geneva: World Health Organization; 2005. pp. 1–227. Department of Mental Health and Substance Abuse. [Google Scholar]
- 6.Rao KN, Begum S, Venkataramana V, Gangadharappa N. Nutritional neglect and physical abuse in children of alcoholics. Indian J Pediatr. 2001;68:843–5. doi: 10.1007/BF02762109. [DOI] [PubMed] [Google Scholar]
- 7.Bhatt RV. Domestic violence and substance abuse. Int J Gynaecol Obstet. 1998;63(Suppl 1):S25–S31. doi: 10.1016/s0020-7292(98)00181-7. [DOI] [PubMed] [Google Scholar]
- 8.Nayak MB, Patel V, Bond JC, Greenfield TK. Partner alcohol use, violence and women’s mental health: Population-based survey in India. Br J Psychiatry. 2010;196:192–9. doi: 10.1192/bjp.bp.109.068049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.John A, Barman A, Bal D, Chandy G, Samuel J, Thokchom M, et al. Hazardous alcohol use in rural southern India: Nature, prevalence and risk factors. Natl Med J India. 2009;22:123–5. [PubMed] [Google Scholar]
- 10.Ghosh S, Samanta A, Mukherjee S. Patterns of alcohol consumption among male adults at a slum in Kolkata, India. J Health Popul Nutr. 2012;30:73–81. doi: 10.3329/jhpn.v30i1.11279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D’Costa G, Nazareth I, Naik D, Vaidya R, Levy G, Patel V, King M. Harmful alcohol use in Goa, India, and its associations with violence: A study in primary care. Alcohol Alcohol. 2007;42:131–7. doi: 10.1093/alcalc/agl103. [DOI] [PubMed] [Google Scholar]
- 12.Gladstone BP, Muliyil JP, Jaffar S, Wheeler JG, Le Fevre A, Iturriza-Gomara M, et al. Infant morbidity in an Indian slum birth cohort. Arch Dis Child. 2008;93:479–84. doi: 10.1136/adc.2006.114546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldberg DP. The detection of psychiatric illness by questionnaire: A technique for the identification and assessment of non-psychotic psychiatric illness. Oxford: Oxford University Press; 1972. pp. 1–156. [Google Scholar]
- 14.Goldberg D, Williams P. A user’s guide to the General Health Questionnaire. London: NFER-Nelson; 1991. pp. 1–129. [Google Scholar]
- 15.Kuruvilla A, Pothen M, Philip K, Braganza D, Joseph A, Jacob KS. The validation of the Tamil version of the 12 item general health questionnaire. Indian J Psychiatry. 1999;41:217–21. [PMC free article] [PubMed] [Google Scholar]
- 16.John S, Vijaykumar C, Jayaseelan V, Jacob KS. Validation and usefulness of the Tamil version of the GHQ-12 in the community. Br J Community Nurs. 2006;11:382–6. doi: 10.12968/bjcn.2006.11.9.21760. [DOI] [PubMed] [Google Scholar]
- 17.Babor T, Higgins-Biddle JC, Saunders JB, Monteirs MG. AUDIT: The alcohol use disorders identification test: Guidelines for use in primary care. 2nd. Geneva: World Health Organization; 2001. pp. 1–39. Department of Mental Health and Substance Dependence. Available at http://whqlibdoc.who.int/hq/2001/who_msd_msb_01.6a.pdf (accessed on 17 Aug 2012) [Google Scholar]
- 18.Jacob KS. Alcohol and public health policies in India. Natl Med J India. 2010;23:224–5. [PubMed] [Google Scholar]


