Abstract
Stigma shapes all aspects of HIV prevention and treatment, yet there are limited data on how HIV-infected youth and their families are affected by stigma in sub-Saharan Africa. The authors conducted a qualitative study using focus group discussions among 39 HIV-infected adolescents receiving care at HIV clinics in western Kenya and 53 caregivers of HIV-infected children. Participants felt that while knowledge and access to treatment were increasing, many community members still held negative and inaccurate views about HIV, including associating it with immorality and believing in transmission by casual interactions. Stigma was closely related to a loss of social and economic support but also included internalized negative feelings about oneself. Participants identified treatment-related impacts of stigma, including nonadherence, nondisclosure of status to child or others, and increased mental health problems. Qualitative inquiry also provided insights into how to measure and reduce stigma among affected individuals and families.
Keywords: HIV, stigma, adolescents, caregivers, resource-limited setting
Introduction
For people living with HIV, HIV/AIDS-related stigma (H/A stigma) shapes all aspects of HIV treatment, including delayed HIV testing and enrollment in care,1–3 increased barriers to access and retention in HIV care,4–6 nonadherence to medications,7–10 and increased transmission risk through unsafe sex and nondisclosure to sexual partners.11,12 Furthermore, stigma-related experiences like social rejection, discrimination, and physical violence increase the risk for psychological problems among HIV-infected individuals, which may also hamper treatment behaviors.13,14 Several studies among adults have found an association between H/A stigma and self-reported depression symptoms, anxiety, and hopelessness and decreased quality of life.13,15–17
There are fewer data on how H/A stigma affects the world’s 3.2 million HIV-infected children, of whom over 90% live in sub-Saharan Africa (SSA)18 as well as the 5 million HIV-infected youth aged 15 to 24.19 A few studies among HIV-infected youth highlight experiences of H/A stigma from peers at school in the form of taunting, gossiping, or bullying, because of either their own status or the status of a family member,20–23 which may lead to problems in school attendance or accessing peer support networks.24–26 Physical characteristics of HIV infection (eg, stunted growth and delayed bodily development) and HIV treatment (eg, lipodystrophy resulting in body fat changes) may be additional, important sources of stress and anxiety for HIV-infected children and adolescents that lead to social isolation from peers,25,27 but these experiences have not been well characterized.
Even less is known about the impact of H/A stigma for the family units of HIV-infected children.28 In SSA, it is estimated that 50% of orphans with AIDS are now adolescents,29 with many being cared for by uninfected relatives and extended family members.30 Some data suggest that H/A stigma and discrimination experienced at the caregiver level (whether the caregiver is HIV infected or not) negatively impact HIV-infected children,31–33 including delays in giving children medicines or taking them to clinic.34–36 HIV/AIDS-related stigma has been hypothesized to exacerbate poverty, malnutrition, and access to services for HIV-affected families, but there are few data examining these issues.37,38 Reliable and valid stigma measures are essential to assess the impact of H/A stigma on HIV prevention and treatment and to evaluate stigma-reduction strategies, yet few validated instruments exist.39,40 Although several instruments have been tested for use among HIV-infected adults, they have not been validated for HIV-infected children and adolescents and their families in SSA.41–43
The objective of the following study was to characterize how HIV-infected adolescents and their caregivers understood, experienced, and were impacted by H/A stigma as well as their perspectives on how to measure and intervene to reduce H/A stigma. To do so, we solicited perspectives using focus group discussions (FGDs) with infected adolescents and caregivers enrolled in a large HIV treatment program—the Academic Model Providing Access to Healthcare (AMPATH)—in western Kenya. Our long-term goal is to use these preliminary data to inform the construction of an H/A stigma measurement tool for use among HIV-infected children and their families in Kenya.
Methods
Setting
Study participants were recruited from AMPATH HIV clinics in western Kenya. A collaboration of Moi University School of Medicine, Moi Teaching and Referral Hospital (MTRH), and a consortium of North American academic medical centers, AMPATH is led by the Indiana University School of Medicine.44,45 Through a network of 58 government health facilities in 19 districts across western Kenya, AMPATH provides comprehensive HIV care and treatment that is largely free to the patients, as well as chronic disease management, primary healthcare services, and nutritional support. Since its inception, AMPATH has enrolled over 156 000 HIV-infected or exposed individuals, including over 35 000 children, and initiated 90 000 of these patients on antiretroviral therapy (ART). In February 2014, at the time of this study, AMPATH was actively following over 5867 children under 15 years of age on ART. Participants for this study were recruited from 3 AMPATH clinics—MTRH (an urban clinic following 1254 children), Kitale Health Centre (a semiurban clinic following 706 children), and Burnt Forest Rural Health Centre (a rural clinic following 165 children).
Study Design
We conducted a qualitative study using FGDs with HIV-infected adolescents aged 10 to 15 years who knew their HIV status and with caregivers (infected or uninfected) of HIV-infected children. Adolescents and caregivers were recruited separately, and the adolescent participants did not necessarily represent the children of caregiver participants. No further considerations, such as gender or relation of caregiver, were made while structuring the groups. Convenience sampling was employed to recruit study participants, who were referred to the study team by clinicians, nurses, and other clinic personnel, or self-referred through study fliers placed at participating clinics. Participants provided written informed consent prior to participation in an FGD, with adolescent participants required to provide both assent for themselves and consent from a caregiver. All participants completed a short, interviewer-administered questionnaire of basic demographic and clinical characteristics before the FGD.
A total of 11 FGDs were held between February 11, 2014, and April 17, 2014. Focus group discussions were audiotaped and led by a trained facilitator in Kiswahili, 1 of the 2 national languages of Kenya and the most widely spoken language in western Kenya. Each FGD lasted approximately 2 hours. The facilitator used semistructured interview guides containing open-ended questions to guide discussions (interview guides provided by authors upon request). The interview guides were created by the authors, with questions informed by grounded theory, input from local healthcare providers, and a systematic review of relevant literature.46 Separate interview guides were used for adolescent and caregiver FGDs; however, both covered similar themes including community and cultural beliefs about HIV, experiences of H/A stigma and discrimination, strategies for H/A stigma measurement, and potential interventions to reduce H/A stigma. For analysis, the FGD recordings were transcribed and translated into English by a trained translator. This study was approved by the institutional review board of Indiana University School of Medicine in Indianapolis, Indiana, and by the institutional research and ethics committee of Moi University School of Medicine and MTRH in Eldoret, Kenya.
Data Analysis
The FGD transcripts were analyzed to arrive at a contextualized understanding of adolescent and caregiver perspectives on H/A stigma in this setting. A priori codes were created prior to data analysis. These codes emanated from the interview guide and were used as a starting point for analysis. We then employed constant comparison, axial coding, and triangulation to identify central concepts.47,48 The initial stage of constant comparative analysis was done through coding by 2 investigators (M.L.S. and R.C.V). Line-by-line analysis of each transcribed page from FGD was completed to elucidate the meanings and processes around H/A stigma in this setting. Lines were coded individually by the investigators using the qualitative analysis software Dedoose—a Web application for managing, analyzing, and presenting qualitative and mixed method research data.49 The same 2 investigators independently extracted and compared themes to high degrees of agreement between the open codes and the themes extracted (agreement >90%). Three investigators (M.L.S., M.S.M., and L.J.F.) performed axial coding—the process of relating categories to their subcategories and linking them together at the level of properties and dimensions47,48—to organize themes into relevant relationships. Relevant themes and concepts were developed inductively from the data. Quotes are provided in text to add descriptive detail and highlight major themes.
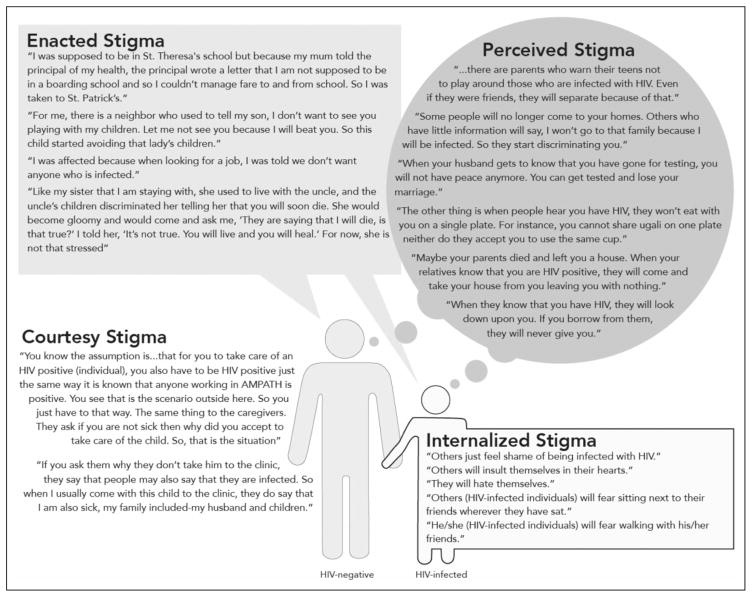
To further analyze and organize our data in this setting, we used previously published models on the ways in which H/A stigma may impact HIV-infected individuals and health outcomes. Prior work proposes 3 distinct types of H/A stigma or stigma mechanisms: (1) “perceived stigma”—the belief among HIV-infected individuals that stigma and discrimination might or will occur, (2) “enacted stigma”—the belief among HIV-infected individuals that stigma and discrimination have occurred, and (3) “internalized stigma”—negative beliefs among HIV-infected individuals about themselves due to their status.50,51 Within a family unit, an additional mechanism has been proposed called “courtesy stigma”—H/A stigma directed at an uninfected individual who is associated with or caring for an HIV-infected person (eg, a child).52 We used these potential mechanisms to guide parts of our analysis and further explore how H/A stigma operated at the level of the child and family in this setting.
Results
Study Participants’ Characteristics
Thirty-nine adolescents participated in 5 FGDs (n = 6–11), and 53 caregivers participated in 6 FGDs (n = 5–12). Mean age of adolescents was 13 years, most were female, and almost all were currently on ART (Table 1). Over 25% of the adolescent participants were complete orphans—that is, lost both parents. Only 23% of adolescents reported telling another person about their HIV status. Mean age of caregiver participants was 40 years and roughly half were the biological mother of an HIV-infected child (51%). A majority of caregivers reported telling at least one other person about the child’s HIV status, mostly another family member (88%).
Table 1.
Study Participant Characteristics.
| Mean (Standard Deviation) or Frequency Count (%) | |
|---|---|
| Adolescent participants, n = 40 | |
| Age, years | 13 (1.3) |
| Gender | |
| Female | 28 (70%) |
| With whom does the child live? | |
| Mother only | 12 (31%) |
| Aunt/uncle | 7 (18%) |
| Grandparent | 6 (15%) |
| Mother and father | 3 (8%) |
| Father only | 3 (8%) |
| Other (eg, sibling, other relative, children’s home) | 8 (20%) |
| Orphan status | |
| Both parents alive | 12 (31%) |
| Both parents dead | 11 (28%) |
| Only father alive | 9 (23%) |
| Only mother alive | 7 (18%) |
| On ARV medications | |
| Yes | 37 (95%) |
| Have you told anyone else about your HIV status? | |
| Yes | 9 (23%) |
| Caregiver participants, n = 53 | |
| Age, years | 40 (11.1) |
| Gender | |
| Female | 44 (83%) |
| Age of child, years | 11 (2.7) |
| Relationship to child | |
| Mother | 27 (51%) |
| Aunt/uncle | 10 (19%) |
| Father | 7 (12%) |
| Grandparent | 3 (6%) |
| Sibling | 3 (6%) |
| Other | 3 (6%) |
| Child on ARV medications | |
| Yes | 50 (94%) |
| Child knows their HIV status | |
| Yes | 27 (51%) |
| Have you told anyone else about child’s HIV status? | |
| Yes | 43 (81%) |
| Who knows the child’s HIV status? | |
| Family member(s) | 47 (88%) |
| Close friend(s) or neighbor(s) | 18 (34%) |
| Teacher(s)/principal(s) | 12 (23%) |
| Pastor(s) | 5 (9%) |
Abbreviation: ARV, antiretroviral.
Community Beliefs about HIV
Participants reported that knowledge about HIV, its treatment, and its transmission was increasing in community settings. Participants largely credited churches, healthcare providers, schools, village meetings or mbaraza, and word-of-mouth as venues through which people received information about HIV in the community, but the media was by far the most commonly cited source of information about HIV. Common media sources included radio, TV, billboards, and the Internet. Adolescent participants especially highlighted social media outlets where information about HIV was available, including Facebook and Twitter.
Even though knowledge was increasing, participants noted that negative beliefs and misinformation about HIV were still common in the community. Immorality, particularly sexual immorality, was often associated with a diagnosis of HIV. Many participants also described community members using religion to explain HIV infection. One caretaker said, “In the church, they know that the disease gets those who have sinned. As a result, they take the disease as a punishment.” Participants discussed the large amount of misinformation in the community around HIV transmission. Specifically, caregivers and adolescents reported that casual contact, such as “using the same plate” or “sharing a cup,” was still thought to transmit HIV. They noted that HIV-infected children are often isolated at meal times, as others “do not want to take food [with them].” Caretakers also noted that HIV-infected children were not allowed to play with uninfected children out of fear that transmission would occur.
Finally, although HIV treatment was generally believed by community members to improve the health and survival of those with HIV, participants reported that many people in the community still viewed HIV as a death sentence. One adolescent stated, “Others will say it is the end of life.” A caregiver also noted, “When you have the disease, you no longer have life; they look at you as someone who is already dead.” Interestingly, several caregivers noted that some community members resented the availability of HIV treatment, as it allows HIV-infected individuals to appear healthy and hide their infection status. One caregiver said, “If you grow fat, they will still say, ‘that one will kill a lot of men.’ Even the women will talk and gossip [about] you a lot, saying, ‘that one has lost the appearance and has the look of an HIV-positive person—we have to take care of our husbands.”’
Prominent Role of H/A Stigma
Adolescents and caregivers described significant and diverse experiences of H/A stigma in this setting (Figure 1). In most discussions about H/A stigma, the stigma described would be categorized as perceived stigma. Caregivers and adolescents spoke at length about fears of H/A stigma, particularly physical, emotional, or social isolation at the hands of various actors, including other family members, neighbors, and peers. Caregivers’ fears of their infected child centered on the child being discriminated against because of their HIV status, including the child losing friends or not being able to share food or sleep in the same room as other children. One caregiver stated, “There are parents who warn their teens not to play around those who are infected with HIV. Even if they were friends, they will separate because of that.” Adolescents had similar fears about discrimination and social isolation, with the most significant being that of losing friends, diminished social interactions, and loss of respect among peers. One adolescent reported that if children were to find out about another child’s HIV status, “ (they) will hate you and will be chasing you away.” Another child feared being told openly, “don’t touch me.” Most of the fears about perceived stigma focused on the loss of social interactions, but participants also described fears of losing resources because of stigma. One participant reported, “when they know that you have HIV, they will look down upon you. If you [try to] borrow from them, they will never give [anything to] you.” This characterizes not only fears of social isolation but also fears that those with HIV will lose out on community resources. Another adolescent talked about a scenario where, “Maybe your parents died and left you a house. When your relatives know that you are HIV positive, they will come and take your house from you, leaving you with nothing.” The majority of both adolescents’ and caregivers’ discussions of perceived H/A stigma involved fears of discrimination and isolation; however, these fears were closely tied to being afraid of losses of material support like food, housing, and employment.
Figure 1.
Mechanisms of stigma and illustrative quotes.
Fewer participants described instances of lived experiences of H/A stigma (or “enacted” stigma), but some caregivers did describe specific examples illustrating how HIV-infected people experience such stigma. These examples include the following—loss of community due to neighbors moving away after knowing one’s HIV status, loss of employment or loss of customers by HIV-infected business owners, family members and friends refusing to share food or utensils, and a general loss of respect in the community. Several caregivers talked about loss of economic stability because of HIV status, with one stating, “I was affected because when looking for a job, I was told we don’t want anyone who is infected.” Participants described how community members often talked and “gossiped” about others’ HIV status with specific stories accounting either their own experiences of stigma or the experience of a family member or friend.
Internalized stigma was prominent in caregiver and adolescent discussions as a common experience manifested at some point during their own or their child’s life. Internalized stigma was often experienced as feelings of shame of being infected or, for mothers, shame from infecting their child. A common manifestation of internalized stigma was having low self-esteem, and participants described feelings of “hating themselves” and “insult[ing] themselves in their hearts.” Participants described sometimes feeling unworthy of the very social interactions with family and friends that they so feared losing due to their HIV status. Even if others were not aware of the child’s status, some caretakers admitted that they still prevented their HIV-infected child from playing and sharing toys with other children for fear that HIV could be transmitted or that others would discover the child’s status. In this manner, caregivers enacted the social isolation presumptively based on their fears.
Finally, caregivers described instances of courtesy stigma at the level of the caregiver or wider family due to their child’s HIV status. Caregivers described instances where H/A stigma was directed at them because they cared for an HIV-infected child, even though they themselves were uninfected or their status was not known. Participants noted that community members believe that, if the child is infected, their caregiver must also be infected. Courtesy stigma was especially prominent when caregivers were taking a child to clinic, and caregivers felt that anyone who saw them at an HIV clinic would assume that they were there because they were infected, even though the caregiver might be uninfected and simply accompanying a child who is infected.
Impact of H/A Stigma on HIV Treatment and Prevention
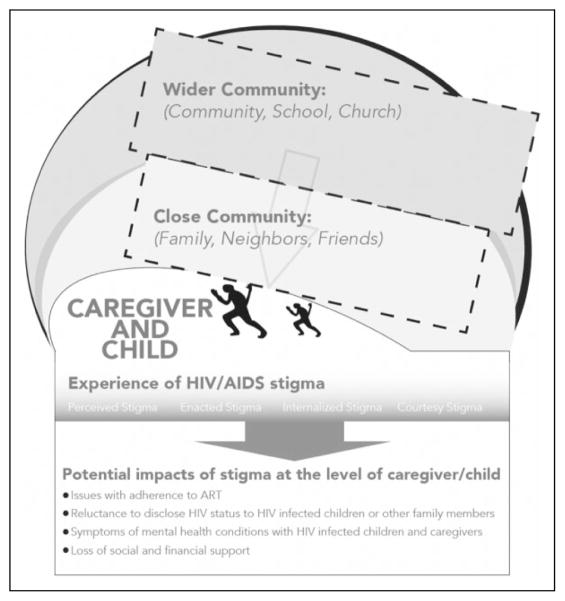
Adolescents and caregivers described multiple ways in which H/A stigma could impact their linkage or retention in HIV care as well as their ability to adhere to therapy. For example, caregivers described traveling extra distance to attend clinics far from home to avoid recognition either by healthcare staff or by other clinic attendees. Some caregivers shared stories of mothers and other caregivers who were reluctant to take their children to a clinic because of the fear of courtesy stigma; they were afraid that they would be seen at the HIV clinic and others would assume they were infected. Both adolescents and caregivers described not telling others they are on a medication, hiding medicines at their homes, and taking the medication in secret—all of which sometimes led to nonadherence. Caregivers described delaying disclosure of their HIV status or the child’s HIV status to spouses, sexual partners, and children because of fears about stigma. Not wanting to reveal one’s HIV status out of the fear of subsequent stigma results in barriers to HIV testing, treatment, and prevention. As 1 caregiver stated, “When your husband gets to know you have gone for testing, you will not have peace anymore. You can get tested and lose your marriage.” The fear of H/A stigma prevents people from being tested for HIV since they worry about being accused of infidelity or losing social or material support from family members and/or spouses. These impacts create challenging experiences for households caring for HIV-infected children (Figure 2).
Figure 2.
Experience of HIV/AIDS stigma on HIV-infected children and their caretakers.
Perspectives on Identifying, Measuring, and Reducing H/A Stigma
Focus group discussion participants described potential manifestations of H/A stigma, including physical, clinical, and psychological, that may be used to identify someone experiencing H/A stigma. First, both adolescents and caregivers thought that physical appearance could be an important indicator of stigma, with someone experiencing H/A stigma more likely look physically ill or “dirty.” For younger children whose caregiver was experiencing H/A stigma, participants’ thought that the child would be more likely to look generally neglected. HIV/AIDS-related stigma is connected to negative physical manifestations because of the associated withdrawal of material support when one is known to have HIV. In addition, H/A stigma could create psychological stress, which then results in physical illness or ill appearance, largely because of nonadherence to HIV treatment. Participants identified adherence as being closely associated with H/A stigma in that persons experiencing high levels of H/A stigma were less likely to be adherent, with subsequent physical illness or weight loss altering the physical appearance. Finally, participants thought that psychological distress in the form of feeling depressed, “stressed,” “restless,” or “losing hope” were all associated with H/A stigma. Symptoms of psychological distress were also sometimes described as general confusion, as 1 caregiver explained how to identify H/A stigma as, “You will just know from the way a person will come to clinic. They will look confused, he or she may enter [the clinic] and stand for so long even if there is a bench nearby.”
To measure H/A stigma in a clinical setting, participants overwhelmingly preferred strategies involving assessment through one-on-one or group counseling compared to filling out questionnaires. They cited potential difficulties completing a self-administered questionnaire, including illiteracy and concerns that patients would not understand questions about H/A stigma. Participants identified many topics for discussion during counseling sessions to assess H/A stigma, including types and experiences of H/A stigma, adherence to medications, and general financial and social difficulties, presumably due to loss of support by enacted stigma. Caregivers also stressed the importance of asking about disclosure of the individual’s or their child’s status to others. One caregiver suggested, “Ask them if, when they have gone to the clinic, do their neighbors know where they have gone?” For assessing H/A stigma in infected children, caregivers particularly stressed the importance of asking the child’s caregiver about difficulties for the child at school (academic achievement and social relationships with peers), adherence to medications, and general difficulties in caring for the child.
Several strategies to combat H/A stigma at the level of the community and for individuals experiencing stigma were proposed by participants. At the community level, caregivers highlighted educational campaigns, particularly those led by healthcare workers and infected individuals in rural areas where stigma was most rampant, as critical to changing attitudes and discriminatory practices. One caregiver stated, “I think the best thing is to create awareness in the [community]. First, you should educate caregivers so they can deal with their own stigma and then later the caregivers can help you educate people in the rural areas.” Participants also encouraged opportunities and venues for interaction between HIV-infected and noninfected community members, including clinics that do not segregate services based on HIV status. A caregiver explained, “For instance, here in the hospital we were mixed together with other people who are not infected, [this was] better—unlike now. You know when you get into the gate [of an HIV clinic], they will just say, ‘that one is infected.”’ HIV/AIDS-related stigma reduction strategies among those infected and affected by HIV centered on increasing family and peer support and clinic-level services like counseling. Treatment access, adherence, and economic security were associated with decreased vulnerability to H/A stigma and seemed to be related to the idea that an improvement in physical appearance decreased the likelihood of experiencing stigma. Not disclosing their own or their child’s (in the case of caregivers) HIV status was an important strategy to avoid stigma and discrimination for many participants.
Discussion
HIV/AIDS-related stigma remains a prominent concern for families and adolescents in western Kenya. In this setting, negative beliefs and misinformation about HIV are still common in the community, and participants in the qualitative inquiry process described significant and diverse experiences of H/A stigma. Living daily with perceived stigma imbued participants’ lives with fear, particularly about physical, emotional, or social isolation resulting from H/A stigma. Participants also highlighted how H/A stigma could impact the entire cascade of HIV testing, prevention, and care because stigma would negatively impact adherence to treatment, disclosure of HIV status, mental health, support networks, and economic stability.
Overall, we found that framing our understanding of H/A stigma through the major mechanisms of stigma (perceived, enacted, internalized, and courtesy) used elsewhere50–52 also worked well in this population and setting. Adolescents and caregivers identified H/A stigma operating through each of the mechanisms, although courtesy stigma was discussed more frequently by the caregiver groups. The HIV status of the caregivers was not recorded for this study. Thus, it is not surprising that some may be HIV uninfected and were presumably discussing their experiences of courtesy stigma. For both adolescents and caregivers, perceived H/A stigma (the fear of H/A stigma occurring) was featured most prominently. Even specific types of perceived H/A stigma, such as a child’s isolation from peers at school, were expressed by both caregivers and the adolescents themselves. These similarities reinforced the idea that this type of stigma is pervasive within the communities which they live. However, it was not always clear whether fears of H/A stigma arose from witnessing stigma directed at others, stories of stigma, or was simply informed by stigmatizing beliefs in the community about HIV.
Although the association between H/A stigma and adherence to treatment is well established in the adult literature,53 the relationship is not fully characterized for children.54,55 Our data support a relationship between H/A stigma and nonadherence as participants frequently discussed keeping medications a secret or attending a clinic that allowed them to keep their HIV status a secret from their community. This suggests a potential link between nonadherence to ART or to clinic attendance among children and adolescents as a consequence of H/A stigma. Participants further enforced this potential link by suggesting that assessments of H/A stigma include questions about adherence. Studies show that adolescents with chronic diseases generally have lower rates of adherence to treatment compared to younger children and adults,56,57 including lower rates of adherence to ART that contribute to higher rates of virologic failure.58–61 Identifying strategies to reduce H/A stigma among children and adolescents should include components related to adherence.
A significant milestone in most children’s long-term disease management is learning their HIV status. Reviews of disclosure of HIV status to children report that children in resource-limited settings are often less likely to know their HIV status and learn it at older ages compared to children in high-income settings.62 Caregivers often cite fears about the child telling others and subsequent H/A stigma and discrimination of the child and family as a major barrier to disclosure,63 including previous work in this setting.64 Perspectives from caregivers in our FGD are consistent with previous literature, with some caregivers identifying nondisclosure of a child’s or the caregiver’s status to relatives, neighbors, and others as an important protective strategy against H/A stigma. HIV/AIDS-related stigma was identified as a barrier to HIV testing even among spouses, which has been noted elsewhere.65,66 Self-disclosure by children and adolescents is less explored but limited evidence suggests that children and adolescents also weigh potential benefits with risks, with a major risk being H/A stigma and discrimination.67,68 Efforts to promote disclosure will need to consider and confront challenges related to H/A stigma.
Participants clearly identified H/A stigma as contributing to mental health issues such as depression and anxiety, consistent with other studies among adults69–71 and adolescents.72,73 The relationship between H/A stigma and mental health among adolescents in SSA is complicated by a lack of validated mental health measures in this setting74 as well as confounding variables such as orphanhood,75 adherence to ART,76–78 disclosure of HIV status,63,79–81 and higher rates of substance abuse and risky sexual behaviors.82 Supporting mental health is particularly critical among HIV-infected adolescents, as studies show that this population is at increased risk for mental health disorders.83–86
The relationship between loss of support and H/A stigma was highlighted by FGD participants. Loss of support was often characterized as both loss of social support and loss of financial support. The loss of these supports was often intertwined and may create a cycle with deleterious effects on HIV outcomes. Others have also noted that stigmatization and exclusion from social networks erode food and economic security, which undermines adherence to ART and then only further perpetuating this cycle.87 Data from our FGD seem to support this idea, with participants identifying social and economic security as important strategies to reduce H/A stigma for affected individuals and families.
Although H/A stigma is a persistent and significant barrier to achieving success in HIV prevention and treatment, it has only recently become a priority for HIV researchers, funders, and programs, particularly in SSA.88,89 In 2011, the United Nations General Assembly Political Declaration on HIV/AIDS made “eliminating stigma and discrimination” 1 of its 10 targets for ending HIV/AIDS.90 As millions of children gain access to lifesaving treatment and transition into adolescence and adulthood, understanding the unique experiences of H/A stigma for children and their families is critical to inform valid H/A stigma measurement tools and interventions to address the significant impacts of H/A stigma on long-term outcomes.
In western Kenya, we are trying to understand how H/A stigma impacts children and their families. The People Living with HIV Stigma Index was used in Kenya to survey 1086 people living with HIV in 2009 to 2010 and found that 30% of respondents reported experiencing H/A stigma in the past year and that 50% of respondents blamed themselves for their infection, including nearly 1 in 5 who reported feeling suicidal.91 Although research of H/A stigma among adults has increased, the experiences of children, adolescents, and their caregivers are still underexplored. In Kenya, less than 3% of respondents of the People Living with HIV Stigma Index were 19 years old or younger, and uninfected caregivers of HIV-infected children and adolescents were not included.91 In this evaluation, H/A stigma operating at the level of the caregiver and family was thought to have significant treatment implications for infected children in this setting, whether the caregiver was infected or not. As specific cultural contexts give H/A stigma meaning and power to negatively impact HIV-infected and affected individuals,92,93 it is critical to better understand how H/A stigma functions for pediatric patients and their families in the particular contexts of SSA if we are to improve their experiences, care, and outcomes.94 For example, a study in Kenya showed that families with fewer stigmatizing beliefs about HIV were more likely to provide care and support to children orphaned by HIV/AIDS.95
This study has a number of limitations for consideration. The perspectives gathered in this study are from a specific population in western Kenya and may not be generalizable to other regions in SSA or resource-limited countries. In addition, we relied on a convenience sample of caregivers and HIV-infected adolescents, which may also limit generalizability; albeit, this is not atypical for a qualitative inquiry. Within this study, this led to an overrepresentation of females in several of the adolescent groups and, unsurprisingly, in most of the caregiver groups. In order to create a heterogeneous group, FGDs were held in a variety of clinical settings (urban, semiurban, and rural) and included both biological and nonbiological caregivers as well as caregivers who have disclosed to their children and those who have not. In addition, we compared findings between both adolescents and caregivers of children. Good thematic saturation was achieved.
Conclusion
Despite the high prevalence of HIV and increasing access to HIV-related services, HIV-infected adolescents and caregivers in western Kenya describe an environment in which H/A stigma remains a major part of everyday life for HIV-infected and affected individuals. Participants provided novel insight into persistent negative and inaccurate community beliefs about HIV that influence social and treatment-related behaviors as well as potential strategies to identify, measure, and reduce H/A stigma in this setting. These data are critical to inform next steps and to move toward ending H/A stigma and discrimination.
Acknowledgments
The authors would like to thank the participants of the focus group discussions for their time and invaluable insights.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by a grant entitled “Stigma in AIDS Family Inventory” (3R01MH099747-01S1) to Dr Rachel Vreeman from the National Institute for Mental Health, Bethesda, Maryland.
Footnotes
Authors’ Note
This study was approved by the institutional review board of Indiana University School of Medicine in Indianapolis, Indiana, and by the institutional research and ethics committee of Moi University School of Medicine and MTRH in Eldoret, Kenya. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Indiana University School of Medicine, Moi University School of Medicine, or National Institutes of Health.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. Am J Public Health. 2007;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steward WT, Bharat S, Ramakrishna J, Heylen E, Ekstrand ML. Stigma is associated with delays in seeking care among HIV-infected people in India. J Int Assoc Provid Aids Care. 2013;12(2):103–109. doi: 10.1177/1545109711432315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDs. 2007;21(8):584–592. doi: 10.1089/apc.2006.0202. [DOI] [PubMed] [Google Scholar]
- 6.Lifson AR, Demissie W, Tadesse A, et al. Barriers to retention in care as perceived by persons living with HIV in rural Ethiopia: focus group results and recommended strategies. J Int Assoc Providers AIDS Care. 2013;12(1):32–38. doi: 10.1177/1545109712456428. [DOI] [PubMed] [Google Scholar]
- 7.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDs. 2006;20(5):359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 8.Kumarasamy N, Safren SA, Raminani SR, et al. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care STDs. 2005;19(8):526–537. doi: 10.1089/apc.2005.19.526. [DOI] [PubMed] [Google Scholar]
- 9.Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;10(5):473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dlamini PS, Wantland D, Makoae LN, et al. HIV stigma and missed medications in HIV-positive people in five African countries. AIDS Patient Care STDs. 2009;23(5):377–387. doi: 10.1089/apc.2008.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Trans Infect. 2007;83(1):29–34. doi: 10.1136/sti.2006.019893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peretti-Watel P, Spire B, Obadia Y, Moatti JP VESPA Group. Discrimination against HIV-infected people and the spread of HIV: some evidence from France. PLoS One. 2007;2(5):e411. doi: 10.1371/journal.pone.0000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark HJ, Lindner G, Armistead L, Austin BJ. Stigma, disclosure, and psychological functioning among HIV-infected and non-infected African-American women. Women Health. 2003;38(4):57–71. doi: 10.1300/j013v38n04_04. [DOI] [PubMed] [Google Scholar]
- 14.Major B, O’Brien LT. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- 15.Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS Behav. 2002;6:309–319. [Google Scholar]
- 16.Thomas BE, Rehman F, Suryanarayanan D, et al. How stigmatizing is stigma in the life of people living with HIV: a study on HIV positive individuals from Chennai, South India. AIDS Care. 2005;17(7):795–801. doi: 10.1080/09540120500099936. [DOI] [PubMed] [Google Scholar]
- 17.Greeff M, Uys LR, Wantland D, et al. Perceived HIV stigma and life satisfaction among persons living with HIV infection in five African countries: a longitudinal study. Int J Nurs Stud. 2010;47(4):475–486. doi: 10.1016/j.ijnurstu.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Global Update on the Health Sector Response to HIV. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 19.UNICEF. Opportunity in Crisis: Preventing HIV from Early Adolescence to Young Adulthood. New York, NY: UNICEF; 2011. [Google Scholar]
- 20.Chase E, Aggleton P. Stigma, HIV/AIDS and Prevention of Mother-to-Child Transmission: A Pilot Study in Zambia, India, Ukraine and Burkina Faso. United Kingdom: United Nations Children’s Fund/Panos Institute; 2001. [Google Scholar]
- 21.Baggaley R, Sulwe J, Chilala M, Mashambe C. HIV stress in primary school teachers in Zambia. Bull World Health Organ. 1999;77(3):284–287. [PMC free article] [PubMed] [Google Scholar]
- 22.Mahati ST, Chandiwana B, Munyati S, et al. A Qualitative Assessment of Orphans and Vulnerable Children in Two Zimbabwean Districts. Cape Town, South Africa: HSRC Press; 2006. [Google Scholar]
- 23.Alliance StC. Mitigation of HIV/AIDS Impact on Orphans, Vulnerable Children and their Families. London, UK: Save the Children Alliance and Hope for African Children Initiative (HACI); 2005. [Google Scholar]
- 24.O’Hare BA, Venables J, Nalubeg JF, Nakakeeto M, Kibirige M, Southall DP. Home-based care for orphaned children infected with HIV/AIDS in Uganda. AIDS Care. 2005;17(4):443–450. doi: 10.1080/09540120412331291779. [DOI] [PubMed] [Google Scholar]
- 25.Dago-Akribi HA, Cacou Adjoua MC. Psychosexual development among HIV-positive adolescents in Abidjan, Cote d’Ivoire. Reprod Health Matters. 2004;12(23):19–28. doi: 10.1016/s0968-8080(04)23109-3. [DOI] [PubMed] [Google Scholar]
- 26.Eisenberg N, Fabes RA, Guthrie IK. Coping with stress: the roles of regulation and development. In: Wolchik SA, Sandler IN, editors. Handbook of Children’s Coping: Linking Theory and Intervention. New York, NY: Plenum Press; 1997. [Google Scholar]
- 27.Ammassari A, Antinori A, Cozzi-Lepri A, et al. AdICoNA Study Group, LipoICoNA Study Group. Relationship between HAART adherence and adipose tissue alterations. J Acquir Immune Defic Syndr. 2002;31(suppl 3):S140–S144. doi: 10.1097/00126334-200212153-00011. [DOI] [PubMed] [Google Scholar]
- 28.Deacon H, Stephney I. HIV/AIDS, Stigma and Children: A Literature Review. Cape Town, South Africa: Human Sciences Research Council; 2007. [Google Scholar]
- 29.Monasch R, Boerma JT. Orphanhood and childcare patterns in sub-Saharan Africa: an analysis of national surveys from 40 countries. AIDS (London, England) 2004;18(suppl 2):S55–S65. doi: 10.1097/00002030-200406002-00007. [DOI] [PubMed] [Google Scholar]
- 30.Ntozi JPM, Mukiza-Gapere J. Care for AIDS orphans in Uganda: findings from focus group discussions. Health Trans Rev. 1995;5(suppl):245–252. [PubMed] [Google Scholar]
- 31.Rebhun LA. Sexuality, color, and stigma among Northeast Brazilian women. Med Anthropol Q. 2004;18(2):183–199. doi: 10.1525/maq.2004.18.2.183. [DOI] [PubMed] [Google Scholar]
- 32.Mawn B. Raising a child with HIV: an emerging phenomenon. Families Sys Health. 1999;17(2):197–215. [Google Scholar]
- 33.Poindexter CC. ‘It don’t matter what people say as long as I love you’: experiencing stigma when raising an HIV-infected grandchild. J Mental Health Aging. 2002;8(4):331–348. [Google Scholar]
- 34.Strode A, Barrett-Grant K. The Role of Stigma and Discrimination in Increasing Vulnerability of Children and Youth Infected with and Affected with HIV/AIDS. United Kingdom: Save the Children; 2001. [Google Scholar]
- 35.Robertson BA, Ensink K. The psychosocial impact of human immunodeficiency virus infections in children. South Afr J Child Adolesc Psychiatr. 1992;4:46–49. [Google Scholar]
- 36.Vreeman RC, Nyandiko WM, Ayaya SO, Walumbe EG, Marrero DG, Inui TS. Factors sustaining pediatric adherence to antiretroviral therapy in western Kenya. Qual Health Res. 2009;19(12):1716–1729. doi: 10.1177/1049732309353047. [DOI] [PubMed] [Google Scholar]
- 37.Giese S, Meintjes H, Croke R, Chamberlain R. Health and Social Services to Address the Needs of Orphans and Other Vulnerable Children in the Context of HIV/AIDS: Research Report and Recommendations Report Submitted to HIV/AIDS Directorate, National Department of Health. Cape Town, South Africa: Children’s Institute, University of Cape Town; 2003. [Google Scholar]
- 38.Davids A, Letlape L, Magome K, et al. A Situational Analysis of Orphans and Vulnerable Children in Four Districts of South Africa. Cape Town, South Africa: HSRC Press; 2006. [Google Scholar]
- 39.Nyblade L, MacQuarrie K. Can We Measure H/A Stigma and Discrimination? Current Knowledge About Quantifying Stigma in Developing Countries. Washington, DC: UNAIDS; 2006. [Google Scholar]
- 40.Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychol Health Med. 2006;11(3):335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- 41.Kalichman SC, Simbayi LC, Jooste S, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- 42.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- 43.Holzemer WL, Uys LR, Chirwa ML, et al. Validation of the HIV/AIDS Stigma Instrument—PLWA (HASI-P) AIDS Care. 2007;19(8):1002–1012. doi: 10.1080/09540120701245999. [DOI] [PubMed] [Google Scholar]
- 44.Einterz RM, Kimaiyo S, Mengech HN, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82(8):812–818. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 45.Inui TS, Nyandiko WM, Kimaiyo SN, et al. AMPATH: living proof that no one has to die from HIV. J Gen Intern Med. 2007;22(12):1745–1750. doi: 10.1007/s11606-007-0437-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McAteer CI, Truong N, Aluoch J, et al. A systematic review of measures of HIV/AIDS Stigma in Pediatric HIV-Infected and Affected Populations. Journal of the International AIDS Society. doi: 10.7448/IAS.19.1.21204. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, NY: Aldine Publishing Company; 1967. [Google Scholar]
- 48.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: SAGE Publications; 1990. [Google Scholar]
- 49.Dedoose (Version 5.0.11) Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Methods Research Data. Los Angeles, CA: SocioCultural Research Consultants, LLC; 2014. [Google Scholar]
- 50.Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225–1235. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wight RG, Aneshensel CS, Murphy DA, Miller-Martinez D, Beals KP. Perceived HIV stigma in AIDS caregiving dyads. Soc Sci Med. 2006;62(2):444–456. doi: 10.1016/j.socscimed.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 53.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martinez J, Harper G, Carleton RA, et al. The impact of stigma on medication adherence among HIV-positive adolescent and young adult females and the moderating effects of coping and satisfaction with health care. AIDS Patient Care STDs. 2012;26(2):108–115. doi: 10.1089/apc.2011.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- 56.Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22(4):405–411. doi: 10.1097/MOP.0b013e32833a46a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Desai M, Oppenheimer JJ. Medication adherence in the asthmatic child and adolescent. Curr Allergy Asthma Rep. 2011;11(6):454–464. doi: 10.1007/s11882-011-0227-2. [DOI] [PubMed] [Google Scholar]
- 58.Bakanda C, Birungi J, Mwesigwa R, et al. Survival of HIV-infected adolescents on antiretroviral therapy in Uganda: findings from a nationally representative cohort in Uganda. PLoS One. 2011;6(4):e19261. doi: 10.1371/journal.pone.0019261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bygrave H, Mtangirwa J, Ncube K, Ford N, Kranzer K, Munyaradzi D. Antiretroviral therapy outcomes among adolescents and youth in rural Zimbabwe. PLoS One. 2012;7(12):e52856. doi: 10.1371/journal.pone.0052856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Evans D, Menezes C, Mahomed K, et al. Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Res Hum Retroviruses. 2013;29(6):892–900. doi: 10.1089/aid.2012.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nachega JB, Hislop M, Nguyen H, et al. Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in southern Africa. J Acquir Immune Defic Syndr. 2009;51(1):65–71. doi: 10.1097/QAI.0b013e318199072e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pinzon-Iregui MC, Beck-Sague CM, Malow RM. Disclosure of their HIV status to infected children: a review of the literature. J Trop Pediatr. 2013;59(2):84–89. doi: 10.1093/tropej/fms052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vreeman RC, Gramelspacher AM, Gisore PO, Scanlon ML, Nyandiko WM. Disclosure of HIV status to children in resource-limited settings: a systematic review. J Int AIDS Soc. 2013;16:18466. doi: 10.7448/IAS.16.1.18466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vreeman RC, Nyandiko WM, Ayaya SO, Walumbe EG, Marrero DG, Inui TS. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDs. 2010;24(10):639–649. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chesney MA, Smith AW. Critical delays in HIV testing and care: the potential role of stigma. Am Behav Sci. 1999;42:1162–1174. [Google Scholar]
- 66.Mall S, Middelkoop K, Mark D, Wood R, Bekker LG. Changing patterns in HIV/AIDS stigma and uptake of voluntary counselling and testing services: the results of two consecutive community surveys conducted in the Western Cape, South Africa. AIDS Care. 2013;25(2):194–201. doi: 10.1080/09540121.2012.689810. [DOI] [PubMed] [Google Scholar]
- 67.Thoth CA, Tucker C, Leahy M, Stewart SM. Self-disclosure of serostatus by youth who are HIV-positive: a review. J Behav Med. 2014;37(2):276–288. doi: 10.1007/s10865-012-9485-2. [DOI] [PubMed] [Google Scholar]
- 68.Midtbo V, Shirima V, Skovdal M, Daniel M. How disclosure and antiretroviral therapy help HIV-infected adolescents in sub-Saharan Africa cope with stigma. Afr J AIDS Res. 2012;11(3):261–271. doi: 10.2989/16085906.2012.734987. [DOI] [PubMed] [Google Scholar]
- 69.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India—a community based cross sectional study. BMC Public Health. 2012;12:463. doi: 10.1186/1471-2458-12-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21(8):1007–1013. doi: 10.1080/09540120802614358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cluver LD, Gardner F, Operario D. Effects of stigma on the mental health of adolescents orphaned by AIDS. J Adolesc Health. 2008;42(4):410–417. doi: 10.1016/j.jadohealth.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 73.Tanney MR, Naar-King S, MacDonnel K Adolescent Trials Network for HIVAIPT. Depression and stigma in high-risk youth living with HIV: a multi-site study. J Pediatr Health Care. 2012;26(4):300–305. doi: 10.1016/j.pedhc.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mabugu T, Revill P, van den Berg B. The methodological challenges for the estimation of quality of life in children for use in economic evaluation in low-income countries. Value Health Reg Issues. 2013;2:231–239. doi: 10.1016/j.vhri.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 75.Cluver L, Gardner F. The mental health of children orphaned by AIDS: a review of international and southern African research. J Child Adolesc Ment Health. 2007;19(1):1–17. doi: 10.2989/17280580709486631. [DOI] [PubMed] [Google Scholar]
- 76.Murphy DA, Wilson CM, Durako SJ, Muenz LR, Belzer M Adolescent Medicine HIVARN. Antiretroviral medication adherence among the REACH HIV-infected adolescent cohort in the USA. AIDS Care. 2001;13(1):27–40. doi: 10.1080/09540120020018161. [DOI] [PubMed] [Google Scholar]
- 77.Williams PL, Storm D, Montepiedra G, et al. PACTG 219C Team. Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics. 2006;118(6):e1745–e1757. doi: 10.1542/peds.2006-0493. [DOI] [PubMed] [Google Scholar]
- 78.Kang E, Delzell DA, Chhabra M, Oberdorfer P. Factors associated with high rates of antiretroviral medication adherence among youth living with perinatal HIV in Thailand. Int J STD AIDS. 2015;26(8):534–541. doi: 10.1177/0956462414545524. [DOI] [PubMed] [Google Scholar]
- 79.Mellins C, Brackis-Cott E, Dolezal C, Richards A, Nicholas S, Abrams E. Patterns of HIV status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clin Child Psychol Psych. 2002;7(1):101–114. [Google Scholar]
- 80.Menon A, Glazebrook C, Campain N, Ngoma M. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;46(3):349–354. doi: 10.1097/QAI.0b013e3181565df0. [DOI] [PubMed] [Google Scholar]
- 81.Tsai AC, Bangsberg DR, Kegeles SM, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013;46(3):285–294. doi: 10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Murphy DA, Durako SJ, Moscicki AB, et al. No change in health risk behaviors over time among HIV infected adolescents in care: role of psychological distress. J Adolesc Health. 2001;29(3 suppl):57–63. doi: 10.1016/s1054-139x(01)00287-7. [DOI] [PubMed] [Google Scholar]
- 83.Betancourt TS, Rubin-Smith JE, Beardslee WR, Stulac SN, Fayida I, Safren S. Understanding locally, culturally, and contextually relevant mental health problems among Rwandan children and adolescents affected by HIV/AIDS. AIDS Care. 2011;23(4):401–412. doi: 10.1080/09540121.2010.516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gaughan DM, Hughes MD, Oleske JM, et al. Pediatric AIDS Clinical Trials Group 219C Team. Psychiatric hospitalizations among children and youths with human immunodeficiency virus infection. Pediatrics. 2004;113(6):e544–e551. doi: 10.1542/peds.113.6.e544. [DOI] [PubMed] [Google Scholar]
- 85.Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. Psychiatric disorders in youth with perinatally acquired human immunodeficiency virus infection. Pediatr Infect Dis J. 2006;25(5):432–437. doi: 10.1097/01.inf.0000217372.10385.2a. [DOI] [PubMed] [Google Scholar]
- 86.Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc. 2013;16:18593. doi: 10.7448/IAS.16.1.18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Med. 2013;10(11):e1001557. doi: 10.1371/journal.pmed.1001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Piot P. AIDS: from crisis management to sustained strategic response. Lancet. 2006;368(9534):526–530. doi: 10.1016/S0140-6736(06)69161-7. [DOI] [PubMed] [Google Scholar]
- 89.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.United Nations General Assembly Political Declaration on HIV/AIDS. Ten targets: 2011 United Nations General Assembly Political Declarations on HIV/AIDS. UNAIDS; 2011. [Accessed June 8, 2015]. Web site. http://www.unaids.org/sites/default/files/media_asset/JC2262_UNAIDS-ten-targets_en_1.pdf. [Google Scholar]
- 91.National Empowerment Network of People Living With HIV and AIDS in Kenya (NEPHAK) People Living with HIV Stigma Index: Country Assessment—Kenya. Nairobi, Kenya: NEPHAK, GNP; 2011. [Google Scholar]
- 92.Airhihenbuwa CO, Webster JD. Culture and African contexts of HIV/AIDS prevention, care and support. SAHARA J. 2004;1(1):4–13. doi: 10.1080/17290376.2004.9724822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 94.Bogart LM, Cowgill BO, Kennedy D, et al. HIV-related stigma among people with HIV and their families: a qualitative analysis. AIDS Behav. 2008;12(2):244–254. doi: 10.1007/s10461-007-9231-x. [DOI] [PubMed] [Google Scholar]
- 95.Hamra M, Ross MW, Karuri K, Orrs M, D’Agostino A. The relationship between expressed HIV/AIDS-related stigma and beliefs and knowledge about care and support of people living with AIDS in families caring for HIV-infected children in Kenya. AIDS Care. 2005;17(7):911–922. doi: 10.1080/09540120500100593. [DOI] [PubMed] [Google Scholar]