Abstract
Early posterior cervical approach is an effective strategy for patients with cervical tuberculosis in the appropriate circumstances.
Keywords: Diagnostics, infection, neurology, radiology and imaging, spinal cord, surgery
Case report
Spinal tuberculosis (TB) is an uncommon condition with an incidence of 1–2% worldwide.1 Cervical spine TB is particularly rare, representing 3–5% of all spinal TB cases.2 The large diameter of the cervical cord in relation to the spinal canal makes cervical TB a dangerous condition in which the patient’s neurological status can deteriorate rapidly. In addition, cervical TB can be accompanied by a retropharyngeal abscess leading to acute airway compromise.3
The treatment of cervical spine TB is controversial. The mainstay of treatment is ambulatory chemotherapy with surgery limited to refractory cases in the presence of neurological deficit. In cases of surgery, the surgical approach is principally an anterior one.4
We report a case of severe destructive cervical TB with cord compression and quadraparesis, treated successfully with a posterior cervical surgical approach.
A 43-year-old Senegalese right-handed gentleman presented to a district general hospital Accident and Emergency department with a nine-month history of worsening neck pain. He also reported symptoms of malaise, weight loss, night sweats and fevers. He denied any bladder or bowel symptoms. He had no medical history, was HIV negative and was independent in his activities of daily living. He worked as a taxi driver and was a non-smoker, non-drinker with no tuberculosis contacts. He was discharged from hospital without imaging following conservative treatment and planned outpatient investigations.
The morning following his discharge he was re-admitted to hospital with sudden worsening of neck pain, inability to ambulate and respiratory distress. On examination, his Glasgow Coma Scale was 15/15. Upper and lower limbs were hypotonic and hyporeflexic. Power was 2/5 in upper and lower limbs with sensation reduced. Anal tone and perianal sensation were reduced. American Spinal Injury Association (ASIA) Impairment scale was graded A (complete). Laboratory tests revealed a C-reactive protein of 224 mg/l and white cell count of 14.8 × 109. He was subsequently admitted to the intensive care unit where he was intubated, resuscitated, catheterised and commenced on intravenous steroids.
Multi-slice cervical computerised tomography (CT) and magnetic resonance imaging (MRI) scanning with T1, T2 and Short TI Inversion Recovery (STIR) sequences were performed with and without contrast (Figure 1). This demonstrated a large destructive mass almost completely replacing the odontoid peg and axis, with involvement of the superior aspect of the C3 vertebral body. There was also anterior subluxation of the atlas in relation to the previous position of the axis and sub-axial spine with a degree of rotational mal-alignment. Soft tissue was noted to extend posteriorly into the spinal canal with compression of the spinal cord from just below the foramen magnum down to the C3/C4 disc space. The soft tissue mass also extended laterally with involvement of the exiting foramina at the C2/C3 and C3/C4 levels. A pre-vertebral fluid collection was seen extending anteriorly from the level of the nasopharynx down to the C5/C6 disc level. CT scanning of the thoracic and lumbar spine, demonstrated a central lytic lesion within the L2 vertebral body.
Figure 1.
CT and MRI imaging.
CT scanning of the chest showed left apical lung scarring with a small inflammatory nodule less than 1 cm in the left upper lobe. The radiology results in combination with the clinical history suggested TB as the probable diagnosis.
He was transferred to our neurosurgical unit, arriving at 2:30 am with a diagnosis of cord compression with spinal shock. The Consultant Spinal Surgeon had arranged for the theatre and anaesthetic staff to be on standby to operate without delay due to the patient’s clinical status. The patient remained intubated and underwent emergency C1/C2 decompression and occipito-cervical fixation 3 h post admission at 5:30 am.
The patient was rolled with in-line immobilisation and placed prone on a Montreal mattress with pressure areas protected. The head was held in a Mayfield clamp, allowing good access to the posterior and lateral neck as well as to the airway for possible anaesthetic intervention.
The skin was prepared with 2% chlorhexidine, disposable drapes and an iodine impregnated transparent dressing. A posterior, mid-line approach was taken. After routine exposure, a C1 and C2 laminectomy with excision of the ligamantum flavum was performed. A considerable amount of pus was identified lateral to the C1 and C2 vertebrae which was extruded. The approach continued around the C1 and C2 vertebrae where a large retropharyngeal abscess was present involving the odontoid peg. A washout with 3 litres of saline was conducted. Following maximal spinal decompression, the Mayfield was carefully released and the head was slowly lifted to reduce the subluxation. A posterior occipito-cervical stabilisation was then performed from occiput to C6. An occipital plate was fixed to the occiput and lateral mass screws and rods were positioned. We decided to fix down to this level to provide a secure caudal base for the fixation to the skull due to the significant instability of atlantoaxial articulation. The lamina and occiput were decorticated with a bur. The facet joints were decorticated posteriorly and curetted to remove the cartilage. A chronos strip (artificial bone matrix fashioned into a flat strip in which blood is incorporated) was placed over the occipital plate, sutured to this and then placed longitudinally and sutured to the C2 spinous process. This partly re-created the posterior tension band and provided a barrier between the dura and the posterior musculature. Artificial bone graft (Actifuse) was placed over the lamina and facet joints. Surgical closure was in layers over a drain on suction. The total length of surgery was 4 h. Fluid and bone samples were sent for microbiology and histology. There were no surgical complications. Post operatively his L2 lytic lesion was treated conservatively with a thoracic brace.
Intraoperative biopsies confirmed a diagnosis of spinal TB, fully sensitive to anti-TB therapy.
Post-operatively following Microbiology advice, he was commenced on a one-year course of ambulant chemotherapy.
He was extubated seven days post operatively in the intensive care unit and received regular input from the neuro-rehabilitation team. Neurological examination two months post-operatively demonstrated: power 4+ in arms and legs with normal tone, reflexes and sensation. He was discharged with ASIA Impairment Scale grade E (normal).
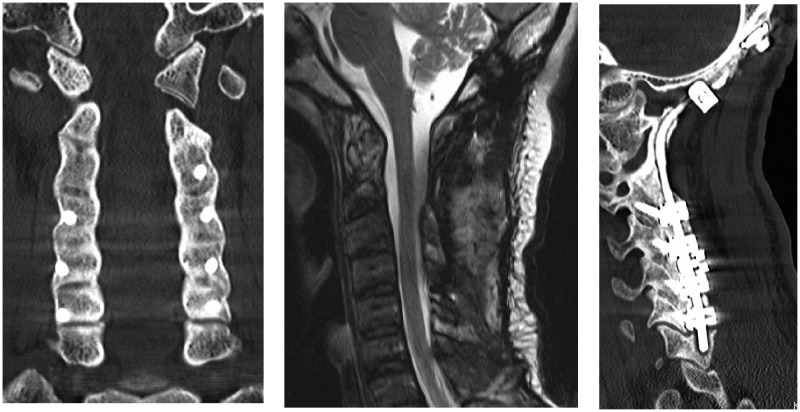
During serial neurosurgical follow-up, he demonstrated full neurological recovery. Repeat CT and MRI scanning showed stable and solid fusion of C1/C2 vertebrae with no signs of cord compression (Figure 2).
Figure 2.
CT and MRI imaging at latest follow-up.
His neck and chest brace were removed four months post operatively. At latest follow-up, two years following his operation, he has returned to work as a taxi driver and is fully independent in his activities of daily living. His range of neck motion is also remarkably good, being able to rotate his frontal gaze to 45° bilaterally.
Discussion
We present a case of destructive cervical TB with quadriplegia, respiratory compromise and spinal shock, treated with a posterior cervical surgical approach resulting in an excellent post-operative functional outcome.
The role of surgery in the management of spinal TB is controversial. The majority of cases are treated with ambulant chemotherapy with a Cochrane review noting that evidence is insufficient to support the routine use of surgery.1,5 Similarly, the Medical Research Council found no definite advantage of early surgery over medical management for spinal TB.6 Of note, this did not include patients with cervical disease.
There is, however, support for surgery in certain circumstances including: spinal TB refractory to medical therapy, pan vertebral lesions, progressive neurological deficit and severe deformity.2–5,7 Our reported case meets these surgical criteria.
The surgical strategy for spinal TB focuses on spinal biomechanical stabilisation, neural decompression and infectious tissue removal. Surgery is usually conducted via an anterior approach.2,8 There are few cases that report a posterior surgical approach for cervical TB. Moon et al.9 in their retrospective study of 134 cases of surgically treated cervical TB over a 45-year period report that only eight cases underwent a posterior only surgical approach.
The anterior cervical approach for spinal TB can be associated with recurrent laryngeal nerve injury, oesophageal injury, tracheal injury, major vessel injury and pre-vertebral haematoma. Our reported case suggests that a posterior cervical approach may be a safe and effective strategy for patients with cervical TB. A posterior approach may be beneficial in the appropriate circumstances for the following reasons: (1) Reduced operative time and blood loss, (2) fewer anatomical hazards and (3) easier visualisation of the dural sac and nerve roots.
In this case, we opted for occipito-cervical fixation due to the severe instability present and the difficulty in achieving a stable enough construct with C1 screws. The senior surgeon also felt that due to the nature of the patient’s condition, it would not be wise to risk vertebral artery injury in this case.
Further reporting is required to accurately assess the efficacy of this surgical approach. We also highlight the importance of early diagnosis and treatment in such cases and would like to emphasise the good prognosis possible in TB cases even when presenting with severe neurological deficit.
Acknowledgements
None
Declarations
Competing interests
None declared
Funding
None declared
Guarantor
RM.
Ethics approval
Written informed consent for patient information and images to be published was provided by the patient.
Contributorship
All authors made a substantial contribution to: the concept and design; acquisition and interpretation of information; writing of the article; and all authors approved the version to be published.
Provenance
Not commissioned; peer-reviewed by Herbert Budka.
References
- 1.Jutte PC, Van Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev 2006; 5: CD004532–CD004532. [DOI] [PubMed] [Google Scholar]
- 2.He M, Xu H, Zhao J, Wang Z. Anterior debridement, decompression, bone grafting, and instrumentation for lower cervical spine tuberculosis. Spine J 2014; 14: 619–627. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari A, Garg RK, Malhotra HS, Verma R, Singh MK, Jain A, et al. Outcome assessment in conservatively managed patients with cervical spine tuberculosis. Spinal Cord 2014; 52: 489–493. [DOI] [PubMed] [Google Scholar]
- 4.Hahn BS, Kim KH, Kuh SU, Park JY, Chin DK, Kim KS, et al. Surgical treatment in patients with cervical osteomyelitis: single institute's experiences. Korean J Spine 2014; 11: 162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garg RK, Somvanshi DS. Spinal tuberculosis: a review. J Spinal Cord Med 2011; 34: 440–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MRC Working Party on Tuberculosis of the Spine and J. Darbyshire. Five-year assessment of controlled trials of short-course chemotherapy regimens of 6, 9 or 18 months' duration for spinal tuberculosis in patients ambulatory from the start or undergoing radical surgery. Fourteenth report of the Medical Research Council Working Party on Tuberculosis of the Spine. Int Orthop 1999; 23: 73–81. [DOI] [PMC free article] [PubMed]
- 7.Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res 2007; 460: 39–49. [DOI] [PubMed] [Google Scholar]
- 8.Hassan MG. Anterior plating for lower cervical spine tuberculosis. Int Orthop 2003; 27: 73–77. [DOI] [PubMed] [Google Scholar]
- 9.Moon MS, Kim SS, Moon YW, Moon H, Kim SS. Surgery-related complications and sequelae in management of tuberculosis of spine. Asian Spine J 2014; 8: 435–445. [DOI] [PMC free article] [PubMed] [Google Scholar]