Abstract
Pediatric hypertension is a risk for adult cardiovascular disease, making early detection important. The prevalence of pediatric essential hypertension is rising due to the increased prevalence of obesity. Though guidelines for screening, diagnosis, evaluation, and management are available, there are barriers to accurate diagnosis of pediatric hypertension, including lack of knowledge and complexity of blood pressure standards. We aimed to gain insights into reasons for low rates of diagnosis and treatment from primary care providers. As part of a multisite randomized controlled trial, we interviewed 8 providers in a community health center network. We used a grounded theoretical approach to analyze transcripts. Providers reflected on numerous barriers to diagnosis, management, and follow-up; recommendations for educational content; and how community health center systems can be improved. Findings informed development of a multifaceted intervention. Despite lack of training on essential hypertension, providers were comfortable recommending lifestyle changes to promote healthier weight and reduced blood pressure.
Keywords: pediatric hypertension, obesity, lifestyle management, clinical decision support, qualitative research
Introduction
There is substantial evidence that risk factors for adult cardiovascular disease including obesity, diabetes, hyperlipidemia, and hypertension are established in childhood. Identification, evaluation, and management of these risks, therefore, should also take place in childhood.1 Hypertensive children are likely to become hypertensive adults.2 Hypertension in childhood itself is associated with damage to target organs including left ventricular hypertrophy, increased thickness of carotid intima media, and microalbuminuria.3-5 Among adults, target organ damage of this type is strongly associated with cardiovascular morbidity and mortality.6-8 Moreover, effective and safe treatments for hypertension in children are available and have been shown to reverse target organ damage.9
Guidelines for the screening for and diagnosis, evaluation, and management of hypertension in children have been available for 40 years.10 Unfortunately, clinicians consistently fail to recognize the problem, and the majority of hypertensive children remain undiagnosed.11 Several reasons for this have been documented including lack of knowledge of the problem and the complexity of blood pressure standards among children.12 Treatment for hypertension begins with adoption of lifestyle changes based on the Cardiovascular Health Integrated Lifestyle Diet guidelines from the National Heart, Lung, and Blood Institute.13 In prior research exploring pediatric subspecialists’ perspectives on the diagnosis and management of hypertension, subspecialists endorsed that medication and other hypertension management should occur in subspecialty settings.14 This same study highlighted the additional work needed to coordinate co-management of patients between primary and subspecialty care.
In this study, our goal was to gain detailed insight into provider perspectives about pediatric hypertension from clinicians on the front line, who care for large numbers of children in community-based primary care practices. Our study specifically focuses on perspectives of community health providers who care for a larger percentage of high-risk patients and may be increasingly responsible for more intensive management of children with hypertension due to limited access to subspecialists. Our specific objectives were not only to understand reasons for low rates of diagnosis and treatment but also to understand what clinicians feel would help them improve their own performance. Findings from these interviews informed development of a novel multifaceted intervention to overcome barriers to diagnosis, evaluation, and management of pediatric hypertension identified by provider participants and supported by the literature. The components of this intervention are described in the discussion.
Methods
Context
The findings presented here are from the formative phase of a larger quality improvement program titled, “Improving Diagnosis of Hypertension in Children.” The qualitative phase was carried out to inform development of a multifaceted practice-based intervention that is being studied in a cluster randomized controlled trial. We conducted semistructured telephone interviews with pediatric providers (pediatricians and family medicine physicians).
Setting and Recruitment
The healthcare setting for this qualitative study is a multi-specialty community health center (CHC) network in the Chicago area that provides care to children and adults who are predominantly Latino and African American. Nearly 40% of patients are under the age of 18 and over 98% are raised in households that are at or below 200% of the federal poverty level. Nearly half of patients have English as their second language. Over 44% of the pediatric population has a body mass index classification in the category of overweight or obese. The health center offers various health promotion programs including health education and cooking classes, exercise groups, and on-site nutritional services through the Women, Infants, and Children program.
Providers in this practice have access to an electronic health record system (EHRS) with basic built-in tools for identification of obesity, automatic calculation of blood pressure percentiles, and recommendations for nutrition counseling. Clinical providers caring for children include pediatricians, family medicine physicians, and pediatric and family medicine nurse practitioners. For study recruitment, a letter explaining the project and encouraging provider participation was disseminated to the 4 provider types from 5 sites within the same health center organization, and a total of 18 providers who care for pediatric patients were approached for inclusion in the study. Respondents interested in the study were formally consented.
Interview Guide
The interview guide for the semistructured interviews was first drafted by the principal investigator of the study and then disseminated to the research team and the project committee to provide feedback. The research team was composed of core co-investigators and research staff, while the project committee consisted of external members with expertise in various scientific fields that relate to the research study. After multiple iterations, the final agreed-upon interview guide included the following sections: introduction, general knowledge, prioritization, barriers to diagnosis, preferences for clinical decision support (CDS), recommendations for the Extension for Community Healthcare Outcomes (ECHO) Curriculum, individual experience, and additional input. ECHO is an established video-conference based training system for primary care providers to improve their knowledge and self-efficacy in management of specific conditions.15 Participants had variable knowledge about ECHO as it has been used many times in the past among providers in the study health care organization to provide optional training about key topics including childhood obesity and attention deficit hyperactivity disorder. For providers less familiar with ECHO, the purpose and structure of the curriculum was explained prior to relevant questions. Each section of the guide included 1 to 6 question prompts to ensure that ample information on each topic was collected from participants (see Table 1).
Table 1.
Question Prompts From Semistructured Interviews of Pediatric Providers.
| Topic | Question Prompts |
|---|---|
| General knowledge | 1. What do you know about hypertension in children? |
| 2. Are you familiar with guidelines for diagnosis, evaluation, and management of pediatric hypertension? | |
| a. On a scale of 1 to 10 how comfortable are you with the diagnosis, evaluation, and management of hypertension in children? | |
| Prioritization | 1. What is your perception of the significance of pediatric hypertension and the importance of diagnosis and management? |
| Barriers to diagnosis | 1. In many cases the diagnosis of hypertension is missed in children. What do you believe are the reasons for this? |
| 2. What do you believe are the barriers to diagnosis in your practice/clinic? | |
| Clinical decision support | 1. What tools and or features within an electronic medical record would help you with diagnosis of pediatric hypertension? |
| a. With evaluation? | |
| b. With management? | |
| ECHO curriculum | 1. Would you find it useful to participate in an educational program on pediatric hypertension? |
| a. Why or why not? | |
| 2. If yes, what would you like to see as part of this educational program? | |
| a. What modality would be most helpful in implementing this educational program? Webinar? In- person? | |
| Individual experience | 1. Can you think of a case where you worked with a patient who had pediatric hypertension? |
| a. If so, how, when, and by whom was the diagnosis made? | |
| b. How was the patient evaluated and managed? |
Technical Aspects
Each participant provided written informed consent prior to the phone interview. Interviews were carried out by the study’s principal investigator and a co-investigator and lasted approximately 30 minutes. Each interview was recorded and then transcribed verbatim by a professional transcription company. All identifying information was removed from the transcripts. Each participant received a $100 check to compensate them for their time. All analyses were carried out using NVivo 10 software (QSR International, Doncaster, Australia).
Analysis
The transcripts from the recorded interviews were independently reviewed and coded by the principal investigator and one of the co-investigators in NVivo. Using an approach based in grounded theory, they each independently coded the first 3 transcripts, then met to discuss codes and emerging themes (consistently reported observations, ideas, or concerns) resolving discrepancies through discussion. They then independently coded the remaining 5 transcripts and met again to review and resolve discrepancies by then recoding transcripts as necessary until a mutually agreed-upon list of themes developed. These themes were shared and discussed with the research team and the project committee, ultimately to be used to inform the development of a multifaceted practice-based intervention that included training for clinicians and the development of an advanced CDS tool. This study was approved by the Institutional Review Board at NorthShore University HealthSystem and the study network’s research review committee.
Results
Of the 18 providers within the health care system who received an invitation to participate, 8 consented and completed an interview. Participants included 6 pediatricians, 1 family medicine physician, and 1 family medicine nurse practitioner from 4 clinic locations in the study health center network. Participants had been in practice for an average of 9 years, with a range of 3 to 27 years. All participants practice in primary care clinics offering adult, pediatric, prenatal, senior, and behavioral health services. Six of the participants practice in a diverse urban setting, 5 of those in a community that is majority Latino or African American, and one of which also provides dental and HIV/AIDS services. Two participants practice in a diverse suburban setting that provides dental services. Characteristics of the patients served by providers recruited for the study were representative of the populations served by all pediatric providers in the sites represented. See Table 2 for provider characteristics.
Table 2.
Provider Characteristics.
| Interviewed Providers, n | |
|---|---|
| Gender | |
| Female | 7 |
| Male | 1 |
| Specialty | |
| Pediatrics | 6 |
| Family medicine | 2 |
| Years in practice | |
| 0-5 years | 3 |
| 6-11 years | 3 |
| 12-17 years | 0 |
| 18-23 years | 1 |
| 24-27 years | 1 |
Emergent Themes
Three important general themes emerged that were each commented on by at least 6 of the 8 providers: (a) among providers, there is the perception of an increased prevalence of pediatric hypertension in clinical practice that is associated with the increasing prevalence of obesity; (b) there are numerous system- and patient-level barriers to the accurate diagnosis of hypertension in children; and (c) providers want a CDS tool to assist in accurate diagnosis, a Medical Assistant (MA) training program to overcome barriers to blood pressure measurement, and an interactive provider training program, such as ECHO, to increase knowledge of evaluation and referral.
Increased Prevalence of Pediatric Hypertension Due to Obesity
Providers’ understanding of the importance of pediatric hypertension is shaped by their awareness of its increasing prevalence related to obesity and lifestyle factors among children that make it imperative to identify early to prevent long-term sequelae. Pediatricians feel their training was focused on evaluation to identify causes of secondary hypertension and referral to specialists for management, but they are less familiar with essential hypertension in children. Providers expressed a desire to have a better understanding of ways to address the role of lifestyle and obesity, specifically, the nutritional counseling and healthy lifestyle education services they could provide in primary care prior to referral to a specialist for evaluation and additional management. Family medicine providers, while more comfortable with essential hypertension in adults, expressed a desire for more training and resources to specifically overcome barriers to addressing lifestyle management in children. The following direct quotes from participants exemplify these findings:
In the course of my career as a pediatrician we’re seeing a shift that goes along with the increase in obesity in our population and certainly, especially at least with older pediatric patients, we’re thinking that often the hypertension relates to lifestyle and obesity issues. But certainly the issue is not going away and it’s something we’re confronting more and more frequently.
. . . lack of medical education when I was a student and a resident because it wasn’t, maybe, so much of a big problem when I was there and now it’s becoming more and more of a primary care issue as obesity rates grow . . .
I think managing behavior change in children and especially in an area that is underserved or people don’t have a lot of resources and there’s a lot of social determinants of how managing behavior change around diet and exercise and healthy eating and lifestyle and stress and sleep and all the things that go along with it is difficult.
I have to say I refer a fair number of patients on and most of my patients get told to do lifestyle modifications even though they see the specialist which is a little bit frustrating to me because I spend a lot of time trying to work with them on lifestyle modifications. . . . To have the specialist start over and tell them they have to do 6 months of lifestyle modifications exasperates me at times.
I think, myself as a pediatrician, that’s something that I didn’t get a lot of training in because we learned more about secondary hypertension in very young children, and not so much about essential hypertension in older children with obesity.
I do not feel comfortable at all in managing it in terms of medication management, so I have never started a child on any ACE [angiotensin-converting enzyme] inhibitor or any other antihypertensive agent on my own. I typically talk to families about weight reduction. I talk about exercise and kind of nonpharmacologic measures to treat the hypertension.
Significant Barriers to Diagnosis of Pediatric Hypertension
Providers described numerous system- and patient-level barriers that make diagnosing pediatric hypertension extremely challenging. First, there is a lack of a systematic approach among providers to review blood pressure values or clearly identified mechanisms to synthesize previous blood pressure values that are necessary to make a diagnosis. There are barriers related to provider workflow including EHRS workflows and blood pressure measurement.
Specifically, providers described inaccurate blood pressure readings due to difficulty in measurement in children who do not sit still, use of improper technique, lack of proper equipment (wrong size cuff), and not using a manual blood pressure machine when rechecking abnormal values. These measurement issues are related to problems with workflow in a busy clinical setting, in that MAs may not have time to follow proper technique and recheck values due to time constraints, as well as a lack of adequate training in pediatric blood pressure measurement.
Finally, lack of follow-up serves as a barrier in 2 ways. First, there are inadequate systems in place to ensure that patients with abnormal blood pressure readings have follow-up appointments scheduled and lack of ability for providers to indicate which patients need follow-up so they or clinic staff can make sure they return when indicated. Second, even with systems in place to ensure follow-up, many patients may not return to clinic due to a variety of barriers or personal choices. The following quotations illustrate these barriers:
I sometimes ignore values that I’m fairly certain are outside a range or now that [the EHRS] tells me are outside the range becauseanxiety and fear can cause those to be elevated. . . . I sometimes look at it and go, “Mm,” and don’t always create a system for circling back to check it at another time to make sure that it’s not a real value that I should be responding to.
Getting a blood pressure takes time and the medical assistants are being asked to do more and more and more and more things.
I would say one barrier is the medical assistants, there’s a lot of turnover, so they don’t frequently alert me to a highly abnormal blood pressure. I think technique might sometimes be an issue. . . . I have to retrain people constantly to say, “Repeat the blood pressure if it’s above normal. Tell me if it’s abnormal.” I’ve had medical assistants that literally just didn’t put the number in because it was high.
I know a lot of offices don’t have even the appropriately-sized cuffs . . .
If this is somebody that has borderline or pre-hypertension that I would ask to come back in 2 weeks, I would say probably about 25% of the patients I ask for follow-up in 2 weeks or a week to recheck blood pressure actually come back.
Preferences for CDS Tools and Education
Providers described the need for EHRS tools and educational resources to help them more accurately diagnose, evaluate, and manage pediatric hypertension. Many providers felt the currently available resources within the EHRS was helpful, as it provided a basic interpretation of a blood pressure reading based on a patient’s age, height, and gender. However, providers expressed a desire to see additional features in a comprehensive CDS tool that would allow for a clear display averaging previous blood pressure values on the same screen as the current blood pressure reading. While they want the values to be synthesized and a diagnosis clearly labeled, they also want the ability to interpret the results and record a diagnosis of elevated blood pressure or hypertension on their own. As part of a comprehensive CDS tool, providers expressed interest in standardized order sets to aid in diagnostic evaluation including labs and referrals.
When asked about preferences for educational content, providers placed strong emphasis on evaluation of secondary causes of pediatric hypertension, the integration of weight management into treatment for hypertension, reasons to refer to a specialist, and to a lesser extent, pharmacological management. Providers preferred a webinar format, such as ECHO, for education because it is both convenient and interactive, as opposed to a recorded webinar or live training. Providers felt that an essential component to overcome barriers to diagnosis of pediatric hypertension is to do a training for MAs to address issues with measurement technique and workflow. Finally, providers highlighted the need for educational materials on lifestyle management, including a healthy diet that should be disseminated to parents of children as part of a comprehensive management strategy. The following quotations illustrate preferences for a CDS tool and education:
If they could make it [CDS tool] in a way that would not overwhelm me. I think in that case when you choose your value, like if you click on something, it has the blood pressure and the interpretation and you create your interpretation that says yes I agree, this is hypertension.
[Describing preferences for provider education] . . . get together with . . . cardiology, nephrology, and talk about what is it that they want us to do beforehand, and then we could create custom lists around that.
I think giving a video conference or a webinar—would be great, because it’s something that then you could access regardless of where you are.
[Of content in provider education materials] . . . more on the management pieces. When they need to be referred and when they don’t need to be referred and they can be treated in primary care.
If there was something to click on that said help with management, yeah, it could be useful if it basically summed up the CDC guidelines as opposed to you having to read the whole article.
Discussion
Review of Key Findings
The findings from these interviews with pediatric providers at a CHC network in the Chicago area highlight an awareness of the growing problem of childhood obesity and lifestyle factors that directly affect their experience with diagnosis and management of hypertension in a vulnerable population of children where access to subspecialists may be limited by insurance type and lengthy wait times due to comparative acuity of illness. Providers described numerous barriers to accurate diagnosis of pediatric hypertension that included both system- and individual-level factors. Participants expressed valuable insights into aspects of an intervention they believe would improve their ability to accurately diagnose, evaluate, and manage pediatric hypertension that included both staff and provider education as well CDS in the EHRS. This study harnessed input from providers to design staff and provider educational programing and EHRS tools to overcome barriers to accurate diagnosis and management in this high-risk population with a growing prevalence of essential hypertension. By integrating feedback from frontline providers who have firsthand experience with the workflows in their care settings, the resulting process improvements have the potential to improve the cardiovascular health of children and reduce long-term complications of hypertension. Findings from future studies reporting on the outcomes of these interventions may provide knowledge that is generalizable to other practices caring for similar populations and encountering similar workflow challenges.
Consistency With What Is Already Known About Practice and Attitudes
Our findings are consistent with prior research indicating that while there is an acknowledgement of increased prevalence of hypertension, there is substantial variability in the initial diagnostic evaluation of hypertensive patients. Past studies indicate that only 7% of pediatricians routinely start antihypertensive drug treatment for hypertension, with 82% referring their hypertensive patients to a specialist and 40% feeling uncomfortable with evaluation and treatment.16 There is a well-known gap in identifying children with mildly or moderately elevated blood pressure,17 with technique in blood pressure measurement cited as a major barrier to accurate diagnosis.18 Consistent with findings from prior studies, participants in our study expressed the need to overcome numerous barriers to collecting accurate blood pressure measurements and increasing their knowledge of evaluation and referral as well as the need for multiple accurate blood pressure measurements to make a diagnosis. Finally, multiple studies have demonstrated underdiagnosis of hypertension in practices as well as an acknowledgement of the need to seamlessly integrate improved processes into the clinical workflow to support providers in detecting abnormal blood pressures.11
Though the challenges with improving rates of diagnosis have been known for some time, our study uncovered important barriers to evaluation and management of hypertension as well. Providers felt that their training, and hence their priority in evaluating children with elevated blood pressure, was to identify secondary causes of hypertension (eg, renal artery disease). They expressed unfamiliarity with the evaluation of essential hypertension. This is an important finding as it implies that curricula that address hypertension at the residency level or in continuing education programs ought to be revised.
The reluctance to prescribe medications was striking. Given the significant prevalence of hypertension in children, referring all children in whom pharmacotherapy is indicated to specialists may not be feasible in a large city like Chicago, let alone in other areas where specialist resources are more limited. Providers expressed either anxiety or hesitation about starting medication, as well as the feeling that pharmacotherapy was outside the scope of their practice. To overcome hesitation and to incorporate pharmacotherapy into their management, additional training with clear scenarios about when to initiate, titrate, or switch medication for hypertension are likely to be helpful. In addition, provider comfort may be increased through the ability to obtain input from specialists even when formal referral and co-management is not indicated.
Despite their reluctance to prescribe medications for pediatric hypertension, even when indicated, the providers we interviewed readily embraced lifestyle changes as an initial treatment strategy. Education about lifestyle management was perceived as being necessary and valuable. Specifically, the desire among clinicians for education about how to promote lifestyle changes, including improved nutrition, is consistent with the well-documented lack of nutrition education in medical training and poor knowledge of nutrition among physicians generally.19,20
Implications for Current Practice and Contributions to Development of a Multifaceted Intervention
Data from the semistructured interviews highlighted the need for clinical skills improvements (including among medical assistants), clinic workflows, provider workflows, clinical staff education, and improvement in EHRS tools to enhance the resources available to accurately diagnose elevated blood pressure in children. Participants also highlighted the need for educational materials that could be disseminated to parents of children around lifestyle management, including healthy nutritional practices. Based on findings from the provider interviews, we designed a novel multifaceted practice-based intervention to overcome barriers to accurate diagnosis, evaluation, and management of pediatric hypertension in this CHC network. The medical assistant training, professional training, and CDS tool components of the intervention are described below.
Medical Assistant Training
With MAs increasingly being viewed as integral members of the care team and in many cases being integrated in diverse patient care activities,21 maximizing the clinical skills of MAs has far-reaching implications for improving the diagnosis of pediatric blood pressure. Based on findings from these interviews, a MA training program was conducted to address barriers in accurate blood pressure measurements. This training included an educational video collectively viewed by all health center organization MAs involved in pediatric care regarding critical aspects of blood pressure measurement including correct cuff size, position, and automatic and manual measurements. Immediately following the viewing of the educational video, on-site demonstration of proper technique with direct observation was conducted for all participating MAs.
Participants in this training provided positive feedback regarding skills refinement in blood pressure measurement. As a result of this new training program, clinic administrators identified several themes that will inform future training competencies for medical assistants in this CHC network. A key theme was that pediatric specific training programs around obtaining vitals should be part of competency assessments in health systems where clinical staff apply their skills to both adult and pediatric populations. Additionally, in settings where automated blood pressure devices are used, periodic training on retaining skills of manual blood pressure measurement is necessary and should be encouraged.
Professional Training
Findings from specific questions about the ECHO curriculum in the semistructured interviews guided the focus of the ECHO Chicago curriculum for pediatric providers around blood pressure management. Provider discomfort around medication management for children with hypertension highlighted the need for more education and reference materials to disseminate evidence-based guidelines around treatment including lifestyle modification and medication management where appropriate. Providers desired education on how to effectively counsel on lifestyle changes in the primary care setting prior to and in addition to referral to specialists. Because intensive nonpharmacological treatment is integral to preventing the negative long-term sequelae of pediatric hypertension,9 increased education and availability of resources that address lifestyle and nutrition factors are essential for pediatric providers. The ECHO curriculum on pediatric hypertension was created as part of a larger curriculum on management of childhood obesity. All health center clinicians have been encouraged to enroll in the larger ECHO childhood obesity curriculum.
Previous studies focused on enhancing provider knowledge highlight the need for a variety of learning activities for providers.22 Consistent with this finding, the responses from providers in this study highlighted the need for educational opportunities in addition to the ECHO curriculum for providers that can be easily embedded in clinical workflows or with learning achievable in an efficient fashion. As such, as part of this project, educational materials such as power point presentations on best practices for blood pressure management were disseminated through an online community of CHC pediatric providers. Additionally, reference materials were created in order to efficiently, and concisely communicate evidence based guidelines; these were incorporated in the CDS.
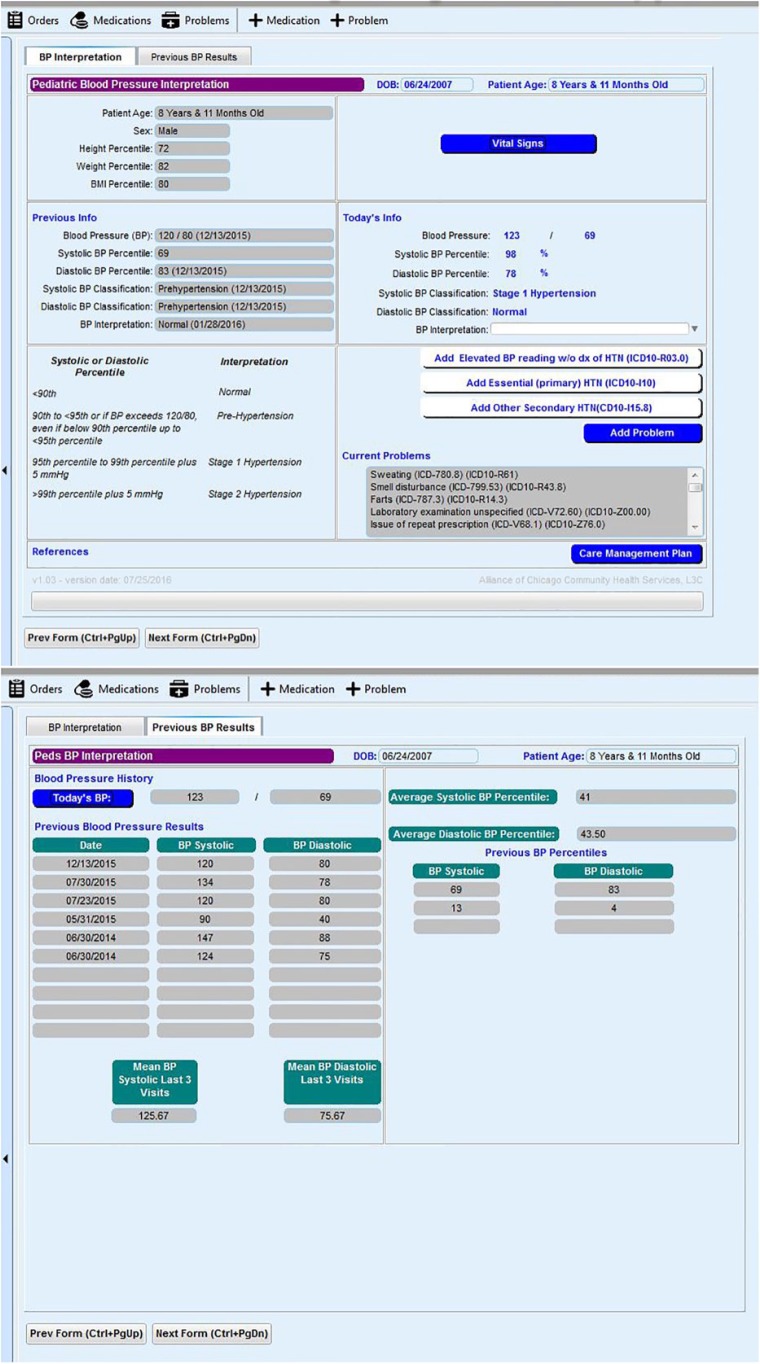
Clinical Decision Support Tools
Past studies indicate that an EHRS alone may not improve the diagnosis and management of hypertension. Optimizing CDS tools, specifically ones that integrate evidence at the point-of-care, may be more useful in promoting adherence to evidence-based recommendations for blood pressure management.23 In this qualitative study, although providers indicated overall satisfaction with existing EHRS-based tools, specifically calculation of blood pressure percentiles based on a patient’s gender, age, and height, there were gaps identified in the current EHRS’ capabilities for diagnosing hypertension in children. The most critical gap was an easy mechanism for displaying and interpreting past blood pressure values such that patients who meet diagnostic criteria are readily identified. The new CDS tool developed from providers’ input during study interviews offers a view of the past 3 blood pressure readings along with the average percentiles of the past blood pressures. The new tool also offers enhanced resources for provider and patient education pertaining to lifestyle management. In response to providers’ desire for a condensed resource or reference for management guidance, a reference document was created to be made available within the CDS. Having such a reference material readily available at the point of care has the potential to minimize workflow challenges that require referring to blood pressure management resources that are not native to an EHRS system, such as externally available evidence-based guidelines (see Figures 1 and 2).
Figures 1 and 2.
Screen shots of clinical decision support tool created and integrated in the study clinic network’s EHRS based on pediatric provider input from semi-structured interviews.
Limitations
This study has several limitations. First, is the relatively small number of study participants. Despite our best efforts to recruit a larger sample, only 8 of the 18 providers agreed to participate. However, the characteristics of these 8 providers were representative of the pediatric providers from the 5 practice locations within the clinic network. Importantly, the diverse perspectives of the participants yielded a rich data set from which we identified 3 important themes. However, the study findings may not encompass the beliefs and/or workflow of all providers working within the 13-location health center network serving a diverse urban and suburban setting as well as those who use the same EHRS but serve other populations. In addition, these findings may not be generalizable to other clinic settings. Last, providers’ roles and/or time working within the health center setting may influence their responses as their familiarity of the EHRS system, clinic workflows, or clinical subject matter may vary.
Conclusions
This study provides key insights into the barriers to diagnosis and management of pediatric hypertension in a vulnerable population with an increasing prevalence of obesity, specifically knowledge gaps through medical education and training on essential hypertension in children. Other barriers include problems with clinic workflow that inhibit accurate blood pressure measurement and interpretation, patient follow-up after abnormal readings, and lack of comfort with pharmacological and lifestyle management. To overcome these barriers, pediatric providers desire additional education that will allow them to address the health needs of their patient population, with a specific focus on lifestyle management, as well as a CDS tool to aid in diagnosis and management at the point of care. These provider perspectives were used to develop a novel multifaceted intervention that will be implemented and tested in this CHC network.
Author Contributions
JKB: Contributed to the design of the study and contributed to acquistion, analysis, and interpretation of the results.
NM: Contributed to the conception and design of the study and to interpretation of the results.
VB and SSR: Contributed to the design of the study and interpretation of the results.
GR: Contributed to the conception and design of the study and contributed to acquistion, analysis, and interpretation of the results.
All co-authors drafted, critically revised, and gave final approval of the manuscript.
Acknowledgments
The authors gratefully acknowledge the support of the providers and staff at the study clinic, the staff at Alliance of Chicago Community Health Services, and the study’s community advisory committee.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Agency for Healthcare Research & Quality (1R21HS024100-01).
References
- 1. Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673-1686. doi: 10.1161/circulationaha.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171-3180. doi: 10.1161/circulationaha.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brady TM, Fivush B, Flynn JT, Parekh R. Ability of blood pressure to predict left ventricular hypertrophy in children with primary hypertension. J Pediatr. 2008;152:73-78.e1. doi: 10.1016/j.jpeds.2007.05.053. [DOI] [PubMed] [Google Scholar]
- 4. Sorof JM, Alexandrov AV, Garami Z, et al. Carotid ultrasonography for detection of vascular abnormalities in hypertensive children. Pediatr Nephrol. 2003;18:1020-1024. doi: 10.1007/s00467-003-1187-0. [DOI] [PubMed] [Google Scholar]
- 5. Assadi F. Effect of microalbuminuria lowering on regression of left ventricular hypertrophy in children and adolescents with essential hypertension. Pediatr Cardiol. 2007;28:27-33. doi: 10.1007/s00246-006-1390-4. [DOI] [PubMed] [Google Scholar]
- 6. Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114:345-352. [DOI] [PubMed] [Google Scholar]
- 7. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459-467. doi: 10.1161/circulationaha.106.628875. [DOI] [PubMed] [Google Scholar]
- 8. Bigazzi R, Bianchi S, Baldari D, Campese VM. Microalbuminuria predicts cardiovascular events and renal insufficiency in patients with essential hypertension. J Hypertens. 1998;16:1325-1333. [DOI] [PubMed] [Google Scholar]
- 9. Litwin M, Niemirska A, Sladowska-Kozlowska J, et al. Regression of target organ damage in children and adolescents with primary hypertension. Pediatr Nephrol. 2010;25:2489-2499. doi: 10.1007/s00467-010-1626-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Blumenthal S, Epps RP, Heavenrich R, et al. Report of the task force on blood pressure control in children. Pediatrics. 1977;59(5 2 suppl):I-ii, 797-820. [PubMed] [Google Scholar]
- 11. Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874-879. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 12. Rao G. Diagnosis, epidemiology, and management of hypertension in children. Pediatrics. 2016;138(2). doi: 10.1542/peds.2015-3616. [DOI] [PubMed] [Google Scholar]
- 13. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213-S256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yoon E, McCool B, Filipp S, Rocchini A, Kershaw D, Clark S. Pediatric hypertension specialists’ perspectives about adolescent hypertension management: implications for primary care providers. Clin Pediatr (Phila). 2015;54:551-556. doi: 10.1177/0009922814558248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arora S, Kalishman S, Thornton K, et al. Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52:1124-1133. doi: 10.1002/hep.23802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Boneparth A, Flynn JT. Evaluation and treatment of hypertension in general pediatric practice. Clin Pediatr (Phila). 2009;48:44-49. doi: 10.1177/0009922808321677. [DOI] [PubMed] [Google Scholar]
- 17. Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125:e1286-e1293. doi: 10.1542/peds.2009-0555. [DOI] [PubMed] [Google Scholar]
- 18. Patel ND, Newburn A, Brier ME, Chand DH. Pediatric hypertension: are pediatricians following guidelines? J Clin Hypertens (Greenwich). 2016;18:1230-1234. doi: 10.1111/jch.12915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24:546-552. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 20. Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr Clin Pract. 2010;25:471-480. doi: 10.1177/0884533610379606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bodenheimer T, Willard-Grace R, Ghorob A. Expanding the roles of medical assistants: who does what in primary care? JAMA Intern Med. 2014;174:1025-1026. doi: 10.1001/jamainternmed.2014.1319. [DOI] [PubMed] [Google Scholar]
- 22. Cha SD, Chisolm DJ, Mahan JD. Essential pediatric hypertension: defining the educational needs of primary care pediatricians. BMC Med Educ. 2014;14:154. doi: 10.1186/1472-6920-14-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Samal L, Linder JA, Lipsitz SR, Hicks LS. Electronic health records, clinical decision support, and blood pressure control. Am J Manag Care. 2011;17:626-632. [PubMed] [Google Scholar]