Abstract
Coagulase-negative staphylococci, with the leading species Staphylococcus epidermidis, are the predominant cause of hospital-acquired infections. Treatment is especially difficult owing to biofilm formation and frequent antibiotic resistance. However, virulence mechanisms of these important opportunistic pathogens have remained poorly characterized. Here we demonstrate that S. epidermidis secretes poly-γ-DL-glutamic acid (PGA) to facilitate growth and survival in the human host. Importantly, PGA efficiently sheltered S. epidermidis from key components of innate host defense, namely antimicrobial peptides and neutrophil phagocytosis, and was indispensable for persistence during device-related infection. Furthermore, PGA protected S. epidermidis from high salt concentration, a key feature of its natural environment, the human skin. Notably, PGA was synthesized by all tested strains of S. epidermidis and a series of closely related coagulase-negative staphylococci, most of which are opportunistic pathogens. Our study presents important novel biological functions for PGA and indicates that PGA represents an excellent target for therapeutic maneuvers aimed at treating disease caused by S. epidermidis and related staphylococci.
Introduction
Over the past decade, Staphylococcus epidermidis has become the most prevalent pathogen involved in nosocomial infections (1). Usually an innocuous commensal microorganism on human skin, this member of the coagulase-negative group of staphylococci can cause severe infection after penetration of the epidermal protective barriers of the human body. In the US alone, S. epidermidis infections on in-dwelling medical devices, which represent the main type of infection with S. epidermidis, cost the public health system approximately $1 billion per year (1). Importantly, S. epidermidis is frequently resistant to common antibiotics (1). It is, therefore, essential to find new molecular targets for drug development against S. epidermidis infections. The formation of surface-attached cellular agglomerations, so-called biofilms, is a major determinant of S. epidermidis pathogenicity (2). Biofilm formation is believed to contribute significantly to antibiotic resistance and protection from innate host defense (3). Resistance of S. epidermidis biofilms to some antibiotics might, in part, be due to a status of generally reduced metabolism (4). Yet, by and large, the specific mediators of biofilm resistance and immune evasion in S. epidermidis are unknown.
Poly-γ-DL-glutamic acid (PGA) is an anionic, extracellular polymer, in which the α-amino and γ-carboxy groups of D- or L-glutamic acid are linked by isopeptide bonds (5). PGA is produced primarily by Bacillus strains but also infrequently by other strains of bacteria, archaebacteria, and some eukaryotes (5). On the whole, the biological role of PGA has remained unclear. Presumably, it serves as an external C and N reserve or protects from environmental factors such as high osmolarity (5). In Bacillus anthracis, a PGA capsule has a hitherto unique role in sheltering the bacteria from phagocytosis (6). Homologs of the cap locus for PGA biosynthesis are found in a restricted number of human pathogens, including the spirochaete Leptospira interrogans, which causes the waterborne disease leptospirosis (7), and Fusobacterium nucleatum, which causes periodontal disease (8). However, it is unknown whether PGA is produced and plays a role in virulence in these organisms.
Here we demonstrate PGA production in S. epidermidis and related coagulase-negative staphylococci. We constructed an isogenic cap mutant strain of S. epidermidis to analyze the role of PGA in protection from environmental factors and innate host defense and as a virulence determinant in an animal infection model. Our study indicates an important function of PGA during both the commensal and infectious lifestyles of S. epidermidis and presents PGA production as the first widespread mechanism of immune evasion in this principal opportunistic pathogen.
Results
The S. epidermidis genome contains the genes that code for PGA synthesis.
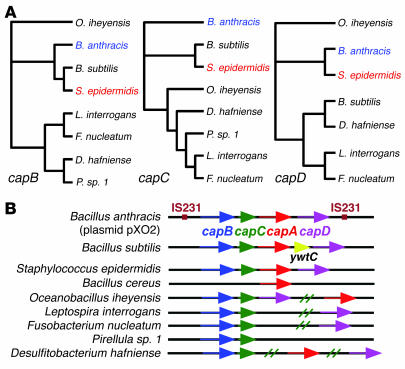
To survive on the human skin and during infection of in-dwelling medical devices, S. epidermidis must have mechanisms to circumvent human innate host defense. Only recently, we discovered that the biofilm exopolysaccharide polysaccharide intercellular adhesin (PIA) protects S. epidermidis from major mechanisms of innate host defense (9). However, PIA is restricted to a subpopulation of S. epidermidis, and therefore, a ubiquitous principle protecting S. epidermidis from innate host defense has remained elusive. We searched the recently published S. epidermidis genome (10) for gene loci potentially involved in such protection. We found that, in contrast to its relative S. aureus, S. epidermidis has the cap locus that codes for production of the anionic exopolymer PGA. The S. epidermidis cap genes show high similarity to those of B. anthracis and B. subtilis (Figure 1A). Of note, in contrast to B. subtilis and several human pathogens that have parts of the cap genes, the genetic organization of the cap locus of B. anthracis is well conserved in S. epidermidis (Figure 1B).
Figure 1.
Molecular genetic comparison of bacteria with genes encoding a putative PGA synthesis machinery. (A) Phylogenetic trees based on sequence comparisons of the capB (amide ligase), capC (unknown function), and capD (depolymerase) genes. CapA is a putative PGA exporter. We have excluded a comparison of capA genes, because capA homologs were not found in all the organisms and comparison of transporters is normally less indicative of phylogenetic relations. Of the microorganisms shown, production of PGA has been demonstrated previously only in B. anthracis and B. subtilis, and in this study, in S. epidermidis. (B) cap genes and homologs in bacteria for which genetic information is available. The B. anthracis cap gene cluster is located on a plasmid and flanked by IS231 insertion sequences. All other genes are located in the bacterial chromosomes.
The S. epidermidis cap gene locus drives production of surface-attached PGA.
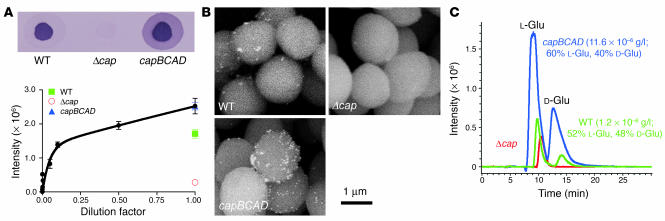
To analyze the role of the cap genes in S. epidermidis, we constructed a deletion mutant (S. epidermidis Δcap), in which the entire cap locus was replaced by a spectinomycin resistance cassette. To complement the mutant, we cloned the cap operon with its natural promoter in a plasmid and transformed the mutant with that plasmid (pRBcapBCAD). First, we determined PGA production in the mutant, wild-type, and complemented strains. Real-time PCR data indicated that the cap genes in S. epidermidis are expressed (data not shown). Accordingly, immunodetection of PGA in cell surface extracts of the wild-type and complemented strains demonstrated that PGA is synthesized by S. epidermidis and attached to the bacterial cell surface (Figure 2A). The PGA production level in the complemented strain was 147% of that of the wild-type strain. There was no detectable signal in the cap deletion strain or in any samples obtained from culture filtrates (Figure 2A and data not shown). Scanning electron microscopy with immunogold labeling confirmed that PGA is located on the S. epidermidis cell surface (Figure 2B). Next, we purified the immunoreactive material and performed quantitative and qualitative analyses to verify that it constitutes PGA. In contrast to B. anthracis PGA, which is entirely composed of D-glutamic acid (11), S. epidermidis PGA consisted of about equal amounts of D- and L-glutamic acid (Figure 2C). Notably, PGA production in S. epidermidis was far less than that reported for B. anthracis (1.2 × 10–6 g/l for S. epidermidis versus 5–10 g/l for B. anthracis; ref. 12). Taken together, our data demonstrate that the cap locus in S. epidermidis drives production of a surface-attached form of DL-PGA.
Figure 2.
PGA production in S. epidermidis. (A) Relative expression of PGA determined by immuno-dot blot analysis. PGA was extracted from bacterial cell surfaces as described in Methods. A calibration curve was obtained by dilution of the most intensive sample obtained from the PGA-overexpressing complemented strain S. epidermidis Δcap (pRBcapBCAD). Results are the mean ± SEM of 4 experiments for the samples and the mean ± SEM of 4 different serial dilutions for the calibration curve. A representative blot is shown at the top. (B) Detection of S. epidermidis PGA with immunoscanning electron microscopy. PGA was detected with anti-PGA antiserum. (C) Analysis of D-glutamic (D-Glu) and L-glutamic (L-Glu) acid in S. epidermidis PGA by stereoselective chromatography and liquid chromatographic–mass spectrometric detection of glutamic acid. To determine D- and L-glutamic acid amounts, the L-glutamic acid background detected in the cap mutant strain (Δcap) was subtracted from PGA expression strains. (A–C) Δcap, isogenic cap deletion strain; capBCAD, complemented strain S. epidermidis Δcap (pRBcapBCAD).
The cap gene locus and PGA production are ubiquitous among S. epidermidis strains.
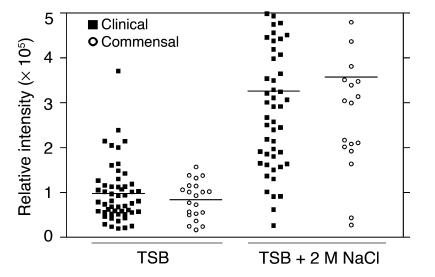
Some virulence factors in staphylococci, such as PIA, are mostly restricted to invasive strains (13, 14). In contrast, all 74 S. epidermidis strains of clinical and commensal origin that we investigated had the cap gene locus as shown by analytical PCR (data not shown) and were positive for PGA by immuno-dot blot analysis (Figure 3), indicating that PGA production is ubiquitous in S. epidermidis. Remarkably, there was no significant difference in PGA production between commensal and clinical strains (Figure 3). We therefore hypothesized that PGA is important for the survival of S. epidermidis as a skin commensal organism and during infection.
Figure 3.
PGA production in S. epidermidis strains. PGA expression in S. epidermidis strains of clinical and commensal origin, and under low and high salt conditions, determined by immuno-dot blot analysis. Cells were grown for 24 hours at 37°C with shaking at 200 rpm. PGA was then purified as described in Methods. Horizontal bars show the group mean. The membrane background was subtracted from each sample. The experiment, including purification and detection, was repeated twice with very similar results.
PGA contributes to resistance of S. epidermidis to high salt concentration.
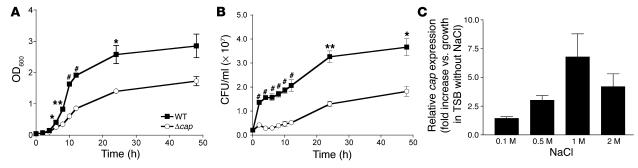
We first determined whether PGA impacts survival of S. epidermidis under conditions found in its natural habitat, i.e., the human skin. The environment on human skin is characterized by high and varying salt concentration. S. epidermidis can withstand very high salt concentrations of up to approximately 2 M NaCl, but the reasons for this extraordinary resistance are not completely clear (13). Growth and viability of the cap mutant strain were significantly impaired at high concentrations of NaCl (shown for 2 M NaCl in Figure 4, A and B), whereas growth at physiological salt concentration was similar for the wild-type and mutant strains (data not shown). Furthermore, quantitative real-time PCR analysis using a capB probe (Figure 4C) and immuno-dot blots (data not shown) demonstrated that S. epidermidis upregulates cap expression in response to high NaCl concentration. Additionally, in most strains of our collection, PGA production was greater at high NaCl concentration (Figure 3). These data suggest that PGA contributes to survival of S. epidermidis on human skin.
Figure 4.
Role of PGA in osmoprotection and inducibility of cap expression by NaCl. (A) Growth (OD600) and (B) viability (CFU) of wild-type and cap mutant strains in Luria-Bertani medium supplemented with 2 M NaCl. Bacteria were inoculated from an overnight preculture (1:1,000) and grown in flasks at 37°C with shaking at 200 rpm. Values are the mean ± SEM of 3 experiments. *P < 0.05; **P < 0.01; #P < 0.001 (wild-type versus mutant strain). (C) Quantitative real-time PCR analysis of NaCl inducibility of cap expression. Bacteria were grown as in (A) with the indicated concentrations of NaCl. Cells were harvested after 6 hours of growth, RNA was isolated, and real-time PCR was performed using a capB probe. Values are the mean ± SEM of 3 experiments.
S. epidermidis PGA protects from key components of innate host defense.
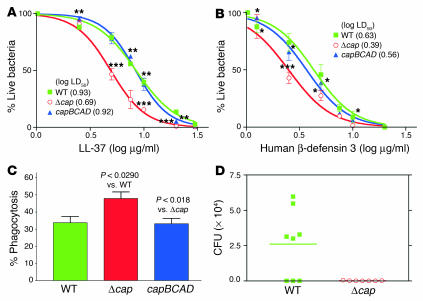
Next, we investigated whether PGA contributes to S. epidermidis virulence. Unlike its more aggressive relative S. aureus, S. epidermidis does not have a large arsenal of virulence factors (1). Rather, it causes relatively silent, chronic infections during which resistance against attacks by the innate immune system is of special importance to bacterial survival (1). Therefore, we analyzed whether cap expression in S. epidermidis affects resistance to key components of innate host defense against bacterial infections, namely antibacterial peptides and neutrophil phagocytosis. The cap mutant strain had significantly reduced resistance to 2 representative antibacterial peptides from human skin and neutrophil specific granules, LL-37 and human β-defensin 3 (Figure 5, A and B) and significantly increased susceptibility to phagocytosis by human neutrophils (Figure 5C). The phagocytosis rate was 42% higher with the mutant strain compared to the wild-type strain, which is a relatively large difference compared with what we observe with other single pathogen factors. These findings indicate that PGA plays a critical role in protecting S. epidermidis from the microcidal effects of innate host defense components.
Figure 5.
Role of PGA in immune evasion and virulence of S. epidermidis. (A and B) Resistance to cationic antimicrobial peptides. Washed S. epidermidis cells (approximately 105) were incubated with LL-37 (A) or human β-defensin 3 (B) in various concentrations for 2 hours at 37°C. Thereafter, S. epidermidis survivor cells were counted by plating. Results are shown as dose-response curves. The log LD50 values for all strain/peptide combinations are given in the key. Statistical analyses are for each peptide concentration. Values of significance were calculated against the wild-type (for Δcap) and Δcap (for capBCAD) strains. (C) Resistance to neutrophil phagocytosis. Phagocytosis by human neutrophils was determined after 30 minutes of incubation with S. epidermidis at a ratio of 20 bacteria per PMN. (D) Mouse model of subcutaneous device-related infection. Catheter pieces with equal amounts of adhered S. epidermidis cells (2 × 105) were placed under the dorsum of the animals. CFU on implanted devices 1 week after infection were counted. The horizontal bar shows the group mean. *P < 0.05; ***P < 0.01; ***P < 0.001.
PGA is indispensable for S. epidermidis persistence on in-dwelling medical devices in an animal infection model.
The role of PGA in protection from innate host defense components suggested that PGA facilitates pathogen survival during S. epidermidis infection. To test this hypothesis, we compared persistence of wild-type and isogenic cap mutant strains in a mouse model of subcutaneous catheter infection. Importantly, biofilm formation on plastic material and intercellular aggregation in vitro did not differ between wild-type and cap mutant strains (data not shown), indicating that colonization and persistence in the animal model were not due to differences in the physicochemical interaction with the catheter material. Most mice (5 of 8) infected with the wild-type strain had significant numbers of bacteria (approximately 3 × 104–6 × 104 CFU) on implanted catheters after 1 week of infection, whereas all 7 mice infected with the cap mutant strain had completely cleared the infection (Figure 5D). This pronounced difference indicates that PGA is a key factor for the success of S. epidermidis in device-associated infection, which represents the predominant type of disease caused by this organism.
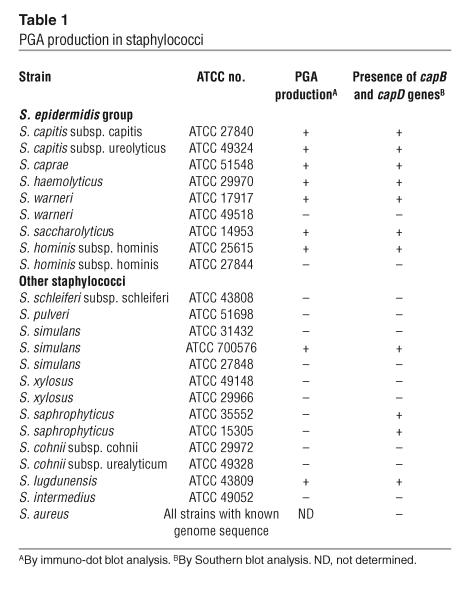
A group of coagulase-negative staphylococci related to S. epidermidis also produces PGA.
We know from publicly available genome sequencing data that the cap locus is absent from S. aureus. To investigate whether other staphylococcal species have the genetic information for PGA production, we tested a series of staphylococcal strains for the presence of the cap genes by DNA-DNA hybridization using capB and capD probes and a cocktail of probes from all 4 cap genes. Of 22 strains, representing 16 different species and subspecies, genomic DNA from 11 strains hybridized with the probes (Table 1). Except for S. saprophyticus strains, all strains with a signal in the Southern blot also produced surface-attached PGA, which was demonstrated using anti-PGA antisera (Table 1). Although there are some intraspecies differences, it is remarkable that all phylogenetically related members of the S. epidermidis group (S. epidermidis, S. capitis, S. warneri, S. saccharolyticus, S. caprae, S. hominis, and S. haemolyticus) (15) have the ability to produce PGA, whereas it is far less distributed among other species (Table 1).
Table 1.
PGA production in staphylococci
Discussion
We are only beginning to understand strategies used by pathogenic bacteria to evade the efficient bactericidal mechanisms of innate host defense (16). To survive in its natural habitat, i.e., on human skin, S. epidermidis needs to protect itself from antibacterial peptides of human epithelial cells. Furthermore, to persist during human infection, it must have efficient protection from ingestion by neutrophils and associated bactericidal mechanisms. Here we present PGA as the first widespread mechanism of immune evasion in S. epidermidis. Notably, we demonstrate a hitherto unknown role for PGA in resistance to cationic antimicrobial peptides. Further, PGA was critical for the establishment of chronic infection by S. epidermidis. The difference in persistence of the cap mutant and wild-type strains was more pronounced than with any other virulence determinant of S. epidermidis that has been investigated by an animal infection model. Inasmuch as PGA production in S. epidermidis is approximately 1 million times lower than in B. anthracis, one can conclude that the efficiency of PGA-mediated protection from innate host defense in the case of S. epidermidis is extraordinary. The mechanism of protection is unclear. Presumably, it is based on the strong anionic properties of PGA. For example, PGA may bind antibacterial peptides, which are usually cationic (17), and thus prevent them from reaching their target, the cytoplasmic membrane. However, protection by PGA may also be mediated, for example, by binding of PGA to other surface polymers, which might enhance the protective effect.
Except for the role that PGA has in protecting B. anthracis from phagocytosis, the biological function of PGA, particularly in noninfectious organisms, has remained speculative. It is known that several halophilic bacteria synthesize PGA (5). Therefore, it has been assumed that PGA serves to protect from high osmolarity. In our study, we show for the first time that PGA contributes to resistance against high salt concentration. It has been speculated that binding of water molecules by negatively charged PGA protects bacteria from dehydration (18). However, the low level of PGA production suggests that mechanisms other than direct binding of water by PGA might be involved in the protective effect in S. epidermidis.
Importantly, PGA production did not affect the aggregation behavior or biofilm formation of S. epidermidis, demonstrating that our observations are not due to secondary effects of cell aggregation. However, recent results that we obtained by microarray analysis of gene expression in S. epidermidis biofilms indicated that the cap locus is upregulated in biofilms (4). PGA may thus contribute to the overall resistance of S. epidermidis biofilms to innate immunity, although it does not appear to directly influence biofilm formation.
The S. epidermidis cap locus shows high similarity to that of B. anthracis. The genetic information for PGA production in B. anthracis is located on a plasmid (pXO2) (19, 20) and shows high genetic mobility (21). It might have been transferred between B. anthracis and staphylococci and from one strain of Staphylococcus to another. Coinfection of humans or human ancestors may represent a likely scenario for these events. Of note, most of the staphylococcal strains that produce PGA are opportunistic human pathogens. Consistent with its role in S. epidermidis, PGA might thus contribute to survival of those strains in the human host, although this notion remains to be demonstrated.
In conclusion, PGA appears to play a key role for the survival of S. epidermidis in the human host during colonization and infection. Remarkably, though produced in very small amounts, PGA contributes significantly to the pathogenicity of S. epidermidis, which underscores the efficiency of PGA-mediated protection. PGA may represent an excellent target for drug or vaccine development against infection with S. epidermidis and possibly other staphylococcal pathogens. Anti-PGA antibodies have been suggested for the treatment and prophylaxis of B. anthracis infections. Although PGA has a generally low immunogenicity, recent studies have shown that anti-PGA antibodies efficiently protect from anthrax infection in animal models (22–25). Our data indicate that they might also be valuable for the treatment of chronic infections by S. epidermidis and certain other pathogenic staphylococci.
Methods
Bacterial strains, growth conditions, and basic molecular biology methods.
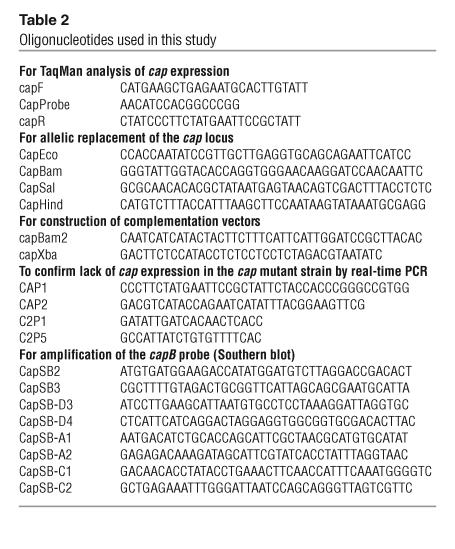
The clinical isolate S. epidermidis 1457 (26) was used in this study. Bacteria were grown in tryptic soy broth (TSB) unless otherwise noted. Antibiotics were used at the following concentrations: chloramphenicol, 10 μg/ml; spectinomycin, 100 μg/ml; and ampicillin, 100 μg/ml. Cultures were incubated at 37°C with shaking at 200 rpm. DNA manipulation, isolation of plasmid DNA, and transformation of Escherichia coli were performed using standard procedures. Staphylococcal plasmid DNA was prepared with the Qiagen Plasmid Midi Kit as described (27). S. epidermidis was transformed by electroporation as described (28). PCRs were performed with Ready-To-Go PCR Beads (Amersham Biosciences) as recommended by the manufacturer. DNA was sequenced using Big Dye Terminator cycle sequencing (version 3.0) on an ABI3700 sequencer (Applied Biosystems). Nucleotide sequences were analyzed using the program Vector NTI Suite (InforMax). Primers for DNA amplifications by PCR (Table 2) were purchased from Sigma Genosys. The 74 strains used for epidemiological studies were obtained from N. El Solh (Institut Pasteur, Paris, France) and are predominantly nonclonal (29).
Table 2.
Oligonucleotides used in this study
Real-time PCR.
RNA isolation was performed using a FastPrep BLUE Kit (Q-BioGene Inc.). Oligonucleotide primers and probes were designed using Primer Express 2.0 software (Applied Biosystems). The probe used for analysis of cap expression was located within the capB gene. TaqMan analysis was performed in a 384-well MicroAmp Optical using a 7900 Sequence Detector (Applied Biosystems). Standard curves were determined with purified chromosomal template DNA at concentrations ranging from 0.001 ng/ml to 10 ng/ml. Assays were performed in triplicate using cDNA samples, and 16S rRNA as control, with a standard cycle protocol.
Southern blot analysis.
Equal amounts of EcoRV-digested genomic DNA were separated by gel electrophoresis on a 0.7% agarose gel and visualized by ethidium bromide staining. DNA was transferred onto a nylon membrane (GE Osmonics Labstore) and probed with digoxigenin-labeled PCR product amplified from the capB or capD genes of S. epidermidis 1457 or with a cocktail of probes amplified from the capA, capB, capC, and capD genes. Prehybridization, hybridization, posthybridization, and immunologic detection were performed as described in the technical update accompanying the nonradioactive DNA Labeling and Detection Kit (Roche Applied Science). For immunologic detection, the membrane was incubated with a 1:5,000 dilution of sheep anti-digoxigenin Fab fragments conjugated to alkaline phosphatase. Probe-target hybrids were detected using the chromogenic substrate nitroblue tetrazolium/5-bromo-4-chloro-3-indolyl phosphate.
Immuno-dot blot assay.
Surface-attached PGA was released from the cell surface by boiling bacteria for 30 minutes at 100°C or by autoclaving. PGA was then purified by acid precipitation as described (12). Aliquots (3 μl) of the samples were spotted on a nitrocellulose membrane, air-dried, and PGA was detected with anti-PGA antiserum using a scanner and Total Lab Version 2003 software (Nonlinear USA). The assay was calibrated by serial dilution of the most intensive sample. The value detected in the wild-type strain was set to 100% and production values in the other strains were expressed relative to that value. Anti-PGA antiserum (kindly provided by R. Schneerson, National Institute of Child Health & Human Development, NIH, Bethesda, Maryland, USA) was developed against PGA from Bacillus pumilus. For Staphylococcus strains other than S. epidermidis, a strain with a signal higher than that of the background of the S. epidermidis Δcap mutant was considered a PGA producer.
Construction of an isogenic cap deletion mutant and cap-complementing vector.
To delete capBCAD in S. epidermidis 1457, PCR-amplified regions flanking the cap locus and a spectinomycin resistance cassette were cloned into plasmid pBT2 (30), yielding plasmid pBTΔcap, which was used for allelic replacement as described (31). The proper integration of the resistance gene marker spc was verified by direct sequencing of the genomic DNA at the borders of the PCR-derived regions. Lack of cap transcript in the cap mutant strain was verified by real-time PCR (data not shown). S. epidermidis 1457 in which capBCAD was deleted was named S. epidermidis Δcap. To complement for capBCAD in S. epidermidis Δcap, capBCAD genes were cloned into plasmid pRB474 (30). The resulting plasmid was named pRBcapBCAD.
Purification of PGA and detection of d- and l-glutamic acid.
Cultures were grown in TSB medium supplemented with 1 M NaCl to induce PGA production. PGA was first purified as described above. Then, PGA samples were further purified by ion exchange chromatography using a RESOURCE Q 6 ml column (Amersham Biosciences) on an AKTA Purifier 10 (Amersham Biosciences) and a gradient from 0.2% acetic acid to 0.2% acetic acid/1 M NaCl in 20 column volumes at a flow rate of 5 ml/min. Fractions with positive reaction in an immuno-dot blot were combined, dialyzed against water, lyophilized, resuspended in 6 M HCl, and hydrolyzed at 110°C for 24 hours. Samples were lyophilized again and dissolved in 200 μl of water. Ten microliters of the samples were then injected onto a Chirobiotic T column (Astec) using 0.1% triethylammonium acetate (pH 4.0) in 80% ethanol as elution buffer at a flow rate of 0.4 ml/min. Chromatography was performed using an Agilent 1100 series HPLC connected to a VL Trap mass spectrometer. The extracted ion chromatograms at 146 Da, the mass of glutamic acid, were used to determine the amounts of D- and L-glutamic acid by peak integration in comparison to pure D- and L-glutamic acid.
Isolation of human polymorphonuclear leukocytes and phagocytosis experiments.
Human polymorphonuclear leukocytes (PMNs) were isolated from heparinized venous blood of healthy individuals with a standard method (32). All studies were performed in accordance with a protocol approved by the Institutional Review Board for Human Subjects of NIAID. Cell preparations contained approximately 99% PMNs and all reagents used contained <25.0 pg/ml endotoxin. Phagocytosis of S. epidermidis by human PMNs was analyzed by flow cytometry with a previously described method (32). Briefly, bacteria were cultured to stationary growth phase, washed in PBS, and labeled with fluorescein-5-isothiocyanate for 15 minutes. PMNs (106/100 μl) and bacteria (2 × 107/100 μl) were combined in wells of serum-coated 96-well round-bottom microtiter plates. Plates were incubated for 30 minutes at 37°C and the degree of phagocytosis was determined by flow cytometry.
Peptide bacterial killing assays.
S. epidermidis cultures were harvested, washed with PBS buffer, and resuspended in 10 mM sodium phosphate buffer (pH 7.0). Bacterial killing assays were performed using a final concentration of approximately 105 S. epidermidis cells in each sample. Antimicrobial peptides were dissolved in the following solutions: human β-defensin 3, 10 mM acetic acid, and LL-37, 10% acetonitrile with 0.1% trifluoroacetic acid. The bacteria were exposed to a range of antimicrobial peptide concentrations (0, 5, 10, 20, 30, and 40 μg/ml). An equal volume of the respective peptide dilution buffer was applied to control samples. Samples were incubated at 37°C for 2 hours and appropriate dilution series of the samples were plated on TSB agar. Survivor S. epidermidis cells were enumerated after 24 hours of incubation at 37°C. The percentage of killed S. epidermidis was calculated using the formula (1 – [CFU peptide / CFUcontrol]) × 100.
Scanning immunoelectron microscopy.
Fifty-microliter aliquots of S. epidermidis cultures were washed with PBS buffer. Cells were resuspended in 200 μl of anti-PGA antiserum and incubated at 37°C with agitation at 400 rpm for 12 hours. Samples were washed with PBS and pellets were subsequently incubated with goat anti-rabbit IgG conjugated with 20 nm of gold (BB International) at 37°C with agitation at 400 rpm for 2 hours. Following antibody labeling, the cell suspensions were attached to coverslips, fixed with 2.5% glutaraldehyde in 0.1 M sodium cacodylate, and post-fixed with 1% osmium tetroxide in 0.1 M sodium cacodylate. Samples were washed with distilled water, dehydrated in a graded ethanol series, critical-point dried under CO2 with a Bal-Tec model cpd 030 drier (Balzers), mounted on aluminum studs, and sputter-coated with 100 angstroms of chromium in a model IBS/TM200S ion beam sputterer (South Bay Technologies) prior to viewing at 10 kV on a Hitachi S-4500 field emission scanning electron microscope (Hitachi) in backscatter imaging mode.
Murine model of device-related infection.
Female Balb/c mice were used in a model of subcutaneous implanted device-related infection as described (33). Two catheter pieces of 1-cm length were placed under the skin of the dorsum of each animal. CFUs on catheters were counted before insertion and were in the range of 2 × 105 on all implanted catheters. CFU on excised catheters and surrounding tissues were counted after 1 week of infection. All studies were performed in accordance with a protocol approved by the Animal Care and Use Committee of Rocky Mountain Laboratories, NIAID.
Statistics and DNA sequence analysis.
Statistical analysis was performed using GraphPad Prism version 4.0. DNA sequences were compared using Clustal W software.
Acknowledgments
The authors would like to thank Rachel Schneerson for providing anti-PGA antisera, Nevine El Solh for S. epidermidis strains, Aaron B. Carmody for technical assistance, and Donald Gardner, Michael Parnell, and Ralph Larson for help with animal studies.
Footnotes
Nonstandard abbreviations used: PGA, poly-γ-dl-glutamic acid; PIA, polysaccharide intercellular adhesin; PMN, polymorphonuclear leukocyte; TSB, tryptic soy broth.
Conflict of interest: The authors have declared that no conflict of interest exists.
References
- 1.Vuong C, Otto M. Staphylococcus epidermidis infections. Microbes Infect. 2002;4:481–489. doi: 10.1016/s1286-4579(02)01563-0. [DOI] [PubMed] [Google Scholar]
- 2.Götz F. Staphylococcus and biofilms. Mol. Microbiol. 2002;43:1367–1378. doi: 10.1046/j.1365-2958.2002.02827.x. [DOI] [PubMed] [Google Scholar]
- 3.Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284:1318–1322. doi: 10.1126/science.284.5418.1318. [DOI] [PubMed] [Google Scholar]
- 4.Yao Y, Sturdevant DE, Otto M. Genome-wide analysis of gene expression in Staphylococcus epidermidis biofilms: insights into S. epidermidis biofilm pathophysiology and the role of phenol-soluble modulins in biofilm formation. J. Infect. Dis. 2005;191:289–298. doi: 10.1086/426945. [DOI] [PubMed] [Google Scholar]
- 5.Oppermann-Sanio FB, Steinbüchel A. Occurrence, functions and biosynthesis of polyamides in microorganisms and biotechnological production. Naturwissenschaften. 2002;89:11–22. doi: 10.1007/s00114-001-0280-0. [DOI] [PubMed] [Google Scholar]
- 6.Little SF, Ivins BE. Molecular pathogenesis of Bacillus anthracis infection. Microbes Infect. 1999;1:131–139. doi: 10.1016/s1286-4579(99)80004-5. [DOI] [PubMed] [Google Scholar]
- 7.Ren SX, et al. Unique physiological and pathogenic features of Leptospira interrogans revealed by whole-genome sequencing. Nature. 2003;422:888–893. doi: 10.1038/nature01597. [DOI] [PubMed] [Google Scholar]
- 8.Kapatral V, et al. Genome sequence and analysis of the oral bacterium Fusobacterium nucleatum strain ATCC 25586. J. Bacteriol. 2002;184:2005–2018. doi: 10.1128/JB.184.7.2005-2018.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vuong C, et al. Polysaccharide intercellular adhesin (PIA) protects Staphylococcus epidermidis against major components of the human innate immune system. Cell. Microbiol. 2004;6:269–275. doi: 10.1046/j.1462-5822.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- 10.Zhang YQ, et al. Genome-based analysis of virulence genes in a non-biofilm-forming Staphylococcus epidermidis strain (ATCC 12228) Mol. Microbiol. 2003;49:1577–1593. doi: 10.1046/j.1365-2958.2003.03671.x. [DOI] [PubMed] [Google Scholar]
- 11.Ashiuchi M, Misono H. Biochemistry and molecular genetics of poly-gamma-glutamate synthesis. Appl. Microbiol. Biotechnol. 2002;59:9–14. doi: 10.1007/s00253-002-0984-x. [DOI] [PubMed] [Google Scholar]
- 12.Hanby WE, Rydon HN. The capsular substance of Bacillus anthracis. Biochemistry. 1946;40:297–307. [PubMed] [Google Scholar]
- 13.Otto M. Virulence factors of the coagulase-negative staphylococci. Front. Biosci. 2004;9:841–863. doi: 10.2741/1295. [DOI] [PubMed] [Google Scholar]
- 14.Galdbart JO, Allignet J, Tung HS, Ryden C, El Solh N. Screening for Staphylococcus epidermidis markers discriminating between skin-flora strains and those responsible for infections of joint prostheses. J. Infect. Dis. 2000;182:351–355. doi: 10.1086/315660. [DOI] [PubMed] [Google Scholar]
- 15.Saruta K, et al. Rapid identification and typing of Staphylococcus aureus by nested PCR amplified ribosomal DNA spacer region. FEMS Microbiol. Lett. 1997;146:271–278. doi: 10.1111/j.1574-6968.1997.tb10204.x. [DOI] [PubMed] [Google Scholar]
- 16.Hornef MW, Wick MJ, Rhen M, Normark S. Bacterial strategies for overcoming host innate and adaptive immune responses. Nat. Immunol. 2002;3:1033–1040. doi: 10.1038/ni1102-1033. [DOI] [PubMed] [Google Scholar]
- 17.Hancock RE, Diamond G. The role of cationic antimicrobial peptides in innate host defences. Trends Microbiol. 2000;8:402–410. doi: 10.1016/s0966-842x(00)01823-0. [DOI] [PubMed] [Google Scholar]
- 18.Hezayen FF, Rehm BH, Eberhardt R, Steinbüchel A. Polymer production by two newly isolated extremely halophilic archaea: application of a novel corrosion-resistant bioreactor. Appl. Microbiol. Biotechnol. 2000;54:319–325. doi: 10.1007/s002530000394. [DOI] [PubMed] [Google Scholar]
- 19.Green BD, Battisti L, Koehler TM, Thorne CB, Ivins BE. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 1985;49:291–297. doi: 10.1128/iai.49.2.291-297.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Makino S, Sasakawa C, Uchida I, Terakado N, Yoshikawa M. Cloning and CO2-dependent expression of the genetic region for encapsulation from Bacillus anthracis. Mol. Microbiol. 1988;2:371–376. doi: 10.1111/j.1365-2958.1988.tb00041.x. [DOI] [PubMed] [Google Scholar]
- 21.Green BD, Battisti L, Thorne CB. Involvement of Tn4430 in transfer of Bacillus anthracis plasmids mediated by Bacillus thuringiensis plasmid pXO12. J. Bacteriol. 1989;171:104–113. doi: 10.1128/jb.171.1.104-113.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leppla SH, Robbins JB, Schneerson R, Shiloach J. Development of an improved vaccine for anthrax. J. Clin. Invest. 2002;110:141–144. doi:10.1172/JCI200216204. doi: 10.1172/JCI16204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schneerson R, et al. Poly(gamma-D-glutamic acid) protein conjugates induce IgG antibodies in mice to the capsule of Bacillus anthracis: a potential addition to the anthrax vaccine. Proc. Natl. Acad. Sci. U. S. A. 2003;100:8945–8950. doi: 10.1073/pnas.1633512100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kozel TR, et al. mAbs to Bacillus anthracis capsular antigen for immunoprotection in anthrax and detection of antigenemia. Proc. Natl. Acad. Sci. U. S. A. 2004;101:5042–5047. doi: 10.1073/pnas.0401351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rhie GE, et al. A dually active anthrax vaccine that confers protection against both bacilli and toxins. Proc. Natl. Acad. Sci. U. S. A. 2003;100:10925–10930. doi: 10.1073/pnas.1834478100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mack D, et al. Characterization of transposon mutants of biofilm-producing Staphylococcus epidermidis impaired in the accumulative phase of biofilm production: genetic identification of a hexosamine-containing polysaccharide intercellular adhesin. Infect. Immun. 1994;62:3244–3253. doi: 10.1128/iai.62.8.3244-3253.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vuong C, Gerke C, Somerville GA, Fischer ER, Otto M. Quorum-sensing control of biofilm factors in Staphylococcus epidermidis. J. Infect. Dis. 2003;188:706–718. doi: 10.1086/377239. [DOI] [PubMed] [Google Scholar]
- 28.Augustin J, et al. Genetic analysis of epidermin biosynthetic genes and epidermin-negative mutants of Staphylococcus epidermidis. Eur. J. Biochem. 1992;204:1149–1154. doi: 10.1111/j.1432-1033.1992.tb16740.x. [DOI] [PubMed] [Google Scholar]
- 29.Galdbart JO, Morvan A, Desplaces N, el Solh N. Phenotypic and genomic variation among Staphylococcus epidermidis strains infecting joint prostheses. J. Clin. Microbiol. 1999;37:1306–1312. doi: 10.1128/jcm.37.5.1306-1312.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brückner R. Gene replacement in Staphylococcus carnosus and Staphylococcus xylosus. FEMS Microbiol. Lett. 1997;151:1–8. doi: 10.1111/j.1574-6968.1997.tb10387.x. [DOI] [PubMed] [Google Scholar]
- 31.Vuong C, Götz F, Otto M. Construction and characterization of an agr deletion mutant of Staphylococcus epidermidis. Infect. Immun. 2000;68:1048–1053. doi: 10.1128/iai.68.3.1048-1053.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Voyich JM, et al. Genome-wide protective response used by group A Streptococcus to evade destruction by human polymorphonuclear leukocytes. Proc. Natl. Acad. Sci. U. S. A. 2003;100:1996–2001. doi: 10.1073/pnas.0337370100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kadurugamuwa JL, et al. Direct continuous method for monitoring biofilm infection in a mouse model. Infect. Immun. 2003;71:882–890. doi: 10.1128/IAI.71.2.882-890.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]