Abstract
Human cytomegalovirus (HCMV) is an opportunistic pathogen that has been implicated in the pathogenesis of vascular diseases. HCMV infection of endothelial cells may lead to vascular damage in vitro, and acute-phase HCMV infection has been associated with thrombosis. We hypothesized that viral infection of endothelial cells activates coagulation cascades and contributes to thrombus formation and acute vascular catastrophes in patients with atherosclerotic disease. To assess the effects of HCMV on thrombogenesis, we examined the adhesion and aggregation of blood platelets to uninfected and HCMV-infected endothelial cells. At 7 days after infection, platelet adherence and aggregation were greater in infected than in uninfected cultures (2,000 platelets/100 cells and 225 ± 15 [mean ± standard error of the mean] aggregates/five microscopic fields versus 100 platelets/100 cells and no aggregates). von Willebrand factor (vWF), ICAM-1, and VCAM-1 but not collagen IV, E-selectin, P-selectin, CD13, and CD31 were expressed at higher levels on infected cells than on uninfected cells. Platelet aggregation was inhibited by blocking of platelet GPIb (with blocking antibodies) or GPIIb/IIIa (with ReoPro) or by blocking of vWF (with polyclonal antibodies to vWF). Furthermore, blocking of vWF, platelet GPIb, and ICAM-1 but not of the endothelial cell marker CD13, α5β3-integrin, or HCMV glycoprotein B reduced platelet adherence to infected cells by 75% ± 5%, 74% ± 5%, or 18% ± 5%, respectively. The increased thrombogenicity was dependent on active virus replication and could be inhibited by foscarnet and ganciclovir; these results suggest that a late viral gene may be mediating this phenomenon, which may contribute to vascular catastrophes in patients with atherosclerotic disease.
Human cytomegalovirus (HCMV), a member of the herpesvirus family, persists in a latent form after primary infection and can be reactivated. HCMV infections are generally subclinical but can be fatal in immunocompromised patients. About 50 to 90% of bone marrow and organ transplant recipients experience postoperative HCMV infections, and the prevalence of HCMV approaches 100% in patients infected with human immunodeficiency virus (2).
HCMV can infect virtually all organ tissues and has been implicated in the development of cardiovascular disease, chronic graft-versus-host disease, and inflammatory bowel disease (1, 7, 33). In particular, HCMV has been linked to the development of atherosclerosis, arterial restenosis after angioplasty, and transplant vascular sclerosis (TVS) (9, 22, 23, 31, 41). HCMV antigens and nucleic acids have been both detected and not detected in early lesions of diseased vessels by different investigators (23, 39), and HCMV seropositivity has been associated with the development of carotid and coronary artery diseases and TVS (22, 23, 31, 39, 41). Antiviral prophylaxis significantly decreases the risk of TVS after heart transplantation (40). Animal studies have also provided evidence for a pathological role of cytomegalovirus in the development of vascular diseases (10).
Various mechanisms have been proposed to explain the role of infectious pathogens in atherosclerosis; these include endothelial cell injury, induction of inflammation, and effects on lipid metabolism, smooth muscle cell physiology, and possibly thrombosis (16, 23, 35). However, because 60 to 90% of the population is infected with HCMV, it has been difficult to specifically link the virus to particular vascular diseases. HCMV infects endothelial cells, smooth muscle cells, and macrophages—all of which are considered to be important in the pathogenesis of vascular diseases. The virus may also contribute to the development of these diseases through its effects on various cellular and immunological functions (19).
The most appealing evidence for a direct role of HCMV in the pathogenesis of vascular diseases has been obtained from in vitro models. We previously showed that HCMV infection of smooth muscle cells results in their migration, which is mediated by the viral chemokine receptor homologue US28 (34). This observation provides a molecular link between HCMV and the pathogenesis of vascular diseases. HCMV may also exacerbate inflammation in diseased vessels by altering the expression of cell adhesion molecules and by interfering with cytokine signaling (14). It may also contribute to atherogenesis by altering lipid metabolism and increasing oxidative stress (14).
The endothelium plays a fundamental role in many vascular pathologies, including early atherogenesis, plaque rupture, restenosis after angioplasty, and late vein graft failure (25). HCMV infects endothelial cells both in vivo and in vitro and alters the expression of cell adhesion molecules (28). In patients with HCMV disease, circulating infected endothelial cells may help to disseminate the virus (12). Certain viral infections, including HCMV infection, increase the risk of thrombosis. Mesenteric arterial or venous thrombosis can occur in patients with acute-phase HCMV infections, and the virus may be associated with vasculitis in these patients (16, 26). HCMV seropositivity increases the risk of hepatic artery thrombosis fivefold (21).
Hypothetical mechanisms for the increased risk of thrombogenic events include the loss of anticoagulant factors (e.g., thrombomodulin, prostacyclin, and tissue plasminogen activator), increasing levels of procoagulation factors (e.g., factor VIII), vasculopathy, endothelitis, and anticardiolipin syndrome (24, 37). HCMV may directly damage intact vascular endothelium, possibly by altering its thromboresistant surface (37) In this study, we sought to determine whether HCMV infection alters the thrombogenic ability of human pulmonary arterial endothelial cells (HPAEC). Specifically, we examined platelet adhesion and aggregation in uninfected and HCMV-infected endothelial cell cultures. We also assessed the expression and secretion of von Willebrand factor (vWF; a protein that plays a key role in hemostasis and induction of arterial thrombosis), ICAM-1, VCAM-1, CD13, CD31, α5β3-integrin (vitronectin, vWF, fibrinogen, and thrombospondin receptor on endothelial cells), α2β1-integrin (collagen receptor), E-selectin, and P-selectin (a monocyte receptor that translocates to the endothelial cell surface in response to the local generation of thrombin on herpesvirus-infected cells).
MATERIALS AND METHODS
Cells and viruses.
HPAEC (Clonetics) were cultured in EGM-2 medium containing growth factors (Clonetics) at 37°C in 5% CO2. At 80% confluence, the cultures were infected with HCMV (laboratory strains Towne and AD169, endothelial cell-tropic strain Toledo, clinical isolate HA, purified HCMV [Towne], virus-free supernatant, and UV-irradiated virus). Infection was performed at multiplicities of infection (MOIs) of 0.5, 1, 3, and 5 for Towne and an MOI of 5 for Toledo, AD169, clinical isolate HA, and purified HCMV (Towne). UV-irradiated virus and virus-free supernatants were used in equal volumes as virus-containing stocks. To avoid inhibition of viral entry, the cells were incubated in heparin-free medium (EBM; Clonetics) with 2% fetal calf serum, 100 U of penicillin/ml, and 100 μg of streptomycin/ml for at least 1 h prior to and throughout the course of infection. Cell-free virus stocks were prepared from supernatants of HCMV-infected fibroblasts by centrifugation and were stored at −86°C until use. Platelets were obtained from the blood bank at the Karolinska University Hospital.
Purified virus preparation.
HCMV (Towne) was used to infect subconfluent human foreskin fibroblast monolayers. At 7 days postinfection (dpi), the conditioned medium was collected and centrifuged at 1,700 × g for 5 min (three times) at 4°C to remove cell debris. The supernatant was finally centrifuged at 19,000 × g for 6 h at 4°C in order to pellet virus particles. The pellet was suspended in freezing medium, consisting of 100 mM NaCl, 50 mM Tris-HCl, and 0.5 mM EDTA, and stored at −86°C.
Generation of virus-free supernatants.
Virus-containing supernatants were collected from Towne-infected human foreskin fibroblasts at 7 dpi. Harvested supernatants were filtered by using a 0.1-μm-pore-size Supor membrane (PALL Gelman Laboratory). Virus-free supernatants were determined to be free of infectious virus when the presence of immediate-early antigen (IEA) in HPAEC was investigated.
UV irradiation of a virus stock.
An HCMV stock was UV irradiated by using a Stratagene UV Stratalinker 1800 at 1,200 μJ four times. The absence of IEA in endothelial cells was investigated to ensure that UV inactivation was successful.
Platelet aggregation and adhesion assays.
At 1, 3, 5, and 7 dpi, uninfected HPAEC and HPAEC infected with Towne, purified HCMV (Towne), virus-free supernatants, UV-irradiated virus, HCMV clinical isolate HA, and endothelial cell-tropic Toledo (tagged with green fluorescent protein [GFP] expressed under the control of the HCMV IE promoter; American Type Culture Collection, Manassas, Va.) were washed and incubated with platelets diluted in 0.9% NaCl (50 platelets/cell) in the presence or absence of 2 mM CaCl2 and 2 mM MgCl2 at 37°C for 5 min with gentle stirring. In some experiments (when the cells were infected with Towne at MOIs of 0.5, 1, 3, and 5), platelets preactivated with ADP (10−6 mol/liter; Sigma, St. Louis, Mo.) were used. Platelets preactivated with thrombin (0.5 U/ml) were used as positive controls. Cells were fixed with 1% paraformaldehyde (PFA) at room temperature for 1 h. Cells then were washed with phosphate-buffered saline (PBS) to remove the PFA, and platelet aggregates (>10 platelets/cell) in each culture were counted in five microscopic fields. Adherent platelets were also counted in samples containing at least 100 HPAEC. Adherent platelets and aggregates on HPAEC were counted by light microscopy (six independent experiments). The numbers of platelets adherent to uninfected HPAEC and to cells infected with GFP-tagged endothelial cell-tropic Toledo were determined at 1 and 7 dpi by both light microscopy and fluorescence microscopy (six independent experiments).
Supernatants from uninfected and HCMV (Towne)-infected HPAEC were collected at 1, 3, 5, and 7 dpi and stored at −86°C until use. Aliquots of platelets (100 μl; 108 platelets/ml) were incubated with 100 μl of nonfiltered or filtered (0.1-μm-pore size) supernatants from infected or uninfected cells in the presence or absence of 2 mM CaCl2 and 2 mM MgCl2. Incubation was carried out with gentle stirring at 37°C for 20 min. Platelets were fixed with 1% PFA for 1 h. Platelet aggregates in each well were examined macroscopically. Platelets preactivated with thrombin (0.5 U/ml) were used as positive controls (three independent experiments).
Immunofluorescence analyses.
HPAEC were grown in 96-well tissue culture plates (Costar) and infected at 80% confluence with HCMV (Towne, AD169, Toledo, or HA). At 1, 3, 5, and 7 dpi, the cells were fixed with methanol-acetone (1:1) or 1% PFA. Double-immunofluorescence analysis was performed to detect HCMV IEA and vWF (Dakopatts, Glostrup, Denmark), collagen IV (Dakopatts), or P-selectin (Becton Dickinson, San Jose, Calif.), and three-color fluorescence analysis was performed to detect HCMV glycoprotein B (gB) (anti-gpUL55; kindly provided by William Britt, University of Alabama, Birmingham) and vWF or collagen IV. 4′,6′-Diamidino-2-phenylindole (DAPI) was used to stain the nucleus blue. Fixed cells (except those infected with Toledo, which was tagged with GFP) were incubated for 30 min with a mouse monoclonal antibody against HCMV IE protein (Argene Biosoft, Varilhes, France) or late HCMV gB. Binding of the primary antibody was detected with R-phycoerythrin-labeled anti-mouse antibody [F(ab′)2] (Dakopatts). For the detection of vWF, collagen IV, or P-selectin, infected and uninfected cells were fixed with methanol-acetone or 1% PFA and stained with a monoclonal antibody against vWF or collagen IV (Dakopatts) or against P-selectin. Binding of the primary antibody was detected with fluorescein isothiocyanate-labeled rabbit anti-mouse antibody [F(ab′)2] (Dakopatts) (six independent experiments).
Flow cytometric analyses.
Uninfected and HCMV-infected HPAEC were harvested with nonenzymatic cell dissociation solution (Sigma-Aldrich Sweden AB, Tyresö, Sweden) at 1, 3, 5, and 7 dpi, washed three times with PBS, incubated in PBS with 20% AB serum for 10 min on ice, and washed twice with PBS. For the detection of vWF or collagen IV, cells were permeabilized by incubation with Cytofix/Cytoperm solution (PharMingen, Becton Dickinson). Cells were incubated for 30 min with mouse monoclonal antibodies against human vWF, human collagen IV, ICAM-1 (Dakopatts), VCAM-1 (Dakopatts), P-selectin, E-selectin (BD Biosciences), CD13 (Dakopatts), α5β3-integrin (BD Biosciences), α2β1-integrin (BD Biosciences), and CD31 (BD Biosciences) and then with fluorescein isothiocyanate-conjugated or R-phycoerythrin-conjugated anti-mouse antibody [F(ab′)2] (Dakopatts). Cells were analyzed by flow cytometry (FACSCalibur; Becton Dickinson), and cell viability was determined by staining with 0.1% trypan blue (Sigma-Aldrich) (five independent experiments).
Western blot analyses.
Monolayers from uninfected and HCMV-infected HPAEC at 1, 3, 5, and 7 dpi were washed twice with PBS and scraped into 300 μl of lysis buffer (50 mM Tris-HCl [pH 7.4], 150 mM NaCl, 1% NP-40, 5 mM EDTA, 0.5 mM phenylmethylsulfonyl fluoride, 0.1 mg of aprotinin/ml, 0.02 mg of leupeptin/ml, 0.01 M dithiothreitol [all from Sigma-Aldrich]). After sonication and centrifugation, the supernatants were stored at −86°C until use. Protein concentrations were determined by the bicinchoninic acid method with bicinchoninic acid protein assay reagent (Pierce, Rockford, Ill.). Proteins (15 μg) were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 4 to 20% gels by the method of Laemmli (17) and processed for immunoblotting. For immunoblot analysis, the proteins were transferred electrophoretically from gels to nitrocellulose membranes (Bio-Rad, Richmond, Calif.). The immunoreactive bands were detected by incubation of the nitrocellulose membranes with a vWF-specific monoclonal antibody followed by a horseradish peroxidase-conjugated secondary antibody (Dakopatts). Finally, the bands were visualized by incubation of the nitrocellulose membranes with the chemiluminescence substrate Luminal (Amersham Biosciences, Uppsala, Sweden) and exposure to Kodak X-OMAT AR-5 film according to the manufacturer's instructions. Molecular weights were assessed in comparison to molecular weight standards (Bio-Rad) (three independent experiments).
Measurement of soluble vWF and P-selectin in supernatants obtained from uninfected and HCMV-infected HPAEC.
vWF and P-selectin levels in conditioned medium from uninfected and HCMV (Towne)-infected HPAEC were measured at 1, 3, 5, and 7 dpi by enzyme-linked immunosorbent assays (ELISAs) (a vWF ELISA kit from America Diagnostica and a P-selectin ELISA kit from R&D Systems, Minneapolis, Minn.). A standard curve was generated with commercial vWF (America Diagnostica) and P-selectin (R&D Systems) (three independent experiments carried out in triplicate).
Measurement of soluble P-selectin and serotonin in supernatants obtained from platelets incubated with uninfected or HCMV-infected HPAEC.
Soluble P-selectin and serotonin levels in supernatants obtained from cultures containing platelets incubated on uninfected or HCMV-infected HPAEC were measured at 1, 3, 5, and 7 dpi by ELISAs (the serotonin ELISA kit from Beckman Coulter, Bromma, Sweden). A standard curve was generated with commercial P-selectin and serotonin (Beckman Coulter).
Measurement of P-selectin expression on platelets incubated with supernatants from uninfected and HCMV-infected HPAEC.
Nonfiltered and filtered (0.1-μm-pore size) supernatants from uninfected and HCMV-infected HPAEC were collected at 1, 3, 5, and 7 dpi and incubated with platelets (107/well) in 96-well plates (Maxisorp; Nunc, Roskilde, Denmark) in the presence of 2 mM CaCl2 and 2 mM MgCl2. Incubation was carried out with gentle stirring at 37°C for 20 min. Following centrifugation at 640 × g for 15 min, the platelets were fixed with 1% PFA for 20 min. Supernatants were removed, and the fixed platelets were washed. Following incubation of the fixed platelets with 5% bovine serum albumin (Sigma), the cells were incubated first with mouse monoclonal antibodies against P-selectin and then with peroxidase-conjugated rabbit anti-mouse antibodies. Finally, the cells were incubated with the substrate 3,3′,5,5′-tetramethylbenzidine (Sigma), and the absorbance was measured with a spectrophotometer.
Blocking of vWF, ICAM-1, HCMV gB, α5β3-integrin, and CD13 on endothelial cells.
To obtain anti-vWF, anti-ICAM-1, and anti-α5β3-integrin F(ab′)2 fragments, polyclonal mouse anti-vWF (Dakopatts) and monoclonal anti-ICAM-1 and anti-α5β3-integrin antibodies were digested with pepsin (2 mg/ml of immunoglobulin G [IgG]) for 24 h at 37°C and dialyzed (3 mg/ml of purified IgG) against acetate buffer (pH 4.0) for 4 h at 4°C; the reaction was stopped by the addition of 2 M Tris. The digested protein was dialyzed against PBS overnight, and the F(ab′)2 fragments were separated after incubation with protein A for 1 h at 4°C. F(ab′)2 fragments of CD13-specific antibodies (MY7; Coulter Clone) and mouse IgG (Dakopatts) were obtained in the same way. Uninfected and HCMV (Towne)-infected HPAEC were incubated with polyclonal mouse anti-human vWF F(ab′)2 at a concentration of 0.5 mg/ml (at 7 dpi) and with monoclonal mouse anti-ICAM-1 F(ab′)2 at 1 mg/ml (at 1 and 7 dpi), anti-α5β3-integrin F(ab′)2 at 0.5 mg/ml (at 1 and 7 dpi), and anti-HCMV gB F(ab′)2 at 1 mg/ml (kindly provided by Mats Olin, Lund University, Lund, Sweden) in heparin-free EBM with 2% fetal calf serum, 100 U of penicillin/ml, and 100 μg of streptomycin/ml for 1 h at 37°C in 5% CO2. Cells were washed with PBS. Platelet adhesion and aggregation were assessed as described above. Mouse anti-human CD13 (MY7) F(ab′)2 and mouse IgG F(ab′)2 were used as controls at the same concentrations as anti-human vWF F(ab′)2 antibodies (three independent experiments).
Blocking of platelet GPIIb/IIIa and GPIb.
At 7 dpi, uninfected and HCMV (Towne)-infected HPAEC were washed with PBS and incubated with platelets diluted in 0.9% NaCl (50 platelets/cell) and ReoPro (abciximab; Eli Lilly, Stockholm, Sweden; 0.125 mg/ml), which blocks platelet GPIIb/IIIa, in the presence of 2 mM Ca2+ and Mg2+ at 37°C for 5 min with gentle stirring. Furthermore, at 1 and 7 dpi, uninfected and HCMV (Towne)-infected HPAEC were washed and incubated with platelets on which GPIb was blocked by using anti-human CD42b antibodies (BD Biosciences; 0.1 mg/ml) at room temperature for 1 h with gentle stirring. Cells were fixed with 1% PFA for 1 h and then washed with PBS to remove PFA. Platelet adhesion was assessed as described above (three independent experiments).
Inhibition of HCMV infection in endothelial cells.
At 1, 3, 5, and 7 dpi, uninfected and HCMV (Towne or Toledo)-infected HPAEC were left untreated or were treated with 3.0 mM foscarnet (Foscavir; Astra Zeneca, Södertälje, Sweden) or 1.2 mM ganciclovir (Astra Zeneca) for the remainder of the infection period. Foscarnet and ganciclovir block the expression of late viral genes. To exclude toxicity effects of these antiviral agents, cells were examined by trypan blue staining. No toxicity was observed at the concentrations used. The ability of cells to induce platelet adherence and platelet aggregation was examined as described above. The expression of HCMV IEA and HCMV gB was determined by immunofluorescence analysis as described above (six independent experiments).
Statistical methods.
The values are expressed as the means ± standard errors of the means (SEMs), and statistical significance was tested by using Student's unpaired t test.
RESULTS
HCMV-infected endothelial cells are thrombogenic.
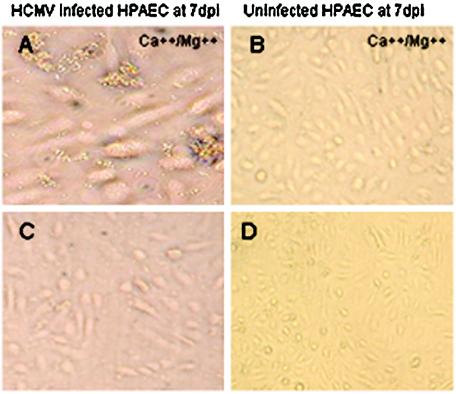
To assess the effects of HCMV on platelet adhesion and aggregation, we incubated uninfected and HCMV (Towne, Toledo, purified virus [Towne], UV-irradiated virus [Towne], or virus-free supernatant)-infected HPAEC with blood platelets in the presence or absence of CaCl2 and MgCl2. Within 5 min, platelet aggregation was macroscopically visible in some infected cultures (Towne at MOIs of 3 and 5; Toledo and purified virus at an MOI of 5) (data not shown). The cells then were fixed and washed, and adherent platelets and aggregates on HPAEC were counted by light microscopy. No aggregates were seen in uninfected cultures (Fig. 1B and D), in cultures infected with UV-irradiated virus or virus-free supernatant (data not shown), or HCMV-infected cultures in the absence of CaCl2 and MgCl2 (Fig. 1C). In infected cultures, platelet adherence and aggregation occurred only in the presence of CaCl2 and MgCl2 (Fig. 1A) and increased with time after infection. Aggregation (>10 platelets/cell; generally at least 40 platelets/aggregate) was observed after 3 dpi. Platelets pretreated with thrombin aggregated within a few seconds on uninfected or HCMV-infected HPAEC in the presence or absence of Ca2+ and Mg2+ (data not shown).
FIG. 1.
Platelet adherence and aggregation on HCMV-infected HPAEC. Uninfected and HCMV-infected HPAEC cultures were incubated with blood platelets in the presence or absence of Ca2+ and Mg2+. Platelet aggregation was observed on HCMV-infected cells in the presence of Ca2+ and Mg2+ (A) but not in the absence of Ca2+ and Mg2+ (C). Platelet aggregation was not observed on uninfected cells in the presence or absence of Ca2+ and Mg2+ (B and D). Original magnifications: A, ×40; C, ×20; B, ×20; D, ×10. Six experiments were done.
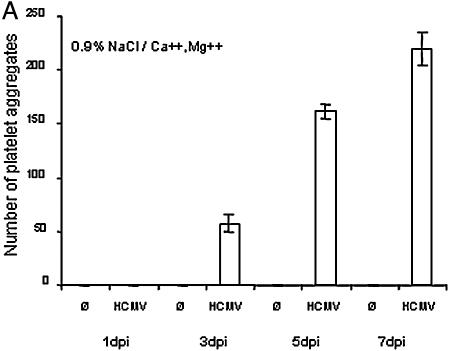
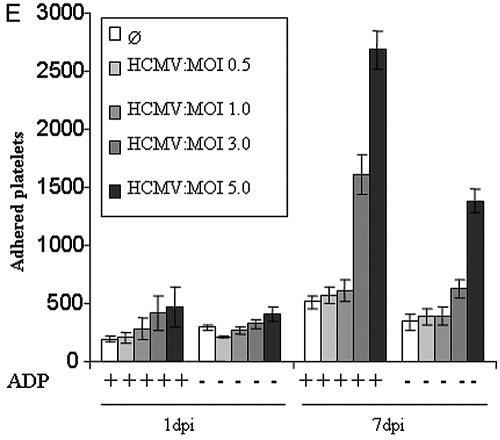
In each infected culture, the mean ± SEM numbers of aggregates were 150 ± 5 at 5 dpi and 225 ± 15 at 7 dpi (Fig. 2A ). Platelet adherence was 8-fold greater to infected cells than to uninfected cells at 5 dpi and 10-fold greater at 7 dpi (Fig. 2B). No significant increase in the number of adherent platelets was observed in cultures infected with UV-irradiated virus or virus-free supernatant compared to uninfected cultures (Fig. 2C). In the absence of CaCl2 and MgCl2, however, only a twofold increase was seen at 5 dpi and a fourfold increase was seen at 7 dpi (Fig. 2D). Furthermore, preactivation of platelets with ADP induced a change in platelet shape and a significantly increased number of adherent platelets in HCMV-infected cultures (MOIs of 3 and 5) at 7 dpi compared to uninfected cultures (Fig. 2E). These results suggest that increased platelet adherence is a characteristic of HCMV-infected endothelial cells.
FIG. 2.
Increasing platelet adherence and aggregation on HCMV-infected HPAEC with MOI and time after infection. Platelets were incubated with uninfected and HCMV (Towne)-infected HPAEC (1, 3, 5, and 7 dpi) in the presence of Ca2+ and Mg2+. Cells were fixed, and aggregates containing >10 platelets/cell were counted in five representative microscopic fields. No aggregates were seen in uninfected cultures. The number of platelet aggregates increased with increasing time of infection (A). Platelets were incubated with uninfected and HCMV (Towne)-infected HPAEC in the presence or absence of Ca2+ and Mg2+. Adherent platelets were counted after fixation. At least 100 HPAEC were examined in each sample. In the presence of Ca2+ and Mg2+, platelet adherence to infected cells was 8-fold greater than that to uninfected cells at 5 dpi and 10-fold greater at 7 dpi (B). No significant change in the number of adherent platelets was observed in cultures infected with UV-irradiated virus or virus-free supernatants compared to uninfected cultures (C). In the absence of CaCl2 and MgCl2, however, only a twofold increase was seen at 5 dpi and a fourfold increase was seen at 7 dpi (D). Furthermore, the number of adherent platelets in HCMV-infected cultures (at MOIs of 3 and 5) at 7 dpi was significantly higher with ADP preactivation than without it (E). The numbers of adherent platelets in cultures infected with GFP-tagged endothelial cell-tropic HCMV strain Toledo at 1 and 7 dpi were three and five times larger, respectively, than those in uninfected cultures (F). Data represent the mean ± SEM for six experiments.
We also found that the numbers of platelets adherent to infected cells were 3 and 5 times higher at 1 and 7 dpi, respectively, than the numbers of platelets adherent to uninfected cells (Fig. 2F).
Platelet aggregation was macroscopically visible in wells containing nonfiltered or filtered supernatants from HCMV-infected HPAEC collected at 5 and 7 dpi (only in the presence of Ca2+ and Mg2+). No aggregation was observed in wells containing supernatants from uninfected cells (data not shown).
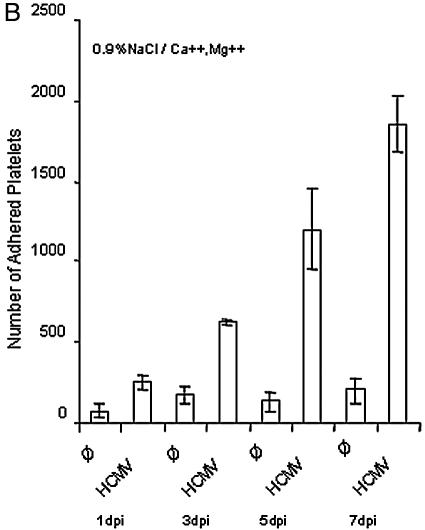
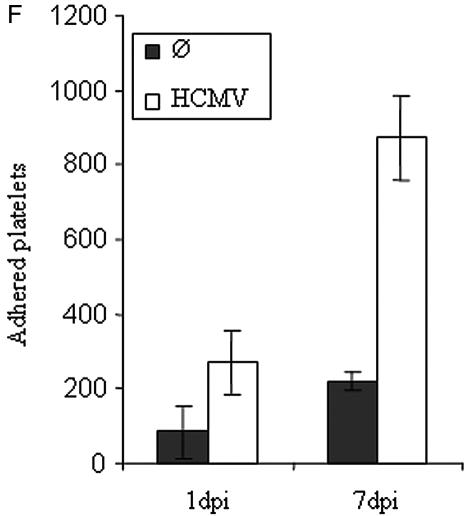
Next, we examined the abilities of various strains of HCMV (laboratory strains Towne and AD169, endothelial cell-tropic strain Toledo, and clinical isolate HA) to infect HPAEC and to mediate platelet adhesion and aggregation. After infection with AD169 and HA, less than 10% of infected cells expressed HCMV IEA (data not shown). After infection with Towne and Toledo, however, 80% of HCMV-positive cells expressed HCMV IEA and 40% expressed HCMV gB at 7 dpi (data not shown). Treatment with 3.0 mM foscarnet or 1.2 mM ganciclovir during the time of infection (5 and 7 days) completely blocked platelet aggregation and significantly reduced platelet adherence in Towne-infected HPAEC (Fig. 3). Foscarnet and ganciclovir also reduced HCMV gB expression by 95% but did not affect the expression of HCMV IEA (data not shown).
FIG. 3.
Foscarnet and ganciclovir blocked blood platelet aggregation in HPAEC cultures infected with HCMV. Platelet aggregation did not occur in HCMV-infected HPAEC cultures treated with foscarnet or ganciclovir (A). The numbers of platelets that adhered to foscarnet- or ganciclovir-treated HCMV-infected HPAEC were significantly reduced at various times after infection (B and C). Data represent the mean ± SEM for three experiments.
HCMV infection increases intracellular and cell surface expression of vWF.
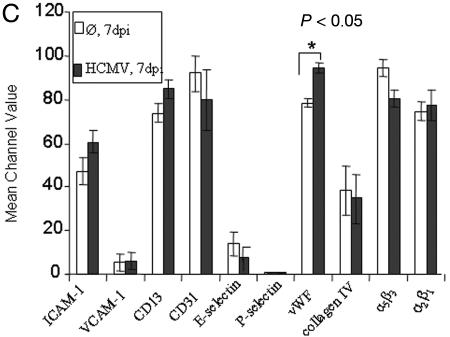
In response to vascular damage, vWF, CAMs, selectins, and collagen IV are expressed on the vascular endothelium, but mainly vWF appears to initiate thrombogenesis (8). The patterns of expression of vWF, collagen IV, ICAM-1, VCAM-1, P-selectin, E-selectin, CD13 α5β3-integrin, α2β1-integrin, and CD31 on uninfected and HCMV-infected HPAEC at 1, 3, 5, and 7 dpi were examined by flow cytometric analyses.
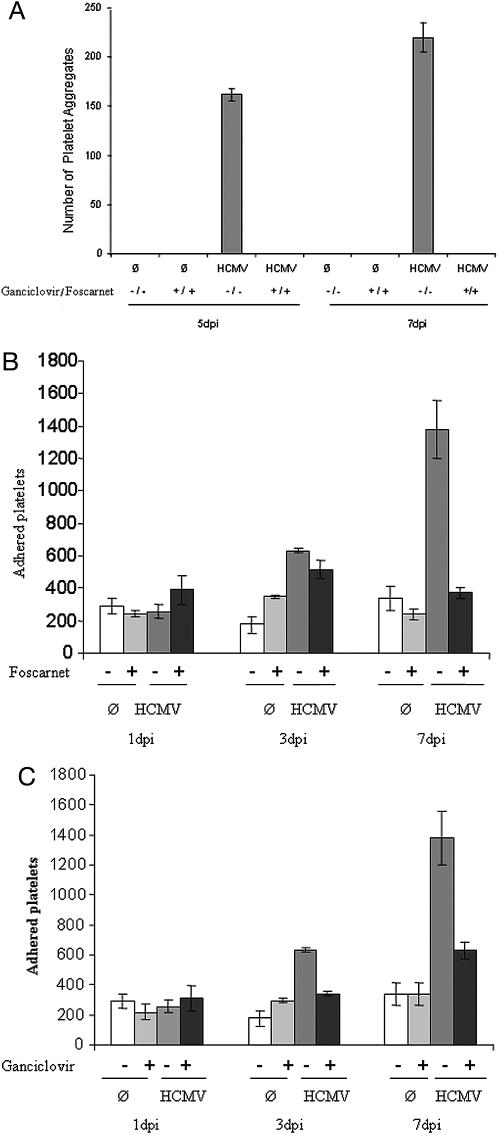
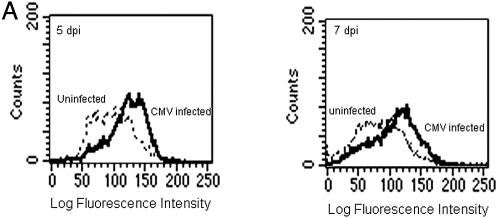
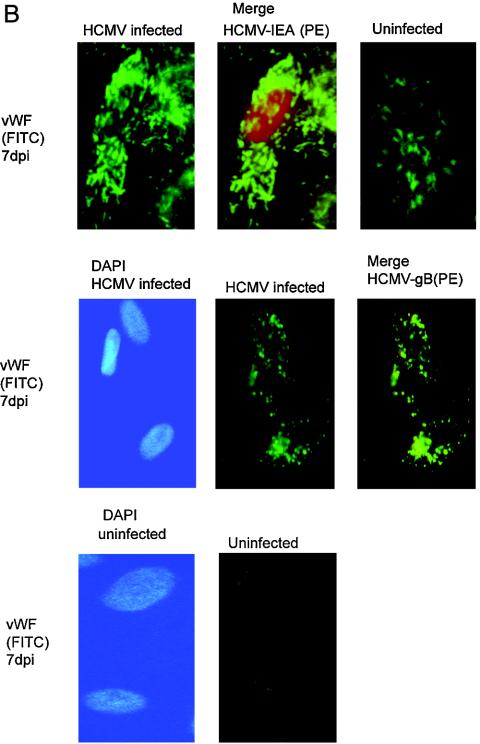
We also investigated the expression of intracellular and cell surface-bound vWF and the extracellular levels of collagen IV in HPAEC infected with Towne, Toledo, AD169, and HA. In addition, we examined the expression of ICAM-1, VCAM-1, E-selectin, P-selectin, CD13, and CD31 on HCMV (Towne or AD169)-infected HPAEC and of α5β3-integrin and α2β1-integrin on HCMV (Towne)-infected cells. As shown by flow cytometry, the levels of intracellular and membrane-bound vWF at 5 dpi (P < 0.005) and 7 dpi (P < 0.05) were higher in cells infected with Towne (Fig. 4A) and Toledo than in uninfected cells or cells infected with HA or AD169 (data not shown). In addition, we observed a stronger fluorescence signal for vWF in cells infected with Towne (Fig. 4B) and Toledo (data not shown) than in uninfected cells (Fig. 4C). Furthermore, we did not detecte P-selectin on HCMV (Towne)-infected cells but did detect P-selectin on uninfected cells (data not shown). In addition, while the expression of ICAM-1 increased with time (1 to 5 dpi) and the expression of VCAM-1 increased at 5 dpi, P-selectin could not be detected on uninfected or infected cells by flow cytometric analyses (data not shown). Furthermore, whereas infection of HPAEC with Towne resulted in a slight reduction in the expression of α5β3-integrin at 3 to 7 dpi (Fig. 4A), the expression of α2β1-integrin decreased at 3 dpi and increased at 5 dpi (data not shown). No significant differences in the expression of collagen IV, E-selectin, CD13, and CD31 were observed between infected and uninfected cells (Fig. 4A).
FIG. 4.
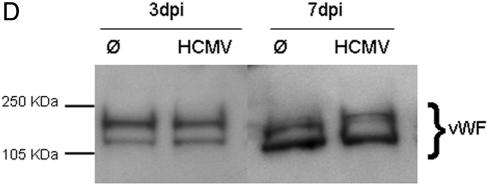
HCMV infection of HPAEC increases intracellular and cell surface expression of vWF. (A) As shown by flow cytometry, the levels of intracellular and membrane-bound vWF at 5 and 7 dpi were higher in cells infected with Towne than in uninfected cells. (C) While the expression of vWF was increased, no significant differences in the expression of ICAM-1, VCAM-1, collagen IV, P-selectin, E-selectin, α2β1-integrin, CD13, and CD31 could be detected between infected cells and uninfected cells at 7 dpi. However, infecting HPAEC with HCMV (Towne) at 7 dpi resulted in a slight reduction in the expression of α5β3-integrin. Data represent the mean ± SEM for five experiments. An unpaired t test was used for statistical analysis; the asterisk indicates a P value of <0.05. (B) Fluorescence microscopy analysis of uninfected and HCMV-infected HPAEC at 7 dpi (fixed with acetone and methanol) demonstrated higher expression of intracellular vWF (green) on HPAEC expressing HCMV IEA (red) (top row, left and middle panels) than on uninfected cells (top row, right panel). Fluorescence microscopy analysis of uninfected and HCMV-infected HPAEC at 7 dpi (fixed with 1% PFA) demonstrated higher expression of cell surface-bound vWF (green) on HPAEC expressing HCMV gB (red) (middle row, middle and right panels) than on uninfected cells (bottom row, right panel). DAPI was used to stain the nucleus blue in uninfected and HCMV-infected HPAEC (middle and bottom rows, left panels). PE, phycoerythrin; FITC, fluorescein isothiocyanate. (D) Western blot analysis showed no difference in the amounts of vWF in uninfected and HCMV-infected HPAEC (three experiments).
We also performed Western blot analysis to detect the amounts of vWF protein in uninfected and HCMV-infected HPAEC at different times after infection. However, we did not observe a difference in the amounts of vWF protein in cells from uninfected and infected cultures (Fig. 4C).
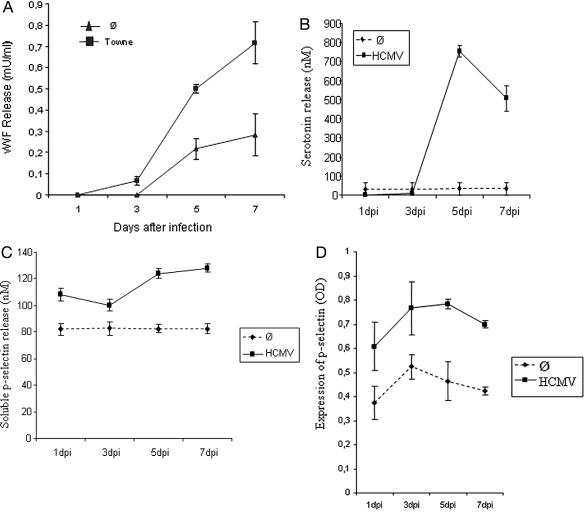
Next, we assessed soluble vWF and P-selectin secretion by uninfected and HCMV-infected cultures secreted into the culture medium by uninfected and Towne-infected HPAEC at 1, 3, 5, and 7 dpi. While infected cells secreted 2.5-fold more vWF than uninfected cells at 5 and 7 dpi (Fig. 5A), the amount of soluble P-selectin was surprisingly negligible (data not shown). We also examined the secretion of serotonin and soluble P-selectin from platelets incubated with uninfected and HCMV-infected cells at 1, 3, 5, and 7 dpi. High levels of P-selectin and serotonin were released from platelets incubated with supernatants obtained from HCMV-infected cells collected at 5 and 7 dpi (Fig. 5B and C) but not from platelets incubated with uninfected cells.
FIG. 5.
(A) Release of soluble vWF from uninfected and HCMV-infected HPAEC, as measured by an ELISA. Infected cells secreted 2.5-fold more vWF than uninfected cells at 5 and 7 dpi. (B and C) Secretion of serotonin (B) and soluble P-selectin (C) from platelets incubated with uninfected and HCMV-infected cells at 1, 3, 5, and 7 dpi. High levels of P-selectin and serotonin were observed to be secreted from platelets incubated with HCMV-infected cells at 5 and 7 dpi compared to platelets incubated with uninfected cells. (D) Expression of P-selectin on platelets incubated with nonfiltered or filtered supernatants obtained from HCMV-infected cells. Expression was twofold higher for HCMV-infected cells than for uninfected cells. OD, optical density. Data represent the mean ± SEM for three experiments.
Furthermore, we also measured the expression of P-selectin on platelets incubated with nonfiltered or filtered supernatants obtained from HCMV-infected cells by an ELISA. The expression of P-selectin on the platelet surface was increased twofold on platelets incubated with supernatants from HCMV-infected cells compared to uninfected cells (Fig. 5D).
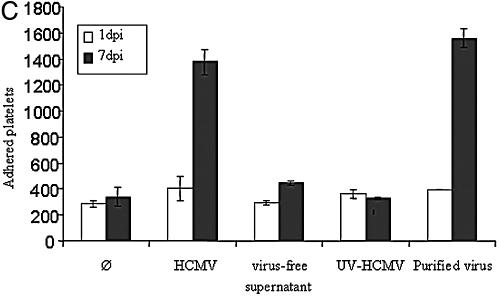
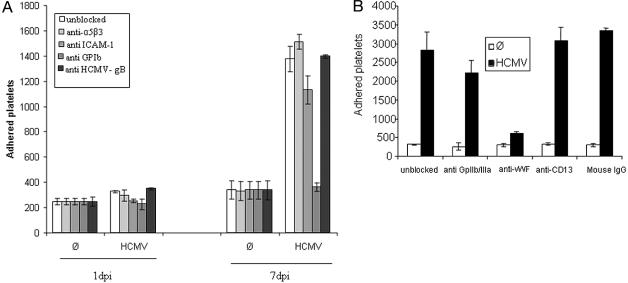
To determine whether molecules that are involved in the normal aggregation of platelets were also involved in the HCMV-induced aggregation process, we treated uninfected and HCMV (Towne)-infected HPAEC with F(ab′)2 fragments of mouse polyclonal antibodies against human vWF (at 7 dpi), monoclonal antibodies against ICAM-1, HCMV gB, and α5β3-integrin (at 1 and 7 dpi) and CD13, or mouse IgG at 7 dpi before the addition of platelets. Furthermore, we blocked platelet GPIb by using monoclonal antibodies and the GPIIb/IIIa protein by using ReoPro (which binds to GPIIb/IIIa on platelets). While blocking of vWF and ICAM-1 on HCMV-infected HPAEC and GPIb on platelets reduced the number of platelets adherent to HCMV-infected cells at 7 dpi by 75, 18, and 74%, respectively, anti-platelet GPIIb/IIIa treatment with ReoPro and blocking of α5β3-integrin, HCMV gB, or CD13 did not reduce the number of adherent platelets compared to that in untreated cells (Fig. 6). Furthermore, at 1 dpi, blocking of ICAM-1, GPIb, and α5β3-integrin reduced the number of adherent platelets by 23, 30, and 9%, respectively (Fig. 6A). However, platelet aggregation was completely inhibited by blocking of either vWF or GPIb with F(ab′)2 fragments of specific antibodies or platelet GPIIb/IIIa with ReoPro. An effect on platelet aggregation was not observed with F(ab′)2 fragments of antibodies against ICAM-1, HCMV gB, α5β3-integrin, and CD13 or mouse IgG (data not shown).
FIG. 6.
(A and B) The expression of vWF, ICAM-1, HCMV gB, and α5β3-integrin (at 1 and 7 dpi), CD13, or mouse IgG was blocked before the addition of platelets. Furthermore, the expression of platelet GPIb and GPIIb/IIIa proteins was also blocked. While blocking of vWF and ICAM-1 on HCMV-infected HPAEC and platelet GPIb reduced the number of platelets adherent to HCMV-infected cells at 7 dpi by 75, 18, and 74%, respectively, anti-platelet GPIIb/IIIa treatment with ReoPro and blocking of α5β3-integrin or HCMV gB did not reduce the number of adherent platelets compared to that seen in untreated cells. At 1 dpi, blocking of ICAM-1, GPIb, and α5β3-integrin reduced the number of adherent platelets by 23, 30, and 9%, respectively. Data represent the mean ± SEM for three experiments.
DISCUSSION
This study shows that HCMV infection of HPAEC induces platelet adherence and aggregation and that the expression of vWF increases with time after infection. At late time points, platelet aggregation was inhibited by blocking vWF expression on HCMV infected cells with polyclonal antibodies against vWF or by blocking platelet GPIb with monoclonal antibodies or GPIIb/IIIa with ReoPro (11). These data suggest that molecules that are involved in the normal aggregation of platelets are also involved in the HCMV-induced aggregation process. Inhibiting HCMV infection with the antiviral drug foscarnet or ganciclovir also blocked platelet aggregation and significantly reduced the number of platelets adherent to endothelial cells. Since HCMV-infected cells treated with foscarnet or ganciclovir expressed IEA but not late HCMV protein gB, these results suggest that a viral gene produced late during the infectious cycle is responsible for the increased thrombogenesis. Importantly, these observations provide a rationale for the use of antiviral therapy during HCMV infection, especially in patients already at risk of thrombogenic events.
The endothelial cell is a key cell type in the pathogenesis of HCMV infection (29). Endothelial cells, particularly those from the microvasculature in the brain, lungs, heart, gastrointestinal tract, and placenta, are frequently infected (29), and circulating infected endothelial cells have been identified in HCMV-infected patients. The ability of HCMV to replicate in endothelial cells is also considered important in enabling the virus to maintain a lifelong infection within the host.
The replication of HCMV in endothelial cells is influenced by the viral strain, suggesting that specific viral genes may be required for efficient replication in this cell type (4). In our study, only about 10% of endothelial cells were infected with laboratory-adapted strain AD169 or clinical isolate HA, whereas 70 to 80% were infected with laboratory-adapted strains Towne and Toledo. In early studies, clinical HCMV isolates lost their endothelial tropism after multiple passages in human fibroblasts (commonly used to produce high-titer virus stocks), suggesting that certain properties of the virus are lost after propagation in these cells (20, 30).
Although there is evidence for a genetic basis of cell tropism (20), the genes responsible have been difficult to identify. In our study, infection with strain Towne or Toledo increased the intracellular and cell surface expression of vWF. Furthermore, infecting HPAEC with HCMV (Towne) at 3 to 7 dpi resulted in a slight reduction in the expression of α5β3-integrin, probably either as a result of infection or because epitopes were occupied by binding of released vWF to α5β3-integrin (which may serve as a receptor for vWF).
However, in cells infected with HA or AD169, vWF and collagen IV were expressed at lower levels than in uninfected cells. Furthermore, cells infected with Towne secreted significantly higher levels of soluble vWF than uninfected cells, is in accordance with the findings of Bruggeman et al., who reported reduced expression of vWF in AD169-infected cells (3). Our findings are also supported by the observation in vivo that the level of vWF in plasma has been shown to be increased during HCMV infection in kidneys (13).
vWF plays a key role in hemostasis and induction of arterial thrombosis. Indeed, in rheological situations, where platelets are flowing at a physiologic speed in vitro, the only reaction that appears to initiate mural thrombogenesis is the interaction of vWF with platelet GpIb (8). vWF can be released by stimulation with various factors, such as stress hormones or adrenaline and desmopressin (8). vWF can be expressed by binding to subendothelial microfibrils on stimulated or damaged endothelial cells (8). Interactions of circulating vWF in plasma with platelet GPIIb/IIIa may regulate platelet-to-platelet contact and platelet adhesion to the subendothelial matrix (8). In this study, we have shown that platelet aggregation and adhesion to virus-injured endothelial cells may be mediated by the surface expression of vWF on the cells in an in vitro model. Further studies that aim to study these phenomena under flow conditions are ongoing in our laboratory.
We observed increased secretion of soluble vWF and increased cell-surface expression of vWF by HCMV-infected HPAEC. However, in a Western blot analysis, no difference was found in the levels of vWF between uninfected and infected cells. Furthermore, we could not detect the expression of P-selectin (by flow cytometry) or the increased release of P-selectin (by an ELISA) from infected cells. The level of expression of P-selectin was, however, low in infected cells compared to uninfected cells by immunofluorescence analysis. These data may be explained by rapid degradation or autocrine uptake of released P-selectin from infected cells.
In human umbilical vein endothelial cells infected with herpes simplex virus (HSV) type 1, platelet adhesion appears to be mediated by HSV type 1 glycoprotein C, which can bind to and activate coagulation factor X, leading to thrombin generation and platelet adhesion (38). Visser et al. suggested that decreased prostacyclin synthesis may account in part for the increased adherence of platelets to HSV-infected endothelial cells; however, indomethacin did not abolish the increased adherence, indicating that other factors, possibly vWF, may be involved (38). With regard to HCMV, a number of reports have shown increased expression of sialyl Lewis(x) and ICAM-1 on endothelial cells; both of these may increase thrombogenicity and leukocyte adherence, respectively (5, 28). In this study, we found that the number of adherent platelets on infected cells was significantly reduced at late time points in cells treated with foscarnet or ganciclovir. UV-treated virus was not able to induce platelet adherence and aggregation. These observations suggest that active virus replication and a late viral gene are involved in these phenomena. Furthermore, platelet adhesion was completely or significantly reduced by blocking of vWF or platelet GPIb, but blocking of platelet GPIIb/IIIa did not significantly inhibit platelet adhesion to HCMV-infected cells. Furthermore, blocking of ICAM-1 on HCMV-infected HPAEC at 1 and 7 dpi reduced the numbers of adherent platelets by 23 and 18%, respectively. These data suggest that increased expression of ICAM-1 on endothelial cells may also increase thrombogenicity. None of these studies was performed under flow conditions. Therefore, it is presently unknown how the various viruses affect thrombogenic events under flow conditions.
The results of our study show an activation of platelets that come in contact with HPAEC infected with HCMV at late time points after infection. This activation results in the release of soluble P-selectin and serotonin from activated platelets, and increased expression of P-selectin was detected on platelets incubated with supernatants from HCMV-infected cells but not on platelets incubated with supernatants from uninfected cells. This activation could be mediated by soluble factors, such as vWF, released by HCMV-infected cells at late time points after infection. However, experiments determining the role of such up-regulation in increased thrombogenesis cannot be conclusive when blocking agents are used, since their action is dependent on the presence of vWF to mediate increased platelet adherence and aggregation. Hence, it is unclear whether the up-regulation of vWF expression on HCMV-infected cells leads to the increased thrombogenicity observed in this study.
Increasing evidence suggests that HCMV infection can induce vascular damage that may be directly associated with thrombosis and life-threatening complications. However, vasculopathy with thrombosis is a rare presentation of HCMV infection; it is primarily reported in transplant patients receiving high-dose immunosuppressive therapy and in patients infected with human immunodeficiency virus (15, 32). In a review of 102 cardiac transplant patients, McDonald et al. (22) found that 16% had accelerated allograft vasculopathy; moreover, 62% of the HCMV-seropositive patients had evidence of coronary vascular thrombosis, compared with only 25% of HCMV-seronegative patients. Furthermore, in several case reports, extensive vascular involvement and thrombosis were noted in nonimmunocompromised hosts with acute-phase HCMV infections (18, 26). Microscopic examination typically revealed evidence of perivascular inflammation, endothelial and smooth muscle cell proliferation, and thrombosis (26).
HCMV infection of endothelial cells has also been proposed as a cause of hepatic artery thrombosis (27). Several case reports have described immunocompetent persons with acute-phase HCMV infections that were complicated by extensive vasculitis and thrombosis of the hepatoportal veins and mesenteric arteries and splenic infarctions (26, 27). Hence, HCMV may promote thrombosis and disseminated intravascular coagulation as a result of endothelial injury—or, as we have found, possibly by increasing the surface expression of vWF, perhaps by causing the translocation of already formed vWF present in Weibel-Palade bodies to the cell surface, as suggested by Etingin et al. (6). In vitro, HCMV infects and appears to rapidly convert vascular endothelial cells from a noncoagulant to a procoagulant phenotype (36) through the expression of an unknown viral late gene(s). Attempts to identify this viral mechanism are ongoing in our laboratory.
Acknowledgments
This study was supported by grants from the Swedish Research Council (K2002-16X-12615-05B), the Swedish Society of Medicine (2002-761 and 2003-633), the Tobias Foundation (20/01, 33/02, and 28/03), the Heart and Lung Foundation (2001;41486 and 1999;41305), the Swedish Children's Cancer Research Foundation (PROJ 01/046), and the Emil and Wera Cornells Foundation.
REFERENCES
- 1.Berk, T., S. J. Gordon, H. Y. Choi, and H. S. Cooper. 1985. Cytomegalovirus infection of the colon: a possible role in exacerbation of inflammatory bowel disease. Am. J. Gastroenterol. 80:355-360. [PubMed] [Google Scholar]
- 2.Britt, W. J., and M. Mach. 1996. Human cytomegalovirus glycoproteins. Intervirology 39:401-412. [DOI] [PubMed] [Google Scholar]
- 3.Bruggeman, C. A., W. H. Debie, A. D. Muller, B. Schutte, and M. C. van Dam-Mieras. 1988. Cytomegalovirus alters the von Willebrand factor content in human endothelial cells. Thromb. Haemost. 59:264-268. [PubMed] [Google Scholar]
- 4.Brune, W., C. Menard, J. Heesemann, and U. H. Koszinowski. 2001. A ribonucleotide reductase homolog of cytomegalovirus and endothelial cell tropism. Science 291:303-305. [DOI] [PubMed] [Google Scholar]
- 5.Cebulla, C. M., D. M. Miller, D. A. Knight, B. R. Briggs, V. McGaughy, and D. D. Sedmak. 2000. Cytomegalovirus induces sialyl Lewis(x) and Lewis(x) on human endothelial cells. Transplantation 69:1202-1209. [DOI] [PubMed] [Google Scholar]
- 6.Etingin, O. R., R. L. Silverstein, and D. P. Hajjar. 1993. Von Willebrand factor mediates platelet adhesion to virally infected endothelial cells. Proc. Natl. Acad. Sci. USA 90:5153-5156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grattan, M. T., V. A. Moreno-Cabral, P. E. Starnes, P. E. Oyer, E. B. Stinsen, and N. E. Shunway. 1989. Cytomegalovirus infection is associated with cardiac allograft rejection and atherosclerosis. JAMA 261:3561-3566. [PubMed] [Google Scholar]
- 8.Hoffbrand, A. V., and J. E. Pettit. 1993. Platelets, blood, coagulation and haemostasis. Essential haematology, p. 299-317. Blackwell Publishers, London, United Kingdom.
- 9.Horne, D. B., J. B. Muhlestein, J. F. Cariquist, T. L. Bair, T. E. Madsen, N. I. Hart, and J. L. Andersson. Inter mountain Heart collaborative (THC) study Group. 2003. Statin therapy interacts with cytomegalovirus seropositivity and high C-reactive protein in reducing mortality among patients with angiographically significant coronary disease. Circulation 107:258-263. [DOI] [PubMed] [Google Scholar]
- 10.Hsich, E., Y. F. Zhou, B. Paigen, T. M. Johnson, M. S. Burnett, and S. E. Epstein. 2001. Cytomegalovirus infection increases development of atherosclerosis in apolipoprotein-E knockout mice. Atherosclerosis 156:23-28. [DOI] [PubMed] [Google Scholar]
- 11.Ibbotson, T., J. K. McGavin, and K. L. Goa. 2003. Spotlight on abciximab in patients with ischemic heart disease undergoing percutaneous coronary revascularization. Am. J. Cardiovasc. Drugs 3:381-386. [DOI] [PubMed] [Google Scholar]
- 12.Kas-Deelen, A. M., M. C. Harmsen, de Maar, E. F., W. J. VanSon, and T. H. The. 1998. A sensitive method for quantify cytomegalic endothelial cells in peripheral blood from cytomegalovirus-infected patients. Clin. Diagn. Lab. Immunol. 5:622-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kas-Deelen, A. M., M. C. Harmsen, E. F. De Maar, W. W. Oost-Kort, J. W. Tervaert, J. Van Der Meer, W. J. Van Son, and T. H. The. 2000. Acute rejection before cytomegalovirus infection enhances von Willebrand factor and soluble VCAM-1 in blood. Kidney Int. 58:2533-2542. [DOI] [PubMed] [Google Scholar]
- 14.Koskinen, P. K., E. A. Kalli, J. M. Tikkanen, R. K. Sihvola, P. J. Hayry, and K. B. Lemstrom. 1999. Cytomegalovirus infection and cardiac allograft vasculopathy. Transpl. Infect. Dis. 1:115-126. [DOI] [PubMed] [Google Scholar]
- 15.Koskinen, P. K., M. S. Nieminen, and L. A. Krogerus. 1993. Cytomegalovirus infection and accelerated cardiac allograft vasculopathy in human cardiac allografts. J. Heart Lung Transplant. 12:724-729. [PubMed] [Google Scholar]
- 16.Labarca, J. A., P. A. Gaete, M. Gutierrez, and C. M. Perez. 2002. Thrombosis, vasculitis, and cytomegalovirus infection. Clin. Infect. Dis. 34:1658-1659. [DOI] [PubMed] [Google Scholar]
- 17.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacterophage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 18.Lanari, M., T. Lazzartto, I. Papa, V. Venturi, G. Bronzetti, B. Guerrra, G. Faldella, L. Govaglia, F. M. Picchio, M. P. Landini, and G. P. Salvioli. 2002. Neonatal aortic arch thrombosis as a result of congenital cytomegalovirus infection. Pediatrics 108:E114. [DOI] [PubMed] [Google Scholar]
- 19.Loenen, W. A., C. A. Bruggeman, and E. J. Wiertz. 2001. Immune evasion by human cytomegalovirus: lessons in immunology and cell biology. Semin. Immunol. 13:41-49. [DOI] [PubMed] [Google Scholar]
- 20.MacCormac, L. P., and J. E. Grundy. 1999. Two clinical isolates and Toledo strain of cytomegalovirus contain endothelial cell tropic variants that are not present in the AD169, Towne, or Davis strain. J. Med. Virol. 57:298-307. [DOI] [PubMed] [Google Scholar]
- 21.Madalosso, C., N. F. de Souza, D. M. Ilstrup, R. H. Wiesner, and R. A. Krom. 1998. Cytomegalovirus and its association with hepatic artery thrombosis after liver transplantation. Transplantation 66:294-297. [DOI] [PubMed] [Google Scholar]
- 22.McDonald, K., T. S. Rector, E. A. Braulin, S. H. Kubo, and M. T. Olivari. 1989. Association of coronary artery disease in cardiac transplant recipients with cytomegalovirus infection. Am. J. Cardiol. 64:359-362. [DOI] [PubMed] [Google Scholar]
- 23.Melnick, J. I., E. Adam, and M. E. DeBakey. 1995. Cytomegalovirus and atherosclerosis. Bioessays 17:899-903. [DOI] [PubMed] [Google Scholar]
- 24.Nicholson, A. C., and D. P. Hajjar. 1999. Herpesviruses and thrombosis: activation of coagulation on the endothelium. Clin. Chim. Acta 286:23-29. [DOI] [PubMed] [Google Scholar]
- 25.Nicklin, S. A., P. N. Reynolds, M. J. Brosnan, S. J. White, D. T. Curiel, A. F. Dominiczak, and A. H. Baker. 2001. Analysis of cell-specific promoters for viral gene therapy targeted at the vascular endothelium. Hypertension 38:65-70. [DOI] [PubMed] [Google Scholar]
- 26.Ofotokun, I., C. Carlson, S. D. Gitlin, G. Elta, T. P. Singleton, and D. M. Markovitz. 2001. Acute cytomegalovirus infection complicated by vascular thrombosis: a case report. Clin. Infect. Dis. 32:983-986. [DOI] [PubMed] [Google Scholar]
- 27.Pastacaldi, S., R. Teixeira, P. Montalto, K. Rolles, and A. K. Burroughs. 2001. Hepatic artery thrombosis after orthotopic liver transplantation: a review of nonsurgical causes. Liver Transpl. 7:75-81. [DOI] [PubMed] [Google Scholar]
- 28.Sedmark, D. D., D. A. Knight, N. C. Vook, and J. W. Waldman. 1994. Divergent patterns of ELAM, ICAM, and VCAM expression on cytomegalovirus infected endothelial cells. Transplantation 58:1379-1385. [PubMed] [Google Scholar]
- 29.Sinzger, C., A. Grefte, B. Plachter, A. S. Goum, T. H. The, and G. Jahn. 1995. Fibroblasts, epithelial cells, endothelial cells and smooth muscle cells are major targets of human cytomegalovirus infection in lung and gastrointestinal tissues. J. Gen. Virol. 76:741-750. [DOI] [PubMed] [Google Scholar]
- 30.Sinzger, C., K. Schmidt, J. Knapp, M. Kahl, R. Beck, J. Waldman, H. Hebart, H. Einselen, and G. Jahn. 1999. Modification of human cytomegalovirus tropism through propagation in vitro is associated with changes in the viral genome. J. Gen. Virol. 80:2867-2877. [DOI] [PubMed] [Google Scholar]
- 31.Smieja, M., J. Gnarpe, E. Lonn, H. Gnarpe, G. Olsson, Q. Yi, V. Dzavik, M. McQueen, and S. Yusuf. 2003. Multiple infection and subsequent cardiovascular events in the Heart Outcomes Prevention Evaluation (HOPE) study. Circulation 107:251-257. [DOI] [PubMed] [Google Scholar]
- 32.Smith, K. J., H. G. Skelton, and J. Yeager. 1995. Cutaneous thrombosis in human immunodeficiency virus type 1 positive patients and cytomegalovirus viremia. Arch. Dermatol. 131:357-358. [DOI] [PubMed] [Google Scholar]
- 33.Speir, E., R. Modali, E. S. Huang, M. B. Leon, L. F. Shaw, T. Finkel, and S. E. Epstein. 1994. Potential role of human cytomegalovirus and p53 interaction in coronary restenosis. Science 265:391-394. [DOI] [PubMed] [Google Scholar]
- 34.Streblow, D. N., C. Söderberg-Naucler, J. Vieira, P. Smith, E. Wakabayashi, F. Ruchti, K. Mattison, Y. Altschuler, and J. A. Nelson. 1999. The human cytomegalovirus chemokine receptor US28 mediates vascular smooth muscle cell migration. Cell 99:511-520. [DOI] [PubMed] [Google Scholar]
- 35.The, T. H., A. M. Kas-Deelen, E. F. de Maar, C. Driessen, Hamsen mC, and W. J. VanSon. 2001. Cellular and humoral parameters for vascular damage in blood during cytomegalovirus infections. Transplant. Proc. 33:1813. [DOI] [PubMed] [Google Scholar]
- 36.Van Geelen, A. G., M. E. Slobbe-van Drunen, A. D. Muller, C. A. Bruggeman, and M. C. VanDam-Mieras. 1995. Membrane related effects in endothelial cells induced by human cytomegalovirus. Arch. Virol. 140:1601-1612. [DOI] [PubMed] [Google Scholar]
- 37.Vercellottio, G. M. 1998. Effects of viral activation of the vessel wall on the inflammation and thrombosis. Blood Coagul. Fibrinolysis 9:3-6. [PubMed] [Google Scholar]
- 38.Visser, M. R., P. B. Tracy, G. M. Verecellotti, J. L. Goodman, H. C. White, and H. S. Jacob. 1988. Enhanced thrombin generation and platelet binding on herpes simplex virus-infected endothelium. Proc. Natl. Acad. Sci. USA 85:8227-8230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watt, S., B. Aesch, P. Lanotte, and F. Tranquart. 2003. Viral and bacterial DNA in carotid atherosclerotic lesions. Eur. J. Clin. Microbiol. Infect. Dis. 22:99-105. [DOI] [PubMed] [Google Scholar]
- 40.Weill, D. 2001. Role of cytomegalovirus in cardiac allograft vasculopathy. Transpl. Infect. Dis. 3(Suppl. 2):44-48. [DOI] [PubMed] [Google Scholar]
- 41.Zhou, Y. F., M. B. Leon, M. A. Waclawiw, J. J. Popma, Z. X. Yu, T. Finkel, and S. E. Epstein. 1996. Association between prior cytomegalovirus infection and the risk of restenosis after coronary atherectomy. N. Engl. J. Med. 335:624-630. [DOI] [PubMed] [Google Scholar]