Abstract
Background
Long-acting reversible contraceptives such as intrauterine devices (IUDs) are highly effective in preventing pregnancy, cost effective, and increasing in popularity. It is unclear whether changes in IUD use are associated with changes in rates of irreversible tubal sterilization. In this analysis, we evaluate changes in rates of tubal sterilization, insertion of copper or levonorgestrel (LNG) IUDs, and related complications over time.
Methods
Data were obtained from a retrospective claims database (OptumTM ClinformaticsTM Data Mart) of women aged 15 to 45 years who underwent insertion of copper or LNG IUD or tubal sterilization between 1/1/2006 and 12/31/2011. Outcomes of interest included annual rates of insertion or sterilization and annual rates of potential complications and side effects.
Results
The number of women included in the analysis each year ranged from 1,870,675 to 2,016,916. Between 2006 and 2011, copper IUD insertion claim rates increased from 0.18 to 0.25% and LNG IUD insertion claim rates increased from 0.63 to 1.15%, while sterilization claims decreased from 0.78 to 0.66% (P < 0.0001 for all comparisons). Increases in IUD insertion were apparent in all age groups; decreases in tubal sterilization occurred in women aged 20 to 34 years. The most common side effects and complications were amenorrhea (7.36–11.59%), heavy menstrual bleeding (4.85–15.69%), and pelvic pain (11.12–14.27%). Significant increases in claims of certain complications associated with IUD insertion or sterilization were also observed.
Conclusion
Between 2006 and 2011, a decrease in sterilization rates accompanied an increase in IUD insertion rates, suggesting that increasing numbers of women opted for reversible methods of long-term contraception over permanent sterilization.
Keywords: Copper IUD, Levonorgestrel IUD, Tubal sterilization
Plain English summary
Long-acting reversible contraceptives such as intrauterine devices (IUDs) are among the most effective options for preventing pregnancy, and their popularity is increasing. However, whether changes in IUD use are associated with changes in rates of tubal sterilization, a largely irreversible and permanent contraceptive option, is unclear. In this study, we evaluated changes in rates of tubal sterilization, insertion of two different types of IUDs (copper or levonorgestrel [LNG] IUDs) and side effects associated with these devices over time. Data were obtained from an insurance claims database that included women aged 15 to 45 years who underwent insertion of copper or LNG IUD insertion or tubal sterilization between 1/1/2006 and 12/31/2011. Approximately 2 million women were included in the database each year. Between 2006 and 2011, copper IUD insertion rates increased from 0.18 to 0.25% and LNG IUD insertion rates increased from 0.63 to 1.15%, while sterilization claims decreased from 0.78 to 0.66%. Increases in IUD insertion were apparent in all age groups; decreases in tubal sterilization occurred in women aged 20 to 34 years. Results from our study suggest that increasing numbers of women are opting for copper and LNG IUDs over permanent sterilization.
Background
Intrauterine devices (IUDs) are the most common method of reversible contraception [1, 2], used by approximately 14.3% of reproductive-aged women worldwide [3]. However, they are used only by 6.4% of American women using contraception [4]. Two commonly used IUDs in the US include the copper T380A IUD (copper IUD) and the levonorgestrel 20-mcg-releasing intrauterine device (LNG IUD). Both IUDs have been shown to be cost effective, have few contraindications, and are well tolerated [5–9].
Although the use of both IUDs is low in the US compared with the rest of the world, data suggest that use has substantially increased in recent years [10, 11]. Factors that may affect IUD use, including changes in rates of tubal sterilization, complications, or side effects have not been investigated.
In this report, we compare the use and complications associated with the copper IUD, LNG IUD, and tubal sterilization using data obtained from the Optum™ Clinformatics™ Data Mart database.
Methods
The Optum™ Clinformatics™ Data Mart database is a large database of medical claims, pharmacy claims, lab results, and administrative data that contains information on patient characteristics, inpatient and outpatient encounters, and outpatient prescription drug coverage throughout the US. The database includes approximately 13 million unique individuals each year. Most individuals included in the database are commercially insured. The database is fully compliant with the Health Insurance Portability and Accountability Act.
This study evaluated claims from January 1, 2006, to December 31, 2011, among women aged 15–45 years as of the index date, defined as the insertion date of copper IUD (Healthcare Common Procedure Coding System [HCPCS] code J7300) or LNG IUD (HCPCS code J7302), or date of sterilization by tubal ligation/tubal occlusion, based on receipt of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 66.2 or 66.3 or Current Procedure Terminology codes 58600, 58605, 58611, 58615, 56870, or 56871.
Outcomes of interest included the rate of copper IUD insertion, LNG IUD insertion, and tubal sterilization by year (2006–2011) and by age group (ages 15–19, 20–24, 25–34, and 35–45), and changes in rate of potential complications and side effects over time. Complications and side effects were assessed based on receipt of ICD-9-CM codes for the following conditions: uterine perforation, pelvic inflammatory disease, post-insertion infection, dysmenorrhea, heavy menstrual bleeding (HMB), menorrhagia, anemia, ovarian cyst, pelvic pain, and amenorrhea.
All analyses were conducted using SAS®, version 9.3 (SAS Institute Inc., Cary, NC, USA). Chi square analyses were used to analyze categorical variables; analyses of variance were used to evaluate continuous variables. Findings with associated P values <0.05 were considered statistically significant.
Results
The number of women included in the analysis each year ranged from 1,870,675 to 2,016,916. Rates of tubal sterilization decreased and rates of insertion of both copper and LNG IUDs increased between 2006 and 2011 (Table 1, Fig. 1). The percentage of women who underwent tubal ligation/tubal occlusion decreased from 0.78% (14,887/1,907,748) in 2006 to 0.66% (12,560/1,909,316) in 2011 (P < 0.0001), while rates of copper IUD insertion increased from 0.18% (3,454/1,907,748) to 0.25% (4,682/1,909,316) (P < 0.0001) and rates of LNG IUD insertion increased from 0.63% (12,028/1,907,748) to 1.15% (22,035/1,909,316) (P < 0.0001) from 2006 to 2011, respectively.
Table 1.
Rate of IUD insertion and tubal sterilization over time
| Copper IUD | LNG IUD | Tubal Sterilization | ||
|---|---|---|---|---|
| Year | Total N | n (%) | n (%) | n (%) |
| 2006 | 1,907,748 | 3454 (0.18) | 12,028 (0.63) | 14,887 (0.78) |
| Age 15 to 19 y | 293,354 | 52 (0.02) | 216 (0.07) | 38 (0.01) |
| Age 20 to 24 y | 220,950 | 330 (0.15) | 1257 (0.57) | 451 (0.20) |
| Age 25 to 34 y | 566,152 | 1735 (0.31) | 6230 (1.10) | 6642 (1.17) |
| Age 35 to 45 y | 827,292 | 1337 (0.16) | 4325 (0.52) | 7756 (0.94) |
| 2007 | 1,940,301 | 3803 (0.20) | 16,789 (0.87) | 14,769 (0.76) |
| Age 15 to 19 y | 299,599 | 79 (0.03) | 416 (0.14) | 42 (0.01) |
| Age 20 to 24 y | 224,324 | 403 (0.18) | 1813 (0.81) | 444 (0.20) |
| Age 25 to 34 y | 583,955 | 1964 (0.34) | 8533 (1.46) | 6471 (1.11) |
| Age 35 to 45 y | 832,423 | 1357 (0.16) | 6027 (0.72) | 7812 (0.94) |
| 2008 | 2,001,739 | 4474 (0.22) | 24,276 (1.21) | 14,667 (0.73) |
| Age 15 to 19 y | 308,311 | 102 (0.03) | 690 (0.22) | 21 (0.01) |
| Age 20 to 24 y | 237,192 | 455 (0.19) | 2845 (1.2) | 410 (0.17) |
| Age 25 to 34 y | 615,537 | 2368 (0.38) | 12,545 (2.04) | 6473 (1.05) |
| Age 35 to 45 y | 840,699 | 1549 (0.18) | 8196 (0.97) | 7763 (0.92) |
| 2009 | 2,016,916 | 4868 (0.24) | 24,811 (1.23) | 14,881 (0.74) |
| Age 15 to 19 y | 312,431 | 93 (0.03) | 777 (0.25) | 37 (0.01) |
| Age 20 to 24 y | 237,723 | 460 (0.19) | 2920 (1.23) | 394 (0.17) |
| Age 25 to 34 y | 625,323 | 2578 (0.41) | 12,614 (2.02) | 6232 (1.00) |
| Age 35 to 45 y | 841,439 | 1737 (0.21) | 8500 (1.01) | 8218 (0.98) |
| 2010 | 1,870,675 | 5246 (0.28) | 20,639 (1.10) | 13,313 (0.71) |
| Age 15 to 19 y | 289,736 | 142 (0.05) | 677 (0.23) | 37 (0.010 |
| Age 20 to 24 y | 222,812 | 551 (0.25) | 2101 (0.94) | 243 (0.11) |
| Age 25 to 34 y | 574,702 | 2782 (0.48) | 10,316 (1.8) | 5485 (0.95) |
| Age 35 to 45 y | 783,425 | 1771 (0.23) | 7545 (0.96) | 7548 (0.96) |
| 2011 | 1,909,316 | 4682 (0.25) | 22,035 (1.15) | 12,560 (0.66) |
| Age 15 to 19 y | 295,377 | 116 (0.04) | 762 (0.26) | 24 (0.01) |
| Age 20 to 24 y | 265,891 | 601 (0.23) | 2648 (1.00) | 280 (0.11) |
| Age 25 to 34 y | 575,729 | 2451 (0.43) | 10,694 (1.86) | 5102 (0.89) |
| Age 35 to 45 y | 772,319 | 1514 (0.20) | 7931 (1.03) | 7154 (0.93) |
| P Value for Trend Over Time in the Overall Population | <0.0001 | <0.0001 | <0.0001 |
Fig. 1.
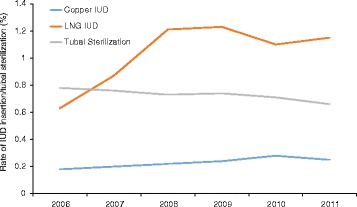
Rate of claims related to copper IUD insertion, LNG IUD insertion, and tubal sterilization by year of insertion/sterilization
Increases in IUD insertion and decreases in tubal sterilization rates were apparent in most age groups (Table 1, Fig. 2). The greatest decreases in rates of sterilization occurred in women ages 25–34. Although insertion of either IUD in adolescents ages 15–19 was rare, the copper IUD insertion rate doubled and the LNG IUD insertion rate more than tripled in this age group between 2006 and 2011.
Fig. 2.
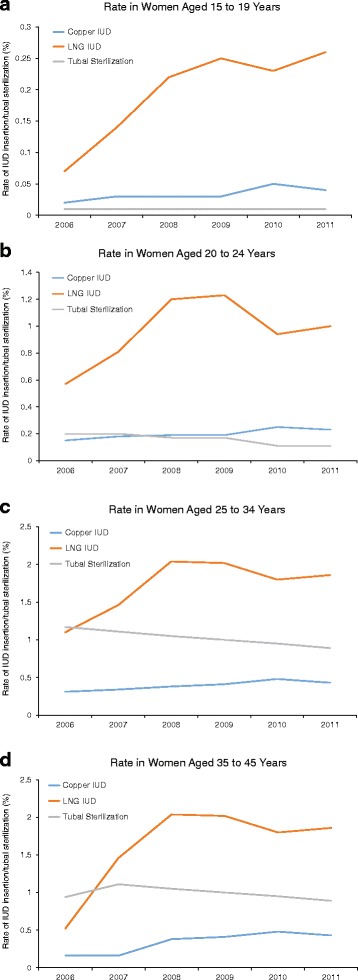
Rate of claims related to copper IUD insertion, LNG IUD insertion, and tubal sterilization by year of insertion or sterilization in women aged 15 to 19 years (a), 20 to 24 years (b), 25 to 34 years (c), and 35 to 45 years (d)
Rates of complications or side effects were low and are shown in Table 2. The most common side effects and complications were amenorrhea (7.36–11.59%), HMB (4.85–15.69%), and pelvic pain (11.12–14.27%). Significant increases over time were observed in rates of perforation of the uterine wall in all groups, HMB and menorrhagia with LNG IUD and tubal sterilization, dysmenorrhea and anemia with sterilization, and ovarian cysts with LNG IUD. A significant decrease in pelvic inflammatory disease was observed over time among women who underwent sterilization.
Table 2.
Complications and side effects associated with IUD insertion and tubal sterilization over time
| Copper IUD | LNG IUD | Tubal Sterilization | |
|---|---|---|---|
| Complications/Side Effect | n (%) | n (%) | n (%) |
| Amenorrhea (ICD-9 626.0) | |||
| Total (2006–2011) | 2385 (8.99)ab | 9077 (7.53)ac | 7050 (11.67)bc |
| 2006 | 308 (8.92) | 941 (7.82) | 1638 (11.00) |
| 2007 | 381 (10.02) | 1278 (7.61) | 1614 (10.93) |
| 2008 | 412 (9.21) | 1873 (7.72) | 1700 (11.59) |
| 2009 | 448 (9.20) | 1845 (7.44) | 1658 (11.14) |
| 2010 | 452 (8.62) | 1518 (7.36) | 1429 (10.73) |
| 2011 | 384 (8.20) | 1622 (7.36) | 1371 (10.92) |
| P Value | 0.0775 | 0.4191 | 0.2768 |
| Anemia (ICD-9 280.xx) | |||
| Total (2006–2011) | 595 (2.24)b | 2832 (2.35)c | 2003 (3.32)bc |
| 2006 | 67 (1.94) | 279 (2.32) | 435 (2.92) |
| 2007 | 78 (2.05) | 386 (2.30) | 433 (2.93) |
| 2008 | 106 (2.37) | 538 (2.22) | 492 (3.35) |
| 2009 | 119 (2.44) | 600 (2.42) | 513 (3.45) |
| 2010 | 135 (2.57) | 512 (2.48) | 481 (3.61) |
| 2011 | 90 (1.92) | 517 (2.35) | 469 (3.73) |
| P Value | 0.1496 | 0.5243 | 0.0001 |
| Dysmenorrhea (ICD-9 625.3) | |||
| Total (2006–2011) | 733 (2.76)ab | 3909 (3.24)ac | 2491 (4.12)bc |
| 2006 | 90 (2.61) | 378 (3.14) | 587 (3.94) |
| 2007 | 85 (2.50) | 566 (3.37) | 591 (4.00) |
| 2008 | 132 (2.95) | 723 (2.98) | 598 (4.08) |
| 2009 | 139 (2.86) | 807 (3.25) | 647 (4.35) |
| 2010 | 137 (2.61) | 692 (3.35) | 649 (4.87) |
| 2011 | 140 (2.99) | 743 (3.37) | 606 (4.82) |
| P Value | 0.6388 | 0.1234 | <0.0001 |
| Heavy Menstrual Bleeding (ICD-9 626.2) | |||
| Total (2006–2011) | 1370 (5.16)ab | 10 204 (8.46)ac | 7328 (12.13)bc |
| 2006 | 204 (5.91) | 1048 (8.71) | 1687 (11.33) |
| 2007 | 198 (5.21) | 1406 (8.37) | 1750 (11.85) |
| 2008 | 224 (5.01) | 1846 (7.60) | 1922 (13.10) |
| 2009 | 256 (5.26) | 1992 (8.03) | 2045 (13.74) |
| 2010 | 261 (4.98) | 1881 (9.11) | 2006 (15.07) |
| 2011 | 227 (4.85) | 2031 (9.22) | 1971 (15.69) |
| P Value | 0.3527 | <0.0001 | <0.0001 |
| Infection (ICD-9 998.5x) | |||
| Total (2006–2011) | 15 (0.06) | 88 (0.07)c | 18 (0.03)c |
| 2006 | 4 (0.12) | 12 (0.10) | 2 (0.01) |
| 2007 | 1(0.03) | 14 (0.08) | 2 (0.01) |
| 2008 | 6 (0.13) | 15 (0.06) | 7 (0.05) |
| 2009 | 2 (0.04) | 25 (0.10) | 4 (0.03) |
| 2010 | 0 (0.00) | 14 (0.07) | 4 (0.03) |
| 2011 | 2 (0.04) | 8 (0.04) | 5 (0.04) |
| P Value | 0.0543 | 0.1255 | 0.4301 |
| Menorrhagia (ICD-9 627.0) | |||
| Total (2006–2011) | 53 (0.20)ab | 528 (0.44)ac | 410 (0.68)bc |
| 2006 | 12 (0.35) | 48 (0.40) | 88 (0.59) |
| 2007 | 6 (0.16) | 58 (0.35) | 94 (0.64) |
| 2008 | 11 (0.25) | 84 (0.35) | 92 (0.63) |
| 2009 | 12 (0.25) | 89 (0.36) | 119 (0.80) |
| 2010 | 8 (0.15) | 121 (0.59) | 121 (0.91) |
| 2011 | 4 (0.09) | 128 (0.58) | 126 (1.00) |
| P Value | 0.1181 | <0.0001 | <0.0001 |
| Ovarian Cyst (ICD-9 620.2) | |||
| Total (2006–2011) | 1157 (4.36)ab | 6340 (5.26)ac | 4324 (7.16)bc |
| 2006 | 140 (4.05) | 539 (4.48) | 1045 (7.02) |
| 2007 | 155 (4.08) | 786 (4.68) | 990 (6.70) |
| 2008 | 211 (4.72) | 1268 (5.22) | 1076 (7.34) |
| 2009 | 209 (4.29) | 1400 (5.64) | 1039 (6.98) |
| 2010 | 223 (4.25) | 1142 (5.53) | 1003 (7.53) |
| 2011 | 219 (4.68) | 1205 (5.47) | 910 (7.25) |
| P Value | 0.5197 | <0.0001 | 0.0975 |
| Pelvic Inflammatory Disease (ICD-9 614.xx–616.xx) | |||
| Total (2006–2011) | 5053 (19.05)ab | 19 063 (15.81)ac | 11 162 (18.48)bc |
| 2006 | 13 (0.38) | 40 (0.33) | 64 (0.43) |
| 2007 | 12 (0.32) | 53 (0.32) | 66 (0.45) |
| 2008 | 23 (0.51) | 74 (0.30) | 69 (0.47) |
| 2009 | 15 (0.31) | 60 (0.24) | 54 (0.37) |
| 2010 | 12 (0.23) | 49 (0.24) | 41 (0.31) |
| 2011 | 18 (0.38) | 58 (0.26) | 25 (0.20) |
| P Value | 0.282 | 0.3727 | 0.02 |
| Pelvic Pain (ICD-9 625.9, 789.00) | |||
| Total (2006–2011) | 3222 (12.15)ab | 13 891 (11.52)ac | 8323 (13.78)bc |
| 2006 | 384 (11.12) | 1395 (11.60) | 1987 (13.35) |
| 2007 | 466 (12.25) | 1915 (11.41) | 1997 (13.52) |
| 2008 | 519 (11.60) | 2729 (11.24) | 1976 (13.47) |
| 2009 | 627 (12.88) | 2897 (11.68) | 2117 (14.23) |
| 2010 | 661 (12.60) | 2419 (11.72) | 1881 (14.13) |
| 2011 | 565 (12.07) | 2536 (11.51) | 1792 (14.27) |
| P Value | 0.1449 | 0.617 | 0.0593 |
| Perforation of Uterine Wall (ICD-9 621.8, 665.3) | |||
| Total (2006–2011) | 412 (1.55)ab | 1558 (1.29)ac | 387 (0.64)bc |
| 2006 | 40 (1.16) | 142 (1.18) | 57 (0.38) |
| 2007 | 51 (1.34) | 176 (1.05) | 76 (0.51) |
| 2008 | 48 (1.07) | 301 (1.24) | 91 (0.62) |
| 2009 | 88 (1.81) | 319 (1.29) | 119 (0.80) |
| 2010 | 98 (1.87) | 307 (1.49) | 103 (0.77) |
| 2011 | 87 (1.86) | 313 (1.42) | 109 (0.87) |
| P Value | 0.0014 | 0.0023 | <0.0001 |
abcChi square pairwise comparisons between groups with the same superscript, P < 0.05. The pairwise comparisons were done for the total for each complication/side effect across years 2006–2011 and not for the individual years
Discussion
Results indicate that tubal sterilization rates decreased and IUD insertion rates increased between 2006 and 2011. These findings were noted across all age groups, with the exception of sterilization in women ages 35–45, the rates of which were constant. By 2008, insertion rates of LNG IUD exceeded rates of sterilization in every age group, including women ages 35–45. Importantly, substantial increases in insertion rates for both the copper and LNG IUDs were seen in younger women, including adolescents.
Results suggesting an increase in IUD use are consistent with data from the National Survey of Family Growth, which showed that from 2002 to 2013, the prevalence of IUD use increased from 2.0 to 10.3% among female contraceptive users aged 15–44 years [12]. The prevalence of female sterilization in the same population decreased from 27.0 to 25.1% over the same time period. In a separate analysis of sexually active women aged 15–24 years, IUD use increased from 0.2 to 2.5% in teens ages 15–19 and from 2.0 to 5.4% in women aged 20–24 years, although the increase was primarily observed in parous women [11]. Another retrospective cohort study found that IUD insertion rates increased nearly 7-fold between 2002 and 2009 [6].
Importantly, women experienced few complications with either IUD. Differences in complication rates between IUDs were of minimal clinical significance. The most frequent complications in both IUD groups were menstrual disorders and pelvic pain; however, patients who underwent tubal sterilization reported these adverse effects more frequently than IUD users. The most serious complications associated with IUD use, such as uterine perforation and pelvic inflammatory disease, were reported in fewer than 2% of women.
Limitations of the study included its observational, retrospective nature, lack of representation of women without health insurance, and nature of claims databases. Despite these limitations, our findings confirm recent data suggesting a shift toward long-acting reversible contraceptive methods and away from permanent methods. Copper IUD and LNG IUD insertion and tubal sterilization were associated with a low rate of complications.
Conclusions
Our analysis of a retrospective claims database supported an increase in women selecting reversible methods of long-term contraception over permanent tubal sterilization, as shown by an increase in copper IUD and LNG IUD insertion rates and decreased sterilization rates between 2006 and 2011. Younger women showed substantial increases in IUD insertion rates. Among all women, rates of complications or side effects were low.
Acknowledgement
The authors thank Nicole Cooper of MedVal Scientific Information Services, LLC, for providing medical writing and editorial assistance. This manuscript was prepared according to the International Society for Medical Publication Professionals’ ‘Good Publication Practice for Communicating Company-Sponsored Medical Research: the GPP2 Guidelines’ and the International Committee of Medical Journal Editors’ ‘Uniform Requirements for Manuscripts Submitted to Biomedical Journals.’
Funding
This analysis was sponsored by Teva Branded Pharmaceutical Products R&D, Inc. Medical writing assistance was provided by MedVal Scientific Information Services, LLC (Skillman, NJ), and was funded by Teva Branded Pharmaceutical Products R&D, Inc. (Frazer, PA). Teva provided a full review of the article.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available in the Optum™ Clinformatics™ Data Mart database.
Authors’ contributions
Study concept and design: BH, EG, ML, BT. Acquisition, analysis, or interpretation of data: All authors. Drafting of manuscript: All authors. Critical revisions of manuscript for important intellectual content: All authors. Statistical analysis: ML. Final approval of manuscript: All authors.
Competing interests
Brandon Howard was an employee of Teva Global Medical Affairs at the time this work was conducted; ElizaBeth Grubb was an employee of Teva Global Health Economics & Outcomes Research at the time this work was conducted; Maureen J. Lage is the managing member of HealthMetrics Outcomes Research and was compensated by Teva Branded Pharmaceutical Products, R&D, Inc. for her work on this project. Boxiong Tang is an employee of Teva Global Health Economics & Outcomes Research.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- HCPCS
Healthcare Common Procedure Coding System
- HMB
Heavy menstrual bleeding
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- IUD
Intrauterine device
- LNG
Levonorgestrel
Contributor Information
Brandon Howard, Email: Brandihoward@gmail.com.
ElizaBeth Grubb, Email: beth.grubb@gmail.com.
Maureen J. Lage, Email: lagemj@hlthmetrics.com
Boxiong Tang, Email: Boxoing.Tang@tevapharm.com.
References
- 1.D’Arcangues C. Worldwide use of intrauterine devices for contraception. Contraception. 2007;75(6 suppl):S2–S7. doi: 10.1016/j.contraception.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 2.Kaneshiro B, Aeby T. Long-term safety, efficacy, and patient acceptability of the intrauterine copper T-380A contraceptive device. Int J Women’s Health. 2010;2:211–220. doi: 10.2147/IJWH.S6914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buhling KJ, Zite NB, Lotke P, Black K. Worldwide use of intrauterine contraception: a review. Contraception. 2014;89:162–73. doi: 10.1016/j.contraception.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Branum A, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS Data Brief. 2015;188:1–8. [PubMed] [Google Scholar]
- 5.National Center for Chronic Disease Prevention and Health Promotion U.S. selected practice recommendations for contraceptive use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition. Morb Mortal Wkly Rep. 2013;62:1–46. [PubMed] [Google Scholar]
- 6.Berenson AB, Tan A, Hirth JM, Wilkinson GS. Complications and continuation of intrauterine device use among commercially insured teenagers. Obstet Gynecol. 2013;121:951–8. doi: 10.1097/AOG.0b013e31828b63a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foster DG, Rostovtseva DP, Brindis CD, Biggs MA, Hulett D, Darney PD. Cost savings from the provision of specific methods of contraception in a publicly funded program. Am J Public Health. 2009;99:446–51. doi: 10.2105/AJPH.2007.129353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87:154–61. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trussell J, Hassan F, Lowin J, Law A, Filonenko A. Achieving cost-neutrality with long-acting reversible contraceptive methods. Contraception. 2015;91:49–56. doi: 10.1016/j.contraception.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu X, Macaluso M, Ouyang L, Kulczycki A, Grosse SD. Revival of the intrauterine device: increased insertions among US women with employer-sponsored insurance, 2002–2008. Contraception. 2012;85:155–9. doi: 10.1016/j.contraception.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Whitaker AK, Sisco KM, Tomlinson AN, Dude AM, Martins SL. Use of the intrauterine device among adolescent and young adult women in the United States from 2002 to 2010. J Adolesc Health. 2013;53:401–6. doi: 10.1016/j.jadohealth.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Daniels K, Daugherty J, Jones J, Mosher W. Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011–2013. Natl Health Stat Report. 2015;86:1–14. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available in the Optum™ Clinformatics™ Data Mart database.


