Abstract
Objective
Adolescents in alternative schools for behavioral and emotional problems have an earlier sexual onset and higher rates of sexual risk than their peers. They also often have difficulty managing strong emotions, which can impair sexual decision-making. Human immunodeficiency virus (HIV) prevention programs for these adolescents may be most effective if skills for coping with strong emotions during sexual situations are included.
Method
This paper reports the 6-month outcomes of a three-arm randomized controlled trial comparing an HIV prevention intervention with affect management (AM) to a standard, skills-based HIV prevention intervention (SB), and a general health promotion intervention (HP). HP was similar to a general health class, and SB was based on previous effective HIV prevention programs used with community adolescents, while AM included affect management skills in addition to effective HIV prevention skills. Youth (n=377) in two US cities were ages 13 to 19 and attending alternative schools for behavioral and emotional problems.
Results
Multiple logistic regression analyses, adjusted for the baseline scores, age, and gender, found adolescents in AM were significantly less likely to report being sexually active at follow-up (80% vs. 91%, adjusted odds ratio [AOR] =0.28, CI=0.08–0.96) and more consistently using condoms than those in HP at follow-up (62%, vs. 39%, AOR=3.42, CI=1.10–10.63).
Conclusion
Affect management techniques tested in this project, focused on sexual situations, are similar to those that are used in dialectical behavioral therapy (DBT) and in clinical practice. These data suggest that these techniques might decrease risk behaviors and improve the health of adolescents with emotional/behavioral problems.
Keywords: adolescents, alternative schools, HIV, affect management
INTRODUCTION
As of 2014, adolescents between the ages of 13 to 24 accounted for nearly 20% of new HIV infections in the US.1 Adolescence is a developmental stage typically characterized by social exploration, experimentation, and increase in risky behavior such as substance use and unprotected sex.2 National data indicate that 41% of high school students report having had sexual intercourse, 43% of those have had sex without a condom, and 21% have used alcohol or drugs prior to having sex.1 Although there are no HIV seroprevalence studies conducted with alternative school students with mental health issues, HIV-risk behaviors such as unprotected sex, substance and alcohol use, and self-destructive tendencies occur at higher rates among adolescents with psychiatric disorders (especially those with bipolar and externalizing disorders), compared to those without disorders.3 Dealing with emotionally charged situations may prove to be difficult for adolescents due to incomplete development of cognitive and planning capacities.4 In addition, deficits in emotion regulation and affect management among adolescents with psychiatric disorders make navigating this stage more difficult. Adolescents who lack skills to effectively manage and express their emotions are more likely to engage in risky sexual behavior in order to cope with stressful and negative emotions.4,5
Adolescents in Alternative School Settings: Risk Behavior and Affect Dysregulation
Adolescents who are unable to successfully function in a traditional school setting attend alternative or therapeutic schools that better address their educational, behavioral, and emotional needs. Youth in alternative schools have emotional and behavioral disorders, are more likely to be sexually active, and less likely to use condoms relative to students in traditional schools.6 For example, one study found that nearly 60% of youth reported having had sex in the past six months.4 Alternative school students are also more likely to smoke cigarettes, binge drink, and use marijuana as well as other drugs in comparison to youth in regular schools.6 Affect dysregulation has been found to be highly prevalent in adolescents, many of whom have psychiatric disorders, who attend alternative schools for behavioral disorders.7 Affect dysregulation, in general, may underlie these behaviors, although specific types of dysregulation have not been studied. It could be useful for prevention to address the role emotion regulation plays in consistently enacting safe behaviors.
HIV Prevention Interventions for Adolescents in Alternative Schools
Traditional HIV prevention interventions have been effective in reducing HIV risk behaviors in several groups of adolescents (e.g. community, homeless, racial minorities),5 but there is limited research to evaluate the efficacy of traditional HIV prevention interventions in alternative or behavioral school settings. Two studies have demonstrated some significant intervention effects for safer sex behaviors among youth in alternative schools. One study used cognitive and emotional monitoring skills with standard skills-based techniques based on Social Learning Theory (SLT) to increase motivation and improve safer sexual skills for youth in alternative schools in Rhode Island.8 Adolescents in the intervention group demonstrated a significant decrease in their sexual risk index (decrease in sexual activity or an increase in consistent condom use) compared to those in the control group at three- and six-month follow-up. The second study, for youth in alternative schools in urban northern California,9 was a randomized controlled trial that compared, to the standard school curriculum, a skills-based HIV, sexually transmitted infection (STI), and pregnancy prevention intervention based on theories compatible with SLT that also had a service-learning component (e.g. volunteering at a senior center). At the six-month follow-up, adolescents in the intervention group were less likely to report having sex without a condom and were more likely to have used a condom at last sexual encounter. The current study addressed three gaps in the designs of the earlier projects. Despite the prevalence of affect dysregulation4,7 and its association with risk behavior, the additional impact of targeting affect dysregulation in sexual situations when combined with standard skills-based SLT HIV prevention interventions was not examined. Affect management skills address awareness of emotional states and distress tolerance practices such as deep breathing, distraction, and emotional expression. Neither study compared an affect management intervention to a standard HIV prevention program. In addition, the prior studies lacked an active control condition, making it difficult to determine the impact of experimental effects of time and attention. Also, the studies were conducted in only one location, limiting the generalizability of the results.
Project Balance
This project, Project Balance, used the Social Personal Framework (SPF), which is compatible with SLT, to inform the important constructs and target of the study. SPF posits that HIV risk for youth is attributed to multiple, co-occurring risk factors (e.g., mental health issues, low socioeconomic status (SES), peers who use substances or engage in delinquent behaviors, and decreased parental support).10 Project Balance was a three-arm randomized controlled trial comparing the relative efficacy of an HIV prevention intervention targeting affect management (AM), a standard HIV knowledge and skills intervention (SB), and a time- and attention-matched general health promotion intervention (HP) as previously described.4 The AM condition addressed the connection between feelings and HIV risk behavior and the interpersonal skills needed to translate personalized knowledge into behavior change. Affect management is informed by dialectical behavior therapy (DBT).6,11 In the AM condition, adolescents learned to identify and monitor their emotions. To manage feelings in sexual risk situations, youth practiced DBT techniques such as deep breathing, distraction, positive thinking, remembering support, and emotional expression. Sessions included development of a personal affect management plan (e.g. remembering advice from a friend when pressured), as well as content on personal relevance of HIV, assertiveness, and condom use similar to SB. The SB condition, based on principles of Social Learning Theory, used HIV prevention strategies shown to be effective in past research with adolescents.12 Session topics included consideration of life goals, HIV risk and triggers to risk behavior, assertiveness, and condom use. The HP condition, similar to school general health class, included topics such as nutrition, exercise, diet, sleep, smoking, drugs/alcohol, and violence. Teens in the HP also received information on HIV and sexual health. Neither SB nor HP conditions discussed regulating emotions. See Table 1 for differences between interventions examples of AM techniques.
Table 1.
Project Balance Topics and Affect Management Techniques
| Project Balance Topics by Intervention | |||
|---|---|---|---|
| Affect Management | Skills-Based | Health Promotion | |
| 1 | Introduction a | Introduction a | Introduction a |
| 2 | Feelings Check in | Personal Triggers | Marijuana |
| 3 | Assertivenessa | Assertivenessa | Cigarettes |
| 4 | Contraceptiona | Contraceptiona | Nutrition I |
| 5 | Affect Management I | Assertiveness II | Nutrition II |
| 6 | Affect Management II | Contraception II | Exercise |
| 7 | Reproduction, STDs a | Reproduction STDs a | Contraception, Abstinence |
| 8 | Personal Vulnerability a | Personal Vulnerability a | Violence |
| 9 | Life Goals, HIV Testing a | Life Goals, HIV Testing a | Sleep, Hygiene |
| 10 | Personal Affect Management Plan | Personal Risk Plan | Caffeine, Drugs |
| 11 | HIV Risk Evaluation a | HIV Risk Evaluation a | HIV Risk Evaluation a |
| 12 | Review a | Review a | Review a |
| Examples of Affect Management Techniques | |
|---|---|
| 1 | Distract yourself |
| 2 | Breathe deeply and relax |
| 3 | Allow the feeling to pass |
| 4 | Consider the options |
| 5 | Remember a plan |
| 6 | Express yourself positively |
| 7 | Apply positive thinking |
| 8 | Name people who care about you |
| 9 | Leave the situation |
Note: STDs = sexually transmitted diseases.
Italics indicates redundancy of topics between intervention conditions.
The immediate (one month posttest) intervention impacts of Project Balance have been reported.4 Adolescents in the affect management intervention (AM) were found to be more likely to use a condom at last sexual encounter and those in the AM and skills-based (SB) interventions were shown to have greater HIV knowledge compared to HP. Although immediate outcomes were positive, there were no differences in recent sexual activity, alcohol use in the past month, or affect dysregulation, perhaps because youth did not have time to practice new skills.
The current analyses aim to examine the longer-term intervention effects of Project Balance at 6 months when opportunity to use and practice skills may have occurred. It was hypothesized that adolescents in AM would demonstrate increased rates of consistent condom use, decreased rates of recent sexual activity, and decreased rates of sex while using drugs and/or alcohol compared to those in HP and that the improvements would be greater than at six months compared to those in the non-affect management interventions (SB and HP). We expected that adolescents in all groups would show less impairment over time due to their enrollment in the alternative school setting, which is tailored to meet the specific needs of adolescents with mental health issues. Finally, although the current intervention did not directly target substance use, we sought to explore the outcomes.
METHOD
Participants
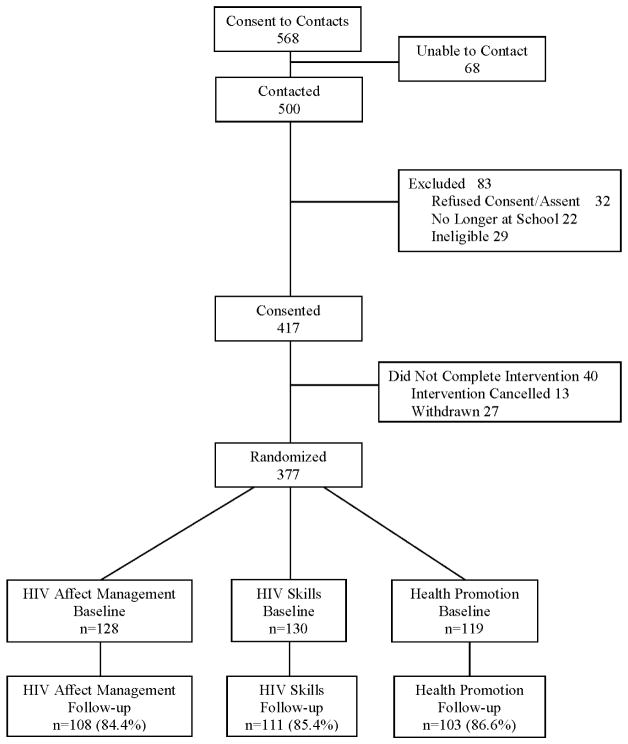
Participants were 13–19 years old from two US cities (Chicago, IL and Providence, RI) attending alternative day schools for students with emotional or behavioral problems.4 The urban and suburban schools were similar on their focus on adolescents who were unable to succeed in a traditional school environment and the use of simple behavioral reinforcement programs without more intensive treatments. To be eligible, schools needed to be able to participate for three years to permit delivery of all three interventions. Twenty schools participated in the interventions, and two schools declined because of programming concerns. Adolescents with a pervasive developmental delay or active psychotic disorder, those who were known to be HIV positive (the interventions were not designed to address disclosure of HIV and treatment), currently pregnant, and those with a history of sexual aggression assault were excluded from the study, and none of the schools had programs for those with substance use disorders. Eligibility was initially determined by staff at the alternative schools and then verified over the phone by study staff. As shown in Figure 1, of the 500 families contacted by study staff, 51 were ineligible, 32 declined participation, and 417 (81% of eligible youths) consented. Of these, 40 (10%) youth did not participate due to withdrawal from the study, leaving the school, or logistical problems preventing their attendance. Thus, 377 (90%) were allocated to one of the three intervention conditions and followed.
Figure 1.
CONSORT summary of participant enrollment retention at 6-month follow-up
Procedures
The institutional review board at both locations approved protocols. Informed consent was obtained from participants 18 years old or older and from parents or guardians of minors 13–17 years of age. Minor participants provided written assent. School staff obtained permission from eligible families to provide contact information to study staff, and face-to-face meetings were scheduled to obtain written consent and assent.
Youth completed baseline and follow-up assessments using audio computer-assisted self-interviews (ACASI). This report focuses on the assessments conducted at the six-month follow-up. Baseline and six-month follow-up assessments took about 75 minutes and 30 minutes to complete, respectively. Participants were compensated for the assessments but not the intervention.
Randomization
Schools were randomized to one of three conditions: affect management HIV prevention (AM), skills-based HIV prevention (SB), or health promotion (HP). Each new academic year, schools were randomized to an intervention condition to minimize treatment contamination. Each school received all three conditions, thus controlling for potential school-related differences.
Intervention Format
All three interventions consisted of twelve 45-minute, manualized sessions conducted during the school day as previously described.4 Sessions were delivered either once or twice a week, depending on the school’s schedule, by two trained facilitators. All three conditions included didactic instruction, games, role-plays, and discussion delivered in mixed gender groups. All written materials were at a fifth-grade level using concepts suitable for young adolescents. Role-plays and discussions allowed for examples to be relevant to youth of all ages. All participants received basic HIV and sexual health information. They also identified a health risk behavior (e.g. smoking) and improvement plan.
Fidelity
All sessions were guided by a manual, and facilitators (psychology postdoctoral fellows and bachelor-level research assistants) received training annually to prevent intervention drift.4 Facilitators read the manual in detail, reviewed project goals, discussed key issues related to implementation and treatment fidelity, and delivered mock sessions to other trainees, who acted as adolescent participants. During training, study investigators observed delivery to verify competence. In addition, quality monitors observed 20% of sessions to rate facilitator competence and the completion of required activities.
Measures
Demographics
Participants reported demographic information including age, gender, race/ethnicity, grade (dichotomized 7–9th grade/10–12th grade), female caregiver in the home, reduced or free lunch status (as a proxy for socioeconomic status), and sexual orientation.
Adolescent Risk Behavior Assessment (ARBA)
The ARBA is designed to assess adolescent self-reported sex and drug use behavior13 and has been found to be reliable and reflects the impact of interventions.7,8,14 Skip patterns minimize follow-up questions for non-endorsed behaviors. All sexual activity questions below include any vaginal, anal, or oral sexual activity. Adolescents reported on occurrence of any vaginal, anal, or oral sexual activity in the past six months (yes/no), sex while using alcohol or other drugs (yes/no), and how often they or their partner used a condom when having sex (five categories, “Always” to “Never”). Consistent condom users were defined as those reporting “Always.” Reliability for this assessment of condom use behavior and its comparability to more detailed measures have previously been demonstrated in adolescents.15 Adolescents also reported alcohol use and other drug use in the past six months (yes/no) and use of substances at time of sex (yes/no).
HIV Knowledge
HIV knowledge was assessed using 20 true/false/don’t know items about HIV and prevention.16 Scores are the number of items correct. Scale internal consistency was strong (α = .83).
Affect Dysregulation Scale (ADS)
The ADS includes six items assessing the frequency of difficulties with affect regulation.7 Participants respond on a 4-point agreement scale to items such as “In the past 3 months, my feelings got in the way of doing things.” Higher scores indicate more difficulty managing feelings, and there is reported no clinical threshold.7 Internal consistency was good (α = .72).
Condom Attitudes
Condom attitudes were assessed using a 5-point agreement scale with 20 items, such as condoms would “make sex less exciting” and “make me feel more responsible.”17 Higher scores indicate more positive condom attitudes. Internal consistency was strong (α = .85).
Columbia Impairment Scale
The Columbia Impairment Scale (CIS) is a 13-item scale measuring global impairment in interpersonal, work and school, or general functioning using a 5-point scale to rate degree of problems for items such as “getting into trouble.” Scores greater than or equal to 15 indicate clinically significant impairment.18 The CIS has good reliability, validity, and is sensitive to the impact of interventions.18
Computerized Diagnostic Interview Schedule for Children
The Computerized Diagnostic Interview Schedule for Children (C-DISC-IV) is a structured audio computer-assisted diagnostic interview that screens for DSM-IV psychiatric diagnoses and has acceptable reliability and validity.3,19,20 This study assessed generalized anxiety disorder, posttraumatic stress disorder, major depressive disorder, mania, hypomania, oppositional defiant disorder, and conduct disorder because of their prevalence in alternative schools. Other disorders were omitted due to infrequency or lack of collateral information, which can reduce screening accuracy (e.g. attention disorders).
Data Analysis
With enrollment of 420 youth and 20% attrition, power was .80 to detect medium adjusted odds ratios (2.5 or greater) between conditions at posttests (p<.05). Independent F-tests and Chi-square analyses were conducted to examine whether differences existed between conditions on baseline. Students who completed both baseline and follow-up assessments (n=322) were compared to those who completed baseline only (n=55). The intraclass correlation (ICC) for baseline continuous outcome measures ranged from .004 to .007, below the recommended cutoff of .25 used to determine the use of modeling techniques to account for group membership.21 Logistic regression analyses were conducted to assess proportional outcomes, adjusting for baseline, age, and gender (because of association with sexual/substance behaviors). Multiple logistic regression analyses were performed with the HP condition as the referent group using past six-month dichotomous outcomes: consistent condom use (“Always” vs. all others), sexual activity (Yes/No), substance use (Yes/No), and substance use at time of sex (Yes/No). Scale outcome scores were analyzed using analysis of covariance (ANCOVA), adjusting for baseline scores and relevant demographics. Per hypotheses, HIV interventions (AM+SB) were compared to HP in knowledge and Condom Attitudes, and AM was compared to non-affect condition (SB+HP) in Affect Dysregulation. Analyses for variables among those who were “recently sexually active” were restricted to those who reported sexual activity in the past six months at baseline and at 6-month postintervention. Cohen’s d was calculated to estimate intervention effect sizes. Data were analyzed using SPSS 22.0.22
RESULTS
Baseline Characteristics
Sixty-two percent of the 322 participants with 6-month data were between the ages of 13 to 15 years, with an average age of 15.1 (1.4) years (see Table 2). The sample average age was 15 years, and 71% were males. The majority (49%) identified racially as White; 31% as Black; 17% as multiracial; 3% as other categories; and 17% identified their ethnicity as Latino. The majority (71%) reported a heterosexual orientation. Approximately half of youth (53%) reported use of alcohol or other drugs in the past 6 months, although only 8% of youth used substances at least twice weekly (not shown in table). Most participants (61%) reported having had vaginal, anal, or oral sex, and 75% of those (n=135) reported having had sex in the last six months, with 51% using condoms consistently. On average, youth answered 50% of the HIV prevention questions correctly, had neutral attitudes about condoms (“neither agree nor disagree”), and reported difficulty managing feelings “a little” or “sometimes.” Approximately half of youth (58%) indicated significant impairment in functioning on the CIS, and half (55%) met threshold or subthreshold criteria for one or more psychiatric diagnoses, most commonly oppositional defiant disorder (31%), conduct disorder (26%), generalized anxiety disorder (14%), major depressive disorder (13%), and posttraumatic stress disorder (11%). Age differed between intervention groups, with those in AM being slightly older (F=3.13, p=.05). Otherwise, there were no differences in baseline attitudes and sexual behaviors. There were no significant differences on demographic variables (p>.10 for all variables) between retained (n=322, 85%) and non-retained (n=55, 15%) youth at follow-up.
Table 2.
Participant Characteristics by Intervention Condition at Baseline
| Total n=322 |
AM n=108 |
SB n=111 |
HP n= 103 |
F/χ2 | p Value | |
|---|---|---|---|---|---|---|
| Age, M(SD) | 15.1 (1.4) | 15.4 (1.5) | 15.1 (1.4) | 15.0 (1.3) | 3.13 | .05 |
| Male, n (%) | 227 (70.5) | 76 (70.4) | 76 (68.5) | 75 (72.8) | 0.49 | .78 |
| Race | 1.70 | .95 | ||||
| White, n (%) | 158 (49.1) | 53 (49.1) | 58 (52.3) | 47 (45.6) | ||
| Black, n (%) | 101 (31.4) | 34 (31.5) | 33 (29.7) | 34 (33.0) | ||
| Multiracial, n (%) | 53 (16.5) | 17 (15.7) | 18 (16.2) | 18 (17.5) | ||
| Other, n (%) | 10 (3.1) | 4 (3.7) | 2 (1.8) | 4 (3.9) | ||
| Latino, n (%) | 55 (17.1) | 16 (14.8) | 16 (14.4) | 23 (22.3) | 2.95 | .23 |
| Grade | 5.03 | .08 | ||||
| 7–9 | 139 (49.8) | 39 (41.1) | 49 (51.6) | 51 (57.3) | ||
| 10–12 | 140 (50.2) | 56 (58.9) | 46 (48.4) | 38 (42.7) | ||
| Female caregiver in home, n (%) | 282 (87.6) | 96 (88.9) | 93 (83.8) | 93 (90.3) | 2.34 | .31 |
| Free lunch eligible, n (%) | 164 (50.9) | 57 (52.8) | 52 (46.8) | 55 (53.4) | 0.40 | .82 |
| Heterosexual, n (%) | 228 (70.8) | 82 (75.9) | 82 (73.9) | 64 (62.1) | 10.16 | .25 |
| Sexually active, n (%)a,b | 113 (81.3) | 46 (85.2) | 35 (81.4) | 32 (76.2) | 1.50 | .47 |
| Alcohol or other drug use, n (%)a | 168 (52.8) | 61 (57.0) | 59 (53.6) | 48 (47.5) | 1.92 | .38 |
| Sex under influence, n (%)a,b | 75 (56.0)b | 24 (49.0) | 25 (61.0) | 26 (59.1) | 1.56 | .46 |
Note: AM = HIV affect management; HP = health promotion; SB = HIV skills based.
In past 6 months
Among those who were sexually active in past 6 months at baseline n=135.
Intervention Effects: Sex Risk Behaviors
Multiple linear regression analyses, adjusting for age, gender and baseline scores, found that adolescents in the AM condition were less likely to have been sexually active in the past six months compared to those in the HP condition (80% vs. 91%, AOR: 0.28; CI=0.08–0.96), but there was no difference between the SB and HP (86% vs. 91%, AOR: 0.57; CI=0.15–2.28; see Table 3). Youth in AM had three times the odds of consistent condom use compared to those in the HP (AOR: 3.42; CI=1.10–10.63), but SB group did not differ from HP. There were no significant differences between conditions on rates of sex while using substances.
Table 3.
Adjusted Odds Ratios (AORs) for Sex Risk Behavior Outcomes
| Pretest % | Post % | AORa | 95% CI | ||
|---|---|---|---|---|---|
| Sexually Active in Past 6 months | AM | 85.2 | 79.6 | 0.28 | 0.08–0.96 |
| SB | 81.4 | 86.0 | 0.57 | 0.15–2.28 | |
| HP | 76.2 | 90.5 | Ref | - | |
|
| |||||
| Consistent Condom Use | AM | 53.8 | 61.5 | 3.42 | 1.10–10.63 |
| SB | 42.4 | 27.3 | 0.72 | 0.22–2.32 | |
| HP | 57.1 | 39.3 | Ref | - | |
|
| |||||
| Sex at Time of Drug and/or Alcohol Use | AM | 0.57 | 0.56 | 1.01 | 0.35–2.93 |
| SB | 0.63 | 0.70 | 1.59 | 0.51–4.92 | |
| HP | 0.57 | 0.61 | Ref | - | |
Note: AM = affect management; HP = health promotion; SB = skills based.
Adjusted for baseline, age, and gender in logistic regression
Intervention Effects: Scale Scores
In ANCOVAs of the HIV-specific education interventions (AM+SB) versus HP, significant intervention effects were observed at 6-month follow-up (see Table 4). Those in the HIV interventions (AM+SB) demonstrated significant (p≤.05) improvements compared to HP in HIV knowledge (18% more correct answers, d=0.4) and condom use attitudes (“agree” with favorable attitudes, d=0.17). There was not a significant difference in change in the Affect Dysregulation Scale (ADS) scores between AM and the non-affect management conditions (SB + HP) at 6-month follow-up (data not shown, F=0.80 p=.37).
Table 4.
Scale Score Intervention Outcomes at 6-Month Follow-Up
| AM | SB | HP | F | p | ||||
|---|---|---|---|---|---|---|---|---|
| Pretest | Post | Pretest | Post | Pretest | Post | |||
| HIV Knowledge- M(SD) | 10.59 (4.43) | 12.27 (5.13) | 10.14 (4.69) | 12.13 (5.04) | 10.21 (4.25) | 11.05 (4.48) | 4.44a | .04 |
| Condom Use Attitudes- M(SD) | 72.18 (10.88) | 73.58 (12.48) | 70.25 (11.96) | 72.66 (12.40) | 70.53 (11.38) | 70.31 (12.24) | 3.86a | .05 |
| Affect Dysregulation Scale- M(SD) | 13.78 (4.46) | 12.57 (3.93) | 13.39 (4.03) | 12.71 (3.68) | 13.44 (3.93) | 12.94 (4.31) | 0.80b | .37 |
| Columbia Impairment Scale- M(SD) | 15.31 (7.70) | 13.22 (7.82) | 15.34 (7.49) | 13.59 (7.22) | 14.66 (8.13) | 12.45 (8.10) | 0.36c | .70 |
Note: AM = affect management; HP = health promotion; SB = skills-based.
Test of HIV interventions (AM +SB) vs. HP, analysis of covariance (ANCOVA) controlling for baseline, age and gender.
Test of AM vs. non-affect management interventions (SB+HP), ANCOVA controlling for baseline, age and gender.
Test for time by group interaction (AM, SB, HP), ANCOVA controlling for baseline, age and gender.
Time and School Effects
Functional impairment, as measured by the CIS, decreased over time for the entire sample (Pretest M=15.11, SD=0.43 [58% impaired]; posttest M=13.10, SD=0.43 [39% impaired]; F=6.22; p=.01), but scores did not differ significantly between intervention groups at six months (F=0.36, p=.70; see Table 3). Substance use rates also decreased over time for the entire sample (pretest 52.8%; posttest 47.5%; χ2=3.31; p=.07), but there were no differences between the groups at six-month follow-up (F=1.36, p=.51) (outcome data not shown).
DISCUSSION
The aim of this study was to examine the effects at six months of a three-arm trial (HIV prevention targeting affect management, skills-based HIV prevention, and a general health promotion intervention) for adolescents in alternative schools. Both HIV prevention conditions resulted in improved HIV knowledge and condom use attitudes; however, HIV prevention with affect management resulted in some behavioral improvement beyond that observed in the skills-based HIV prevention. It significantly reduced sexual activity and increased consistent condom use. These results suggest that providing adolescents who attend alternative schools due to severe emotional and behavioral problems with the skills to recognize and manage strong feelings in high-stress situations, especially sexual ones, can allow them to use self-protective behaviors such as remaining abstinent or using condoms. A reduction in sexual activity limits the opportunities for HIV/STI risk behaviors (e.g. inconsistent or lack of condom use, sex while using drugs or alcohol, etc.). The odds of consistently using condoms at six months were more than three times greater in AM, compared to those in the HP condition. Maintaining consistent condom use for adolescents over time has been a challenge. Affect management techniques used in this intervention are analogous to common therapeutic practices such as distress tolerance and mindfulness, which commonly focus on non-sexual situations. This study illustrates that use of these techniques can be effective when addressing sexual situations and may help guide clinicians and teachers in many clinical or educational settings. These findings suggest that skills-based HIV prevention education alone may not be enough to reduce sexual activity or sustain consistent condom use, especially for youth in alternative schools.
The HIV prevention interventions, whether they included affect management or not, resulted in improved HIV knowledge and condom use attitudes at six months. This finding indicates that the gains observed at one month, in a previous paper, were maintained.4 Although condom use attitudes improved for the skills-based group, there was not comparable improvement in condom use. These findings suggest that the inclusion of affect management education into a traditional skills-based HIV prevention intervention (without adding more intervention time) does not change or take away from the intervention effects on HIV knowledge or condom use attitudes.
Functional impairment was expected to decrease over time for all adolescents because of their enrollment in a conducive learning environment and exposure to behavioral programs operating in the school (e.g. token rewards). Also, some youth were likely receiving individual therapy outside of the school, which may have resulted in reductions in impairment and in substance use. Three reviews indicate that substance use is often targeted in alternative schools even if they do not enroll youth with substance use disorders, and solely reducing substance use may not reduce HIV risk behaviors.23–26 Substance use at time of sex, however, can increase the risk of unprotected sex, but there were no differences between interventions. It is possible that a greater emphasis on substance use and additional skills to reduce substance use in sexual situations was needed. Both impairment and substance use are important factors in the reduction of HIV-risk behaviors among adolescents and need to be further considered.
Despite the strengths of this multisite randomized controlled trial, there are limitations. The outcomes assessed in this study are self-reported and, therefore, susceptible to bias. The use of an audio-assisted computer interview may have reduced this effect; however, there is no method to completely remove this bias. Presumably report biases associated with the safer sex focus of two conditions (AM and SB) would have been similar, but AM outperformed SB in improving safer sex. Over the course of the study, each school received all three conditions, as an attempt to control for any school-related differences. However, the interaction of unique school variables (such as weekly or biweekly frequency of intervention or additional school programs) with the different project interventions cannot be determined by these data. In addition, the sample is too small to examine the moderating role of gender, substance use, or specific psychiatric diagnoses on intervention outcomes. Our previous paper found that affect dysregulation was associated with conduct, hyperactivity, emotional, and peer problems as measured by the Strengths and Difficulties Questionnaire.7 Despite the recruitment of a large and diverse sample, these results may not be generalizable to all adolescents who attend alternative schools, all adolescents with psychiatric disorders, or all adolescents in mental health treatment.
This study adds valuable information about the use of affect management education in conjunction with a traditional skills-based HIV prevention. Results from this study suggest the need to continue exploring the role of including affect management and other therapeutic skills in HIV prevention. This appears to be a promising strategy to improve and sustain HIV prevention practices among adolescents.
Clinical Guidance.
Adolescents with mental health issues have difficulty managing strong emotions.
Impairments in affect management relate to impulsive decision making and risky sexual behavior.
Affect management techniques used in this intervention are similar to those that are commonly used in clinical practice.
Targeting affect management processes (coping with strong emotions and modulating reactions) may enhance clinical and research interventions to reduce sexual risk, HIV, and STIs for adolescents with psychiatric disorders.
Acknowledgments
This research was supported by National Institute of Mental Health grant R01 MH066641to Rhode Island Hospital and University of Illinois at Chicago, and by the Lifespan/Brown/Tufts Center for AIDS Research (P30 AI042853). The funding organizations are public institutions and had no role in the conduct and design of the study; the collection, analysis and interpretation of data; preparation or approval of the report; or the decision to submit the article for publication. The views expressed herein are those of the authors and not necessarily those of the National Institutes of Health, Rhode Island Hospital, or the University of Illinois at Chicago.
Footnotes
Clinical guidance registration information—Therapeutic Schools: Affect Management and HIV Prevention; http://clinicaltrials.gov/; NCT00500487.
Ms. Beausoleil served as the statistical expert for this research.
Disclosure: Drs. Brown, Whiteley, Houck, Donenberg and Mss. Craker, Lowery, Beausoleil report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Larry K. Brown, Rhode Island Hospital in Providence, RI. Warren Alpert Medical School, Brown University, Providence.
Dr. Laura Whiteley, Rhode Island Hospital in Providence, RI. Warren Alpert Medical School, Brown University, Providence.
Dr. Christopher D. Houck, Rhode Island Hospital in Providence, RI. Warren Alpert Medical School, Brown University, Providence.
Ms. Lacey K. Craker, Rhode Island Hospital in Providence, RI.
Ms. Ashley Lowery, Rhode Island Hospital in Providence, RI.
Ms. Nancy Beausoleil, Rhode Island Hospital in Providence, RI.
Dr. Geri Donenberg, College of Medicine at the University of Illinois-Chicago.
References
- 1.CDC. HIV Surveillance Report. 2014;26 http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2015. [Google Scholar]
- 2.Romer D. Adolescent Risk Taking, Impulsivity, and Brain Development: Implications for Prevention. Dev Psychobiol. 2010;52:263–276. doi: 10.1002/dev.20442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown LK, Hadley W, Stewart A, et al. Psychiatric Disorders and Sexual Risk among Adolescents in Mental Health Treatment. J Consult Clin Psychol. 2010;78:590–597. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown LK, Houck C, Donenberg G, Emerson E, Donahue K, Misbin J. Affect management for HIV prevention with adolescents in therapeutic schools: the immediate impact of Project Balance. AIDS Behav. 2013;17:2773–80. doi: 10.1007/s10461-013-0599-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coyle KK, Glassman JR, Franks HM, Campe S, Denner J, Lepore G. Interventions to reduce sexual risk behaviors among youth in alternative schools: A randomized controlled trial. J Adolesc Health. 2013;53:68–78. doi: 10.1016/j.jadohealth.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grunbaum JA, Lowry R, Kann L. Prevalence of health-related behaviors among alternative high school students as compared with students attending regular high schools. J Adolesc Health. 2001;29:337–343. doi: 10.1016/s1054-139x(01)00304-4. [DOI] [PubMed] [Google Scholar]
- 7.Brown LK, Houck C, Lescano C, Donenberg G, Tolou-Shams M, Mello J. Affect regulation and HIV risk among youth in therapeutic schools. AIDS Behav. 2012;16:2272–8. doi: 10.1007/s10461-012-0220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown LK, Nugent NR, Houck CD, et al. Safe Thinking and Affect Regulation (STAR): HIV prevention in alternative/therapeutic schools. J Am Acad Child Adolesc Psychiatry. 2011;50:1065–74. doi: 10.1016/j.jaac.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coyle KK, Kirby DB, Robin LE, Banspach SW, Baumler E, Glassman JR. ALL4YOU! A Randomized Trial of an HIV, Other STDs, and Pregnancy Prevention Intervention for Alternative School Students. AIDS Education and Prevention. 2006;18:187–203. doi: 10.1521/aeap.2006.18.3.187. [DOI] [PubMed] [Google Scholar]
- 10.Donenberg GR, Pao M. Youths and HIV/AIDS: Psychiatry’s Role in a Changing Epidemic. J Am Acad Child Adolesc Psychiatry. 2005;44:728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller AL, Rathus JH, Linehan MM. Dialectical Behavior Therapy with Suicidal Adolescents. New York: Guilford Press; 2007. [Google Scholar]
- 12.Pedlow T, Carey M. Developmentally appropriate sexual risk reduction interventions for adolescents: Rationale, review of interventions, and recommendations for research and practice. Ann Behav Med. 2004;27:172–184. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-Risk Behavior Among Adolescents in Psychiatric Care: Links to Psychopathology and Peer Relationships. J Am Acad Child Adolesc Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown LK, Hadley W, Donenberg GR, et al. Project STYLE: a multisite RCT for HIV prevention among youths in mental health treatment. Psychiatr Serv. 2014;65:338–344. doi: 10.1176/appi.ps.201300095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Houck C, Stewart A, Brown LK, Group PSS. Condom use measurement in adolescent HIV prevention research: Is briefer better? Int Public Health J. 2012;4:369–376. [Google Scholar]
- 16.Brown LK, Fritz GK. Children’s knowledge and attitudes about AIDS. J Am Acad Child Adolesc Psychiatry. 1988;27:504–508. doi: 10.1097/00004583-198807000-00022. [DOI] [PubMed] [Google Scholar]
- 17.Brown LK, Schultz JR, Parsons JT, et al. Sexual behavior change among human immunodeficiency virus-infected adolescents with hemophilia. Adolescent Hemophilia Behavioral Intervention Evaluation Project Study Group. Pediatrics. 2000;106:E22. doi: 10.1542/peds.106.2.e22. [DOI] [PubMed] [Google Scholar]
- 18.Bird HR, Shaffer D, Fisher P, et al. The Columbia Impairment Scale (CIS): Pilot findings on a measure of global impairment for children and adolescents. Int J Methods in Psychiatr Res. 1993;3:167–176. [Google Scholar]
- 19.Fisher P, Lucas C, Shaffer D, Schwab-Stone M, Graae F, Lichtman J. Diagnostic Interview Schedule for Children, Version IV (DISC IV): Test-retest reliability in a clinical sample. Paper presented at: 44th annual meeting of the American Academy of Child and Adolescent Psychiatry; Toronto. 1997. [Google Scholar]
- 20.Diagnostic Interview for Children (DISC 4.0)-Child Version [computer program] New York: Columbia University; 2000. [Google Scholar]
- 21.Guo S. Analyzing grouped data with hierarchical linear modeling. Child Youth Serv Rev. 2005;27:637–652. [Google Scholar]
- 22.Corp. I. IMB SPSS Statistics for Windows, Version 22.0. Armonk, NY: IMB Corp; 2013. [Google Scholar]
- 23.Johnson KE, Morris M, Rew L, Simonton AJ. A systematic review of consent procedures, participation rates, and main findings of health-related research in alternative high schools from 2010 to 2015. J Sch Nurs. 2016;32:20–31. doi: 10.1177/1059840515620841. [DOI] [PubMed] [Google Scholar]
- 24.Johnson KE, Taliaferro LA. Health behaviors and mental health of students attending alternative high schools: a review of the research literature. J Spec Pediatr Nurs. 2012;17:79–97. doi: 10.1111/j.1744-6155.2011.00311.x. [DOI] [PubMed] [Google Scholar]
- 25.Sussman S, Arriaza B, Grigsby TJ. Alcohol, tobacco, and other drug misuse prevention and cessation programming for alternative high school youth: a review. J Sch Health. 2014;84:748–758. doi: 10.1111/josh.12200. [DOI] [PubMed] [Google Scholar]
- 26.Ward CL, Mertens JR, Bresick GF, Little F, Weisner CM. Screening and Brief Intervention for Substance Misuse: Does It Reduce Aggression and HIV-Related Risk Behaviours? Alcohol and Alcoholism (Oxford, Oxfordshire) 2015;50:302–309. doi: 10.1093/alcalc/agv007. [DOI] [PMC free article] [PubMed] [Google Scholar]