Abstract
Background
Hypothyroidism due to non-compliance with levothyroxine therapy (pseudomalabsorption) is rare. The diagnosis is considered in patients with persistent severe hypothyroidism despite treatment with large doses of levothyroxine. Intestinal malabsorption, drug and dietary interference with levothyroxine absorption and nephrotic syndrome should be excluded. The diagnosis of pseudomalabsorption can be demonstrated by using “an oral 1,000 µg of levothyroxine test” showing a rapid decrease in thyroid-stimulating hormone and increase in thyroxine. There are however few data on the sensitivity and specificity of the test in large cohorts of hypothyroid patients. Treatment of pseudomalabsorption is controversial, with reports using parenteral, intramuscular or single weekly oral dosing of levothyroxine.
Cases
We report 3 patients who presented with persistent clinical and biochemical signs of hypothyroidism despite replacement therapy with high doses of levothyroxine. Pseudomalabsorption was diagnosed by a systematic approach, including prior exclusion of digestive, liver and kidney diseases. A peroral challenge test was positive in all cases. Patients denied non-compliance, and a psychiatric approach was elusive. Two of the patients were treated successfully with a single supervised weekly 1,000-µg administration of levothyroxine, while non-supervised weekly administration resulted in hypothyroidism confirming pseudomalabsorption.
Conclusions
Non-compliance with medical therapy should be considered in patients with treatment-refractory hypothyroidism. Supervised once weekly levothyroxine treatment is a safe and well-tolerated treatment option, obviating the need for parenteral administration of the drug. Apart from the medical treatment, there is also a need for psychiatric evaluation and care.
Key Words: Hypothyroidism, Pseudomalabsorption, Levothyroxine substitution, Levothyroxine challenge test, Psychiatric disorder
What Is Known about This Topic?
• Non-compliance with levothyroxine therapy is a frequent problem in clinical practice.
What Does This Case Report Add?
• This article provides insights into the analysis of patients with possible malabsorption of levothyroxine, specially focusing on the psychiatric problems leading to pseudomalabsorption.
Introduction
The usual treatment for hypothyroidism is supplementation with synthetic levothyroxine orally administrated aiming to achieve a normal thyroid-stimulating hormone (TSH) and free levothyroxine (fT4) level. In most cases patients are satisfactorily managed with a single dose of levothyroxine daily. The average treatment dosage of levothyroxine is 1.6 μg/kg body weight daily, ingested on an empty stomach and with the patient avoiding other medications or food for 30-60 min afterwards [1,2,3,4,5,6]. Alternatively, the dose can be administered at night [7]. In some cases however, despite large amounts of levothyroxine, hypothyroidism persists, and further examination is needed to determine its exact origin. Possible causes include gastrointestinal malabsorption, nephrotic syndrome, liver or pancreatic disease, heart disease, pregnancy or drug and dietary interactions, and last but not least pseudomalabsorption [1,6].
We report 3 cases of pseudomalabsorption, defined as non-compliance with oral levothyroxine treatment with the intention to deceive. This entity is a factitious disorder characterized by deficient diagnostic processes, patient denial and difficulties in management [1].
Case Reports
Case 1
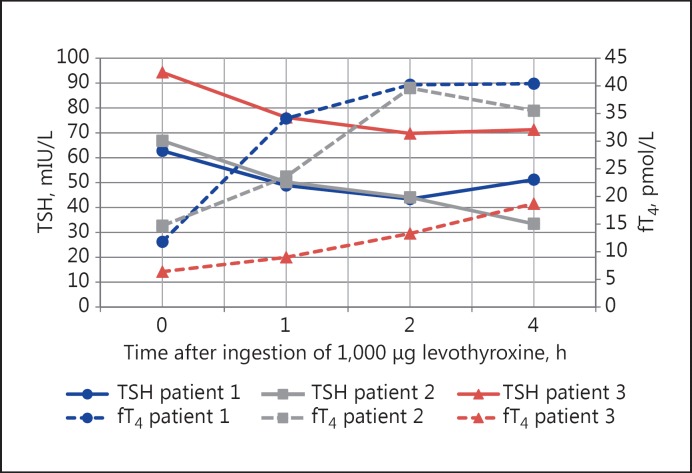
A 25-year-old woman consulted the outpatient clinic of endocrinology because of symptoms of fatigue, weight gain (17 kg in 4 months), intermittent diarrhoea and numbness in the hands. A total thyroidectomy had been performed 4 months prior to her visit for Graves' hyperthyroidism with concomitant goitre. Substitution therapy was initiated with an incremental dose of levothyroxine up to 225 μg daily. Her medical history consisted of functional endoscopic sinus surgery, tension headache and knee surgery with a postoperative Sudeck atrophy. The patient's mother also had a goitre. Other medication consisted of calcium carbonate/cholecalciferol 1,000/880 twice daily (at 15:00 and 22:00 h) and an oral contraceptive. Despite the relatively high dose of levothyroxine, she remained hypothyroid with a TSH level of 83.3 mIU/L (normal values 0.27-4.20 mIU/L) and an fT4 level of 6.2 pmol/L (normal values 12-21.9 pmol/L). The patient was hospitalized for further examination to exclude malabsorption. Physical examination showed a blood pressure of 146/95 mm Hg with a pulse rate of 74/min. The patient was slow-witted, and the physical examination was otherwise unremarkable. Following supervised daily intake of levothyroxine for 1 week, a favourable response of TSH and fT4 was noticed. Blood analysis did not reveal signs of malabsorption, i.e. no anaemia with normal ferritin, vitamin B12 and folic acid, normal albumin, increased cholesterol value, and normal levels of 25(OH) vitamin D. An urea breath test was normal, and antigliadin antibodies were absent. Gastroscopy and colonoscopy were normal. Faeces analysis for Giardia, parasites and Cryptosporidium was negative. Finally, a lactose breathing test was suggestive of lactose intolerance. The patient was discharged from the hospital with a lactose-free diet, calcium carbonate and cholecalciferol once daily taken separately from thyroid hormone. Because of the presence of lactose in most levothyroxine preparations, the treatment was changed to a lactose-free formula of levothyroxine 150 μg (Eferox®) once daily. Despite these changes the symptoms of fatigue persisted with hypothyroidism: TSH 98.2 mIU/L and fT4 of 8.1 pmol/L. A challenge test after an overnight fast with a supervised intake of 1,000 μg levothyroxine (Eferox®) revealed a correct decrease in TSH levels and increase in fT4 levels within hours following ingestion, thereby ruling out a problem of levothyroxine malabsorption (Fig. 1). Baseline values for TSH and fT4 at the beginning of the absorption test were 62.77 mIU/L and 11.8 pmol/L (normal values 12-21.9 pmol/L).
Fig. 1.
Levothyroxine absorption test.
After confrontation with the results the patient denied non-compliance. She was discharged with a dose of levothyroxine (Eferox®) 200 μg once daily. Symptoms of depression, anorexia and hair loss persisted with worsening of the test results on the same dose of levothyroxine. At this time the decision was made to administer a dose of 1,000 μg of levothyroxine orally once a week under supervision in our hospital. The patient became euthyroid. The patient is actually being treated by a psychiatrist, but continues to deny non-compliance.
Case 2
A woman with congenital hypothyroidism and substitution therapy from birth presented for the first time at our outpatient clinic at the age of 19. She described symptoms of intermittent headache, abdominal pain and a weight gain. Laboratory analysis showed a TSH level at that time of 25 mIU/L and an fT4 of 20.6 pmol/L. She admitted to have intermittently forgotten to take her medication of levothyroxine 150 μg daily. Her medical history was unremarkable, and there was no family history of thyroid problems. She had no other concomitant medication that could interfere with levothyroxine absorption or metabolism. Levothyroxine was increased to a dose of 175 μg daily with good evolution of TSH decreasing to 0.96 mIU/L and fT4 of 21.5 pmol/L. After a 1-year follow-up, evolution to severe hypothyroidism was noticed after travelling abroad. Substitution doses up to 250 μg daily were insufficient to achieve normal thyroid hormone levels as demonstrated with laboratory tests revealing serum TSH levels greater than 100 mIU/L and an fT4 level of 8.8 pmol/L. Gliadine and transglutaminase antibodies to detect coeliac disease were negative. All other laboratory tests, including haemoglobin, albumin and vitamins, were within the normal range. An urea breath test was negative for Helicobacter pylori infection. A challenge test with supervised intake of 1,000 μg of levothyroxine was performed and showed peak elevation of fT4 two hours after ingestion with a concomitant decrease in TSH (Fig. 1). Baseline values for TSH and fT4 at the beginning of the absorption test were 66.83 mIU/L and 14.7 pmol/L.
The patient was confronted with the diagnosis of non-compliance. The importance of the correct daily intake of her medication was explained. Treatment failure would call for supervised weekly administration of levothyroxine 1,000 μg. A beneficial evolution of fT4 to 38.6 pmol/L was noted with a suppressed TSH using daily intake. It was even necessary to gradually decrease the dosage during the follow-up. This favourable evolution coincided with her return from abroad.
Case 3
A 55-year-old woman with Graves' hyperthyroidism was treated with 8 mCi radioactive iodine at the age of 48. She subsequently developed severe hypothyroidism (TSH 201 mIU/ml and fT4 of 2.3 pmol/L) with symptoms of fatigue, increasing weight, constipation, hoarse voice and cold intolerance. She also had abnormal liver function tests and dyslipidaemia. In her personal medical history we noted a therapy-resistant essential hypertension necessitating multiple antihypertensive treatments (aliskiren, losartan, moxonidine, felodipine, nebivolol) and depression. Substitution therapy was raised to a dose of 350 μg levothyroxine daily because of evolution to severe hypothyroidism. Baseline laboratory data were unremarkable for the exception of severe hypercholesterolaemia and hypertriglyceridaemia. Urine analysis excluded the presence of severe proteinuria. A test for gliadine antibodies was negative, and lactose and urea breath tests were normal. A challenge test with 1,000 μg levothyroxine was performed. TSH declined to 69.8 mIU/L with a rise of fT4 to 13.3 pmol/L after 2 h, confirming the suspicion of pseudomalabsorption (Fig. 1). Baseline values for TSH and fT4 at the beginning of the absorption test were 94.31 mIU/L and 6.4 pmol/L.
The patient was ordered to take a weekly dose of levothyroxine 1,000 μg in our hospital under close supervision. Follow-up biological testing showed a TSH value of 5 mIU/L and fT4 of 15.9 pmol/L. Several attempts to alter the treatment to a daily dose or a 2-weekly dose led to a recurrence of severe hypothyroidism (TSH 108 mIU/L) and this also despite psychiatric support.
Discussion and Review
Hypothyroidism is a common endocrine disorder that is easily treatable with thyroid hormone replacement therapy which has proven to be an effective and inexpensive treatment. In some patients hypothyroidism persists despite therapy with high doses of levothyroxine [8]. In this clinical setting it is important to rule out gastrointestinal malabsorption (coeliac disease, lactose intolerance/lactase deficiency, intestinal infections, H. pylori infection, gastrointestinal surgery), nephrotic syndrome, liver or pancreatic disease, heart disease, pregnancy and/or interference of absorption by other drugs [6].
The bioavailability of synthetic levothyroxine is approximately 80% after oral ingestion. Absorption occurs mostly in the jejunum and ileum and is enhanced by a fasting state [2,3,6,8,9,10,11]. Interference in absorption of thyroid hormones with dietary elements (soja, prunes, nuts, and herbal remedies) or medication, with the most common being cholestyramine, colestipol, aluminium hydroxide-containing antacids, propranolol, laxatives, ferrous salts, calcium carbonate, lovastatin, phenytoin, carbamazepine and rifampicin, should be excluded if euthyroidism cannot be reached using replacement therapy [1,4,5,6,8,10,12,13,14,15,16]. Other reasons for reduced absorption are high age, high fibre diets, levothyroxine intake with food and hypothyroidism [6,9,17]. Also higher doses of levothyroxine are sometimes needed in rare cases of patients with thyroid hormone resistance.
The most common cause of failure of oral replacement therapy is non-compliance [9]. However, pseudomalabsorption due to intentional non-compliance as part of a psychiatric disorder should be considered, as illustrated in the present and other case reports [1,2,8,10,12,13,18,19,20,21,22,23]. If a patient has variable levels of fT4 and TSH including also periods of completely normal levels having been on the same substitution dosage for a long time, this can also suggest pseudomalabsorption. Diagnosis of pseudomalabsorption can be made after the exclusion of all causes of malabsorption. It is a factitious disorder with psychological and physical symptoms.
In order to diagnose ‘pseudomalabsorption,’' a 1,000-μg levothyroxine absorption/challenge test can be used to demonstrate an appropriate increase in fT4 levels (two- to threefold increase) and a decrease in TSH by 40% of the initial values after 2 h [2,5,17,18,24,25,26]. Using the oral levothyroxine absorption test, it is important that the patient is supervised by an experienced nurse or doctor. Side effects of a single high dose of levothyroxine are limited [13]. This can be explained by the fact that T4 is bound by circulating thyroxine-binding globulin and has to be converted to tri-iodothyronine (T3) to be biologically active. Using the absorption test, serum fT4 and TSH measurements are assessed before and after 1, 2, 4, and 6 h using supervised intake. An increase in fT4 is observed with a maximum level within the first 120 min, known to be a normal time interval for absorption by the small intestine. Moreover, normalization of fT4 and TSH following long-term supervised ingestion is another strong argument against true malabsorption [1,10,11,26,27]. One should further explore the possibility of true malabsorption when the absorption test is negative.
After the diagnosis of pseudomalabsorption one should further analyse these patients for a psychiatric condition. Further treatment may be complicated, when this problem is not recognized. Psychiatric disorders of depressive nature are possible in severe hypothyroidism. Some patients exhibit true psychopathology after successful treatment of the hypothyroidism. Most importantly, it does not correct the patient's attitude towards oral intake [1,2,10,18]. Some patients persist in low compliance in taking levothyroxine and are at risk for serious complications, sometimes also leading to unnecessary medical and surgical procedures. This psychiatric disorder, known as factitious disorder, is characterized by a fictitious history, exaggeration, aggravation, fluctuating physical symptoms, lying or using aliases, multiple hospital admissions without specific reasons, and extensive knowledge of medical symptomatology [1,2,8,22,28,29]. The purpose of this behaviour is to adopt the ‘sick role.’' A psycho-analytic explanation formulated by O'Shea [30] suggests that feelings of neglect and being abandoned are the underlying reason for this behaviour. External reinforcers such as economic gain are absent, so this is not a form of malingering [31]. This pathological behaviour can evoke a lot of ambivalence in clinicians. Clinicians have to be cautious in expressing these feelings, because this influences the outcome in a negative way. The clinician should adopt an empathic and understanding attitude while interacting with the patient [32]. These patients should be observed conservatively, and an attempt should be made to clarify both the medical and psychiatric diagnoses before any invasive procedure is undertaken [2,29]. The goal is to help patients express their emotional stress in a more acceptable and healthful manner. Close collaboration between the clinician and psychiatrist is necessary [32]. Early recognition is important since it could, to a considerable extent, avoid iatrogenic risks. Patients are prone to drop out of therapy with the possibility of seeking medical attention from other physicians [8,18,29]. Avoiding confrontation with the diagnosis of non-compliance may lead to a better therapeutic outcome [1]. It is our view that confronting the patient with non-compliance can be beneficial. This approach can avoid further invasive testing and enable referral to a psychiatrist. Informing the patient about the effects of poor compliance does sometimes improve the 5-year compliance follow-up [2]. This approach should be individually tailored in view of the sensitive nature of this diagnosis. Patients are more likely to accept psychiatric help, when they feel that their behaviour is accepted and understood as an expression of psychological (unconscious) factors [29].
Medical treatment strategies for pseudomalabsorption are parenteral infusion (intravenous every 3-4 days or intramuscular) of levothyroxine or supervised oral ingestion (daily or weekly with supervision by others) [4,12,13,22,26,27,33]. Once weekly administration of levothyroxine is safe and efficient and therefore a possible alternative to customary daily therapy. Autoregulatory mechanisms maintain near-euthyroidism. It is well tolerated, and there is no evidence of possible toxicity, including cardiac side effects. Serum fT4 levels rise significantly after weekly ingestion of levothyroxine, but changes in fT3 are minimal. In previous studies thyroid function tests demonstrate mild hypothyroidism using weekly treatment with higher TSH and lower serum fT3 and fT4 values, suggesting that for complete biochemical euthyroidism a slightly larger dose than 7 times the daily dose may be required. At the peripheral tissue level (cholesterol, sex hormone-binding globulin, liver, bone, and heart), the effects of weekly treatment do not differ from that of customary daily treatment despite differences in serum thyroid hormone levels [33].
Conclusion
In case of failure of oral substitution therapy for hypothyroidism, despite large doses of levothyroxine, an evaluation for drug interaction and diseases causing malabsorption should be performed. A 1,000-μg levothyroxine absorption test can be used to demonstrate pseudomalabsorption [8,20,25]. Treatment should focus on correction of hypothyroidism, frequently by supervised intake of levothyroxine, as well as on psychiatric evaluation and treatment.
Disclosure Statement
The authors declare that no competing financial interests exist.
References
- 1.Lips DJ, van Reisen MT, Voigt V, Venekamp W. Diagnosis and treatment of levothyroxine pseudomalabsorption. Neth J Med. 2004;62:114–118. [PubMed] [Google Scholar]
- 2.Ain KB, Refetoff S, Fein HG, Weintraub BD. Pseudomalabsorption of levothyroxine. JAMA. 1991;266:2118–2120. [PubMed] [Google Scholar]
- 3.Fish LH, Schwartz HL, Cavanaugh J, Steffes MW, Bantle JP, Oppenheimer JH. Replacement dose, metabolism, and bioavailability of levothyroxine in the treatment of hypothyroidism. Role of triiodothyronine in pituitary feedback in humans. N Engl J Med. 1987;316:764–770. doi: 10.1056/NEJM198703263161302. [DOI] [PubMed] [Google Scholar]
- 4.Morris JC. How do you approach the problem of TSH elevation in a patient on high-dose thyroid hormone replacement? Clin Endocrinol (Oxf) 2009;70:671–673. doi: 10.1111/j.1365-2265.2009.03536.x. [DOI] [PubMed] [Google Scholar]
- 5.Mandel SJ, Brent GA, Larsen PR. Levothyroxine therapy in patients with thyroid disease. Ann Intern Med. 1993;119:492–502. doi: 10.7326/0003-4819-119-6-199309150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Benvenga S, Bartolone L, Squadrito S, Lo Giudice F, Trimarchi F. Delayed intestinal absorption of levothyroxine. Thyroid. 1995;5:249–253. doi: 10.1089/thy.1995.5.249. [DOI] [PubMed] [Google Scholar]
- 7.Bolk N, Visser TJ, Nijman J, Jongste IJ, Tijssen JG, Berghout A. Effects of evening vs morning levothyroxine intake: a randomized double-blind crossover trial. Arch Intern Med. 2010;170:1996–2003. doi: 10.1001/archinternmed.2010.436. [DOI] [PubMed] [Google Scholar]
- 8.Eledrisi MS, Szymajda A, Alshanti M, Urban RJ. Noncompliance with medical treatment: pseudomalabsorption of levothyroxine. South Med J. 2001;94:833–836. [PubMed] [Google Scholar]
- 9.Muñoz-Torres M, Varsavsky M, Alonso G. Lactose intolerance revealed by severe resistance to treatment with levothyroxine. Thyroid. 2006;16:1171–1173. doi: 10.1089/thy.2006.16.1171. [DOI] [PubMed] [Google Scholar]
- 10.Ogawa D, Otsuka F, Mimura U, Ueno A, Hashimoto H, Kishida M, Ogura T, Makino H. Pseudomalabsorption of levothyroxine: a case report. Endocr J. 2000;47:45–50. doi: 10.1507/endocrj.47.45. [DOI] [PubMed] [Google Scholar]
- 11.Hays MT. Localization of human thyroxine absorption. Thyroid. 1991;1:241–248. doi: 10.1089/thy.1991.1.241. [DOI] [PubMed] [Google Scholar]
- 12.Molines L, Fromont I, Morlet-Barla N, Nogueira JP, Valéro R, Vialettes B. <span style=“font-variant:small-caps; text-transform:lowercase‛>L</span>-Levothyroxine pseudomalabsorption: a factitious disease. Presse Med. 2007;36:1390–1394. doi: 10.1016/j.lpm.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 13.Livadariu E, Valdes-Socin H, Burlacu MC, Vulpoi C, Daly AF, Beckers A. Pseudomalabsorption of thyroid hormones: case report and review of the literature. Ann Endocrinol (Paris) 2007;68:460–463. doi: 10.1016/j.ando.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Junglee NA, Scanlon MF, Rees DA. Increasing levothyroxine requirements in primary hypothyroidism: don't forget the urinalysis! J Postgrad Med. 2006;52:201–203. [PubMed] [Google Scholar]
- 15.Watts NB, Blevins LS., Jr Endocrinology. JAMA. 1994;271:1666–1668. [PubMed] [Google Scholar]
- 16.Centanni M, Gargano L, Canettieri G, Viceconti N, Franchi A, Delle Fave G, et al. Levothyroxine in goiter, Helicobacter pylori infection, and chronic gastritis. N Engl J Med. 2006;354:1787–1795. doi: 10.1056/NEJMoa043903. [DOI] [PubMed] [Google Scholar]
- 17.Jauk B, Mikosch P, Gallowitsch HJ, Kresnik E, Molnar M, Gomez I, Lind P. Unusual malabsorption of levothyroxine. Thyroid. 2000;10:93–95. doi: 10.1089/thy.2000.10.93. [DOI] [PubMed] [Google Scholar]
- 18.Payer J, Sladekova K, Kinova S, Cesnakova Z, Killinger Z, Krizko M, Klimes I, Langer P. Autoimmune thyroiditis with severe hypothyroidism resistant to the treatment with high peroral doses of levothyroxine: case report. Endocr Regul. 2000;34:189–193. [PubMed] [Google Scholar]
- 19.Goichot B, Vinzio S, Luca F, Sirlin X, Sapin R, Schlienger JL. In vivo evidence for a direct ultra-fast negative feedback of levothyroxine on TSH secretion in humans: a case of <span style=“font-variant:small-caps; text-transform:lowercase”>L</span>-levothyroxine pseudomalabsorption. Clin Endocrinol (Oxf) 2007;67:952–953. doi: 10.1111/j.1365-2265.2007.02975.x. [DOI] [PubMed] [Google Scholar]
- 20.Müssig K, Mörike K, Klein R, Sträter J, Georges G, Häring HU, Schnauder G. Hypothyroidism due to pseudo-malabsorption of levothyroxine - case 12/2009. Dtsch Med Wochenschr. 2009;134:2514. doi: 10.1055/s-0028-1082836. [DOI] [PubMed] [Google Scholar]
- 21.Pedrosa W, Santana G. Pseudomalabsorption of levothyroxine: a case report. Arq Bras Endocrinol Metabol. 2005;49:308–313. doi: 10.1590/s0004-27302005000200020. [DOI] [PubMed] [Google Scholar]
- 22.Kubota S, Fukata S, Matsuzuka F, Kuma K, Miyauchi A. Successful management of a patient with pseudomalabsorption of levothyroxine. Int J Psychiatry Med. 2003;33:183–188. doi: 10.2190/0YWR-8DRV-HHP4-UE2E. [DOI] [PubMed] [Google Scholar]
- 23.Srinivas V, Oyibo SO. Levothyroxine pseudomalabsorption and levothyroxine absorption testing using high-dose levothyroxine: a case report and discussion. Endocr Pract. 2010;16:1012–1015. doi: 10.4158/EP10224.CR. [DOI] [PubMed] [Google Scholar]
- 24.Hays MT. Absorption of oral levothyroxine in man. J Clin Endocrinol Metab. 1968;28:749–756. doi: 10.1210/jcem-28-6-749. [DOI] [PubMed] [Google Scholar]
- 25.Balla M, Jhingam RM, Rubin DJ. Rapid levothyroxine absorption testing: a case series of nonadherent patients. Int J Endocrinol Metab. 2015;13:e31051. doi: 10.5812/ijem.31051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walker JN, Shillo P, Ibbotson V, Vincent A, Karavitaki N, Weetman AP, Wass JAH, Allahabadia A. A thyroxine absorption test followed by weekly thyroxine administration: a method to assess non-adherence to treatment. Eur J Endocrinol. 2013;168:913–917. doi: 10.1530/EJE-12-1035. [DOI] [PubMed] [Google Scholar]
- 27.Butt MI, Gupta N, Tan HL, Waheed N. Clinical application of the levothyroxine absorption test in the diagnosis of pseudo-malabsorption. J Med Case Rep. 2014;2:253–255. [Google Scholar]
- 28.Krahn LE, Li H, O'Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160:1163–1168. doi: 10.1176/appi.ajp.160.6.1163. [DOI] [PubMed] [Google Scholar]
- 29.Gattaz WF, Dressing H, Hewer W. Münchhausen syndrome: psychopathology and management. Psychopathology. 1990;23:33–39. doi: 10.1159/000284635. [DOI] [PubMed] [Google Scholar]
- 30.O'Shea B. Factitious disorders: the Baron's legacy. Intern J Psychiatry Clin Pract. 2003;7:33–39. doi: 10.1080/13651500310001040. [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. ed 4, rev. Washington: American Psychiatric Association; 2000. [Google Scholar]
- 32.Haglund LA. Challenges in the treatment of factitious disorder: a case study. Arch Psychiatr Nurs. 2009;23:53–64. doi: 10.1016/j.apnu.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Grebe SK, Cooke RR, Ford HC, Fagerström JN, Cordwell DP, Lever NA, Purdie GL, Feek CM. Treatment of hypothyroidism with once weekly levothyroxine. J Clin Endocrinol Metab. 1997;82:870–875. doi: 10.1210/jcem.82.3.3830. [DOI] [PubMed] [Google Scholar]