Abstract
Psoriasis is a chronic, recurrent, and relatively common inflammatory dermatologic condition, which demonstrates various clinical manifestations including hair loss. It was once believed that alopecia was not a presentation of scalp psoriasis, but it is now widely accepted that psoriatic alopecia exists. Although the majority of patients get hair regrowth, it can potentially lead to permanent hair loss. Herein, we report a case of 26-year-old female patient with systemic lupus erythematosus who presented with scalp hair loss and nonpruritic scaly plaques on the scalp. Her clinical presentation, dermoscopic, and histopathologic findings were consistent with psoriatic alopecia. Additionally, we also described a novel scalp dermoscopic pattern of “patchy dotted vessels” which we detected in the lesion of scalp psoriasis.
Key Words: Psoriatic alopecia, Scalp psoriasis, Psoriasis
Introduction
Psoriasis is a chronic, recurrent, and relatively common inflammatory dermatologic condition, which demonstrates various clinical manifestations including hair loss. It was once believed that alopecia was not a presentation of scalp psoriasis, but it is now widely accepted that psoriatic alopecia exists [1]. Herein, we report a female patient with systemic lupus erythematosus who presented with scalp hair loss and nonpruritic scaly plaques on the scalp.
Case Report
A 26-year-old woman presented with scalp hair loss that had been noticed for 1 month. She also reported nonpruritic scaly plaques on the scalp. She denied a history of hair pulling. Eleven years before, she had been diagnosed as having systemic lupus erythematosus by the presence of malar rash, polyarthritis, proteinuria, positive antinuclear antibody (ANA), and positive anti-double stranded DNA (dsDNA) and was currently in a period of remission. She has been treated with chloroquine for 10 years, and the current dosage was 250 mg 4 times a week. She reported no family history of psoriasis.
Physical examination showed multiple scaly erythematous alopecic plaques on the frontal and both parietal regions of the scalp (Fig. 1a). Hair pull test was positive and revealed all telogen hairs. There was no nail, mucosal, or other skin lesions. Other physical examinations were unremarkable.
Fig. 1.
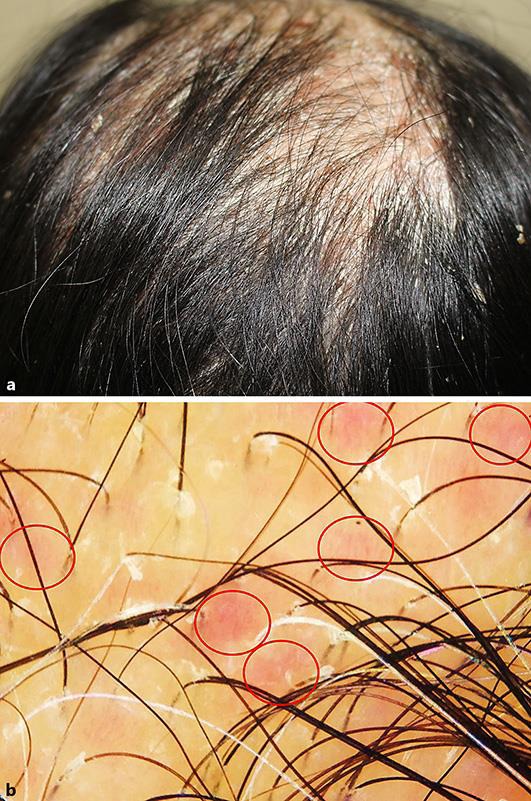
a Multiple scaly erythematous alopecic plaques on the frontal and both parietal regions of the scalp. b Dermoscopic examination (×20) showed decreased hair density, increased vellus hair follicles, diffuse white scales, and patchy dotted vessels (red circles).
Initially, the thick silvery scales were obtained for potassium hydroxide examination but no organisms were seen. Dermoscopic evaluation showed decreased hair density, increased vellus hairs, diffuse white scales, and numerous groups of dotted vessels distributed on the scalp (Fig. 1b). A 4-mm punch biopsy was done on the alopecic scaly erythematous plaque of the scalp for routine histopathologic examination. Histopathologic findings included superficial perivascular infiltration mainly composed of neutrophils, psoriasiform epidermal hyperplasia, parakeratosis, dilated tortuous blood vessels, decreased number of terminal hair, and sebaceous gland atrophy (Fig. 2). Correlating the clinical, dermoscopic, and histopathologic findings, the diagnosis of psoriatic alopecia was established.
Fig. 2.
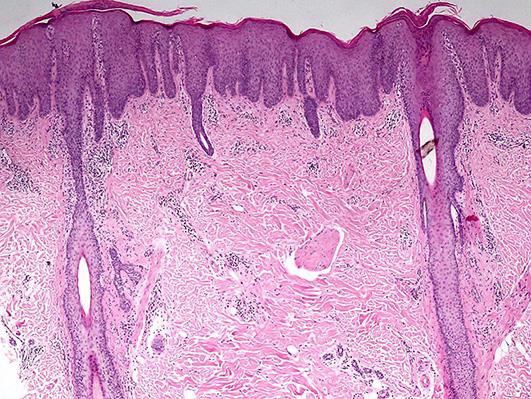
Histopathologic findings included superficial perivascular infiltration mainly composed of neutrophils, psoriasiform epidermal hyperplasia, parakeratosis, decreased number of terminal hair, and sebaceous gland atrophy (HE, ×40).
Treatment in our case included topical desoximethasone 0.25% scalp lotion to apply the scalp lesions twice daily, tar shampoo, and olive oil to the scalp before shampooing. After 3 weeks of treatment, she reported significant improvement in reduction of scales and stabilization of hair shedding (Fig. 3a). She achieved 75% hair regrowth by 3 months after therapy and had no recurrence of alopecia at the 1-year follow-up (Fig. 3b).
Fig. 3.
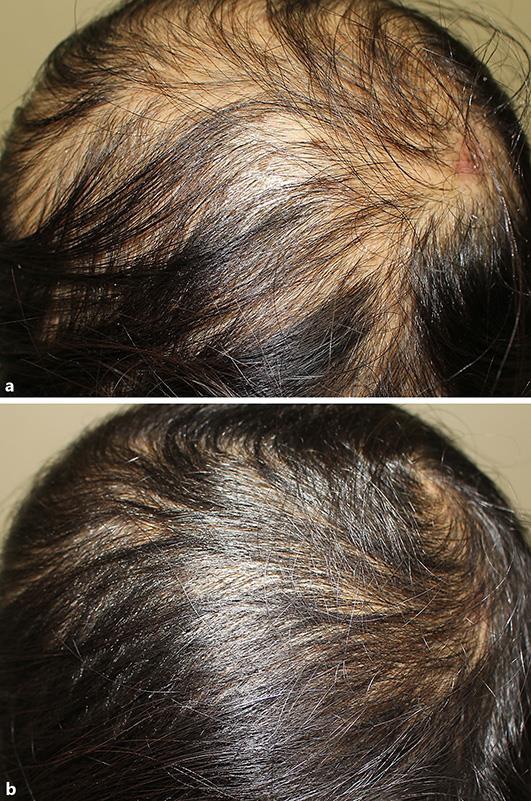
a Significant improvement in terms of decreased scalp inflammation and stabilization of hair loss after 3 weeks of treatment. b The patient achieved 75% hair regrowth at 3 months after treatment.
Discussion
Psoriasis is a chronic, recurrent, and relatively common inflammatory dermatologic condition which exhibits various clinical manifestations. It was believed that alopecia was not a presentation of scalp psoriasis until approximately 4 decades ago [1]. Nevertheless, it is now widely accepted that psoriatic alopecia exists. Hair loss is not restricted only to erythrodermic and generalized pustular psoriasis, but also seen in individuals with plaque-type psoriasis [2]. To date, the pathogenesis of psoriatic alopecia remains to be determined [3]. Alopecia could be a result of telogen effluvium secondary from an inflammatory process or mechanical changes due to friction [4]. Another possible explanation is that normal hair growth may be disturbed by thick adherent scales causing the inability of the hair shafts to grow normally [5]. Recently, it has been reported that hair loss in psoriatic skin may result from abnormal sebaceous gland function [6].
In 1972, Shuster [1] first described 3 types of psoriatic alopecia including psoriatic alopecia confined to lesional skin, acute hair fall associated with telogen effluvium, and psoriatic destructive or scarring alopecia. Psoriatic alopecia confined to lesional skin, which is the most common type, is characterized by nonscarring alopecia, finer hairs, and an increased number of dystrophic bulbs on silvery plaques. The second type, acute hair fall associated with telogen effluvium, is usually found in individuals suffering from severe psoriasis. Psoriatic scarring alopecia, the third type, is the least frequent form with only few published reports [1, 4]. In the largest case series, scarring alopecia secondary to psoriasis was noted in 12% of patients with psoriatic alopecia [5]. It has been suggested that a history of severe psoriasis, long-standing scalp involvement [3], immunosuppression [7], some genetic variants [8], and probably, staphylococcal infection [2, 9] are predisposing factors in developing follicular fibrosis. The clinical features show cicatricial alopecia on erythematous plaques with silvery scales [3].
Diagnosis of psoriatic alopecia can be established mainly based on characteristic clinical features. However, Runne et al. [5] found that 66% of affected individuals have never had psoriasis before and up to 36% experienced only scalp involvement without other manifestations. Therefore, histopathologic examination can be performed in order to confirm the diagnosis as well as to exclude other causes of alopecia.
The histopathologic features of psoriatic alopecia include follicular hyperkeratosis, increased number of telogen hairs, perifollicular lymphohistiocytic cell infiltrate around the isthmus and infundibular region [5]. The sebaceous glands are decreased in size and number. However, the sebaceous gland atrophy can also be found in scalp psoriasis without alopecia [3]. In psoriatic scarring alopecia, the interfollicular epidermis shows psoriasiform epidermal hyperplasia with parakeratosis, intraepidermal microabscesses of neutrophils as well as hypogranulosis. In horizontal sections, the follicular units are reduced in number and replaced by fibrotic tracts. Sebaceous glands are decreased in size and number, or even absent. There are also moderately dense lymphocytic cell infiltrate surrounding the isthmus and infundibular region [3].
In our case, differential diagnoses of the alopecic scaly erythematous plaques with silvery scales on the scalp consist of psoriatic alopecia, tinea capitis, severe seborrheic dermatitis, and importantly, chronic cutaneous lupus erythematosus (CCLE), which can occur in association with her underlying condition. Nevertheless, in our case, scalp dermoscopic and histopathologic evaluation showed concomitant findings of psoriatic alopecia as mentioned above. Kim et al. [10] reported that the most significant dermoscopic features of scalp psoriasis were red dots and globules, twisted red loops, and glomerular vessels. It is consistent with the dermoscopic finding of our case by the presence of numerous groups of dotted vessels distributed on the scalp. We coin the term “patchy dotted vessels” for this novel finding that we detected in the lesion of scalp psoriasis. Similarly, the histopathologic examination also highlighted relatively typical changes of psoriatic alopecia with the absence of CCLE findings. The histopathological features of psoriatic alopecia and CCLE are summarized in Table 1. As a result, CCLE and also other causes of alopecia were confidentially excluded.
Table 1.
Histopathological features of psoriatic alopecia and CCLE
| Psoriatic alopecia | CCLE | |
|---|---|---|
| Epidermal changes | Parakeratosis1 Hypogranulosis1 Psoriasiform epidermal hyperplasia1 |
Epidermal atrophy and/or follicular hyperkeratosis Vacuolar alterations with apoptotic keratinocytes along the basal layer and frequently at the dermal-epidermal junction Thick basement membrane |
| Dermal changes | Focal peribulbar lymphocytic infiltrates with occasional eosinophils Dilated tortuous blood vessels1 |
Dense superficial and deep perivascular lymphoplasmacytic infiltrate with frequent periadnexal involvement Deep dermal mucin may be seen |
| Hair and adnexal structures | Increased catagen or telogen hairs1 Dramatic sebaceous gland atrophy1 |
Normal or increased number of catagen of telogen hairs Preserved sebaceous glands |
The histopathological features that were found in our patient.
The link between psoriasis and lupus erythematosus, particularly in view of the induction or exacerbation of psoriasis during the treatment with synthetic antimalarials, has been reported in the literature [11]. Synthetic antimalarials including chloroquine and hydroxychloroquine have been noted to involve in triggering psoriasis, probably due to an alteration of the activity of enzymes that play a role in the epidermal proliferation process [12]. The average latency period for synthetic antimalarials was 3 weeks but it could take as long as 40.5 weeks in case of pustular eruptions in the patient with preexisting psoriasis [13]. Although it is worth considering drug-induced psoriasis in our case, it is somewhat unlikely. This can be supported by the fact that the latency period was relatively too long, her condition improved well after conventional treatment, and there was no exacerbation despite the continuous use of antimalarials. Our case experienced psoriatic alopecia with the absence of pre-existing psoriasis or other psoriatic features. This confirms the fact that alopecia can be the first and only single manifestation of psoriasis. To the best of our knowledge, no case of psoriatic alopecia in a patient with systemic lupus erythematosus has been previously described in the literature.
In respect to scalp psoriasis, no specific treatment for psoriatic alopecia, has been reported in the literature. Topical corticosteroid is a mainstay of treatment as it can inhibit epidermal proliferation, decrease inflammation, and modulate immune functions [14]. Over-night occlusion by using a shower cap can enhance drug penetration and efficacy. In patients with thick adherent scales or pityriasis amiantacea, topical keratolytics such as salicylic acid should be given as the first step in order to remove thick scales and to allow penetration of other topical medications [15]. Calcipotriol is an antipsoriatic agent since it can reduce epidermal proliferation, enhance normal keratinization, and also has anti-inflammatory effects. Calcipotriol can be used in combined formulations with topical corticosteroid. Other topical agents with active ingredients such as coal tar, dithranol, retinoids, and antifungals provided only minimal benefits [14].
Even though the prognosis of psoriatic alopecia is generally favorable, it can occasionally lead to permanent hair loss. It was reported that, of 41 patients, 34 patients achieved complete hair regrowth, whereas 2 patients suffered from persistent psoriatic alopecia after 7 years of follow-up. Cicatricial alopecia was observed in 7 patients who failed to regrow hair [5]. Thus, early recognition of the potential for permanent alopecia together with appropriate treatment are truly important in order to minimize the chance of developing irreversible scarring alopecia.
In conclusion, we report the case of psoriatic alopecia in a patient with systemic lupus erythematosus with the absence of other psoriatic features. Despite the rarity of psoriatic alopecia, it can be a manifestation of psoriasis and potentially result in permanent scarring alopecia, if it is overlooked or inadequately treated.
Statement of Ethics
We state that our patient gave informed consent. The research complies with all ethical guidelines for human studies.
Disclosure Statement
The authors have no financial disclosure. There was no funding or support.
References
- 1.Shuster S. Psoriatic alopecia. Br J Dermatol. 1972;87:73–77. doi: 10.1111/j.1365-2133.1972.tb05103.x. [DOI] [PubMed] [Google Scholar]
- 2.Van De Kerkhof PC, Chang A. Scarring alopecia and psoriasis. Br J Dermatol. 1992;126:524–525. doi: 10.1111/j.1365-2133.1992.tb11832.x. [DOI] [PubMed] [Google Scholar]
- 3.Bardazzi F, Fanti PA, Orlandi C, Chieregato C, Misciali C. Psoriatic scarring alopecia: observations in four patients. Int J Dermatol. 1999;38:765–768. doi: 10.1046/j.1365-4362.1999.00666.x. [DOI] [PubMed] [Google Scholar]
- 4.George SM, Taylor MR, Farrant PB. Psoriatic alopecia. Clin Exp Dermatol. 2015;40:717–721. doi: 10.1111/ced.12715. [DOI] [PubMed] [Google Scholar]
- 5.Runne U, Kroneisen-Wiersma P. Psoriatic alopecia: acute and chronic hair loss in 47 patients with scalp psoriasis. Dermatology. 1992;185:82–87. doi: 10.1159/000247418. [DOI] [PubMed] [Google Scholar]
- 6.Rittie L, Tejasvi T, Harms PW, Xing X, Nair RP, Gudjonsson JE, et al. Sebaceous gland atrophy in psoriasis: an explanation for psoriatic alopecia? J Invest Dermatol. 2016;136:1792–1800. doi: 10.1016/j.jid.2016.05.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El Shabrawi-Caelen L, La Placa M, Vincenzi C, Haidn T, Muellegger R, Tosti A. Adalimumab-induced psoriasis of the scalp with diffuse alopecia: a severe potentially irreversible cutaneous side effect of TNF-alpha blockers. Inflamm Bowel Dis. 2010;16:182–183. doi: 10.1002/ibd.20954. [DOI] [PubMed] [Google Scholar]
- 8.Cockayne SE, Messenger AG. Familial scarring alopecia associated with scalp psoriasis. Br J Dermatol. 2001;144:425–427. doi: 10.1046/j.1365-2133.2001.04046.x. [DOI] [PubMed] [Google Scholar]
- 9.Wright AL, Messenger AG. Scarring alopecia in psoriasis. Acta Derm Venereol. 1990;70:156–159. [PubMed] [Google Scholar]
- 10.Kim GW, Jung HJ, Ko HC, Kim MB, Lee WJ, Lee SJ, et al. Dermoscopy can be useful in differentiating scalp psoriasis from seborrhoeic dermatitis. Br J Dermatol. 2011;164:652–656. doi: 10.1111/j.1365-2133.2010.10180.x. [DOI] [PubMed] [Google Scholar]
- 11.Basavaraj KH, Ashok NM, Rashmi R, Praveen TK. The role of drugs in the induction and/or exacerbation of psoriasis. Int J Dermatol. 2010;49:1351–1361. doi: 10.1111/j.1365-4632.2010.04570.x. [DOI] [PubMed] [Google Scholar]
- 12.Namazi MR. Aggravation of psoriasis by antimalarials: a comment on the pathogenic mechanism. Indian J Dermatol Venereol Leprol. 2008;74:675–676. doi: 10.4103/0378-6323.45131. [DOI] [PubMed] [Google Scholar]
- 13.Tsankov N, Angelova I, Kazandjieva J. Drug-induced psoriasis. Recognition and management. Am J Clin Dermatol. 2000;1:159–165. doi: 10.2165/00128071-200001030-00003. [DOI] [PubMed] [Google Scholar]
- 14.Papp K, Berth-Jones J, Kragballe K, Wozel G, De La Brassinne M. Scalp psoriasis: a review of current topical treatment options. J Eur Acad Dermatol Venereol. 2007;21:1151–1160. doi: 10.1111/j.1468-3083.2007.02424.x. [DOI] [PubMed] [Google Scholar]
- 15.Van Der Vleuten CJ, Van De Kerkhof PC. Management of scalp psoriasis: guidelines for corticosteroid use in combination treatment. Drugs. 2001;61:1593–1598. doi: 10.2165/00003495-200161110-00006. [DOI] [PubMed] [Google Scholar]


