Abstract
Ribavirin (RBV), used in combination with alpha interferon to treat hepatitis C virus (HCV) infections, is a guanosine nucleotide analog that can increase the error rate of viral RNA-dependent RNA polymerases, imbalance intracellular nucleotide pools, and cause toxicity in many cell types. To determine potential mechanisms of RBV resistance during HCV RNA replication, we passaged HCV replicon-containing cell lines in the presence of increasing concentrations of RBV. RBV-resistant, HCV replicon-containing cell lines were generated, and the majority of RBV resistance was found to be conferred by changes in the cell lines. The resistant cell lines were defective in RBV import, as measured by [3H]RBV uptake experiments. These cell lines displayed reduced RBV toxicity and reduced error accumulation during infection with poliovirus, whose replication is known to be sensitive to RBV-induced error. For one RBV-resistant isolate, two mutations in the replicon RNA contributed to the observed phenotype. Two responsible mutations resided in the C-terminal region of NS5A, G404S, and E442G and were each sufficient for low-level RBV resistance. Therefore, RBV resistance in HCV replicon cell lines can be conferred by changes in the cell line or by mutations in the HCV replicon.
Hepatitis C virus (HCV) has infected approximately 170 million people worldwide, and it causes liver damage, which can progress to hepatocellular carcinoma (53). HCV patients are treated with a combination of ribavirin (RBV) and alpha interferon (IFN-α). This treatment reduces HCV RNA to undetectable levels in 30 to 40% of patients, but the majority of patients are not sustained responders (32). Whether this treatment failure is due to the development of drug-resistant viral variants is unknown. HCV studies are limited, because the virus cannot be grown in laboratory cultures. Fortunately, subgenomic and full-length replicon systems have been developed, allowing analysis of HCV RNA replication (2, 21, 27).
Several different mechanisms for the observed inhibition of HCV replication by RBV have been proposed. First, as has been shown for poliovirus (10, 11), RBV may induce lethal mutagenesis of the HCV genome. RBV is a guanosine nucleotide analog that can base pair with cytosine and uracil, increasing the viral error rate and debilitating the virus population by causing error catastrophe. Support for the hypothesis that RBV induces error catastrophe in the HCV genome comes from the observation that mutations accumulate in HCV replicons passaged in RBV (9). Second, RBV incorporation by the HCV polymerase may block elongation during RNA synthesis and therefore limit replication (28). Third, RBV may act by inhibition of IMP dehydrogenase (IMPDH) (46). IMPDH converts IMP to GMP, and inhibition of its activity alters intracellular nucleotide pools, possibly affecting RNA replication or translation of viral genomes. The toxicity of RBV observed in tissue culture cells may result from this nucleotide pool imbalance or from some other mechanism (1, 47). Fourth, RBV may affect the immune response to HCV, causing a bias in favor of a beneficial Th1 response (49). These potential mechanisms are not mutually exclusive, and it is likely that RBV acts through multiple mechanisms.
Drug resistance has been a major problem in treating RNA virus infections. It was initially thought that mutagenic antiviral drugs like RBV would be refractory to the development of resistance (4). RBV-resistant poliovirus, however, could be generated by passaging the virus in the presence of RBV (38). RBV resistance in poliovirus can be conferred by a single amino acid change, G64S, in the viral RNA-dependent RNA polymerase. G64S poliovirus displayed increased fidelity of RNA replication and reduced sensitivity to RBV and another mutagen, 5-azacytidine. Therefore, the mechanism of RBV resistance in poliovirus is likely to be a general increase in fidelity in the presence or absence of mutagen. Furthermore, that RBV resistance could be conferred by altered fidelity further supports the hypothesis that, in the case of poliovirus, RBV exerts its antiviral effect via increased error rate of the viral polymerase.
Here, we sought to determine whether RBV-resistant HCV replicon cell lines could be generated, both to explore potential mechanisms of RBV resistance and to understand the basis of the antiviral action of RBV for HCV. We found that RBV-resistant HCV replicon cell lines could be generated and that resistance could be conferred either by changes in the cell lines or by mutations in the replicon RNA.
MATERIALS AND METHODS
Replicons and cells.
All cell lines were grown in Dulbecco's modified Eagle medium supplemented with 10% fetal bovine serum, 100 U of penicillin-streptomycin/ml, and 0.1 mM nonessential amino acids. One milligram of G418 (Geneticin; Invitrogen, Carlsbad, Calif.)/milliliter was added to media to maintain Huh-7 cells containing HCV replicons, kindly provided by C. Rice (Rockefeller University) (2). Huh-7 cells were cured of replicon RNA by 2 months of passage in 100 U of interferon-α (Sigma, St. Louis, Mo.) in the absence of G418 as described previously (3). That the cells were cured of functional replicon RNA was confirmed by lack of colony formation by 7 × 106 cells in medium containing 1 mg of G418/ml, the concentration used in subsequent transfections to reintroduce wild-type replicons (data not shown). It should be noted that the RNA replicon transfected into the cured lines and used for subcloning of NS5 mutations differs from the replicons originally in the cells (2) by insertion of a 212-base fragment of nucleotides 74 to 286 of the lacα gene in reverse orientation just 3′ of the neo gene. This fragment was inserted to monitor error accumulation (to be described elsewhere); the modified replicon showed no difference in growth or RBV resistance (data not shown).
RBV passage experiments.
Huh-7 cells containing replicons were passaged every 1 to 3 days in media containing 100 to 400 μM RBV (Sigma) and 1 mg of G418/ml. We chose to use a relatively high, stringent concentration of G418 to ensure that RBV resistance was robust and to reduce background growth of Huh-7 cells. At each passage, most or all of the cells were maintained at a medium to high level of cell confluency. Pools 1, 2, and 4 resulted from a 1-month passage in 100 μM RBV, and potential pool 3 did not survive subsequent passage and was not studied further. For quantitative experiments (see Fig. 3 and 7), 106 cells of each type were passed identically every 1 to 3 days for a week, and cells were either stained with crystal violet or trypsinized and counted using trypan blue and a hemocytometer.
FIG. 3.
Testing cured cells for RBV resistance. (A) Crystal violet-stained cells after incubation with RBV. The original RBV-resistant cell lines from pool 1 and pool 4 were cured of replicon RNA and then transfected with wild-type replicon RNA to yield cured pool 1 plus replicon and cured pool 4 plus replicon lines. RBV resistance of these lines and the Huh-7 replicon-containing reference line were tested by passage in 300 μM RBV for 7 days. (B) Quantitation of cell survival in the presence of RBV. Surviving cells from two plates for each condition shown in panel A were trypsinized, stained with trypan blue, and counted using a hemocytometer. The experiment was repeated twice, and similar results were obtained. (C) [3H]RBV uptake kinetics. Huh-7, cured pool 1 (squares) or cured pool 4 (triangles) cells wereincubated with medium containing 5 μM 3H-labeled RBV. At indicated times the cells were washed, harvested, and lysed. Cell-associated 3H was quantified by scintillation counting. (D) RBV toxicity in the absence of viral genomes. RBV-sensitive (Huh-7) or RBV-resistant (cured pool 4) cell lines lacking HCV replicons were passaged for 7 days with or without 300 μM RBV and 300 μM guanosine. Surviving cells were stained with crystal violet.
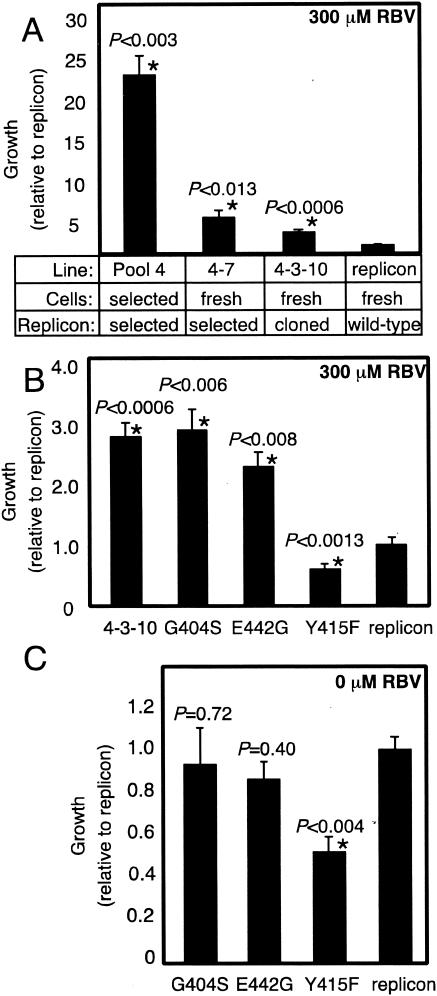
FIG. 7.
RBV resistance profiles of cell lines harboring replicons with mutations in NS5A and NS5B. Cells that contained the indicated replicons were passaged for 7 days in 300 μM RBV (A and B) or 0 μM RBV (C); surviving cells were counted using trypan blue. Data from duplicate plates from two to four independent experiments were averaged and normalized to the replicon control; standard error is shown. Statistically significant growth changes (P < 0.05, determined by two-sample Student's t test) relative to the replicon control are indicated by asterisks.
[3H]RBV uptake assay.
Tissue culture plates (35 mm diameter) containing 5 × 105 cells were treated with 150 μl of medium containing [3H]RBV (Moravek, Brea, Calif.) (the final concentration of RBV was 5 μM, with 4 nmol [3H]RBV at 8 Ci/mmol added). At various time points of incubation at 37°C, the medium was removed, cells were washed twice with cold phosphate-buffered saline and trypsinized, and cell pellets were resuspended in 50 μl of cold cell lysis buffer (10 mM Tris [pH 8], 10 mM NaCl, 1.5 mM MgCl2, 1% NP-40). Cell debris was removed by centrifugation, and 10 μl of the supernatant was quantified by scintillation counting. Less than 1% of the [3H]RBV in the medium was cell associated in these experiments. No difference in uptake rate was observed between 5 μM RBV and 300 μM RBV (data not shown).
RBV toxicity assay.
Approximately 4 × 105 Huh-7 cells or the cured pool 4 cells lacking replicons were split into media with or without 300 μM RBV and 300 μM guanosine. Cells were passed every 1 to 3 days, and on day 7 cells were stained with crystal violet (38).
Poliovirus RBV passage experiments.
For the experiments shown in Fig. 4A, 5 × 105 HeLa, Huh-7, or cured pool 4 cells on 60-mm-diameter tissue culture dishes were pretreated with or without 800 μM RBV for 1.5 h and were infected at a multiplicity of infection (MOI) of 10 PFU of type 1 Mahoney poliovirus per cell, as previously described (38). Five hours after infection, virus was harvested and its titers were determined on HeLa cell monolayers to determine the required inoculum for the next passage. The cycle was repeated for each of two to three passages, infecting with 10 PFU/cell each time.
FIG. 4.
Poliovirus growth and error accumulation during serial passage in RBV-sensitive and RBV-resistant cell lines. RBV-sensitive HeLa, RBV-sensitive Huh-7, or RBV-resistant cured pool 4 cells were infected with poliovirus at an MOI of 10 PFU per cell in the presence or absence of 800 μM RBV. (A) Resulting amounts of virus (PFU per cell) are shown as a function of passage number. Pass 3 for HeLa cells was not performed due to low virus titer in the 800 μM RBV sample from pass 2. Open squares, 0 μM RBV; black squares, 800 μM RBV; ND, not done; passage numbers are indicated below the graphs in panel B. (B) Error accumulation upon passage. Guanidine resistance frequencies of poliovirus progeny from each passage are shown for HeLa, Huh-7, and cured pool 4 cells. The PFU per milliliter on plates containing 0.5 mM guanidine was divided by the PFU per milliliter on plates lacking guanidine to determine an estimate of the error frequency. Clear bars, 0 μM RBV; black bars, 800 μM RBV.
Poliovirus fidelity assay.
The fidelity of poliovirus replication from the passages shown in Fig. 4 was determined by guanidine resistance assay (Fig. 4B), as previously described (38). Briefly, HeLa cell monolayers were infected with dilutions of virus and were incubated for 48 h under agar overlays with or without 0.5 mM guanidine HCl (Sigma). The relative error frequencies were calculated as the titer per milliliter on plates containing guanidine divided by the titer per milliliter on plates lacking guanidine.
RNA isolation, RNA synthesis, and transfections.
Total cellular RNA was harvested from cells by using TRIZOL (Invitrogen). RNA was transcribed in vitro from ScaI-linearized replicon cDNA using the T7 Ampliscribe kit (Epicentre, Madison, Wis.). Contaminating DNA was removed by DNase digestion and acid phenol extraction. Control transfections with mock transcriptions done in the absence of T7 RNA polymerase yielded no G418-resistant colonies, ensuring that colony formation was due to replicon RNA replication and not DNA contamination (data not shown). Huh-7 cells on 35-mm-diameter tissue culture dishes were transfected with 1 to 10 μg of cellular or in vitro-transcribed RNA by using DMRIE-C (Invitrogen) according to the manufacturer's instructions. Forty-eight hours after transfection, cells were split into medium containing 1 mg of G418/ml, and after 2 weeks of selection colonies were either pooled (see Fig. 3; also used to make the clone 4-3-10, G404S, E442G, and Y415F cell lines shown in Fig. 7) or individual colonies were picked and clonally expanded (see Fig. 5).
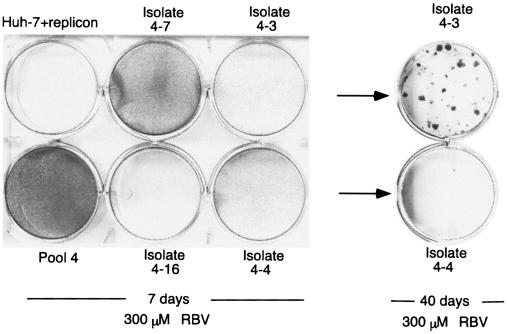
FIG. 5.
Testing replicons for RBV resistance. RNA was harvested from RBV-resistant isolates and transfected into fresh RBV-sensitive Huh-7 cells. After selection in G418, individual colonies were picked and tested for RBV resistance by passaging the cells in 300 μM RBV for 7 days and subsequently staining them with crystal violet. A representative experiment is shown in the left-hand cultures. The right-hand cultures show cells on a duplicate plate allowed to form colonies in 300 μM RBV for an additional 33 days to detect low-level resistance. RBV-sensitive control cell lines were unable to form colonies, even with 60 days of incubation (data not shown).
Cloning and sequencing of the HCV NS5 region.
RNA was isolated from clonal, colony-derived cell lines (see above), and after reverse transcription (RT) (SuperscriptII; Invitrogen) with antisense primers in the 3′-untranslated region (3′UTR) (CCTATTGGCCTGGAGTGTTTA) or 5′ region of NS5B (GATGGTGGTGTCAATTGGTG), products were amplified by PCR using Deep Vent Polymerase (New England Biolabs, Beverly, Mass.) and Taq (QIAGEN, Valencia, Calif.) in a 2:1 ratio with sense primers (GGAAGCTTAGTGGATCAACGAGGACTGCT or GGGAATTCAGATCCTGCGGAGGTCCAGG) and antisense primers (3′UTR above or GGTCTAGAGTTTCCTCCGCAGCGCATG). PCR products were subcloned into pUC19, and the inserts were sequenced (Sequetech, Mountain View, Calif.). Mutations resulting in amino acid changes are indicated in Fig. 6.
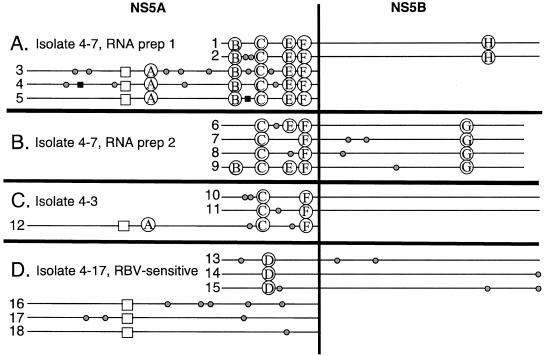
FIG. 6.
NS5A and NS5B sequence alignment from RBV-resistant and RBV-sensitive replicon-containing cell lines. RNA was isolated from colony-derived cell lines, and the NS5 regions of the replicons were amplified by RT-PCR and sequenced. Cloned regions from different isolates were chosen randomly for sequencing. (A and B) Two separate RNA pools from RBV-resistant isolate 4-7. (C) RBV-resistant isolate 4-3. (D) RBV-sensitive control isolate 4-17. Gray circles, nonconserved amino acid changes; black squares, stop codon; open squares, existing adaptive change S232I; A, R246C; B, P351L; C, G404S; D, Q399L; E, S434P; F, E442G; G, L384H; H, I432T. Silent mutations are not shown.
Plasmid construction.
A subset of mutations in NS5A contained in an XhoI/MfeI fragment was subcloned into fresh replicon cDNA from clone 10-derived cDNA (see Fig. 6C), and the resulting plasmid was termed 4-3-10. This clone contained the following mutations in the 3′ end of NS5A: coding changes A387V, V388D, G404S, and E442G and silent mutations at codons 325 and 436. The single NS5A mutations G404S (GGC changed to AGC) and E442G (GAG changed to GGG) were constructed by site-directed mutagenesis and were subcloned into the replicon cDNA via XhoI/MfeI fragments. The Y415F (TAT changed to TTC) NS5B mutation (54) was also made by site-directed mutagenesis and was subcloned into the replicon cDNA by using an MfeI/PflMI fragment. All plasmids were confirmed by sequencing the entire PCR-generated insert.
RESULTS
Passaging HCV replicon cells in RBV to generate RBV-resistant lines.
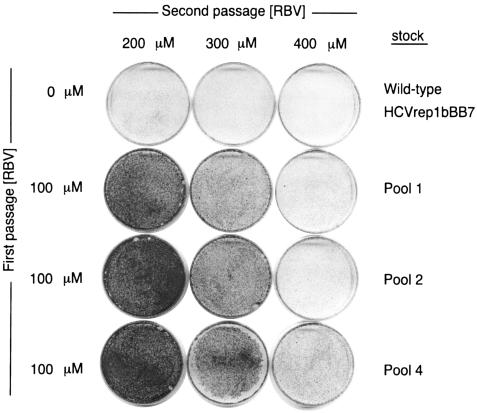
To isolate RBV-resistant HCV-containing cell lines, passages were performed at a variety of RBV concentrations. We chose to assay RBV sensitivity and resistance by the functional assay of cell growth in the presence of RBV and G418 rather than by RNA quantification, because, in the presence of RBV, viral RNAs are known to accumulate even when many are nonfunctional (10). Three separate pools of Huh-7 cells harboring HCV replicons (2) were passed in media containing 100, 200, 300, or 400 μM RBV; after 1 month, only the cells passed in 100 μM RBV survived. The surviving cell pools (pools 1, 2, and 4) from the 100 μM passage were then assayed in media containing 200, 300, or 400 μM RBV for 2 weeks. As shown in Fig. 1, cells that were first passaged in 100 μM RBV were able to survive passage for 2 weeks at higher RBV concentrations, with pool 4 surviving even at the highest RBV concentration tested. Therefore, the generation of RBV-resistant HCV replicon cell lines required passage in increasing concentrations of RBV, similar to the generation of RBV resistance in poliovirus (38).
FIG. 1.
Survival of hepatitis C virus (HCV) replicon-containing cells during passage in ribavirin (RBV). Huh-7 cells containing HCV replicons were passaged in 0 or 100 μM RBV for 4 weeks, as indicated at the left. Cell lines were then passaged in 200, 300, or 400 μM RBV for 2 weeks, and cells were stained with crystal violet.
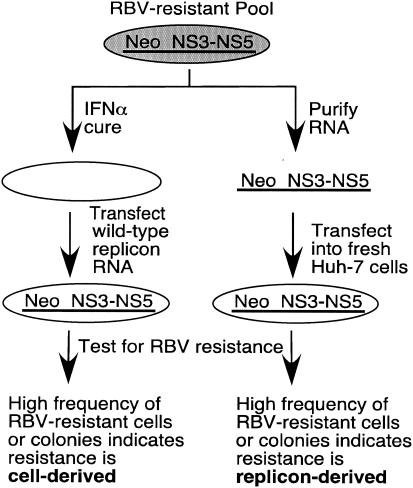
The RBV resistance observed could arise by mutations in the replicon or by changes in the cells. To discriminate between these two possibilities, we analyzed cell-based and replicon-based RBV-resistance separately, as outlined in Fig. 2.
FIG. 2.
Flow chart for mapping RBV resistance to cell line or replicon. The left-hand branch depicts RBV-resistant cell lines cured of replicon RNA by passage in IFN-α in the absence of G418. Cured cells were then transfected with wild-type replicon RNA, and the resulting G418-resistant cells were pooled and tested for resistance to RBV (see Fig. 3 and 4). The right-hand branch depicts total RNA harvested from RBV-resistant cell lines and transfected into fresh Huh-7 cells. After selection in G418, individual colonies were picked, expanded, and tested for resistance to RBV (see Table 1 and Fig. 5 to 7).
RBV resistance can be cell derived.
To test for cell-derived resistance, RBV-resistant pools 1 and 4 were cured of replicon RNA by treatment with IFN-α in the absence of G418 as described previously (3; see also Materials and Methods). Wild-type replicon RNA was then transfected into each of these cured lines, and hundreds of the resulting G418-resistant colonies were pooled to generate cell lines designated cured pool 1 plus replicon and cured pool 4 plus replicon. These cell lines were then tested for RBV resistance as shown in Fig. 3 and 4. Specifically, cured pool 1 and cured pool 4 cell lines that contained wild-type replicons were tested for RBV resistance by passage in 300 μM RBV, a dose that kills nonresistant cell lines in 7 days. As shown in Fig. 3A and B, changes to the cell line were sufficient to confer RBV resistance in both the pool 1 and pool 4 lines. Furthermore, RBV resistance could be selected in Huh-7 cells that did not contain replicons (data not shown). However, the original pool 4 cells, selected from replicon-containing Huh-7 cells, displayed a high level of resistance (Fig. 1); as will be shown later, replicon mutations also contribute to the RBV-resistant phenotype seen in pool 4.
Mechanism of cell-derived RBV resistance.
Reduced import or increased export of nucleoside analog drugs is often a reason for treatment failure in cancer patients (41). To test whether RBV uptake was defective in the RBV-resistant cells, the kinetics of RBV accumulation for Huh-7, cured pool 1, and cured pool 4 cells was monitored over time (Fig. 3C). Cells were incubated in 5 μM 3H-labeled RBV, and cell-associated radioactivity was quantified. The RBV-resistant lines cured pool 1 and cured pool 4 displayed major defects in RBV import or intracellular stability compared to RBV-sensitive Huh-7 cells (Fig. 3C). It is possible this uptake defect may preexist in the Huh-7 cell population, before RBV passage. Huh-7 cells were derived from a differentiated hepatoma tumor and are probably genetically unstable.
In the case of HCV, the antiviral action of RBV may be caused by lethal mutagenesis, nucleotide pool imbalance through IMPDH inhibition, general toxicity, or some combination of these effects. To test whether cellular toxicity plays a role in RBV-mediated death of Huh-7-based cell lines, Huh-7 and cured pool 4 cell lines that lacked replicons were passaged for 7 days in the presence or absence of 300 μM RBV. As shown in Fig. 3D, treatment with 300 μM RBV resulted in significant death of Huh-7 cells, whereas RBV treatment had no effect on the survival of the RBV-resistant cured pool 4 cell line. Interestingly, we found that addition of 300 μM guanosine allowed Huh-7 cell survival when passaged in RBV (Fig. 3D). Zhou et al. (56) had shown previously that guanosine could rescue the RBV sensitivity of HCV replicons. These results argue that RBV is toxic to Huh-7 cells, independent of HCV replicon error accumulation, and selective pressure for RBV resistance may be exerted at the level of cell as well as viral replication.
To test whether error catastrophe occurs more readily in Huh-7, cured pool 4, or HeLa cells, we monitored infections of these cells with poliovirus, which is known to be susceptible to error catastrophe in HeLa cells (10, 11, 38). Figure 4A shows the results of serial single-cycle passages of poliovirus in the presence and absence of 800 μM RBV. Cells were infected at an MOI of 10 PFU/cell, and cell-associated virus was harvested 5 h postinfection and its titer determined as described previously (38). This cycle was repeated for several passages, and each time the inoculum was 10 PFU from the previous passage viral stock/cell. As shown previously (38), poliovirus passaged in HeLa cells was observed to undergo striking titer reduction in the presence of 800 μM RBV (Fig. 4A). Furthermore, this titer reduction was more pronounced in passage 2 than passage 1, despite similar inoculum titers; this accumulation of mutations is a hallmark of error catastrophe. In Huh-7 cells, on the other hand, poliovirus yields showed only a fivefold reduction in titer at each passage in 800 μM RBV. This reduction did not increase with further passage, as would be expected for cumulative mutagenesis. Poliovirus passaged in the cured pool 4 cell line showed no susceptibility to RBV at any passage.
Whether the titer reductions above correlated with increased error frequency was determined by guanidine resistance assay. Poliovirus resistance to guanidine can be generated by single or multiple point mutations in the genome (11, 39, 52). By measuring the number of resistant viruses in a population, relative error frequencies can be determined. The titers of virus from each passage from Fig. 4A were determined in the presence and absence of 0.5 mM guanidine, and the relative error frequencies were graphed as a function of passage number (Fig. 4B). As expected, error frequency increased dramatically for poliovirus passaged in HeLa cells in the presence of 800 μM RBV. For poliovirus passaged in Huh-7 cells, the error frequency increased approximately fivefold, but no additional increase was observed in passages 2 and 3. Finally, for the RBV-resistant cured pool 4 cells, where poliovirus titer was not reduced by RBV treatment, no increase in error frequency was observed in the presence of RBV. These results argue that RBV induces poliovirus error catastrophe strongly in HeLa cells, weakly in Huh-7 cells, and not at all in RBV-resistant cured pool 4 cells.
RBV resistance can be conferred by mutations in the replicon.
To determine whether mutations in the replicons could confer RBV resistance, RNA preparations from the original resistant cell lines, pools 1, 2, and 4, were transfected into Huh-7 cells (Fig. 2). Individual G418-resistant colonies were identified and expanded, and each colony-derived cell line was tested for RBV resistance. From a total of 31 colonies, only two from pool 4 were resistant to 300 μM RBV, and they were designated 4-3 and 4-7 (Table 1). A representative experiment showing the results of the RBV passage is shown in Fig. 5. The parental line, pool 4, showed high-level RBV resistance; the clonal line 4-7 showed mid-level resistance; and the clonal line 4-3 showed low but detectable resistance in which surviving colonies were seen only upon prolonged incubation. Isolate 4-4, like most replicon-containing Huh-7 lines, showed no colony formation even upon prolonged incubation. Therefore, these results argued that RBV resistance could be conferred by the changes in the replicons found in isolates 4-3 and 4-7.
TABLE 1.
RBV resistance of colony cell lines derived from RBV-resistant cell RNA transfected into Huh-7 cells
| RNA pool | No. of colonies tested | No. of RBV-resistant colonies |
|---|---|---|
| 1 | 11 | 0 |
| 2 | 9 | 0 |
| 4 | 11 | 2 (clones 4-3 and 4-7) |
The mutation or mutations in isolates 4-3 and 4-7 that were responsible for RBV resistance could, in principle, be anywhere in the replicon. Based on our previous results with poliovirus, we hypothesized that the mutations would lie within the coding region for the viral RNA-dependent RNA polymerase, NS5B. Therefore, initial sequencing was performed only on the NS5B region of the genome. RNA was isolated from the 4-3 and 4-7 RBV-resistant cell lines, and the NS5B region was amplified by RT-PCR, subcloned, and sequenced. Upon alignment of more than 20 sequences, some of which are shown in Fig. 6, no common amino acid changes were found, although there were many silent mutations and nonconserved amino acid changes, most of which were from transition mutations characteristic of RBV-mediated errors (11 and data not shown). Many such mutations were also found in the clones derived from serially passaged lines that did not prove to be RBV resistant (Fig. 6D). There were several common silent mutations among clonal pools, suggesting that the replicons from which they were derived were of common origin, making it even more surprising that no common NS5B mutations were found. However, several shared amino acid changes were observed at the C terminus of NS5A, a region fortuitously amplified by one of the primer sets. Therefore, the NS5A coding region was sequenced for several RNA preparations, and alignment of NS5A sequences from RBV-resistant lines 4-3 and 4-7 revealed common mutations (Fig. 6A to C). Specifically, two mutations, G404S (mutation C) and E442G (mutation F), were present in every RBV-resistant clone and none of the RBV-sensitive clones.
To determine whether any of the identified mutations in the C terminus of NS5A were sufficient for RBV resistance, a restriction fragment from clone 10 in Fig. 6 was subcloned into a new replicon, RNA transcripts were transfected into Huh-7 cells, and G418-resistant colonies were pooled to yield a cell line termed clone 4-3-10. The clone 4-3-10 replicon cell line had the following mutations in the C terminus of NS5A: G404S and E442G, present in all RBV-resistant replicons, and A387V and V388D, two mutations not conserved among the RBV-resistant clones. As shown in Fig. 7A, the mutations in clone 4-3-10 were sufficient to confer significant RBV resistance. The resistance of the 4-3-10 line and of the 4-7 line, in which total RNA from pool 4 was introduced into fresh Huh-7 cells, were considerably less than that of pool 4; as discussed previously, much of the resistance of pool 4 was cell derived. Nonetheless, mutations in 4-3-10 conferred significant RBV resistance, and when the G404S and E442G mutations, present in all RBV-resistant replicons tested, were analyzed individually for survival in 300 μM RBV, each was sufficient for the level of RBV resistance observed in clone 4-3-10 (Fig. 7B). Although these mutations have not yet been frequently observed in patient polymorphisms, few examinations of HCV quasispecies before and after RBV treatment have been reported.
A mutation in NS5B, Y415F, has been shown to display enhanced sensitivity to RBV, as measured by replicon RNA levels (54). As shown in Fig. 7B, passage in 300 μM RBV reduced growth in the Y415F-containing replicon cell line 1.6-fold compared to that of the replicon cell line control. To test whether differences in the survival of replicon-containing cells could be attributed to growth defects in the different replicon cell lines, growth in the absence of RBV was also monitored (Fig. 7C). The ribavirin-sensitive Y415F replicon cell line indeed showed a slight growth defect compared to the wild-type replicon cell line (Fig. 7C), suggesting that part of its enhanced sensitivity to RBV may result from reduced fitness. Neither of the RBV-resistant replicon cell lines, G404S and E442G, showed enhanced growth compared to that of the wild-type replicon (Fig. 7C), arguing that their enhanced resistance to RBV does not result from increased fitness but instead from resistance to the antiviral function of RBV.
DISCUSSION
Our objective in this study was to generate RBV-resistant HCV replicon cell lines to understand both the antiviral mechanism of RBV and how resistance can arise. We isolated HCV replicon cell lines that were resistant to relatively high concentrations of RBV by stepwise passage in increasing concentrations of RBV. We determined that RBV resistance could be conferred by changes in the cells, in the replicons, or both.
The mechanism of drug resistance in RBV-resistant pool 1 and pool 4 cell lines is reduced RBV import (Fig. 3C). Reduced import or increased export of nucleoside analog-based pharmaceuticals is often a reason for treatment failure in cancer patients (41). Whether HCV patients develop resistance to RBV by reduced import is not known. Nonetheless, the RBV import defect in the RBV-resistant cell lines may result from downregulation of a nucleotide transporter. Although the transporter or transporters required for RBV import into liver cells are not yet known, they are likely among the small number of identified nucleotide transporters (24). Candidates include the human equilibrative nucleoside transporters hENT1 and hENT2, which are predominately responsible for uptake of physiological purine and pyrimidine nucleosides, and the human concentrative nucleoside transporters hCNT1 and hCNT2, which are able to import nucleosides into cells against concentration gradients (5). It has been postulated that intestinal uptake of RBV is mediated by hCNT2 (36), and the hCNT1 protein is known to import several different nucleotide analogs, including the anti-HIV drug AZT and the anticancer drug gemcitabine (30, 40). We are presently comparing RBV-sensitive and RBV-resistant cell lines by DNA microarray analysis to identify potential differences in abundance of individual mRNAs.
The antiviral mechanism of RBV in HCV patients is not known, and it may involve multiple mechanisms. As shown in Fig. 4, poliovirus passaged in HeLa cells in the presence of RBV undergoes error catastrophe, with massive titer reductions that correlate with increases in error frequency. However, poliovirus passaged in Huh-7 cells did not undergo classic error catastrophe: viral titer was reduced only minimally and errors increased, but they did not continue to increase upon passage. These results suggest that Huh-7 cells provide an environment that is more permissive to viral replication in the presence of a mutagen than HeLa cells. RBV was toxic to Huh-7 cells in the absence of poliovirus or HCV replicons (Fig. 3D). Poliovirus replication titers, error accumulation, and cell toxicity were all rescued in the RBV-resistant cell lines (Fig. 3D and 4). Therefore, the mechanism of the antiviral action of RBV in Huh-7 cells could be through error accumulation, cellular toxicity, or both.
RBV resistance was also conferred by mutations in the replicon. We initially hypothesized that RBV resistance would map to NS5B, because RBV resistance in poliovirus was conferred by a mutation in the polymerase (38). To our surprise, mutations in the C terminus of NS5A were sufficient to provide RBV resistance. NS5A has many published functions, which does little to delimit potential mechanisms by which mutations in NS5A could confer RBV resistance. For example, the NS5A mutations could affect the fidelity of RNA synthesis. NS5A interacts with NS5B and can affect its activity (43, 44). Perhaps the mutant NS5A interacts with NS5B and acts as an allosteric effector of fidelity, reducing the number of mutations per genome. Alternatively, the mutations in NS5A could alter the cell environment in a way that promotes increased fidelity of RNA replication. We are presently measuring error frequencies in cell lines harboring mutant or wild-type NS5A replicons.
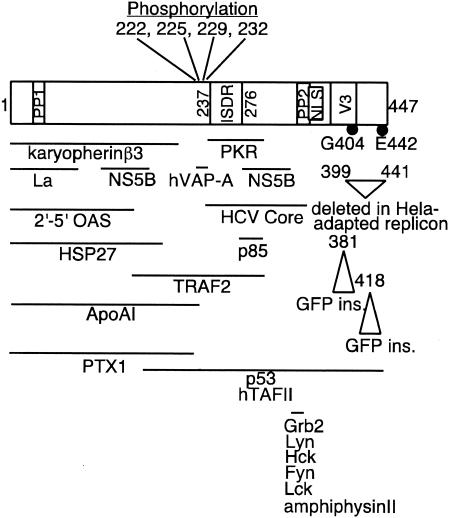
Second, mutations in NS5A may alter the cellular environment in which the replicon is propagated. NS5A has been reported to interact with over 20 different cellular proteins, and the list is growing. Expression of NS5A affects transcription of cellular targets (18, 31), alters signal transduction cascades (20, 35, 50), promotes cell growth (18), inhibits the interferon response (16, 48), and blocks apoptosis (8, 26). A partial summary of NS5A domains and interaction sites is shown in Fig. 8. Interestingly, the C terminus of NS5A contains a variable region termed V3, which includes Gly404, and mutations in this region may affect response to antiviral treatment (34). Additionally, the NS5A C-terminal region is tolerant of insertions such as the entire coding region of green fluorescent protein, and it has been proposed that this region is flexible and exposed, perhaps undergoing induced folding upon ligand binding (33, 37). A deletion in the C terminus of NS5A was found in replicons able to replicate in HeLa cells (57). The viability of RNA containing such a deletion might argue that the primary function of the C terminal region of NS5A is to achieve a dispensable effect on the host.
FIG. 8.
Summary of selected NS5A domains and interaction sites. The locations of Gly404 and Glu442, which were mutated in the RBV-resistant replicons, are indicated by black circles. The 447-amino-acid sequence of NS5A is drawn schematically to scale. PP1 and PP2, polyproline motifs 1 and 2; ISDR, interferon-sensitivity determining region; NLS, nuclear localization sequence; V3, variable region 3. See the following references for more information: phosphorylation sites (25, 51), NLS (23), ISDR (12, 13), V3 (34), PP1 and PP2 (50), karyopherins β3 (7), PKR (15), NS5B (44), hVAP-A (14), La (22), 2′-5′ OAS (2′-5′ oligoadenylate synthetase) (48), HCV core (19), HSP27 (6), p85 (regulatory subunit of phosphatidylinositol 3-kinase) (45), TRAF2 (35), ApoAI (42), PTX1 (17), p53 and hTAFII (26), Grb2 (29, 50), Lyn/Hck/Fyn/Lck (29), amphiphysinII (55), green fluorescent protein insertion sites (33), and region deleted in HeLa-adapted replicon (57).
While testing the NS5A mutations for RBV resistance, we also tested a previously characterized mutation in NS5B, Y415F, which was shown by Young et al. (54) to confer enhanced sensitivity to RBV. They proposed that the wild-type replicon, containing Y415, was actually RBV resistant, perhaps because it was cloned from patients receiving RBV therapy. In their study, RBV resistance was monitored by replicon RNA quantification. Using a cell survival assay instead, we also found that Y415F replicon cells lines showed reduced survival compared to wild-type replicon cell lines (Fig. 7B). Therefore, relative to the Y415F replicon, the wild-type replicon is slightly resistant to RBV. Based on our data, the hierarchy of RBV resistance, from the most to the least resistant, is NS5A-G404S ≅ NS5A-E442G > wild type > NS5B-Y415F. It is possible that other mutations in HCV replicons will also be found to confer enhanced RBV resistance or sensitivity and will inform analysis of the sequence variants found in patient populations.
Acknowledgments
We thank Scott Crowder and Peter Sarnow for critical reviews of the manuscript and Charlie Rice for the HCV replicons.
This work was supported by the National Institutes of Health and the Hutchison Foundation for Translational Research. J.K.P. is a Rebecca Ridley Kry Fellow of the Damon Runyon Cancer Research Foundation.
REFERENCES
- 1.Airaksinen, A., N. Pariente, L. Menendez-Arias, and E. Domingo. 2003. Curing of foot-and-mouth disease virus from persistently infected cells by ribavirin involves enhanced mutagenesis. Virology 311:339-349. [DOI] [PubMed] [Google Scholar]
- 2.Blight, K. J., A. A. Kolykhalov, and C. M. Rice. 2000. Efficient initiation of HCV RNA replication in cell culture. Science 290:1972-1974. [DOI] [PubMed] [Google Scholar]
- 3.Blight, K. J., J. A. McKeating, and C. M. Rice. 2002. Highly permissive cell lines for subgenomic and genomic hepatitis C virus RNA replication. J. Virol. 76:13001-13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cameron, C. E., and C. Castro. 2001. The mechanism of action of ribavirin: lethal mutagenesis of RNA virus genomes mediated by the viral RNA-dependent RNA polymerase. Curr. Opin. Infect. Dis. 14:757-764. [DOI] [PubMed] [Google Scholar]
- 5.Cass, C. E., J. D. Young, and S. A. Baldwin. 1998. Recent advances in the molecular biology of nucleoside transporters of mammalian cells. Biochem. Cell Biol. 76:761-770. [DOI] [PubMed] [Google Scholar]
- 6.Choi, Y. W., Y. J. Tan, S. G. Lim, W. Hong, and P. Y. Goh. 2004. Proteomic approach identifies HSP27 as an interacting partner of the hepatitis C virus NS5A protein. Biochem. Biophys. Res. Commun. 318:514-519. [DOI] [PubMed] [Google Scholar]
- 7.Chung, K. M., J. Lee, J. E. Kim, O. K. Song, S. Cho, J. Lim, M. Seedorf, B. Hahm, and S. K. Jang. 2000. Nonstructural protein 5A of hepatitis C virus inhibits the function of karyopherin beta3. J. Virol. 74:5233-5241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung, Y. L., M. L. Sheu, and S. H. Yen. 2003. Hepatitis C virus NS5A as a potential viral Bcl-2 homologue interacts with Bax and inhibits apoptosis in hepatocellular carcinoma. Int. J. Cancer 107:65-73. [DOI] [PubMed] [Google Scholar]
- 9.Contreras, A. M., Y. Hiasa, W. He, A. Terella, E. V. Schmidt, and R. T. Chung. 2002. Viral RNA mutations are region specific and increased by ribavirin in a full-length hepatitis C virus replication system. J. Virol. 76:8505-8517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crotty, S., C. E. Cameron, and R. Andino. 2001. RNA virus error catastrophe: direct molecular test by using ribavirin. Proc. Natl. Acad. Sci. USA 98:6895-6900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crotty, S., D. Maag, J. J. Arnold, W. Zhong, J. Y. Lau, Z. Hong, R. Andino, and C. E. Cameron. 2000. The broad-spectrum antiviral ribonucleoside ribavirin is an RNA virus mutagen. Nat. Med. 6:1375-1379. [DOI] [PubMed] [Google Scholar]
- 12.Enomoto, N., I. Sakuma, Y. Asahina, M. Kurosaki, T. Murakami, C. Yamamoto, N. Izumi, F. Marumo, and C. Sato. 1995. Comparison of full-length sequences of interferon-sensitive and resistant hepatitis C virus 1b. Sensitivity to interferon is conferred by amino acid substitutions in the NS5A region. J. Clin. Investig. 96:224-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Enomoto, N., I. Sakuma, Y. Asahina, M. Kurosaki, T. Murakami, C. Yamamoto, Y. Ogura, N. Izumi, F. Marumo, and C. Sato. 1996. Mutations in the nonstructural protein 5A gene and response to interferon in patients with chronic hepatitis C virus 1b infection. N. Engl. J. Med. 334:77-81. [DOI] [PubMed] [Google Scholar]
- 14.Evans, M. J., C. M. Rice, and S. P. Goff. 2004. Phosphorylation of hepatitis C virus nonstructural protein 5A modulates its protein interactions and viral RNA replication. Proc. Natl. Acad. Sci. USA 101:13038-13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gale, M., Jr., C. M. Blakely, B. Kwieciszewski, S. L. Tan, M. Dossett, N. M. Tang, M. J. Korth, S. J. Polyak, D. R. Gretch, and M. G. Katze. 1998. Control of PKR protein kinase by hepatitis C virus nonstructural 5A protein: molecular mechanisms of kinase regulation. Mol. Cell. Biol. 18:5208-5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gale, M. J., Jr., M. J. Korth, N. M. Tang, S. L. Tan, D. A. Hopkins, T. E. Dever, S. J. Polyak, D. R. Gretch, and M. G. Katze. 1997. Evidence that hepatitis C virus resistance to interferon is mediated through repression of the PKR protein kinase by the nonstructural 5A protein. Virology 230:217-227. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh, A. K., M. Majumder, R. Steele, R. Ray, and R. B. Ray. 2003. Modulation of interferon expression by hepatitis C virus NS5A protein and human homeodomain protein PTX1. Virology 306:51-59. [DOI] [PubMed] [Google Scholar]
- 18.Ghosh, A. K., R. Steele, K. Meyer, R. Ray, and R. B. Ray. 1999. Hepatitis C virus NS5A protein modulates cell cycle regulatory genes and promotes cell growth. J. Gen. Virol. 80:1179-1183. [DOI] [PubMed] [Google Scholar]
- 19.Goh, P. Y., Y. J. Tan, S. P. Lim, S. G. Lim, Y. H. Tan, and W. J. Hong. 2001. The hepatitis C virus core protein interacts with NS5A and activates its caspase-mediated proteolytic cleavage. Virology 290:224-236. [DOI] [PubMed] [Google Scholar]
- 20.Gong, G., G. Waris, R. Tanveer, and A. Siddiqui. 2001. Human hepatitis C virus NS5A protein alters intracellular calcium levels, induces oxidative stress, and activates STAT-3 and NF-kappa B. Proc. Natl. Acad. Sci. USA 98:9599-9604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo, J. T., V. V. Bichko, and C. Seeger. 2001. Effect of alpha interferon on the hepatitis C virus replicon. J. Virol. 75:8516-8523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Houshmand, H., and A. Bergqvist. 2003. Interaction of hepatitis C virus NS5A with La protein revealed by T7 phage display. Biochem. Biophys. Res. Commun. 309:695-701. [DOI] [PubMed] [Google Scholar]
- 23.Ide, Y., L. Zhang, M. Chen, G. Inchauspe, C. Bahl, Y. Sasaguri, and R. Padmanabhan. 1996. Characterization of the nuclear localization signal and subcellular distribution of hepatitis C virus nonstructural protein NS5A. Gene 182:203-211. [DOI] [PubMed] [Google Scholar]
- 24.Jarvis, S. M., J. A. Thorn, and P. Glue. 1998. Ribavirin uptake by human erythrocytes and the involvement of nitrobenzylthioinosine-sensitive (es)-nucleoside transporters. Br. J. Pharmacol. 123:1587-1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katze, M. G., B. Kwieciszewski, D. R. Goodlett, C. M. Blakely, P. Neddermann, S. L. Tan, and R. Aebersold. 2000. Ser(2194) is a highly conserved major phosphorylation site of the hepatitis C virus nonstructural protein NS5A. Virology 278:501-513. [DOI] [PubMed] [Google Scholar]
- 26.Lan, K. H., M. L. Sheu, S. J. Hwang, S. H. Yen, S. Y. Chen, J. C. Wu, Y. J. Wang, N. Kato, M. Omata, F. Y. Chang, and S. D. Lee. 2002. HCV NS5A interacts with p53 and inhibits p53-mediated apoptosis. Oncogene 21:4801-4811. [DOI] [PubMed] [Google Scholar]
- 27.Lohmann, V., F. Korner, J. Koch, U. Herian, L. Theilmann, and R. Bartenschlager. 1999. Replication of subgenomic hepatitis C virus RNAs in a hepatoma cell line. Science 285:110-113. [DOI] [PubMed] [Google Scholar]
- 28.Maag, D., C. Castro, Z. Hong, and C. E. Cameron. 2001. Hepatitis C virus RNA-dependent RNA polymerase (NS5B) as a mediator of the antiviral activity of ribavirin. J. Biol. Chem. 276:46094-46098. [DOI] [PubMed] [Google Scholar]
- 29.Macdonald, A., K. Crowder, A. Street, C. McCormick, and M. Harris. 2004. The hepatitis C virus NS5A protein binds to members of the Src family of tyrosine kinases and regulates kinase activity. J. Gen. Virol. 85:721-729. [DOI] [PubMed] [Google Scholar]
- 30.Mackey, J. R., R. S. Mani, M. Selner, D. Mowles, J. D. Young, J. A. Belt, C. R. Crawford, and C. E. Cass. 1998. Functional nucleoside transporters are required for gemcitabine influx and manifestation of toxicity in cancer cell lines. Cancer Res. 58:4349-4357. [PubMed] [Google Scholar]
- 31.Majumder, M., A. K. Ghosh, R. Steele, R. Ray, and R. B. Ray. 2001. Hepatitis C virus NS5A physically associates with p53 and regulates p21/waf1 gene expression in a p53-dependent manner. J. Virol. 75:1401-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McHutchison, J. G., S. C. Gordon, E. R. Schiff, M. L. Shiffman, W. M. Lee, V. K. Rustgi, Z. D. Goodman, M. H. Ling, S. Cort, and J. K. Albrecht. 1998. Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. Hepatitis Interventional Therapy Group. N. Engl. J. Med. 339:1485-1492. [DOI] [PubMed] [Google Scholar]
- 33.Moradpour, D., M. J. Evans, R. Gosert, Z. Yuan, H. E. Blum, S. P. Goff, B. D. Lindenbach, and C. M. Rice. 2004. Insertion of green fluorescent protein into nonstructural protein 5A allows direct visualization of functional hepatitis C virus replication complexes. J. Virol. 78:7400-7409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nousbaum, J., S. J. Polyak, S. C. Ray, D. G. Sullivan, A. M. Larson, R. L. Carithers, Jr., and D. R. Gretch. 2000. Prospective characterization of full-length hepatitis C virus NS5A quasispecies during induction and combination antiviral therapy. J. Virol. 74:9028-9038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park, K. J., S. H. Choi, S. Y. Lee, S. B. Hwang, and M. M. Lai. 2002. Nonstructural 5A protein of hepatitis C virus modulates tumor necrosis factor alpha-stimulated nuclear factor kappa B activation. J. Biol. Chem. 277:13122-13128. [DOI] [PubMed] [Google Scholar]
- 36.Patil, S. D., L. Y. Ngo, P. Glue, and J. D. Unadkat. 1998. Intestinal absorption of ribavirin is preferentially mediated by the Na+-nucleoside purine (N1) transporter. Pharm. Res. 15:950-952. [DOI] [PubMed] [Google Scholar]
- 37.Penin, F., J. Dubuisson, F. A. Rey, D. Moradpour, and J. M. Pawlotsky. 2004. Structural biology of hepatitis C virus. Hepatology 39:5-19. [DOI] [PubMed] [Google Scholar]
- 38.Pfeiffer, J. K., and K. Kirkegaard. 2003. A single mutation in poliovirus RNA-dependent RNA polymerase confers resistance to mutagenic nucleotide analogs via increased fidelity. Proc. Natl. Acad. Sci. USA 100:7289-7294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pincus, S. E., and E. Wimmer. 1986. Production of guanidine-resistant and -dependent poliovirus mutants from cloned cDNA: mutations in polypeptide 2C are directly responsible for altered guanidine sensitivity. J. Virol. 60:793-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ritzel, M. W., S. Y. Yao, M. Y. Huang, J. F. Elliott, C. E. Cass, and J. D. Young. 1997. Molecular cloning and functional expression of cDNAs encoding a human Na+-nucleoside cotransporter (hCNT1). Am. J. Physiol. 272:C707—C714. [DOI] [PubMed] [Google Scholar]
- 41.Sampath, J., M. Adachi, S. Hatse, L. Naesens, J. Balzarini, R. M. Flatley, L. H. Matherly, and J. D. Schuetz. 2002. Role of MRP4 and MRP5 in biology and chemotherapy. Am. Assoc. Pharmaceut. Sci. J. 4:E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shi, S. T., S. J. Polyak, H. Tu, D. R. Taylor, D. R. Gretch, and M. M. Lai. 2002. Hepatitis C virus NS5A colocalizes with the core protein on lipid droplets and interacts with apolipoproteins. Virology 292:198-210. [DOI] [PubMed] [Google Scholar]
- 43.Shimakami, T., M. Hijikata, H. Luo, Y. Y. Ma, S. Kaneko, K. Shimotohno, and S. Murakami. 2004. Effect of interaction between hepatitis C virus NS5A and NS5B on hepatitis C virus RNA replication with the hepatitis C virus replicon. J. Virol. 78:2738-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shirota, Y., H. Luo, W. Qin, S. Kaneko, T. Yamashita, K. Kobayashi, and S. Murakami. 2002. Hepatitis C virus (HCV) NS5A binds RNA-dependent RNA polymerase (RdRP) NS5B and modulates RNA-dependent RNA polymerase activity. J. Biol. Chem. 277:11149-11155. [DOI] [PubMed] [Google Scholar]
- 45.Street, A., A. Macdonald, K. Crowder, and M. Harris. 2004. The Hepatitis C virus NS5A protein activates a phosphoinositide 3-kinase-dependent survival signaling cascade. J. Biol. Chem. 279:12232-12241. [DOI] [PubMed] [Google Scholar]
- 46.Streeter, D. G., J. T. Witkowski, G. P. Khare, R. W. Sidwell, R. J. Bauer, R. K. Robins, and L. N. Simon. 1973. Mechanism of action of 1-D-ribofuranosyl-1,2,4-triazole-3-carboxamide (Virazole), a new broad-spectrum antiviral agent. Proc. Natl. Acad. Sci. USA 70:1174-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stuyver, L. J., T. R. McBrayer, P. M. Tharnish, A. E. Hassan, C. K. Chu, K. W. Pankiewicz, K. A. Watanabe, R. F. Schinazi, and M. J. Otto. 2003. Dynamics of subgenomic hepatitis C virus replicon RNA levels in Huh-7 cells after exposure to nucleoside antimetabolites. J. Virol. 77:10689-10694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taguchi, T., M. Nagano-Fujii, M. Akutsu, H. Kadoya, S. Ohgimoto, S. Ishido, and H. Hotta. 2004. Hepatitis C virus NS5A protein interacts with 2′,5′-oligoadenylate synthetase and inhibits antiviral activity of IFN in an IFN sensitivity-determining region-independent manner. J. Gen. Virol. 85:959-969. [DOI] [PubMed] [Google Scholar]
- 49.Tam, R. C., B. Pai, J. Bard, C. Lim, D. R. Averett, U. T. Phan, and T. Milovanovic. 1999. Ribavirin polarizes human T cell responses towards a Type 1 cytokine profile. J. Hepatol. 30:376-382. [DOI] [PubMed] [Google Scholar]
- 50.Tan, S. L., H. Nakao, Y. He, S. Vijaysri, P. Neddermann, B. L. Jacobs, B. J. Mayer, and M. G. Katze. 1999. NS5A, a nonstructural protein of hepatitis C virus, binds growth factor receptor-bound protein 2 adaptor protein in a Src homology 3 domain/ligand-dependent manner and perturbs mitogenic signaling. Proc. Natl. Acad. Sci. USA 96:5533-5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tanji, Y., T. Kaneko, S. Satoh, and K. Shimotohno. 1995. Phosphorylation of hepatitis C virus-encoded nonstructural protein NS5A. J. Virol. 69:3980-3986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tolskaya, E. A., L. I. Romanova, M. S. Kolesnikova, A. P. Gmyl, A. E. Gorbalenya, and V. I. Agol. 1994. Genetic studies on the poliovirus 2C protein, an NTPase. A plausible mechanism of guanidine effect on the 2C function and evidence for the importance of 2C oligomerization. J. Mol. Biol. 236:1310-1323. [DOI] [PubMed] [Google Scholar]
- 53.World Health Organization. 2000. Hepatitis C: global prevalence (update). Wkly. Epidemiol. Rec. 75:18-19. [PubMed] [Google Scholar]
- 54.Young, K. C., K. L. Lindsay, K. J. Lee, W. C. Liu, J. W. He, S. L. Milstein, and M. M. Lai. 2003. Identification of a ribavirin-resistant NS5B mutation of hepatitis C virus during ribavirin monotherapy. Hepatology 38:869-878. [DOI] [PubMed] [Google Scholar]
- 55.Zech, B., A. Kurtenbach, N. Krieger, D. Strand, S. Blencke, M. Morbitzer, K. Salassidis, M. Cotten, J. Wissing, S. Obert, R. Bartenschlager, T. Herget, and H. Daub. 2003. Identification and characterization of amphiphysin II as a novel cellular interaction partner of the hepatitis C virus NS5A protein. J. Gen. Virol. 84:555-560. [DOI] [PubMed] [Google Scholar]
- 56.Zhou, S., R. Liu, B. M. Baroudy, B. A. Malcolm, and G. R. Reyes. 2003. The effect of ribavirin and IMPDH inhibitors on hepatitis C virus subgenomic replicon RNA. Virology 310:333-342. [DOI] [PubMed] [Google Scholar]
- 57.Zhu, Q., J. T. Guo, and C. Seeger. 2003. Replication of hepatitis C virus subgenomes in nonhepatic epithelial and mouse hepatoma cells. J. Virol. 77:9204-9210. [DOI] [PMC free article] [PubMed] [Google Scholar]