Abstract
The purpose of the present study was to test if one bout of moderate exercise performed in either the fasted or the postprandial state affects glucose values measured over 22 hours. Twelve participants diagnosed with hyperglycemia not using antidiabetic medications underwent 3 test days in a randomized cross-over design encompassing one test day without exercise, one test day with 60 min of treadmill walking prior to breakfast, and one test day with an identical bout of exercise 30 min after the start of breakfast. Continuous glucose monitoring was performed until the next morning (>22 hours). There was no significant effect of type of test day on the area under the glucose curve for the entire 22 hours period (p = 0.111). None of the exercise interventions had a significant effect on the area under the glucose curve after breakfast, lunch or dinner. However, the postprandial exercise bout tended to decrease the area under the glucose curve after the evening meal compared to the fasted exercise bout (24.2 ± 6.2 vs. 27.6 ± 6.0 mmol·hour·L-1, p = 0.031). Furthermore, the postprandial exercise decreased the mean of the 10 highest glucose values measured in each individual (8.6 ± 1.9 mmol·L-1) over 22 hours compared to both the control day (9.3 ± 2.1 mmol.L-1) and the day with fasted exercise (9.6 ± 1.7 mmol·L-1, p = 0.012 and 0.009 respectively). Postprandial exercise also decreased the glycemic variability compared to the control day (1.22 ± 0.49 vs. 1.58 ± 0.52 mmol·L-1, p = 0.015). We conclude that performing moderate exercise in the postprandial state after breakfast, but not in the fasted state, decreases glucose excursions during the subsequent 22 hours period in hyperglycemic individuals not using antidiabetic medications.
Key points.
Persons with postprandial hyperglycemia are at increased risk for cardiovascular disease.
Performing moderate exercise in the postprandial state but not post-absorptive state decreases peak postprandial glucose values acutely.
Performing moderate exercise in the postprandial state but not post-absorptive state decreases glycemic variability acutely.
Key words: Blood glucose, physical activity, carbohydrate, walking, continuous glucose monitoring
Introduction
People with hyperglycemia have increased risk for cardiovascular disease and death (DECODE, 2003; Nakagami et al., 2006; Niskanen et al., 1998). In particular, the magnitude of postprandial glycemia seems to be more associated with vascular complications than fasting blood glucose levels (Cavalot et al., 2011; DECODE, 1999; DECODE, 2001; Sasso et al., 2004; Temelkova-Kurktschiev et al., 2000). This association shows no threshold level and starts well below diabetic glucose levels (Coutinho et al., 1999; DECODE, 2003; Levitan et al., 2004). Intermittent elevations in glucose levels do promote oxidative stress, an underlying mechanism of vascular damage (Hirsch and Brownlee, 2005; Monnier and Colette, 2008; Standl et al., 2011). There is also some evidence that intermittent high glucose concentrations and “glycemic spikes” inflict more damage to endothelial cells than constantly elevated glucose levels (Quagliaro et al., 2003; Risso et al., 2001).
Exercise performed in the postprandial state has the ability to blunt postprandial glycemia acutely (Aadland and Høstmark, 2008; Caron et al., 1982; Colberg et al., 2014; Colberg et al., 2009; Dipietro et al., 2013; Dunstan et al., 2012; Hashimoto et al., 2013; Hostmark et al., 2006; Larsen et al., 1997; Larsen et al., 1999; Lunde et al., 2012; Nelson et al., 1982; Nygaard et al., 2009; van Dijk et al., 2013b), even when the exercise is performed at very light intensities and in small doses (Aadland and Høstmark, 2008; Bailey and Locke, 2015; Dipietro et al., 2013; Dunstan et al., 2012; Lunde et al., 2012; Nygaard et al., 2009; van Dijk et al., 2013b). Some studies have compared the effect of exercise in the fasted state with exercise in the postprandial state on blood glucose levels in persons with metabolic syndrome and diabetes. The results indicate that exercise in the fasted state does not affect consecutive postprandial glycemia, in contrast to postprandial exercise (Colberg et al., 2009; Derave et al., 2007; Peddie et al., 2013). Notably, venous blood samples were used to determine glucose levels in those studies, and the sampling was limited to the first 4 – 10 hours after exercise. Lately, devices for continuous glucose monitoring have become commercially available, making it feasible to monitor glucose for longer durations, both day and night, compared to venous blood sampling. Therefore we used continuous glucose monitoring to test the hypothesis that; I) Moderate exercise performed in the fasted or in the postprandial state affects glucose values over 22 hours, in persons diagnosed with hyperglycemia. II) These two different timings of exercise affect glucose values different from each other.
Methods
Participants
Four women and 8 men of European origin completed the study and are included in the results. Characteristics of the participants are summarized in Table 1. Inclusion were restricted to individuals diagnosed with hyperglycemia, i.e. previously measured fasting venous plasma glucose ≥6.1 mmol·L-1 and/or 2 hour glucose tolerance ≥7.8 mmol·L-1, and who did not use glucose lowering medications. Four of the participants were diagnosed with type 2 diabetes. They had a mean glucose value of 7.4 ± 1.4 mmol·L-1 during the control condition while the eight without known diabetes had a value of 6.1 ± 0.9 mmol·L-1. Metabolic disorders, other than diabetes, were set as exclusion criteria. We excluded one participant. She was included based on self-reported hyperglycemia. However, an examination of her patient journal after enrollment showed that she did not meet the inclusion criteria. The participants did not have other diseases that directly affected blood glucose. Some of the participants used hypolipidemic (n = 4), antithrombotic (n = 4), angiotensin II receptor antagonists (n = 2) and ACE inhibitors (n = 1) agents, but dosage and timing of intake were kept stable during the study period. The median time from diagnosis of hyperglycemia to study participation was 8.5 months (IQR: 3-34 months). Seven of the participants had at least one parent or one sibling with diabetes. All women were postmenopausal. The participants reported that they had performed (mean ± SD): 219 ± 237 min of endurance or strength training, 177 ± 143 min of walking and 122 ± 49 min of lighter activity (like gardening and housework) per week for the last three months prior to study enrollment. To obtain a general impression of the dietary habits of the participants prior to the study, they answered a questionnaire. Eleven preferred wholegrain bread to non-wholegrain or semi-wholegrain bread, while one did not eat bread. When asked about how many times per week they ate a selection of specified types of food, answers were as follows (mean ± SD): sugar-containing jam or chocolate spread, 0 ± 0; sugar-rich beverages, 0.04 ± 0.01; candy / chocolate / snacks, 1.4 ± 1.2; boiled food, 3.5 ± 1.6; pan fried food, 2.7 ± 1.4; deep-fried food, 0.1 ± 0.3; fruit and vegetables, 16.6 ± 9.0.
Table 1.
Characteristics of the participants (n = 12). Data are means (±SD).
| Age (yr) | 65 (8 |
| Body weight (kg) | 73.3 (9.7) |
| Height (m) | 1.73 (.08) |
| Body mass index (kg.m-2) | 24.5 (1.9) |
| HbA1c (%) | 6.1 (.6) |
| Total cholesterol (mmol.L-1) | 5.1 (1.3) |
| HDL cholesterol (mmol.L-1) | 1.4 (.6) |
| LDL cholesterol (mmol.L-1) | 3.0 (1.0) |
| Systolic blood pressure (mmHg) | 133(18) |
| Diastolic blood pressure (mmHg) | 74(6) |
Ethics statement
The study was conformed to the Declaration of Helsinki and was approved by The Regional Ethics Committee (REK Sør-Øst, Norway). All participants gave their written informed consent prior to enrollment.
General design
The study was performed using a randomized crossover design. Each subject undertook three test days (Figure 1) in a balanced order, separated by at least six days and no more than 21 days: one test day with a bout of exercise in the fasted state before breakfast (ExBr), one test day with similar exercise in the postprandial state after breakfast (BrEx), and one test day without physical exercise (CON). Except for the different exercise regimes, participants remained sedentary, and each experimental day was identical, with a standardized diet. All test days started in the morning, with average onset of experiments one hour earlier and average onset of breakfast 30 min later for ExBr compared to CON and BrEx. For each participant, onset of breakfast was within the same hour. Continuous glucose measurement was performed for at least 22 hours after breakfast.
Figure 1.
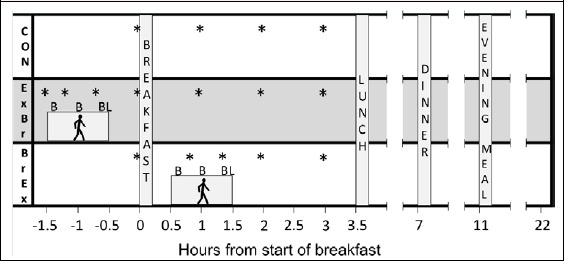
Overview of the test protocol. Continuous glucose monitoring was performed during the 22 hour period of each of the three test days; The control day (CON) in the upper row, the day with exercise in the fasted state (ExBr) in the middle row and the day with exercise in the postprandial state (BrEx) in the bottom row. * = Measure of heart rate, oxygen consumption and respiratory exchange ratio (RER) values. B = Measure of perceived exertion (Borg scale). L = measure of blood lactate.
Standardization of exercise and nutrition
All participants remained in the laboratory facility until the lunch meal was ingested, whereupon the participants were transported home, and stayed home for the remaining time of the 22 hours glucose-monitoring period. They had a checklist with all details concerning the standardization of the experiments, including instructions about timing and amount of food intake. Prior to the first test day, each participant was given a detailed lesson about the importance of experimental standardization, and all procedures necessary for exact standardization. At the end of each test day, we asked the participants to comment on the standardization. No diverges was reported.
The participants were instructed to avoid exercise during the last three days prior to each test day. Any light activity performed on these days prior to the first test day, were recorded and repeated in the same manner before the second and third test day. The exercise sessions in both ExBr and BrEx consisted of 60 min of treadmill walking at an individually standardized speed at 8% inclination. Speed was set at an familiarization session >6 days before the first test, defined as the speed corresponding to 12 at the Borg 6-20 rate of perceived exertion scale (Borg, 1982) after 30 min of walking at 8% inclination. All other physical activity was limited to what was absolute necessary, like walking to the car and moving between living room, toilet, kitchen and bedroom.
We instructed the participants to standardize their diet during the three-day period prior to each test, by writing down food intake leading up to the first test day and repeat this regimen as close as possible on the second and third test day. Absolute dietary standardization was performed on test days, starting 10 hours before breakfast, and lasting until 22 hours after breakfast. Macronutrient intakes from this period are given in Table 2. A digital kitchen scale and a food diary were used to carefully register each meal during the first test day and to repeat the diet on the second and third test day. In the evening 10 hours preceding breakfast, they ate and registered a self-chosen meal containing >30 g carbohydrate. For breakfast, participants ingested 250 ml semi-skimmed milk and cornflakes corresponding to 1g carbohydrate per kg body weight. Lunch (3.5 hours after start of breakfast) contained a yogurt and self-chosen amounts of wholegrain crispbread, butter, cheese and water. For dinner (7 hours after start of breakfast) the participants could choose between several boil in bag dinner packages (salmon with rice and vegetables, chicken casserole, meatballs potatoes and creamed peas or minced steak with stewed cabbage and potatoes; Fjordland AS, Norway). Leftovers were registered on test day one and the corresponding amount of food was removed on the second and third test. The evening meal (11 hours after start of breakfast) consisted of a self-chosen amount of whole meal bread, butter, cheese and skimmed milk. The research team provided subjects with food for breakfast, lunch, dinner and the evening meal on test days.
Table 2.
Macronutrient intake before and during test days. Data are means (±SD).
| kcal | Protein, g | Fat, g | Carbohydrate, g | |
|---|---|---|---|---|
| Evening meal 10 hours before breakfast | 328(231) | 12(6) | 10(4) | 43(27) |
| Breakfast | 380(48) | 13(2) | 3(1) | 74(9) |
| Lunch | 502(197) | 28(14) | 19(10) | 52(19) |
| Dinner | 606(194) | 37(17) | 27(10) | 51(17) |
| Evening meal | 630(234) | 30(8) | 29(12) | 59(33) |
| Total test day (from breakfast) | 2117(450) | 108(33) | 77(22) | 235(47) |
Data sampling
Interstitial glucose was monitored by a Continuous glucose monitoring system, consisting of a sensor (Enlite Glucose Sensor MMT-7008A, Medtronic MiniMed, Northridge, USA) and a recorder (iPro2 MMT-7745WW, Medtronic MiniMed, Northridge, USA) attached to the sensor. The recorder stores mean glucose values every 5th minute. We attached the sensor and the recorder to the skin at the anterior abdominal area lateral to the periumbilical region. The participants were given a glucose meter (Contour XT, Bayer Consumer Care AG, Basel, Switzerland) and were instructed in capillary blood sampling, for determination of capillary blood glucose at baseline, and before the meals at 3.5, 11 and also 22 hours after breakfast. These measurements were done in triplicates at each time point. We downloaded data from the continuous glucose recorder to the accompanying software and calibrated the data by the averages of the capillary blood glucose recordings, before exporting data into Microsoft Excel.
In order to test the validity of the continuous glucose monitoring system, we used venous blood sampled 2.5 hours after breakfast. The venous blood was analyzed for glucose by Furst Medical Laboratories, with Advia 2400 Chemistry system, Siemens Healthcare Diagnostics Inc. Mean plasma venous blood glucose for all 2.5 hour samples was 7.3 ± 2.3 mmol·L-1, while the corresponding continuous glucose monitoring value were 7.2 ± 2.0 mmol·L-1. Coefficient of variation between continuous glucose monitoring and venous blood samples was 7.3%. However, fluctuations in glucose entails a delay between blood glucose and interstitial glucose (Rossetti et al., 2010) that may add inaccuracy to this validation.
We sampled oxygen consumption, respiratory exchange ratio (Oxycon Pro, Erich Jaeger, Hoechberg, Germany) and heart rate for 10 min at several standardized time points until 3 hours after breakfast (Figure 1). Mean values from the last 2 min of sampling were used for analysis. Blood lactate concentration (Biosen C-line, EKF-diagnostic GmbH, Germany) was measured 55 min into each bout of exercise and rate of perceived exertion was reported 5, 30 and 55 min into the exercise bouts with Borg’s 6-20 scale (Borg, 1982).
Calculations and statistical analysis
Aerobic metabolism and carbohydrate and fat oxidation were calculated from oxygen consumption and respiratory exchange ratio values using a table given in McArdle, Katch and Katch textbook of exercise physiology (p. 188) (2010). Area under the glucose curve (AUC) were calculated for the postprandial periods after meals, according to the trapezium rule (Matthews et al., 1990). To further describe the distribution of glucose values, we report percent time spent at glucose values ≥7.8 mmol·L-1, ≥5.6 mmol·L-1 and ≤3.3 mmol·L-1, during each test day. As an indicator of the magnitude of the glycemic spikes, we calculated the mean of the 10 highest glucose values on each test day, independent of when these values were observed. A mean score were calculated, as this was considered more reliable than single data points from the continuous measurement system. In addition, each test day contained four postprandial periods, and the mean of the 10 highest glucose values therefore reflect total glycemic stress better than a single peak value. We assessed glucose variability with calculation of continuous overall net glycemic action (CONGA) (McDonnell et al., 2005). CONGA reflects the magnitude of glucose fluctuations. It is the SD of the differences between each glucose reading and the glucose reading n hours later. We used n = 2 hours (CONGA2) and n = 4 hours (CONGA4).
We calculated effect sizes (ES) for the effect of intervention and between interventions by using Cohen`s dz (Lakens, 2013). Effect sizes were interpreted according to Hopkins et al. (Hopkins et al., 2009): d>0.2=small effect, d>0.6=moderate effect, d>1.2=large effect. We did the statistical analysis with IBM SPSS statistics, version 22.0. All comparisons between test days were performed with a linear mixed model. Participant number was utilized as the repeated “subjects” variable and test day as a fixed factor. Random intercept was included in the model. We checked the residuals for normality and homogeneity. The variable “time at glucose ≥7.8 mmol·L-1” was skewed and we therefore utilized Friedman Test to compare all test days and the Wilcoxon Sign Rank Test for pairwise com parisons. The α-level was set at 0.05 and a p value <0.1 was considered as a tendency towards statistical significance. For pairwise comparisons, we used p ≤ 0.017 and p < 0.034 due to Bonferroni correction. Data are presented as means ± SD unless median ± interquartile range (IQR) are stated. We produced the figures in SigmaPlot 12.0, Systat Software Inc.
Results
There were no differences in baseline values for heart rate, aerobic metabolism, carbohydrate oxidation or fat oxidation between the three test days (Table 3). The exercise bout of ExBr was accompanied by lower heart rate (p = 0.026), a tendency towards lower aerobic metabolism (p = 0.073), lower carbohydrate oxidation (p < 0.001) and higher fat oxidation (p = 0.006) compared to BrEx (Figure 2). Rate of perceived exertion was lower during the ExBr than the BrEx exercise bout (12.0 ± 0.9 vs 12.4 ± 0.9 on Borg RPE, p = 0.021), and the lactate value at the end of exercise was lower after the ExBr bout than the BrEx bout (1.4 ± 0.8 vs 1.7 ± 0.8 mmol·L-1, p = 0.038). ExBr exhibited higher carbohydrate oxidation (p = 0.017) and lower fat oxidation (p=0.029) than ExBr 120 min after breakfast (Figure 2).
Table 3.
Baseline values. Data are means (±SD).
| CON | ExBr | BrEx | p | |
|---|---|---|---|---|
| Heart rate, beats/min | 58(7) | 55(7) | 55(8) | .151 |
| Aerobic metabolism, kcal/min | 1.05 (.17) | 0.91 (.19) | 0.96 (.29) | .146 |
| Carbohydrate oxidation, g/min | .08 (.07) | .06 (.08) | .08 (.07) | .637 |
| Fat oxidation, g/min | .08 (.03) | .07 (.03) | .06 (.04) | .332 |
Mean baseline values of heart rate, aerobic metabolism, carbohydrate oxidation and fat oxidation from the control day without exercise (CON), the day with exercise before breakfast (ExBr) and the day with exercise after breakfast (BrEx).
Figure 2.
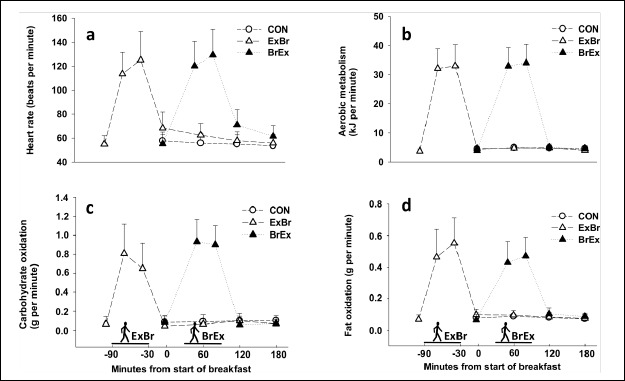
Heart rate and metabolism during and after exercise. Heart rate (A), total aerobic metabolism (B), carbohydrate oxidation (C) and fat oxidation (D) prior to lunch on the three test days; The control day (CON), the day with exercise in the fasted state (ExBr) and the day with exercise in the postprandial state (BrEx).
The results of the continuous glucose monitoring are shown in Figure 3. Mean values for the entire 22 hours test period were 6.5 ± 1.2 mmol·L-1 for CON, 6.8 ± 1.2 mmol·L-1 for ExBr and 6.5 ± 1.3 mmol·L-1 for BrEx. The AUCs for the entire 22 hours period did not differ significantly between test days (CON; 142.9 ± 26.5, ExBr; 150.1 ± 26.6, BrEx; 142.1 ± 27.9 mmol·hour·L-1, p = 0.115). The effect of intervention was small for ExBr (ES = 0.5, vs CON), trivial for BrEx (ES = 0.1, vs CON), while the effect of the difference between ExBr and BrEx was moderate (ES = 0.6). Median time with glucose values ≥7.8 mmol.L-1 differed between test days (CON; 16 ± IQR 18%, ExBr; 21 ± IQR 20, BrEx; 5 ± IQR 22% of time, p = 0.012), but the significant difference disappeared in pairwise analysis between test days. Time with glucose values ≥5.6 mmol·L-1 (CON; 71 ± 27%, ExBr; 77 ± 26%, BrEx; 72 ± 30%), and ≤3.3 mmol·L-1 (CON; 1 ± 2%, ExBr; 0 ± 0%, BrEx; 2 ± 6%) did not differ significantly between test days (p = 0.535 and 0.430 respectively).
Figure 3.
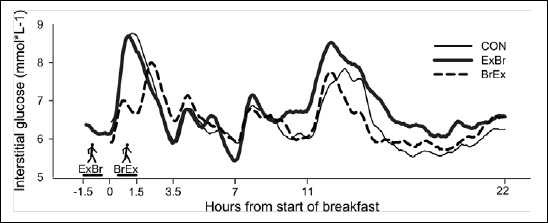
Results from the continuous glucose monitoring. Glucose curves for the entire test period of the three test days; The control day (CON), the day with exercise in the fasted state (ExBr) and the day with exercise in the postprandial state (BrEx).
For the postprandial period after breakfast, defined as 3.5 hours from start of breakfast, there was no effect of type of test day on glucose AUC (p = 0.259). However, there was an effect of test day on glucose AUC measured between 30 and 90 min after breakfast, corresponding to the BrEx exercise period (p = 0.002). This was confirmed by pairwise tests, showing that the glucose AUC differed between CON and BrEx (8.5 ± 2.0 vs. 6.8 ± 1.8 mmol·hour·L-1, p= 0.003) and between ExBr and BrEx (8.4 ± 1.8 vs. 6.8 ± 1.8 mmol·hour·L-1, p = 0.017). There was no significant effect of type of test day on glucose AUC measured between 90 and 210 min after breakfast, corresponding to the period between the BrEx exercise and lunch, p = 0.750).
For the postprandial periods after lunch and dinner (3.5 hours from start of each meal), there was no effect of type of test day on glucose AUC (p = 0.641 and p = 0.691 respectively).
There was an effect of test day on glucose AUC measured in the postprandial period after the evening meal (3.5 hours from start of the meal) (p = 0.037). Pairwise comparisons showed that glucose AUC in BrEx tended to be lower than in ExBr (24.2 ± 6.2 vs. 27.6 ± 6.0 mmol·hour·L-1, p = 0.031), while there was no significant difference between BrEx or ExBr and CON. In the post-absorptive period during the subsequent night and morning (7.5 hours), there was no significant effect of type of test day.
There was an effect of test day on the mean of the 10 highest glucose values measured for each individual (p = 0.016). This was confirmed by pairwise tests, showing a difference between CON and BrEx (9.3 ± 2.1 vs. 8.6 ± 1.9 mmol·L-1, p= 0.012) and between ExBr and BrEx (9.6 ± 1.7 vs. 8.6 ± 1.9 mmol·L-1, p = 0.009), but not between CON and ExBr. The effect of intervention was small for ExBr (ES = 0.2, vs CON), moderate for BrEx (ES = 0.7, vs CON), while the effect of the difference between ExBr and BrEx was moderate (ES = 0.8).
The results of the glycemic variability calculations are presented in Figure 4. There was a tendency towards an effect of test day on CONGA2 (p = 0.096), while there was a significant effect of test day on CONGA4 (p = 0.031). Pairwise comparisons of CONGA4 values revealed that the glycemic variability was larger in CON than in BrEx (1.58 ± 0.52 vs. 1.22 ± 0.49 mmol·L-1, p = 0.015), with no significant difference being found between CON and ExBr or ExBr and BrEx. The effect of intervention on CONGA2 was small for ExBr (ES = 0.2, vs CON), moderate for BrEx (ES = 0.8, vs CON), while the effect of the difference between ExBr and BrEx was small (ES = 0.4). The effect of intervention on CONGA4 was trivial for ExBr (ES = 0.0, vs CON), moderate for BrEx (ES = 0.8, vs CON), while the effect of the difference between ExBr and BrEx was moderate (ES = 0.7).
Figure 4.
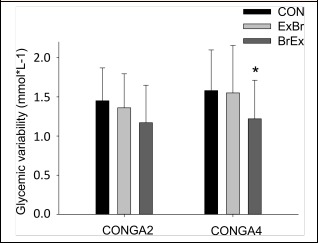
Glycemic variability measured as CONGA scores. CONGA2 and CONGA4 is the SD of the difference between each glucose reading and the glucose reading 2 (CONGA2) and 4 (CONGA4) hours later. * p < 0.017 vs CON.
The magnitude of the AUC, highest glucose values and CONGA scores from CON did not correlate significantly with the changes in AUCs, highest glucose values and CONGA scores as a result of ExBr and BrEx. The magnitude of the AUC for the postprandial period after breakfast (3.5 hours from start of the breakfast) in CON correlated negatively to the changes in the corresponding breakfast AUCs as a result of BrEx (r = -0.738, p = 0.006) and ExBr (r = -0.624, p = 0.030).
Discussion
The main finding was that BrEx attenuated glucose excursions during the subsequent 22 hours compared to CON and ExBr. This improvement in glycemia when activity was performed after breakfast was manifested as a decrease in the mean of the 10 highest glucose values during the entire 22 hours period compared to CON and ExBr, as well as a decrease in glycemic variability, compared to CON. BrEx also tended to decrease glucose AUC after the evening meal compared to ExBr.
These results confirms that exercise in the postprandial phase leads to acutely decreased postprandial glycemia, as observed in several studies using blood glucose as the outcome variable (Aadland and Høstmark, 2008; Caron et al., 1982; Colberg et al., 2014; Colberg et al., 2009; Dunstan et al., 2012; Hashimoto et al., 2013; Hostmark et al., 2006; Larsen et al., 1997; Larsen et al., 1999; Lunde et al., 2012; Nelson et al., 1982; Nygaard et al., 2009) and studies using interstitial glucose as outcome variable (Dipietro et al., 2013; van Dijk et al., 2013b). Our findings also corroborate previous studies directly comparing fasted and postprandial exercise (Colberg et al., 2009; Derave et al., 2007). The findings that postprandial but not fasted exercise reduces glucose peak values and glycemic variability are however novel. Furthermore, while the previous studies that directly compared fasted and postprandial exercise (Colberg et al., 2009; Derave et al., 2007) were limited by the duration of the sampling periods, our results indicat that postprandial exercise might decrease postprandial glycemia several hours after exercise.
In contrast to the results of the present study, a very recent study by Terada et al. (2016) found fasted exercise to be more efficient at lowering postprandial glycemia than postprandial exercise. The exercise intervention in Terada et al. (2016) was very similar to the one utilized in the present study, and the conflicting results are therefore surprising. One might speculate if the different observations result from different metabolic states of the participants or from minor differences in the study design. The onset of the postprandial exercise bout in the study of Terada et al. (2016) appears to have been after peak postprandial glucose concentration. The postprandial physical exercise bout in the present study started 30 min after onset of breakfast. This timing has been suggested to be ideal for lowering postprandial glycemia in diabetic persons, due to a high insulin-to-glucagon ratio at this point. A high insulin-to-glucagon ratio will in turn inhibit the counter regulatory increase in hepatic glucose output occurring when exercise is done in other dietary phases (Chacko, 2014), like the fasted exercise in the present study. Indeed, in a free-living condition, the exercise-mediated decreases in blood glucose are expected to be largest if the exercise takes place when glucose levels is at its highest (Gaudet-Savard et al., 2007). The exact timing of the onset of postprandial exercise could therefore be important, at least for the glycemic changes in the postprandial period when exercise is performed. Favorable effects of fasted exercise were also observed in a study by Borer et al. (2009). However, that study was performed with healthy subjects, using a comprehensive exercise protocol aiming to deplete glycogen stores, arguably representing a different physiological scenario. In the present study, carbohydrate oxidation was higher 120 min after breakfast in ExBr compared to BrEx, indicating that glycogen depletion had not occurred (Devlin and Horton, 1985; Mikines et al., 1988b).
Despite the observed decrease in postprandial glucose during the BrEx exercise bout, the glucose AUC of the entire postprandial period after breakfast was not significantly different between test days. This result does depend on the definition of the length on the “postprandial period analyzed”. Nevertheless, to our knowledge the present study is the first on hyperglycemic participants that does not report decreased glycemia in the postprandial period when exercise is performed (defined as 3.5 hours from start of breakfast). Surprisingly, peak glucose values after breakfast were only slightly higher in this study with hyperglycemic participants compared to a previous study with healthy women above 50 years, ingesting the same breakfast meal (Nygaard et al., 2009). Lower glycemic excursions than expected may have entailed a type 2 error, since the attenuating effect on postprandial glycemia after breakfast of postprandial exercise is likely to be enforced with increased level of glycemia (Gaudet-Savard et al., 2007; Lunde et al., 2012; Nygaard et al., 2009). This is also confirmed in the present study, since the persons with highest glucose AUCs after breakfast in CON had the largest decreases in breakfast AUCs as a result of both ExBr and BrEx compared to CON. Therefore, the results may not be generalized to persons with severe hyperglycemia, where one in general would expect a larger effect of exercise on blood glucose (Aadland and Høstmark, 2008; Church et al., 2010; Hordern et al., 2008; Mikines et al., 1988a; Nygaard et al., 2009; Snowling and Hopkins, 2006; Van Dijk et al., 2013a; Walker et al., 1999). However, the magnitude of the AUC, highest glucose values and CONGA scores for the entire 22 hours period of CON did not correlate significantly with the corresponding changes in AUCs, highest glucose values and CONGA scores as a result of ExBr and BrEx. Nevertheless, with regard to the activity level and the dietary habits reported by the participants (e.g. the low intake of sugar), the results may have been affected by a selection bias, and the possibility that these participants differ from most hyperglycemic individuals (Khunti et al., 2008).
The lack of significant difference in postprandial glycemia after breakfast also appears to be a result of a rebound increase in glucose concentration after the BrEx exercise bout, though not significant. Such rebound increases in glucose values is typical for exercise in the carbohydrate fed state. One plausible mechanism is increased hepatic glucose output as a result of exercise (Gonzalez, 2014). A decrease in postprandial glycemia during exercise and a subsequent increase after exercise could theoretically also be a result of an exercise mediated delay in digestion. This is likely not the case, since exercise does not delay rate of absorption of glucose from the intestine (Karstoft et al., 2014), at least not at a moderate exercise intensity (Lang et al., 2006), nor is rate of gastric emptying reduced by walking (Moore et al., 1990). Hence, the reduction in glucose observed during the BrEx exercise bout is likely a result of changes in energy metabolism, due to a ~8 fold increase in energy expenditure and a shift from fat to carbohydrate metabolism during exercise.
The intention of the present study was to investigate the effect of a moderate load of exercise, feasible for most people, which could be generalized into everyday life of hyperglycemic individuals with some motivation for exercise. However, the relative low intensity and the limited length of the activity may also have contributed to the lack of a more pronounced effect. Several studies have indicated a dose-response relationship between the amount of energy expended during exercise and the effect on glycemia. (Bailey and Locke, 2015; Colberg et al., 2014; Nygaard et al., 2009; van Dijk et al., 2013b). Moreover, exercise at high intensities seem to have more pronounced effect on glycemia than isoenergetic exercise at lower intensities (Little et al. 2014; Terada et al. 2016). It is therefore plausible that a larger dose of exercise and / or higher intensity would have entailed larger effects. However, experiments with low amounts of exercise have also shown acute effects on postprandial glycemia when exercise was performed post-meal (Bailey and Locke, 2015; Colberg et al., 2009; Gillen et al., 2012; Little et al., 2014; Nygaard et al., 2009; Peddie et al., 2013; van Dijk et al., 2013b). Another methodological aspect that can be discussed is the one hour earlier onset of experiment and 30 min later breakfast in ExBr compared to CON and BrEx. We cannot exclude that these systematic differences have affected the results via altered waking time, circadian rhythm and / or glucose tolerance (Scheen and Van Cauter, 1988; Jarrett et al., 1972), although the time lags cannot be described as large.
There was a tendency towards a delayed effect of BrEx compared to ExBr on glucose AUC in the evening, several hours after exercise. The degree of carbohydrate availability during exercise affects the relative expression of fat-promoting and carbohydrate-promoting genes in the metabolism (Civitarese et al., 2005). This may have led to a shift in metabolic protein abundance and / or activity, which may have influenced blood glucose several hours after the exercise. The lack of such an effect after the earlier lunch and dinner meals may be related to slow and time-demanding change in protein activity or to the fact that the glycemic load was higher in the evening meal, making a larger decrease possible (Gaudet-Savard et al. 2007; Høstmark, 2007; Lunde et al., 2012; Nygaard et al. 2009).
It seems likely that the improvement in glycemic variability during BrEx was a result of lower glucose excursions, since this intervention also reduced the mean of the ten highest glucose values. This is also supported by the numerical value of time spent ≥7.8 mmol.L-1, ≥5.6 mmol·L-1 and ≤3.3 mmol·L-1 that indicate that BrEx blunted the peaks more than the nadirs. A lower but longer postprandial increment after breakfast might also have contributed to the improvement in glycemic variability during BrEx. All together, the results show that postprandial exercise has the ability to blunt postprandial glucose excursions and decrease glycemic variability, two outcomes that is related to each other. Since these glycemic parameters are associated with endothelial dysfunction (Hirsch and Brownlee, 2005; Monnier and Colette, 2008; Quagliaro et al., 2003; Risso et al., 2001; Standl et al., 2011) postprandial exercise may be a strategy to prevent metabolic diseases and promote general health in hyperglycemic persons not using antidiabetics. However, behaviors that entails the largest acute effects are not necessarily effective habits to promote health over time. Consequently, the question of whether regularly performing post meal moderate exercise can decrease the risk of cardiovascular disease and hyperglycemia is still unanswered and the practical implications of the present study should be interpreted with caution. While we found a moderate positive effect of postprandial exercise on acute glucose regulation, other studies have found other physiological effects of fasted but not postprandial exercise that may improve hyperglycemia in the long term. Excess accumulation of intramyocellular lipids, which is associated with diabetes (Pan et al., 1997), is lowered more after exercise in the fasted state than after postprandial exercise or exercise accompanied with carbohydrate intake (De Bock et al., 2005; Van Proeyen et al., 2010). Future studies on fasted and / or postprandial exercise should therefore focus on long term effects. Furthermore, future studies of fasted and postprandial exercise should pay attention to markers of cardiovascular health in addition to glucose per se. Based on the present study, one might hypothesize that postprandial exercise exerts advantageous effects on markers of cardiovascular health compared to fasted exercise.
Conclusion
Performing moderate exercise in the postprandial state, but not fasted state, decreases glucose excursions during a subsequent 22 hours period in hyperglycemic individuals not using antidiabetic medications.
Acknowledgment
We are grateful to Tine AS and Fjordland AS for supplying us with food for dietary standardization. A special thanks to Kathrine Kroken and Olav Andreas Tuterud Nordølum for their contribution to the data sampling. The experiments comply with the current laws of the country in which they were performed. The authors have no conflict of interest to declare.
Biographies
Håvard NYGAARD
Employment
Department of Sport Science, Lillehammer University College, Lillehammer, Norway
Degree
MSc, PhD student
Research interests
Exercise physiology, preventive medicine
E-mail: havard.nygaard@inn.no

Bent Ronny RØNNESTAD
Employment
Department of Sport Science, Lillehammer University College, Lillehammer, Norway
Degree
PhD
Research interests
Endurance training, strength training, endurance performance, exercise physiology, cycling performance, concurrent strength and endurance training, training periodization
E-mail: bent.ronnestad@inn.no

Daniel HAMMARSTRÖM
Employment
Department of Sport Science, Lillehammer Univ. College, Lillehammer, Norway
Degree
MSc, PhD student
Research interests
Exercise training, muscle physiology and human performance.
E-mail: daniel.hammarstrom@inn.no

Gerd HOLMBOE-OTTESEN
Employment
Senior prof. in nutrition, Institute of Health and Society, Department of Community Medicine, Univ. of Oslo, Norway
Degree
MSc, PhD
Research interest
Dietary impact on BMI/nutritional status, Metabolic Syndrome and Diabetes. Effect of lifestyle intervention (dietary change and increased physical activity) on BMI and indicators of metabolic syndrome. Ethnic differences in overweight/obesity and lifestyle factors. Community/international nutrition, nutrition epidemiology.
E-mail:
gerd.holmboe-ottesen@medisin.uio.no

Arne Torbjørn HØSTMARK
Employment
Senior professor, Institute of Health and Society, Department of Community Medicine, University of Oslo, Norway
Degree
PhD, MD
Research interests
Preventive medicine, nutrition physiology, endocrinology, carbohydrate and lipid metabolism, lipoproteins and glucose in relation to nutrition and physical activity, diabetes in immigrants.
E-mail: a.t.hostmark@medisin.uio.no
References
- Aadland E., Høstmark A.T. (2008) Very light Physical Activity after a Meal Blunts the Rise in Blood Glucose and Insulin. The Open Nutrition Journal 2, 94-99. [Google Scholar]
- Bailey D.P., Locke C.D. (2015) Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. Journal of Science and Medicine in Sport 18, 294-298. [DOI] [PubMed] [Google Scholar]
- Borer K.T., Wuorinen E.C., Lukos J.R., Denver J.W., Porges S.W., Burant C.F. (2009) Two bouts of exercise before meals, but not after meals, lower fasting blood glucose. Medicine & Science in Sports & Exercise 41, 1606-1614. [DOI] [PubMed] [Google Scholar]
- Borg G.A. (1982) Psychophysical bases of perceived exertion. Medicine & Science in Sports & Exercise 14, 377-381. [PubMed] [Google Scholar]
- Caron D., Poussier P., Marliss E.B., Zinman B. (1982) The effect of postprandial exercise on meal-related glucose intolerance in insulin-dependent diabetic individuals. Diabetes Care 5, 364-369. [DOI] [PubMed] [Google Scholar]
- Cavalot F., Pagliarino A., Valle M., Di Martino L., Bonomo K., Massucco P., Anfossi G., Trovati M. (2011) Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a 14-year follow-up: lessons from the San Luigi Gonzaga Diabetes Study. Diabetes Care 34, 2237-2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chacko E. (2014) Why exercise before breakfast may not be for diabetes patients. Connecticut Medicine 78, 517-520. [PubMed] [Google Scholar]
- Church T.S., Blair S.N., Cocreham S., Johannsen N., Johnson W., Kramer K., Mikus C.R., Myers V., Nauta M., Rodarte R.Q., Sparks L., Thompson A., Earnest C.P. (2010) Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. The Journal of the American Medical Association 304, 2253-2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civitarese A.E., Hesselink M.K., Russell A.P., Ravussin E., Schrauwen P. (2005) Glucose ingestion during exercise blunts exercise-induced gene expression of skeletal muscle fat oxidative genes. American Journal of Physiology. Endocrinology and Metabolism 289, E1023-1029. [DOI] [PubMed] [Google Scholar]
- Colberg S.R., Grieco C.R., Somma C.T. (2014) Exercise effects on postprandial glycemia, mood, and sympathovagal balance in type 2 diabetes. Journal of the American Medical Directors Association 15, 261-266. [DOI] [PubMed] [Google Scholar]
- Colberg S.R., Zarrabi L., Bennington L., Nakave A., Thomas Somma C., Swain D.P., Sechrist S.R. (2009) Postprandial walking is better for lowering the glycemic effect of dinner than pre-dinner exercise in type 2 diabetic individuals. Journal of the American Medical Directors Association 10, 394-397. [DOI] [PubMed] [Google Scholar]
- Coutinho M., Gerstein H.C., Wang Y., Yusuf S. (1999) The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care 22, 233-240. [DOI] [PubMed] [Google Scholar]
- De Bock K., Richter E.A., Russell A.P., Eijnde B.O., Derave W., Ramaekers M., Koninckx E., Leger B., Verhaeghe J., Hespel P. (2005) Exercise in the fasted state facilitates fibre type-specific intramyocellular lipid breakdown and stimulates glycogen resynthesis in humans. The Journal of Physiology 564, 649-660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DECODE. (1999) Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. The DECODE study group. European Diabetes Epidemiology Group. Diabetes Epidemiology: Collaborative analysis Of Diagnostic criteria in Europe. Lancet 354, 617-621. [PubMed] [Google Scholar]
- DECODE. (2001) Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Archives of Internal Medicine 161, 397-405. [DOI] [PubMed] [Google Scholar]
- DECODE. (2003) Is the current definition for diabetes relevant to mortality risk from all causes and cardiovascular and noncardiovascular diseases? Diabetes Care 26, 688-696. [DOI] [PubMed] [Google Scholar]
- Derave W., Mertens A., Muls E., Pardaens K., Hespel P. (2007) Effects of post-absorptive and postprandial exercise on glucoregulation in metabolic syndrome. Obesity 15, 704-711. [DOI] [PubMed] [Google Scholar]
- Devlin J.T., Horton E.S. (1985) Effects of prior high-intensity exercise on glucose metabolism in normal and insulin-resistant men. Diabetes 34, 973-979. [DOI] [PubMed] [Google Scholar]
- Dipietro L., Gribok A., Stevens M.S., Hamm L.F., Rumpler W. (2013) Three 15-min Bouts of Moderate Postmeal Walking Significantly Improves 24-h Glycemic Control in Older People at Risk for Impaired Glucose Tolerance. Diabetes Care 36, 3262-3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunstan D.W., Kingwell B.A., Larsen R., Healy G.N., Cerin E., Hamilton M.T., Shaw J.E., Bertovic D.A., Zimmet P.Z., Salmon J., Owen N. (2012) Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 35, 976-983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaudet-Savard T., Ferland A., Broderick T.L., Garneau C., Tremblay A., Nadeau A., Poirier P. (2007) Safety and magnitude of changes in blood glucose levels following exercise performed in the fasted and the postprandial state in men with type 2 diabetes. European Journal of Cardiovascular Prevention and Rehabilitation 14, 831-836. [DOI] [PubMed] [Google Scholar]
- Gillen J.B., Little J.P., Punthakee Z., Tarnopolsky M.A., Riddell M.C., Gibala M.J. (2012) Acute high-intensity interval exercise reduces the postprandial glucose response and prevalence of hyperglycaemia in patients with type 2 diabetes. Diabetes, Obesity and Metabolism 14, 575-477. [DOI] [PubMed] [Google Scholar]
- Gonzalez J.T. (2014) Paradoxical second-meal phenomenon in the acute postexercise period. Nutrition 30, 961-967. [DOI] [PubMed] [Google Scholar]
- Hashimoto S., Hayashi S., Yoshida A., Naito M. (2013) Acute effects of postprandial aerobic exercise on glucose and lipoprotein metabolism in healthy young women. Journal of Atherosclerosis and Thrombosis 20, 204-13, Feb 22. [DOI] [PubMed] [Google Scholar]
- Hirsch I.B., Brownlee M. (2005) Should minimal blood glucose variability become the gold standard of glycemic control? Journal of Diabetes and its Complications 19, 178-181. [DOI] [PubMed] [Google Scholar]
- Hopkins W.G., Marshall S.W., Batterham A.M., Hanin J. (2009) Progressive statistics for studies in sports medicine and exercise science. Medicine & Science in Sports & Exercise 41, 3-13. [DOI] [PubMed] [Google Scholar]
- Hordern M.D., Cooney L.M., Beller E.M., Prins J.B., Marwick T.H., Coombes J.S. (2008) Determinants of changes in blood glucose response to short-term exercise training in patients with Type 2 diabetes. Clinical Science 115, 273-281. [DOI] [PubMed] [Google Scholar]
- Hostmark A.T., Ekeland G.S., Beckstrom A.C., Meen H.D. (2006) Postprandial light physical activity blunts the blood glucose increase. Preventive Medicine 42, 369-371. [DOI] [PubMed] [Google Scholar]
- Høstmark A.T. (2007) Variations in the glycemic response to carbohydrates: do high responders have a special benefit of using low glycemic foods? The Open Nutrition Journal 1, 1-4. [Google Scholar]
- Jarrett R.J., Baker A.A., Keen H., Oakley N.W. (1972) Diurnal Variation in Oral Glucose Tolerance: Blood Sugar and Plasma Insulin Levels Morning, Afternoon, and Evening. British Medical Journal 1, 199-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karstoft K., Christensen C.S., Pedersen B.K., Solomon T.P. (2014) The acute effects of interval- vs continuous-walking exercise on glycemic control in subjects with type 2 diabetes: a crossover, controlled study. The Journal of Clinical Endocrinology & Metabolism 99, 3334-3342. [DOI] [PubMed] [Google Scholar]
- Khunti K., Skinner T.C., Heller S., Carey M.E., Dallosso H.M., Davies M.J., Collaborative D. (2008) Biomedical, lifestyle and psychosocial characteristics of people newly diagnosed with Type 2 diabetes: baseline data from the DESMOND randomized controlled trial. Diabetic Medicine 25, 1454-1461. [DOI] [PubMed] [Google Scholar]
- Lakens D. (2013) Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Frontiers in Psychology 4, 863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang J.A., Gisolfi C.V., Lambert G.P. (2006) Effect of exercise intensity on active and passive glucose absorption. International Journal of Sport Nutrition and Exercise Metabolism 16, 485-493. [DOI] [PubMed] [Google Scholar]
- Larsen J.J., Dela F., Kjaer M., Galbo H. (1997) The effect of moderate exercise on postprandial glucose homeostasis in NIDDM patients. Diabetologia 40, 447-453. [DOI] [PubMed] [Google Scholar]
- Larsen J.J., Dela F., Madsbad S., Galbo H. (1999) The effect of intense exercise on postprandial glucose homeostasis in type II diabetic patients. Diabetologia 42, 1282-1292. [DOI] [PubMed] [Google Scholar]
- Levitan E.B., Song Y., Ford E.S., Liu S. (2004) Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta- analysis of prospective studies. Archives of Internal Medicine 164, 2147-2155. [DOI] [PubMed] [Google Scholar]
- Little J.P., Jung M.E., Wright A.E., Wright W., Manders R.J. (2014) Effects of high-intensity interval exercise versus continuous moderate-intensity exercise on postprandial glycemic control assessed by continuous glucose monitoring in obese adults. Applied Physiology Nutrition and Metabolism 39, 835-841. [DOI] [PubMed] [Google Scholar]
- Lunde M.S., Hjellset V.T., Hostmark A.T. (2012) Slow post meal walking reduces the blood glucose response: an exploratory study in female pakistani immigrants. Journal of Immigrant and Minority Health 14, 816-822. [DOI] [PubMed] [Google Scholar]
- Manders R.J., Van Dijk J.W., van Loon L.J. (2010) Low-intensity exercise reduces the prevalence of hyperglycemia in type 2 diabetes. Medicine & Science in Sports & Exercise 42, 219-225. [DOI] [PubMed] [Google Scholar]
- Matthews J.N.S., Altman D.G., Campbell M.J., Royston P. (1990) Analysis of serial measurements in medical research. British Medical Journal 300, 230-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle W.D., Katch F.I., Katch V.L. (2010) Exercise physiology. 7 edition Wolters Kluwer, Lippincott Williams & Wilkins. [Google Scholar]
- McDonnell C.M., Donath S.M., Vidmar S.I., Werther G.A., Cameron F.J. (2005) A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technology & Therapeutics 7, 253-263. [DOI] [PubMed] [Google Scholar]
- Mikines K.J., Farrell P.A., Sonne B., Tronier B., Galbo H. (1988a) Postexercise dose-response relationship between plasma glucose and insulin secretion. Journal of Applied Physiology 64, 988-999. [DOI] [PubMed] [Google Scholar]
- Mikines K.J., Sonne B., Farrell P.A., Tronier B., Galbo H. (1988b) Effect of physical exercise on sensitivity and responsiveness to insulin in humans. American Journal of Physiology 254, E248-259. [DOI] [PubMed] [Google Scholar]
- Monnier L., Colette C. (2008) Glycemic variability: should we and can we prevent it? Diabetes Care 31, S150-154. [DOI] [PubMed] [Google Scholar]
- Moore J.G., Datz F.L., Christian P.E. (1990) Exercise increases solid meal gastric emptying rates in men. Digestive Diseases and Sciences 35, 428-432. [DOI] [PubMed] [Google Scholar]
- Nakagami T., Qiao Q., Tuomilehto J., Balkau B., Tajima N., Hu G., Borch-Johnsen K. (2006) Screen-detected diabetes, hypertension and hypercholesterolemia as predictors of cardiovascular mortality in five populations of Asian origin: the DECODA study. European Journal of Cardiovascular Prevention and Rehabilitation 13, 555-561. [DOI] [PubMed] [Google Scholar]
- Nelson J.D., Poussier P., Marliss E.B., Albisser A.M., Zinman B. (1982) Metabolic response of normal man and insulin-infused diabetics to postprandial exercise. American Journal of Physiology 242, E309-316. [DOI] [PubMed] [Google Scholar]
- Niskanen L., Turpeinen A., Penttila I., Uusitupa M.I. (1998) Hyperglycemia and compositional lipoprotein abnormalities as predictors of cardiovascular mortality in type 2 diabetes: a 15-year follow-up from the time of diagnosis. Diabetes Care 21, 1861-1869. [DOI] [PubMed] [Google Scholar]
- Nygaard H., Tomten S.E., Hostmark A.T. (2009) Slow postmeal walking reduces postprandial glycemia in middle-aged women. Applied Physiology Nutrition and Metabolism 34, 1087-1092. [DOI] [PubMed] [Google Scholar]
- Pan D.A., Lillioja S., Kriketos A.D., Milner M.R., Baur L.A., Bogardus C., Jenkins A.B., Storlien L.H. (1997) Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes 46, 983-988. [DOI] [PubMed] [Google Scholar]
- Peddie M.C., Bone J.L., Rehrer N.J., Skeaff C.M., Gray A.R., Perry T.L. (2013) Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. American Journal of Clinical Nutrition 98, 358-366. [DOI] [PubMed] [Google Scholar]
- Quagliaro L., Piconi L., Assaloni R., Martinelli L., Motz E., Ceriello A. (2003) Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes 52, 2795-804. [DOI] [PubMed] [Google Scholar]
- Risso A., Mercuri F., Quagliaro L., Damante G., Ceriello A. (2001) Intermittent high glucose enhances apoptosis in human umbilical vein endothelial cells in culture. American Journal of Physiology. Endocrinology and Metabolism 281, E924-930. [DOI] [PubMed] [Google Scholar]
- Rossetti P., Bondia J., Vehi J., Fanelli C.G. (2010) Estimating plasma glucose from interstitial glucose: the issue of calibration algorithms in commercial continuous glucose monitoring devices. Sensors 10, 10936-10952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasso F.C., Carbonara O., Nasti R., Campana B., Marfella R., Torella M., Nappi G., Torella R., Cozzolino D. (2004) Glucose metabolism and coronary heart disease in patients with normal glucose tolerance. The Journal of the American Medical Association 291, 1857-1863. [DOI] [PubMed] [Google Scholar]
- Scheen A.J., Van Cauter E. (1998) The roles of time of day and sleep quality in modulating glucose regulation: clinical implications. Hormone Research 49, 191-201. [DOI] [PubMed] [Google Scholar]
- Snowling N.J., Hopkins W.G. (2006) Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care 29, 2518-2527. [DOI] [PubMed] [Google Scholar]
- Standl E., Schnell O., Ceriello A. (2011) Postprandial hyperglycemia and glycemic variability: should we care? Diabetes Care 34, Suppl 2, S120-7, May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temelkova-Kurktschiev T.S., Koehler C., Henkel E., Leonhardt W., Fuecker K., Hanefeld M. (2000) Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care 23, 1830-1834. [DOI] [PubMed] [Google Scholar]
- Terada T., Wilson B.J., Myette-Comicronte E., Kuzik N., Bell G.J., McCargar L.J., Boule N.G. (2016) Targeting specific interstitial glycemic parameters with high-intensity interval exercise and fasted-state exercise in type 2 diabetes. Metabolism 65, 599-608. [DOI] [PubMed] [Google Scholar]
- Van Dijk J.W., Manders R.J., Canfora E.E., Mechelen W.V., Hartgens F., Stehouwer C.D., Van Loon L.J. (2013a) Exercise and 24-h glycemic control: equal effects for all type 2 diabetes patients? Medicine & Science in Sports & Exercise 45, 628-635. [DOI] [PubMed] [Google Scholar]
- van Dijk J.W., Venema M., van Mechelen W., Stehouwer C.D., Hartgens F., van Loon L.J. (2013b) Effect of moderate-intensity exercise versus activities of daily living on 24-hour blood glucose homeostasis in male patients with type 2 diabetes. Diabetes Care 36, 3448-3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Proeyen K., Szlufcik K., Nielens H., Ramaekers M., Hespel P. (2010) Beneficial metabolic adaptations due to endurance exercise training in the fasted state. Journal of Applied Physiology 110, 236-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker K.Z., Piers L.S., Putt R.S., Jones J.A., O'Dea K. (1999) Effects of regular walking on cardiovascular risk factors and body composition in normoglycemic women and women with type 2 diabetes. Diabetes Care 22, 555-561. [DOI] [PubMed] [Google Scholar]


