SUMMARY
Objective
Estimate annual incidence rates (IRs) of hip symptoms and three osteoarthritis (OA) outcomes (radiographic, symptomatic, and severe radiographic) overall and by race, sociodemographic characteristics, and hip OA risk factors.
Design
Analyze baseline (1991–1997) and first follow-up (1999–2003) data (n = 1446) from the Johnston County Osteoarthritis Project, a population-based, prospective study of adults ≥45 years in North Carolina. Hip symptoms were pain, aching, and/or stiffness on most days, or groin pain. Radiographic and severe radiographic OA were Kellgren–Lawrence (KL) grades ≥2 and ≥3, respectively. Symptomatic OA was radiographic OA with symptoms in the same hip. Sociodemographics were age, gender, race, highest attained education, and annual household income. Hip OA risk factors were self-reported body mass index (BMI) at age 18 years, clinically measured BMI at baseline, and history of hip injury.
Results
Annual IRs (median = 5.5 years follow-up) were 37, 23, 13, and 2.9 per 1000 person-years for hip symptoms, and radiographic, symptomatic, and severe radiographic hip OA, respectively. We found low IRs of radiographic and symptomatic hip OA among African Americans and high IRs of hip symptoms among the obese and the very poor. Across outcomes, IRs were highest for those with hip injury.
Conclusion
No prior studies have reported IRs of hip symptoms; IRs of radiographic and severe radiographic hip OA were similar to, and the IR of symptomatic hip OA was higher than, previous estimates. Prevention efforts should target low socioeconomic status (SES) populations and obese adults; interventions for hip OA and hip symptoms are imperative for those with hip injuries.
Keywords: Hip osteoarthritis, Hip symptoms, Race, Socioeconomic status, Incidence rates
Introduction
Hip osteoarthritis (OA) is a common cause of pain and disability among older adults and a predominant reason for total hip replacement (THR) surgery1, which, in the US, is expected to grow to half a million procedures annually by 20302. Among adults aged ≥45 years, radiographic hip OA affects 27%, and symptomatic hip OA (defined as radiographic OA with hip symptoms) may affect 3–9%3,4. Hip pain and other OA symptoms can substantially impair health and functioning, limit daily activities and reduce quality of life5,6, and can significantly affect individuals financially through lost wages and need for informal care7,8. Additionally, hip OA has been associated with an increased risk of mortality among older women9. These costs and the poor health associated with hip OA are part of a global public health problem that is predicted to only worsen10.
Epidemiological studies of incident hip OA have examined the role of demographics (women, older age, and white/African American race)11–15 and modifiable risk factors (hip injury and obesity)11,16–25, but most of these studies have reported ratio measures (e.g., odds ratios). Descriptive studies quantifying the incidence rate (IR) – the rate at which new cases arise in the population – provide data that can be used for projecting prevalence and forecasting health service utilization and costs. Further, hip pain and symptoms can have a substantial health and economic impact, but no studies have reported IRs of hip pain/symptoms independently of radiographic hip OA, which can be poorly correlated with symptoms5,6,26.
Of the few studies that have reported IRs of hip OA, some were in limited populations (e.g., white race or women only) and others reported only cumulative incidences27, which may not adequately account for variation in observation time among participants. Furthermore, some US studies were conducted several decades ago and may not represent IRs in current populations given aging, increasing racial/ethnic diversity, and increasing prevalence of obesity in the US over past decades. Of the previous studies, two in the US estimated IRs for symptomatic hip OA from health records; Wilson et al. estimated an age and sex-adjusted rate of 47 per 100,000 person-years for the entire population of Rochester, MN in 198512, and Oliveria et al. estimated an age and sex-adjusted rate of 88 per 100,000 person-years among HMO members aged 20–89 in Worcester County, MA between 1998–199211. Three studies reported cumulative incidence of radiographic OA; from the Study of Osteoporotic Fractures, a multicenter US cohort of Caucasian women ≥65 years (mean follow-up 8 years), Lane et al. found 33% and 14% developed radiographic and severe radiographic OA (KL ≥3) respectively of the hip between 1986–199828; from the Rotterdam Study, a population-based Dutch cohort aged ≥55 (mean follow-up 6.6 years), Reijman et al. estimated 17% developed incident radiographic hip OA as defined by Kellgren–Lawrence (KL) grade ≥2, between 1990–199929; from the Johnston County OA Project (JoCo OA), Kopec et al. reported that radiographic OA developed in 7% of hips (joint-based analysis)13. Grotle et al. estimated 10-year cumulative incidence of self-reported hip OA of 6% in a population-based cohort ages 24–76 years in Ullensaker, Norway in 1994–2004.
Given these limited data on IRs of hip OA-related outcomes, we conducted a comprehensive hip OA incidence study using data from the JoCo OA, a large population-based, prospective cohort study in Johnston County, North Carolina. The purpose of this study was to quantify annual IRs of hip symptoms and three types of hip OA (radiographic, symptomatic, and severe radiographic hip OA). For three outcomes (hip symptoms, radiographic, symptomatic hip OA), we estimated overall IRs among African Americans and whites. For these three outcomes, we also estimated IRs by selected sociodemographic variables and hip OA risk factors, overall and for each race. Annual IRs for subgroups can be used to prioritize susceptible populations for further research and prevention efforts.
Method
We analyzed baseline (1991–1997) and first follow-up (1999–2003) data from the JoCo OA. The study’s overall methodological approach is detailed elsewhere30. Enrolled participants represented civilian, non-institutionalized African Americans and whites ≥45 years who were residents of one of six designated townships in Johnston County for at least 1 year and who were physically and mentally capable of study completion. At both baseline and first follow-up, participants completed two in-home interviews, approximately 2 weeks apart, and a clinical examination. Supine anterior–posterior pelvis radiographs for both hips were read using standard Kellgren–Lawrence (KL) grade (0–4)31. Pelvic radiographs were not obtained from women <50 years. The institutional review boards of the Centers for Disease Control and Prevention and the University of North Carolina Schools of Medicine and Public Health approved the study’s protocol.
JoCo OA staff employed various methods to minimize attrition between baseline and first follow-up. Staff used annual newsletters, personal networks, local advertising, medical providers, and community inquiries to locate and retain participants. Deaths were identified through multiple sources including local obituaries, word-of-mouth, local and North Carolina death records, and the National Death Index (NDI), the most complete source of mortality data.
Measurement of hip symptoms and hip OA outcomes
Annual IRs were estimated for hip symptoms and three types of hip OA (radiographic, symptomatic, and severe radiographic hip OA). Hip symptoms were defined as either a “yes” to the question “On most days, do you have pain, aching, or stiffness in your (right, left) hip?” or reported the presence of (right, left) groin pain. Radiographic and severe radiographic OA were defined as KL grades of ≥2 and ≥3, respectively. Inflammatory arthritis occurred in 21 participants; joints with radiographic evidence of inflammatory arthritis were treated as having missing KL grades and thereby excluded from analysis. Symptomatic OA was defined as having radiographic OA and hip symptoms in the same hip. Because symptomatic OA is the underlying cause in the majority of THRs1, those with THR were classified as affected for all four outcomes, similar to previous studies13,32.
For each outcome, an incident case was a participant who was not affected at baseline who developed the outcome in at least one hip by first follow-up (range 3–13 years). Baseline prevalent cases (i.e., participants having a given outcome in one or both hips at baseline) were excluded from analysis of that outcome, and therefore the number of participants varied for each outcome analysis (Table I). Analyses for hip symptoms included participants aged ≥45 years. Because women of reproductive age (<50 years) (n = 312) did not have hip radiographs, we also excluded men <50 years (n = 175) (Table I) so that the three hip OA outcome analyses comprised the same age groups for women and men.
Table I.
Unweighted sample sizes in the entire baseline, eligible baseline, and analytic samples with incident cases, by hip symptoms and three hip OA outcomes
| All analyses* | Hip symptoms | Hip OA outcomes
|
|||
|---|---|---|---|---|---|
| Radiographic | Symptomatic | Severe radiographic | |||
| Entire baseline sample (1991–1997) | 3068 | 3068 | 3068 | 3068 | 3068 |
| Outcome at baseline | 1228 | 803 | 323 | 72 | |
| Participants at risk at baseline | 1840 | 2265 | 2745 | 2996 | |
| Other baseline exclusions | |||||
| Hip replacement | 24 | 24 | 24 | 24 | |
| Women <50 years | 0 | 312 | 312 | 312 | |
| Men <50 years | 0 | 175 | 175 | 175 | |
| Missing baseline | 72 | 58 | 51 | 60 | |
| Eligible baseline sample | 2788 | 1744 | 1696 | 2183 | 2425 |
| Participant exclusions at 1995–2003 follow-up† | |||||
| Deceased | 200 | 223 | 301 | 338 | |
| Mentally/physically unable | 98 | 123 | 155 | 181 | |
| Moved out of study area | 129 | 119 | 159 | 176 | |
| Declined participation | 276 | 228 | 286 | 296 | |
| No clinic exam | 75 | 83 | 102 | 107 | |
| Unable to locate | 30 | 38 | 48 | 55 | |
| Eligible at follow-up | 936 | 865 | 1124 | 1242 | |
| Missing outcome at follow-up | 0 | 17 | 8 | 30 | |
| Analytic sample | 1446 | 936 | 864 | 1116 | 1212 |
| Incident cases at follow-up | 200 | 107 | 93 | 30 | |
3068 were enrolled at baseline; 2788 were eligible for analysis of at least 1 of the 4 outcomes; 1446 were analyzed for at least 1 of the 4 outcomes.
Participants who were excluded were those who died (deceased), were mentally or physically unable to participate, moved out of the study area, declined to participate, participated in the in-home questionnaire but not the clinic exam (no clinic exam), or were lost to follow up for other reasons (unable to locate).
Sociodemographic and hip OA risk factors
Sociodemographic characteristics (and their categorized levels) analyzed were age (45–54 or 50–54 [as appropriate], 55–64, 65–74, and ≥75 years), sex (men, women), race (African American, white), highest attained education (<high school [<grade 12], some/completed high school [grade 12/GED {general equivalency diploma}], >high school [college/grad school] and annual household income ($0–<15,000, $15,000–<35,000, ≥$35,000). The three hip OA risk factors were self-reported body mass index (BMI) in kg/m2 at age 18 (under/healthy weight [<25], overweight/obese [≥25]) and clinically measured BMI at baseline (under/healthy weight [<25], overweight [25–<30], and obese [≥30] {Class I [30–<35] and Class II–IV [≥35]}), and history of hip injury (yes, no). Self-reported BMI at age 18 was based on participants’ report of their weight at age 18. The denominator for all BMI calculations was clinically measured height at baseline. Hip injury was ascertained during the baseline clinic examination with “Have you ever injured your (right, left) hip?”.
Statistical analysis
Using person as the unit of analysis, we estimated annual IRs using a Poisson model with an offset (a term incorporated into the model to compute rates) taken as the natural logarithm of participant observation time (in years) to accommodate the variation in follow-up time among participants. We computed a crude IR (overall and stratified by sociodemographics and hip OA risk factors described above) with 95% confidence intervals (CI). For overall IRs, we also computed age- and age- and sex-standardized IRs using the 2000 projected US population with the same age categories that we analyzed (45–54 or 50–54 [as appropriate], 55–64, 65–74, and ≥75 years). We estimated race-specific IRs stratified by the same sociodemographics and hip OA risk factors using models that included race as an additional independent variable. We also tested for interactions with race but none was significant, most likely due to small sample sizes and low statistical power to detect these interactions. We did not compute stratified or race-specific IRs of severe radiographic hip OA because these estimates were unreliable due to the small number of unweighted cases (n = 30) (Table I).
To account for the complex sampling design, observations were weighted with population-calibrated sampling weights so that results are generalizable to the target Johnston County population. We calculated 95% CIs using jackknife methods that accounted for stratification and clustering in the sampling design with a finite population correction to adjust for sampling without replacement33,34. Jackknifing produces accurate CIs even in the presence of overdispersion (i.e., variance greater than predicted by a Poisson distribution). We tested for differences in IRs using a Wald test with jackknife variance estimates that accounted for the sampling design. For age, education, self-reported BMI at age 18, and clinically measured BMI at baseline, we also tested for a trend through assessing the slope in models that included each of these characteristics as a continuous variable. Statistical significance was determined using a Bonferroni-corrected alpha of 0.0166 (<0.05/3 outcomes) to adjust for multiple comparisons across three outcomes (hip symptoms, and radiographic and symptomatic hip OA, but not severe radiographic hip OA owing to its lack of formal comparisons)35. We performed statistical analyses with SAS version 9.3.
Sensitivity analysis
We performed sensitivity analyses for income imputation and selection bias following procedures detailed in Murphy et al.36. We conducted these analyses to determine the extent to which missing income data and selection bias due to attrition may have influenced the IRs.
Income imputation
Based on weighted percentages, income was unknown for 18% of participants due to nonresponse (“refused” or “don’t know”), so we repeated the IR analyses using imputed income values to assess bias due to missing data. We performed multiple imputation with baseline variables for sociodemographics, hip OA risk factors/outcomes, and characteristics associated with income or income nonresponse. We found that analyses based on imputed income data produced similar IRs to those presented here. Thus any bias due to missing income data was likely small.
Selection bias
Because approximately 48% of eligible participants were excluded from IR estimation (Table I), we performed additional analyses to evaluate the extent of selection bias in the overall estimates. We computed approximate IRs for the analytic and eligible baseline populations (Table II)36. For all outcomes we found that these approximate IRs were similar to each other. Thus differences between the analytic and baseline eligible populations appeared to have had little impact on IR estimates, and any potential selection bias was likely small.
Table II.
Weighted* distribution (%)† of baseline sociodemographic characteristics and hip OA risk factors for the analytic and eligible baseline samples
| Analytic sample n = 1446 | Eligible baseline sample n = 2778 | |
|---|---|---|
| Sociodemographic characteristics | ||
| Age (years) | ||
| 45–54 | 52 | 30 |
| 55–64 | 26 | 29 |
| 65–74 | 18 | 28 |
| ≥75 | 5 | 13 |
| Median | 55 | 62 |
| Sex | ||
| Men | 42 | 43 |
| Women | 58 | 57 |
| Race | ||
| African American | 20 | 18 |
| White | 80 | 82 |
| Marital status | ||
| Never married | 4 | 3 |
| Married | 73 | 66 |
| Separated/divorced | 9 | 10 |
| Widowed | 13 | 22 |
| Highest education | ||
| <High school | 11 | 21 |
| Some/completed high school | 54 | 52 |
| >High school | 34 | 28 |
| Annual household income | ||
| $0–<$15,000 | 25 | 35 |
| $15,000–<$35,000 | 29 | 27 |
| ≥$35,000 | 28 | 17 |
| Don’t know | 7 | 9 |
| Refused | 11 | 12 |
| Hip OA risk factors | ||
| Self-reported BMI at age 18 (kg/m2) | ||
| Under or healthy weight (<25) | 92 | 90 |
| Overweight or obese (≥25) | 8 | 10 |
| Clinically measured BMI at study baseline (kg/m2) | ||
| Under or healthy weight (<25) | 31 | 34 |
| Overweight (25–<30) | 44 | 42 |
| Obese (≥30) | 25 | 24 |
| Obese Class I (30–<35) | 17 | 17 |
| Obese Class II–IV (≥35) | 7 | 6 |
| History of hip injury | ||
| No | 97 | 95 |
| Yes | 3 | 5 |
The analytic and eligible samples were weighted to the Johnston County population in 2000 and 1990, respectively. Differences in weighted numbers are due to the use of different sampling weights applied to the baseline and follow-up samples.
Percentages may not sum to 100% due to rounding.
Results
Of the 3068 participants in the JoCo OA sample at baseline, 2788 were potentially eligible for analysis after applying baseline exclusions (Table I). Of these 2788, about half (n = 1446) had both baseline and follow-up data for at least 1 of the 4 outcomes and were included in the analytic sample (Table I). The median follow-up time for analyzed participants was 5.5 years (3–13 years).
Based on weighted percentages, the analytic sample represented a population at baseline that was over half women (58%) and predominantly white (80%) having a median age of 55 years (Table II). Most were married (73%) and had completed at least some high school (88%). About 25% had an annual household income under $15,000, 28% had an income of $35,000 or more, and income was unknown for 7% due to “don’t know” and 11% due to “refused” responses. At age 18, only 8% were overweight or obese whereas most were overweight (44%) or obese (25%) at the time of study baseline. Among those who were obese, almost a third were Class II–IV (BMI ≥35). Only 3% had a history of hip injury.
Crude and standardized annual IRs
Crude and standardized annual IRs are presented in Table III. Crude IRs per 1000 person-years for hip symptoms, and radiographic, symptomatic, and severe radiographic hip OA were 37 (95% CI = 33, 41), 20 (95% CI = 18, 23), 13 (95% CI = 12, 16), and 2.9 (95% CI = 2.3, 3.7), respectively. Age-standardized and age- and sex-standardized IRs were higher than crude estimates (Table III).
Table III.
Overall crude, age-standardized, and age- and sex-standardized IRs per 1000 person-years and their 95% CIs for hip symptoms and three hip OA outcomes
| Hip symptoms | OA outcomes
|
|||||||
|---|---|---|---|---|---|---|---|---|
|
|
Radiographic
|
Symptomatic
|
Severe radiographic
|
|||||
| IR | (95% CI) | IR | (95% CI) | IR | (95% CI) | IR | (95% CI) | |
| Crude | 37 | (33, 41) | 20 | (18, 23) | 13 | (12, 16) | 2.9 | (2.3, 3.7) |
| Age-standardized* | 39 | (34, 44) | 24 | (20, 30) | 17 | (14, 20) | 3.2 | (2.5, 4.1) |
| Age- and sex-standardized* | 38 | (34, 43) | 24 | (20, 30) | 17 | (14, 19) | 3.2 | (2.5, 4.1) |
Standardized to the 2000 projected US population.
Stratified and race-specific IRs
Annual IRs stratified by sociodemographic characteristics and hip OA risk factors are presented in Table IV, and race-specific annual IRs are presented in Table V, for the three outcomes of hip symptoms, radiographic OA, and symptomatic OA. We presented overall and race-specific IRs by age group in Figure 1.
Table IV.
IRs per 1000 person-years and their 95% CIs for hip symptoms and OA outcomes by sociodemographic characteristics and hip OA risk factors
| Hip symptoms | OA
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
Radiographic
|
Symptomatic
|
|||||||
| IR | (95% CI) | P value* (PTrend†) | IR | (95% CI) | P value* (PTrend†) | IR | (95% CI) | P value* (PTrend†) | |
| Sociodemographic characteristics | |||||||||
| Race | 0.082 | <0.001‡ | <0.001‡ | ||||||
| African American | 28 | (20, 39) | 7 | (5, 10) | 7 | (5, 11) | |||
| White | 39 | (34, 44) | 24 | (21, 27) | 15 | (13, 18) | |||
| Age (years) | 0.31 | <0.001‡ | <0.001‡ | ||||||
| 45 – 54/50 – 54§ | 34 | (28, 41) | (0.018) | 12 | (10, 16) | (<0.001‡) | 8 | (6, 12) | (<0.001‡) |
| 55–64 | 38 | (32, 44) | 27 | (22, 34) | 16 | (13, 20) | |||
| 65–74 | 43 | (36, 52) | 28 | (22, 36) | 18 | (14, 24) | |||
| ≥75 | 45 | (28, 72) | 28 | (14, 52) | 23 | (16, 33) | |||
| Sex | 0.008‡ | 0.23 | 0.013‡ | ||||||
| Men | 30 | (24, 37) | 19 | (15, 23) | 11 | (8, 14) | |||
| Women | 42 | (36, 48) | 22 | (19, 27) | 16 | (14, 19) | |||
| Highest education | 0.48 | 0.25 | 0.81 | ||||||
| <High school (HS) | 40 | (31, 50) | (0.030) | 22 | (16, 30) | (0.016‡) | 14 | (10, 20) | (0.98) |
| Some/completed HS | 38 | (32, 45) | 22 | (18, 26) | 13 | (10, 16) | |||
| >HS | 33 | (26, 41) | 17 | (13, 22) | 14 | (11, 19) | |||
| Annual household income | 0.022 | 0.57 | 0.76 | ||||||
| $0–<$15,000 | 45 | (37, 53) | 20 | (17, 24) | 14 | (12, 17) | |||
| $15,000–<$35,000 | 34 | (27, 42) | 22 | (18, 28) | 13 | (10, 18) | |||
| ≥$35,000 | 28 | (21, 37) | 18 | (13, 25) | 12 | (8, 18) | |||
| Hip OA risk factors | |||||||||
| Self-reported BMI(kg/m2) at age 18 | 0.40 | 0.67 | 0.005‡ | ||||||
| Underweight/Normal(<25) | 35 | (31, 40) | (0.19) | 21 | (18, 24) | (0.21) | 14 | (12, 17) | (0.10) |
| Overweight/Obese (≥25) | 43 | (28, 66) | 19 | (14, 28) | 5 | (3, 10) | |||
| Clinically measured BMI (kg/m2) at baseline | <0.001‡ | <0.001‡ | 0.73 | ||||||
| Under/healthy (<25) | 24 | (19, 29) | (0.013‡) | 29 | (23, 36) | (0.19) | 14 | (11, 18) | (0.30) |
| Overweight (25–<30) | 41 | (34, 48) | 16 | (13, 20) | 13 | (10, 17) | |||
| Obese (≥30) | 48 | (37, 61) | 20 | (16, 26) | 12 | (10, 16) | |||
| Obese Class I (30–<35) | 49 | (37, 65) | 17 | (12, 24) | 13 | (10, 18) | |||
| Obese Class II–IV (≥35) | 44 | (25, 77) | 27 | (19, 38) | 10 | (6, 17) | |||
| History of hip injury | 0.41 | 0.26 | 0.022 | ||||||
| No | 36 | (3.2, 4.0) | 20 | (18, 23) | 13 | (11, 16) | |||
| Yes | 51 | (2.2, 11.8) | 28 | (16, 52) | 28 | (15, 50) | |||
P-value for differences in IRs.
P-value for trend in IRs; performed through assessment of the slope for continuous variables for age, highest education, self-reported BMI at age 18, and clinically measured BMI at baseline.
Statistically significant at Bonferroni-corrected α = 0.0166.
Hip symptoms: 45–54 years; radiographic and symptomatic OA: 50–54 years.
Table V.
Race-specific IRs per 1000 person-years and their 95% CIs for hip symptoms and OA outcomes by sociodemographic characteristics and hip OA risk factors
| Hip symptoms | OA outcomes
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
Radiographic
|
Symptomatic
|
|||||||
| African American |
White
|
P value† (PTrend‡)
|
African American |
White
|
P value† (PTrend‡)
|
African American |
White
|
P value† (PTrend‡)
|
|
| IR (95% CI) | IR (95% CI) | IR (95% CI) | IR (95% CI) | IR (95% CI) | IR (95% CI) | ||||
| Overall | |||||||||
| Crude | 28 (20, 39) | 39 (34, 44) | 7 (5, 10) | 24 (21, 27) | 7 (5, 11) | 15 (13, 18) | |||
| Age-standardized* | 30 (22, 42) | 41 (36, 47) | 9 (7, 13) | 28 (23, 34) | 9 (6, 14) | 19 (16, 22) | |||
| Age- and sex-standardized* | 30 (22, 41) | 41 (36, 47) | 9 (7, 13) | 29 (24, 36) | 9 (6, 14) | 19 (16, 22) | |||
| Sociodemographic characteristics | |||||||||
| Age (years) | 0.32 | <0.001§ | <0.001§ | ||||||
| 45–54/50–54║ | 27 (18, 38) | 36 (30, 43) | (0.025) | 5 (3, 7) | 15 (11, 19) | (<0.001§) | 5 (3, 8) | 10 (7, 14) | (<0.001§) |
| 55–64 | 29 (20, 41) | 39 (33, 46) | 10 (7, 14) | 32 (26, 39) | 9 (6, 13) | 18 (14, 23) | |||
| 65–74 | 34 (24, 47) | 46 (38, 55) | 10 (7, 15) | 32 (25, 42) | 10 (6, 15) | 20 (15, 27) | |||
| ≥75 | 35 (21, 60) | 48 (30, 76) | 10 (5, 20) | 32 (17, 59) | 12 (7, 21) | 25 (18, 37) | |||
| Sex | 0.008§ | 0.22 | 0.014§ | ||||||
| Men | 23 (16, 34) | 32 (26, 39) | 7 (5, 10) | 22 (18, 27) | 6 (4, 9) | 12 (9, 16) | |||
| Women | 32 (23, 45) | 44 (38, 51) | 8 (6, 11) | 26 (22, 31) | 9 (6, 13) | 19 (16, 22) | |||
| Highest education | 0.36 | 0.12 | 0.72 | ||||||
| <High school (HS) | 31 (22, 45) | 44 (34, 57) | (0.022) | 8 (5, 13) | 28 (20, 38) | (0.003§) | 8 (5, 12) | 17 (12, 25) | (0.81) |
| Some/completed HS | 29 (20, 42) | 41 (34, 49) | 8 (6, 11) | 26 (22, 31) | 6 (4, 10) | 14 (12, 18) | |||
| >HS | 25 (16, 37) | 35 (28, 43) | 6 (4, 8) | 19 (14, 25) | 7 (4, 11) | 16 (12, 22) | |||
| Annual household income | 0.005§ | 0.39 | 0.44 | ||||||
| $0–<$15,000 | 32 (23, 46) | 50 (42, 60) | 8 (6, 10) | 25 (21, 31) | 7 (5, 11) | 17 (14, 21) | |||
| $15,000–<$35,000 | 23 (16, 34) | 36 (28, 45) | 8 (5, 11) | 25 (20, 32) | 6 (4, 11) | 15 (11, 20) | |||
| ≥$35,000 | 19 (12, 29) | 29 (22, 39) | 6 (4, 9) | 20 (14, 27) | 6 (3, 10) | 13 (8, 20) | |||
| Hip OA risk factors | |||||||||
| Self-reported BMI at age 18 (kg/m2) | 0.37 | 0.84 | 0.008§ | ||||||
| Under/healthy (<25) | 25 (18, 34) | 38 (33, 43) | (0.11) | 8 (6, 11) | 24 (21, 28) | (0.45) | 8 (5, 12) | 16 (13, 19) | (0.19) |
| Overweight/obese (≥25) | 30 (16, 59) | 47 (30, 72) | 8 (5, 13) | 23 (16, 33) | 3 (1, 6) | 6 (3, 12) | |||
| Clinically measured BMI at baseline (kg/m2) | <0.001§ | <0.001§ | 0.94 | ||||||
| Under/healthy weight (<25) | 16 (11, 23) | 25 (20, 31) | (<0.004§) | 11 (7, 16) | 32 (25, 39) | (0.50) | 7 (4, 12) | 15 (12, 19) | (0.71) |
| Overweight (25–<30) | 29 (20, 41) | 44 (37, 53) | 6 (4, 9) | 19 (15, 23) | 7 (4, 11) | 15 (12, 20) | |||
| Obese (≥30) | 34 (23, 51) | 53 (41, 68) | 8 (6, 11) | 24 (19, 32) | 7 (4, 10) | 14 (11, 19) | |||
| Obese Class I (30–<35) | 35 (24, 51) | 54 (40, 71) | 7 (5, 10) | 21 (15, 30) | 7 (4, 11) | 15 (11, 21) | |||
| Obese Class II–IV (≥35) | 33 (16, 67) | 51 (29, 90) | 11 (7, 17) | 34 (23, 50) | 6 (3, 11) | 12 (7, 21) | |||
| History of hip injury | 0.28 | 0.14 | 0.011§ | ||||||
| No | 24 (18, 34) | 38 (34, 43) | 7 (5, 10) | 24 (21, 27) | 7 (4, 10) | 15 (13, 18) | |||
| Yes | 38 (17, 86) | 60 (27, 134) | 12 (6, 21) | 36 (20, 65) | 15 (7, 29) | 33 (19, 59) | |||
Standardized to the 2000 projected US population.
P-value for differences in IRs.
P-value for trend in IRs; performed through assessment of the slope for continuous variables for age, highest education, self-reported BMI at age 18, and clinically measured BMI at baseline.
Statistically significant at Bonferroni-corrected α = 0.0166.
Hip symptoms: 45–54 years; radiographic and symptomatic OA: 50–54 years.
Fig. 1.
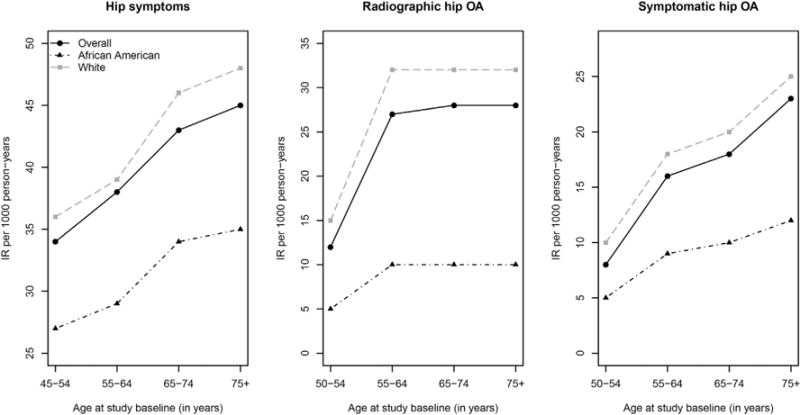
Incidence rate (IR) per 1000 person-years for hip symptoms and OA outcomes by age group, overall and within each race.
Sociodemographic characteristics
Race
Across the three outcomes, IRs were lower among African Americans with significant differences for radiographic and symptomatic OA. The IR of radiographic OA was 24/1000 person-years for whites and 7/1000 person-years for African Americans, just over a quarter the rate of whites. The IR of symptomatic OA was 15/1000 person-years for whites and 7/1000 person-years for African Americans, less than half the rate of whites (Table IV).
Age
Across the three outcomes, IRs increased with greater baseline age, and trends were significant for radiographic and symptomatic OA. The IR of radiographic OA more than doubled from 12 to 27/1000 person-years between ages 50–54 and 55–64 and then remained steady among older ages. The annual IR of symptomatic hip OA almost tripled from 8 to 23/1000 person-years from youngest to oldest ages (Table IV, Fig. 1). Race-specific IRs for age showed similar trends (Table V, Fig. 1).
Sex
Across the three outcomes, IRs were higher among women than men with significant differences for hip symptoms and symptomatic OA, which were almost 50% higher among women (Table IV). Race-specific IRs for sex showed similar patterns (Table V).
Highest education
For hip symptoms and radiographic OA, IRs decreased moderately with greater educational attainment with a significant trend only for radiographic OA (Table IV). The trend in race-specific IRs of radiographic OA was also significant; compared with the overall sample, the decreasing trend appeared stronger among whites but was attenuated among African Americans (Table V).
Annual household income
The annual IR of 45/1000 person-years of hip symptoms for those with lowest income was among the highest rates observed across all subpopulations that we analyzed (Table IV). Across all three outcomes, race-specific IRs decreased with rising income, but differences were significant only for hip symptoms (Table V).
Hip OA risk factors
Self-reported BMI at age 18
The IR of hip symptoms was moderately higher among those with greater BMI at age 18, but there was no significant trend. Conversely for symptomatic OA, the IR among those who were overweight/obese was less than half the IR among those who were under/normal weight at age 18, and though the difference was significant, there was no significant trend. Across the three outcomes, the IRs of radiographic OA varied little (Table IV). Race-specific IRs of BMI at age 18 showed similar patterns (Table V).
Clinically measured BMI at baseline
For hip symptoms, the IR increased significantly with greater BMI at baseline; the IR of 48/1000 person-years among obese persons (≥30) was high at twice the IR of 24/1000 person-years among under/healthy weight (<25) persons (Table IV). The IR of radiographic OA varied significantly across BMI levels but there was no significant trend. The IR of symptomatic OA varied little across BMI levels (Table IV). Race-specific IRs for BMI at baseline showed similar patterns (Table V).
History of hip injury
Across the three outcomes, those with hip injury had the highest IRs of all characteristics that we analyzed. Those with hip injury had higher IRs than those without hip injury, but these differences were not significant in the overall sample (Table IV). After stratifying by race, the difference was significant for symptomatic OA. Within each race, those with hip injury had double the IR of symptomatic OA (Table V).
Discussion
In this study of adults aged ≥45 years followed for a median of 5.5 years, IRs were 37, 20, 13, and 2.9 per 1000 person-years for hip symptoms, and radiographic, symptomatic, and severe radiographic hip OA, respectively. Overall and across sociodemographic subgroups and hip OA risk factors, the IRs of radiographic and symptomatic hip OA among African Americans were significantly lower than IRs for whites. For both African Americans and whites, the highest IRs of hip symptoms occurred among those aged ≥75 years, those with an annual household income <$15,000, those who were obese, and those with history of hip injury. Those with hip injury also had highest IRs of radiographic and symptomatic hip OA, indicating the importance of OA prevention efforts among this subgroup.
Previous studies have assessed hip OA incidence data by race, age, and sex. Our findings of lower IRs of radiographic and symptomatic hip OA among African Americans are consistent with a joint-based (as opposed to person-based) analysis of incident radiographic hip OA in the JoCo OA cohort13. Across outcomes, IRs increased with older age with significant trends for radiographic and symptomatic OA. Although this same pattern has been found with radiographic OA20,21, previous studies have shown declining IRs of incident symptomatic hip OA among the oldest ages11,12. Differences in study populations and small numbers of oldest participants12 likely contribute to variation in trends in oldest ages12. Also reported previously11,12,37, women had significantly higher IRs of hip symptoms and symptomatic hip OA than men.
This is among the first studies of socioeconomic status (SES) and hip OA, and it is the first study to quantify IRs of hip outcomes by household income and educational attainment. Lower education was associated with a higher IR of radiographic OA, and lowest income (<$15,000) was associated with a higher IR of hip symptoms after adjusting for race. Two previous studies, one in the JoCo OA cohort, have also reported higher risk of hip OA among low SES populations38,39, but our IR data further showed that those with lowest income had among the highest rates of hip symptoms across the large number of subpopulations that we analyzed. Regardless of cause, high IRs among low-SES populations are a concern given the substantial economic costs due to OA-associated hip symptoms7 and the disproportionate impact those costs may have on low-income households. Therefore, public health initiatives that prioritize low-SES populations and promote low-cost, evidence-based strategies (e.g., physical activity, weight loss, and self-management) are needed. Furthermore, conducting interventions and addressing barriers to uptake in low SES populations38 may be an effective means of lowering incidence of hip symptoms.
Adults with greater BMI at baseline had a significantly higher IR of hip symptoms with a strong positive trend. We found wide variation in IRs of radiographic OA, with lowest rates among overweight persons, but no significant trend. The IRs of symptomatic hip OA varied little across levels of BMI. Similarly discordant patterns have been reported previously19,40, and our findings for hip OA are consistent with studies reporting a lack of association with incident hip OA20–22,25,41. Given the strong positive association between BMI and hip symptoms and the very high IR of hip symptoms among obese, focusing prevention among overweight/obese adults and emphasizing strategies to maintain healthy weight may reduce incident hip symptoms.
We found that a high BMI at age 18 did not predict the development of incident hip OA among those aged ≥50 years. In fact, those who were overweight/obese at age 18 had a lower IR of symptomatic hip OA, and further we found no significant trend between BMI at age 18 and onset of any hip outcomes. Variation in estimates and lack of significance was also found for self-reported hip OA with clinically measured and self-reported BMI in a previous study among young men16. Characteristics that we did not analyze such as life-course BMI42–45 and other population characteristics (e.g., sex, age, and BMI at baseline) may explain the patterns in IRs that we observed.
Consistent with previous studies, hip injury was associated with a higher IR of symptomatic hip OA17,18,22,24 after adjusting for the effect of race. For the three hip outcomes, those with hip injury had highest IRs across all characteristics that we analyzed. Therefore targeted interventions for hip OA prevention and self-management may greatly benefit those with hip injuries.
Compared with previous studies, the overall IRs of radiographic and severe radiographic hip OA are consistent with annual rates reported previously27–29. We found no other studies reporting IRs of hip pain/symptoms to compare with IRs of hip symptoms. Our overall IR of symptomatic hip OA was substantially higher than previous IR estimates based on health records of inpatient and outpatient visits for clinical care11,12, which may be conservative since a majority of adults with joint pain do not seek care for their symptoms46,47. Differences in study population characteristics and OA definitions also likely contribute to differences in estimates.
This study has several limitations. First, similar to most longitudinal studies, the results are in a small geographic area and may have limited generalizability to other populations. Second, death and loss to follow-up are common for longitudinal studies in older populations, particularly with longer follow-up intervals as in this study, and attrition in the JoCo OA was not trivial. Although we determined that selection bias resulting from attrition was likely small, there remains the possibility that we may not have accounted for other types of bias potentially associated with attrition. Third, because we estimated incident hip symptoms and hip OA outcomes, relatively rare conditions, we had insufficient numbers of cases and low power to detect some effects (e.g., hip injury) and assess differential patterns of association (i.e., interactions) by race.
This study also has several important strengths. First, we conducted a comprehensive, descriptive analysis of incident hip outcomes from which we have presented IRs of four hip OA-related outcomes for a large population-based prospective study. We estimated IRs for African Americans and whites, and we identified dramatically lower IRs of hip OA for African Americans, overall and across all subpopulations that we analyzed. These population-based IRs provide relatively more recent data to improve projections of costs, prevalence, and demand for health services in increasingly diverse populations. Secondly, we estimated IRs of hip symptoms which can substantially impair health even in the absence of radiographic signs of hip OA5. Knowing these IRs can help clinicians and public health professionals recognize additional high risk groups for intervention opportunities to reduce and prevent hip symptoms. Thirdly, we quantified IRs overall and by numerous sociodemographic characteristics and hip OA risk factors. Quantifying IRs can identify subpopulations in which the prevalence and consequent burden of hip OA is growing most rapidly in addition to determining those at increased risk of hip OA-related outcomes.
The IRs we present provide valuable insights to clinicians and public health practitioners in their ongoing efforts to reduce the future impact of hip OA. In the JoCo OA cohort, the IR of hip symptoms was high, and, compared with earlier estimates, we found substantially higher IRs of symptomatic hip OA. The IRs of radiographic and severe radiographic hip OA were similar to previous estimates. African Americans had low IRs of radiographic and symptomatic hip OA compared with whites. In addition to higher IRs among women (hip symptoms and symptomatic OA), oldest ages (radiographic and symptomatic OA), and those with hip injury (symptomatic OA), those with lower education had a higher IR of radiographic OA, and several of the highest IRs of hip symptoms occurred among those with lowest income and greatest BMI. Across outcomes, IRs were highest among those with a hip injury. Public health efforts should prioritize low-SES populations, obese adults, and those with a hip injury for further action and prevention of hip symptoms and hip OA.
Acknowledgments
The authors thank Ms Carol Patterson for her administrative support, Janice M. Woodard for coordinating the field work of the study, and participants and staff of the Johnston County Osteoarthritis Project who made this study possible.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Role of the funding source
Funding sources: The Johnston County Osteoarthritis Project is supported in part by cooperative agreements S043, S1734, and S3486 from the Centers for Disease Control (CDC) and Prevention/Association of Schools of Public Health; the NIAMS Multipurpose Arthritis and Musculoskeletal Disease Center grant 5-P60-AR30701; and the NIAMS Multidisciplinary Clinical Research Center grants -5 P60 AR49465 and P60-AR064166. A.S. Moss’ work was made possible by a contract with the National Association of Chronic Disease Directors (contract no. 117-1400-5).
Study sponsors had no involvement in study design, collection, analysis and interpretation of data, in the writing of the manuscript, or the decision to submit the manuscript for publication.
Contributions
A Susan Moss: conception and design; analysis and interpretation of the data; drafting of the article; critical revision of the article for important intellectual content; final approval of the article; statistical expertise; responsibility for the integrity of the work as a whole, from inception to finished article zbr3@cdc.gov.
Louise B Murphy: conception and design; analysis and interpretation of the data; critical revision of the article for important intellectual content; final approval of the article; responsibility for the integrity of the work as a whole, from inception to finished article lmurphy1@cdc.gov.
Charles G Helmick: conception and design; analysis and interpretation of the data; critical revision of the article for important intellectual content; final approval of the article; administrative, technical, or logistic support.
Todd A Schwartz: conception and design; analysis and interpretation of the data; critical revision of the article for important intellectual content; final approval of the article; statistical expertise; administrative, technical, or logistic support.
Kamil E Barbour: conception and design; analysis and interpretation of the data; critical revision of the article for important intellectual content; final approval of the article.
Jordan B Renner: critical revision of the article for important intellectual content; final approval of the article; collection and assembly of the data.
William Kalsbeek: conception and design; analysis and interpretation of the data; critical revision of the article for important intellectual content; final approval of the article; statistical expertise.
Joanne M Jordan: conception and design; analysis and interpretation of the data; critical revision of the article for important intellectual content; final approval of the article; provision of study materials or patients; obtaining of funding; administrative, technical, or logistic support; collection and assembly of the data.
Ethics
The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. The study was approved by the Institutional Review Boards of the University of North Carolina Schools of Medicine and Public Health, and the Centers for Disease Control and Prevention. All participants gave written informed consent at recruitment and follow-up.
Competing interests
Ms. Moss has nothing to disclose.
Dr. Murphy has nothing to disclose.
Dr. Helmick has nothing to disclose.
Dr. Schwartz has nothing to disclose.
Dr. Barbour has nothing to disclose.
Dr. Renner has nothing to disclose.
Dr. Kalsbeek has nothing to disclose.
Dr. Jordan reports personal fees from ProActiva, personal fees from Samumed, personal fees from Flexion, other from American College of Rheumatology Board of Directors, other from American College of Rheumatology Division Directors Task Force, other from American College of Rheumatology Committee on Training and Work Force, other from Chair, Chronic OA Management Initiative of US Bone and Joint Initiative, other from Chair, Osteoarthritis Research Society International Initiative on Recommendations on OA Clinical Trials, other from Executive Committee, Analgesic, Anesthetic, and Addiction Clinical Trial, other from Translations, Innovations, Opportunities, and Networks (ACTTION), a public-private partnership with the FDA, other from Deputy Editor, Osteoarthritis and Cartilage, outside the submitted work.
References
- 1.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83-A:1622–9. doi: 10.2106/00004623-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009;36:809–15. doi: 10.3899/jrheum.080677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birrell F, Croft P, Cooper C, Hosie G, Macfarlane G, Silman A. Health impact of pain in the hip region with and without radiographic evidence of osteoarthritis: a study of new attenders to primary care. The PCR Hip Study Group Ann Rheum Dis. 2000;59:857–63. doi: 10.1136/ard.59.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Odding E, Valkenburg HA, Algra D, Vandenouweland FA, Grobbee DE, Hofman A. Associations of radiological osteoarthritis of the hip and knee with locomotor disability in the Rotterdam Study. Ann Rheum Dis. 1998;57:203–8. doi: 10.1136/ard.57.4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta S, Hawker GA, Laporte A, Croxford R, Coyte PC. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology (Oxford) 2005;44:1531–7. doi: 10.1093/rheumatology/kei049. [DOI] [PubMed] [Google Scholar]
- 8.Gabriel SE, Crowson CS, Campion ME, O’Fallon WM. Indirect and nonmedical costs among people with rheumatoid arthritis and osteoarthritis compared with nonarthritic controls. J Rheumatol. 1997;24:43–8. [PubMed] [Google Scholar]
- 9.Barbour KE, Lui LY, Nevitt MC, Murphy LB, Helmick CG, Theis KA, et al. Hip osteoarthritis and the risk of all-cause and disease-specific mortality in older women: population-based cohort study. Arthritis Rheumatol. 2015;73:1798–805. doi: 10.1002/art.39113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323–30. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 11.Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38:1134–41. doi: 10.1002/art.1780380817. [DOI] [PubMed] [Google Scholar]
- 12.Wilson MG, Michet CJ, Jr, Ilstrup DM, Melton LJ., 3rd Idiopathic symptomatic osteoarthritis of the hip and knee: a population-based incidence study. Mayo Clin Proc. 1990;65:1214–21. doi: 10.1016/s0025-6196(12)62745-1. [DOI] [PubMed] [Google Scholar]
- 13.Kopec JA, Sayre EC, Schwartz TA, Renner JB, Helmick CG, Badley EM, et al. Occurrence of radiographic osteoarthritis of the knee and hip among African Americans and whites: a population-based prospective cohort study. Arthritis Care Res (Hoboken) 2013;65:928–35. doi: 10.1002/acr.21924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scher DL, Belmont PJ, Jr, Mountcastle S, Owens BD. The incidence of primary hip osteoarthritis in active duty US military servicemembers. Arthritis Rheum. 2009;61:468–75. doi: 10.1002/art.24429. [DOI] [PubMed] [Google Scholar]
- 15.Prieto-Alhambra D, Judge A, Javaid MK, Cooper C, Diez-Perez A, Arden NK. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. 2014;73:1659–64. doi: 10.1136/annrheumdis-2013-203355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Body mass index in young men and the risk of subsequent knee and hip osteoarthritis. Am J Med. 1999;107:542–8. doi: 10.1016/s0002-9343(99)00292-2. [DOI] [PubMed] [Google Scholar]
- 17.Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med. 2000;133:321–8. doi: 10.7326/0003-4819-133-5-200009050-00007. [DOI] [PubMed] [Google Scholar]
- 18.Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635–46. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 19.Lievense AM, Bierma-Zeinstra SM, Verhagen AP, van Baar ME, Verhaar JA, Koes BW. Influence of obesity on the development of osteoarthritis of the hip: a systematic review. Rheumatology (Oxford) 2002;41:1155–62. doi: 10.1093/rheumatology/41.10.1155. [DOI] [PubMed] [Google Scholar]
- 20.Reijman M, Pols HA, Bergink AP, Hazes JM, Belo JN, Lievense AM, et al. Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann Rheum Dis. 2007;66:158–62. doi: 10.1136/ard.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grotle M, Hagen KB, Natvig B, Dahl FA, Kvien TK. Obesity and osteoarthritis in knee, hip and/or hand: an epidemiological study in the general population with 10 years follow-up. BMC Musculoskelet Disord. 2008;9:132. doi: 10.1186/1471-2474-9-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Juhakoski R, Heliovaara M, Impivaara O, Kroger H, Knekt P, Lauren H, et al. Risk factors for the development of hip osteoarthritis: a population-based prospective study. Rheumatology (Oxford) 2009;48:83–7. doi: 10.1093/rheumatology/ken427. [DOI] [PubMed] [Google Scholar]
- 23.Lohmander LS, Gerhardsson de Verdier M, Rollof J, Nilsson PM, Engstrom G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population-based prospective cohort study. Ann Rheum Dis. 2009;68:490–6. doi: 10.1136/ard.2008.089748. [DOI] [PubMed] [Google Scholar]
- 24.Richmond SA, Fukuchi RK, Ezzat A, Schneider K, Schneider G, Emery CA. Are joint injury, sport activity, physical activity, obesity, or occupational activities predictors for osteoarthritis? A systematic review J Orthop Sports Phys Ther. 2013;43:515–B519. doi: 10.2519/jospt.2013.4796. [DOI] [PubMed] [Google Scholar]
- 25.Mork PJ, Holtermann A, Nilsen TI. Effect of body mass index and physical exercise on risk of knee and hip osteoarthritis: longitudinal data from the Norwegian HUNT Study. J Epidemiol Community Health. 2012;66:678–83. doi: 10.1136/jech-2011-200834. [DOI] [PubMed] [Google Scholar]
- 26.Birrell F, Lunt M, Macfarlane G, Silman A. Association between pain in the hip region and radiographic changes of osteoarthritis: results from a population-based study. Rheumatology (Oxford) 2005;44:337–41. doi: 10.1093/rheumatology/keh458. [DOI] [PubMed] [Google Scholar]
- 27.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage. 2011;19:1270–85. doi: 10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 28.Lane NE, Lin P, Christiansen L, Gore LR, Williams EN, Hochberg MC, et al. Association of mild acetabular dysplasia with an increased risk of incident hip osteoarthritis in elderly white women: the study of osteoporotic fractures. Arthritis Rheum. 2000;43:400–4. doi: 10.1002/1529-0131(200002)43:2<400::AID-ANR21>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 29.Reijman M, Hazes JM, Pols HA, Koes BW, Bierma-Zeinstra SM. Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam Study. Arthritis Rheum. 2005;52:787–93. doi: 10.1002/art.20886. [DOI] [PubMed] [Google Scholar]
- 30.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–80. [PubMed] [Google Scholar]
- 31.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murphy LB, Helmick CG, Schwartz TA, Renner JB, Tudor G, Koch GG, et al. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthritis Cartilage. 2010;18:1372–9. doi: 10.1016/j.joca.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shao J, Tu D. The Jackknife and Bootstrap. New York, NY, USA: Springer Verlag; 1995. [Google Scholar]
- 34.Rust KF, Rao JN. Variance estimation for complex surveys using replication techniques. Stat Methods Med Res. 1996;5:283–310. doi: 10.1177/096228029600500305. [DOI] [PubMed] [Google Scholar]
- 35.Miller RG. Simultaneous Statistical Inference. 2nd. New York: Springer-Verlag; 1981. [Google Scholar]
- 36.Murphy LB, Moss S, Do BT, Helmick CG, Schwartz TA, Barbour KE, et al. Annual incidence of knee symptoms and four knee osteoarthritis outcomes in the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2016;68:55–65. doi: 10.1002/acr.22641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thiem U, Lamsfuss R, Gunther S, Schumacher J, Baker C, Endres HG, et al. Prevalence of self-reported pain, joint complaints and knee or hip complaints in adults aged >/= 40 years: a cross-sectional survey in Herne, Germany. PLoS One. 2013;8:e60753. doi: 10.1371/journal.pone.0060753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cleveland RJ, Schwartz TA, Prizer LP, Randolph R, Schoster B, Renner JB, et al. Associations of educational attainment, occupation, and community poverty with hip osteoarthritis. Arthritis Care Res (Hoboken) 2013;65:954–61. doi: 10.1002/acr.21920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reyes C, Garcia-Gil M, Elorza JM, Mendez-Boo L, Hermosilla E, Javaid MK, et al. Socio-economic status and the risk of developing hand, hip or knee osteoarthritis: a region-wide ecological study. Osteoarthritis Cartilage. 2015;23:1323–9. doi: 10.1016/j.joca.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 40.Lubbeke A, Duc S, Garavaglia G, Finckh A, Hoffmeyer P. BMI and severity of clinical and radiographic signs of hip osteoarthritis. Obesity (Silver Spring) 2009;17:1414–9. doi: 10.1038/oby.2008.663. [DOI] [PubMed] [Google Scholar]
- 41.Oliveria SA, Felson DT, Cirillo PA, Reed JI, Walker AM. Body weight, body mass index, and incident symptomatic osteoarthritis of the hand, hip, and knee. Epidemiology. 1999;10:161–6. [PubMed] [Google Scholar]
- 42.Apold H, Meyer HE, Espehaug B, Nordsletten L, Havelin LI, Flugsrud GB. Weight gain and the risk of total hip replacement a population-based prospective cohort study of 265,725 individuals. Osteoarthritis Cartilage. 2011;19:809–15. doi: 10.1016/j.joca.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 43.Holliday KL, McWilliams DF, Maciewicz RA, Muir KR, Zhang W, Doherty M. Lifetime body mass index, other anthropometric measures of obesity and risk of knee or hip osteoarthritis in the GOAL case-control study. Osteoarthritis Cartilage. 2011;19:37–43. doi: 10.1016/j.joca.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 44.Wang Y, Wluka AE, Simpson JA, Giles GG, Graves SE, de Steiger RN, et al. Body weight at early and middle adulthood, weight gain and persistent overweight from early adulthood are predictors of the risk of total knee and hip replacement for osteoarthritis. Rheumatology (Oxford) 2013;52:1033–41. doi: 10.1093/rheumatology/kes419. [DOI] [PubMed] [Google Scholar]
- 45.Abbate LM, Jordan JM. Weight change in osteoarthritis. Osteoarthritis Cartilage. 2012;20:268–70. doi: 10.1016/j.joca.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 46.Thorstensson CA, Gooberman-Hill R, Adamson J, Williams S, Dieppe P. Help-seeking behaviour among people living with chronic hip or knee pain in the community. BMC Musculoskelet Disord. 2009;10:153. doi: 10.1186/1471-2474-10-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paskins Z, Sanders T, Hassell AB. What influences patients with osteoarthritis to consult their GP about their symptoms? A narrative review BMC Fam Pract. 2013;14:195. doi: 10.1186/1471-2296-14-195. [DOI] [PMC free article] [PubMed] [Google Scholar]


