Abstract
Objective:
To evaluate the outcomes of lengthening post-traumatic femoral segments using a recently available magnetic intramedullary (IM) lengthening system.
Design:
Retrospective cohort study.
Setting:
Urban level II Trauma Center.
Patients/Participants:
Patients treated for post-traumatic femoral shortening at our institution between 2012 and 2015. We identified 17 femurs lengthened (14 men and 3 women). The mean age was 30 years (range, 11–72 years).
Intervention:
Magnetic IM lengthening system.
Main Outcome Measurements:
Amount of lengthening achieved, consolidation index, and complications encountered.
Results:
The mean follow-up was 2.2 years (range, 1–3.7 years). Sixteen patients achieved the planned lengthening, a mean of 3.8 cm (range, 2.3–6.0 cm). Regenerate consolidation occurred at a mean of 119 days (range, 57–209 days). The mean consolidation index was 32 d/cm (range, 16–51 d/cm). Three patients (18%) experienced complications.
Conclusion:
IM lengthening nails are an improvement over external fixators for treatment of post-traumatic femoral shortening. Within certain limits, their use can be extended to problems of limb-length discrepancy with angular/rotational deformity.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Key Words: post-traumatic, femur, lengthening, intramedullary
INTRODUCTION
Post-traumatic limb-length discrepancies (LLDs) are challenging problems for orthopaedic surgeons.1 These deformities may result from bone loss, comminution, bayonet apposition, malunion, bone debridement due to infection, or premature growth arrest in cases of pediatric growth plate fractures. In addition to the challenges associated with lengthening in post-traumatic bones, these cases may be complicated by scarring and/or retained hardware from previous procedures.1
Distraction osteogenesis has been frequently used to correct post-traumatic limb shortening.2 Previous studies have described successful outcomes using external fixation devices such as the Ilizarov and other circular or monolateral fixators.3,4 However, many complications such as joint stiffness, muscle contracture, pin site infection, regenerate bone fracture postframe removal, and patient dissatisfaction have been reported with external fixation.5 Many of these issues are related to limb lengthening itself, and others are specifically a byproduct of the external fixator. Internal lengthening techniques have been developed in an attempt to eliminate the need for external fixation and to minimize the complications. Alternatives include lengthening over nail,6 lengthening over plate,7 lengthening and then plating,8 and lengthening and then nailing.9 However, serious complications such as deep infections, refractures, and axial deviation were still observed.10–12
Lengthening with fully implantable intramedullary (IM) nails is an alternative technique devised to decrease complications and increase patient satisfaction.13 The PRECICE intramedullary limb lengthening system (NuVasive Specialized Orthopedics Inc, Aliso Viejo, CA) received FDA 510K approval in 2011. The PRECICE nail provides accurate distraction and compression using an internal rare earth magnet controlled by a handheld external remote controller (ERC).14,15 It is the only FDA-approved device in its class currently available in the United States. The purpose of this study is to evaluate the effectiveness of the PRECICE nail in treating post-traumatic femoral shortening.
PATIENTS AND METHODS
After obtaining institution review board approval, we retrospectively evaluated all patients who underwent lengthening using the PRECICE lengthening system between January 2012 and September 2015 and had a minimum of 1-year follow-up. A total of 115 patients were initially identified in this period. From this group, we identified 4 tibial and 17 femoral cases with post-traumatic etiologies. We excluded the low number tibia cases because of the low number of cases and the statistical inability to compare them with the larger femur group. A total of 17 patients (14 men and 3 women) with post-traumatic femur etiologies were finally included in this study. The mean age was 30 years (range, 11–72 years). The etiology was post-traumatic growth arrest in 35% of the cases (6 patients), growth arrest postvascular trauma during infancy in 6% of the cases (1 patient), and post-traumatic malunion with shortening in 59% of the cases (10 patients) (Fig. 1).
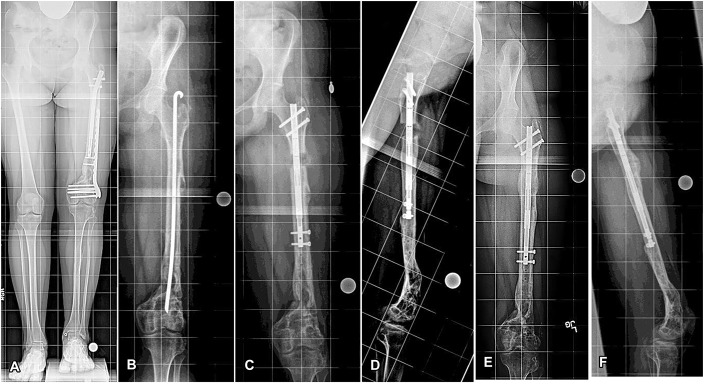
FIGURE 1.
A–F, (Case #9) 16-year-old girl with 4-cm discrepancy post left comminuted femoral healed fracture due to motor vehicle accident. A, Healed fracture with failed previous attempt at another hospital to lengthen with the ISKD nail. B, After hardware removal and prophylactic IM Rush rod fixation for 4.5 months. C and D, 1 month after lengthening using the PRECICE nail. E and F, Complete consolidation and healing 5 months post PRECICE insertion and 4 cm lengthening (Used with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
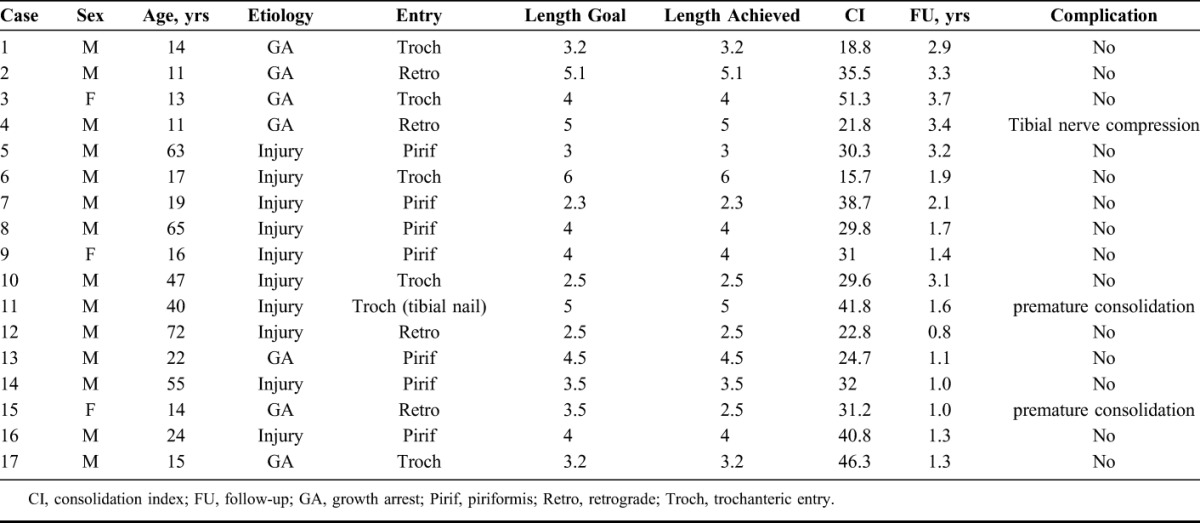
We used trochanteric entry in 6 and piriformis fossa entry in 7 femurs. Four rods were inserted retrograde. The mean goal of lengthening was 3.8 cm (range, 2.3–6.0 cm). The mean follow-up was 2.2 years (range, 1–3.7 years) (Table 1).
TABLE 1.
Patient Data
Preoperative planning and x-ray evaluation were performed by the senior authors. Identification of the osteotomy site was planned according to the nail length in relation to the bony segment length. Osteotomy sites were planned if possible at the level of the apex of the malunion. Whenever possible, we avoided sclerotic post-traumatic areas. Perioperative antibiotic prophylaxis was prescribed for all patients: Cefazolin IV injection (1 hour preoperative dose and every 6 hours for 24 hours postoperatively). In case of Penicillin sensitivity, we used Clindamycin IV injection (1 hour preoperative dose and every 8 hours for 24 hours postoperatively). For thromboembolic prophylaxis, we used subcutaneous enoxaparin sodium (40 mg) once a day or a 325 mg of aspirin once a day for 2–4 weeks. Patients began lengthening with the ERC after 5–7 days latency. The ERC was initially programmed to distract the femur by 1 mm/d in 0.25 mm steps. This rate was adjusted if needed according to the regenerate bone quality at each follow-up radiograph (every 10–14 days during the distraction phase).
Patients were prescribed regular physiotherapy visits (3–5 times per week) to maintain active and passive joint motion and to prevent soft-tissue contracture. Extension splints were used to prevent knee flexion contracture. Partial weight-bearing (20–25 kg) was allowed until consolidation was confirmed by radiographs. Full weight-bearing was permitted after 3 of 4 cortices in the AP and lateral radiographs were bridged.
RESULTS
Sixteen patients achieved the desired length, a mean of 3.8 cm (range, 2.3–6.0 cm). Only 1 patient achieved 2.5 cm instead of the planned 3.5 cm because of premature consolidation; the patient refused surgery for re-osteotomy. Complete regenerate consolidation with full weight-bearing occurred at a mean of 119 days (range, 57–209 days). The mean consolidation index (number of days from surgery until consolidation divided by the length achieved) was 32 d/cm (range, 16–51 d/cm) (Table 1). Twelve of the 17 patients (71%) had their nails removed in a mean of 1.1 years (range, 0.7–2.5 years) after surgery. The other patients have been recommended to remove their nails.
Three patients (18%) developed complications. One patient developed premature consolidation resulting in proximal nail migration. This was managed with a repeat osteotomy and nail exchange 45 days after the index surgery (Fig. 2). The second patient had premature consolidation after she achieved 2.5 cm (the goal was 3.5 cm), and the patient refused another surgery for re-osteotomy for the remaining 1 cm discrepancy. The third patient presented 10 days after femoral lengthening surgery with an ulcer on the posteromedial aspect of the lower leg due to pressure from a postoperative splint. The ulcer showed excellent healing but the patient began having increased symptoms of posterior tibial nerve compression with paresthesias and pain. One month after the index surgery, a tarsal tunnel decompression was performed and the nerve recovered. All complications were resolved without permanent sequelae (Table 1).
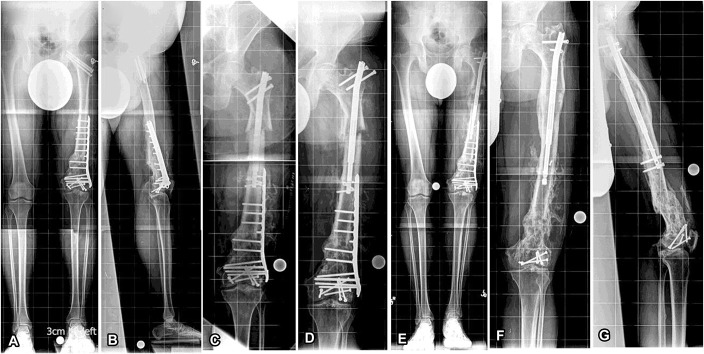
FIGURE 2.
A–G, (Case # 11) 40-year-old man with post-traumatic left femoral shortening 5 cm. A and B, Preoperative photos showing the implants for fracture fixation. C, Immediate postoperative radiograph with the PRECICE nail inserted. D, Premature consolidation with proximal migration of the nail (40 days after surgery). E, Re-osteotomy with rod exchange to resume lengthening (55 days after surgery). Tibial nail used for different locking patterns. F and G, Post-consolidation and distal plate removal (Used with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
DISCUSSION
The concept of distraction osteogenesis using the Ilizarov apparatus has been successfully used as the gold standard for treating limb shortening or deformity correction.16,17 Despite its success, the Ilizarov technique requires long-term placement of an external fixator, which is associated with many complications.18,19 IM limb lengthening has emerged as an accepted alternative to external fixators.13 However, not every case is suitable for IM lengthening nails. Post-traumatic LLD is a common complaint and occurs usually because of bone loss, post-debridement, or growth arrest in skeletally immature patients.3 Limb lengthening in post-traumatic cases is challenging to orthopaedic specialists. This might be due to the possibility of bony and soft-tissue compromise as a result of the initial trauma and management.
This study has limitations. First, it is a retrospective study. Second, as this is a preliminary experience with a new device, the small size of our cohort is a limitation. Third, the study included only femur cases. Femurs are known to provide better outcomes and fewer complications than tibia cases because of anatomical considerations. Because of the very low number of available tibia cases, we excluded the tibia. Conclusions from these data cannot be assumed to be transferrable to the tibia. Another limitation is that the population is heterogeneous, with the youngest patient being 11 years and the oldest being 72 years old. Finally, the short follow-up for some of our patients is another potential limitation, but the PRECICE nail was only recently introduced to the market, hence, longer follow-up is not yet possible.
There is limited literature describing the results of lengthening lower limbs in post-traumatic cases using the Fitbone telescope active actuator nail (TAA; Wittenstein intens GmbH, Igersheim, Germany), the Intramedullary Skeletal Kinetic Distractor (ISKD; Orthofix, Lewisville, TX), and the PRECICE IM nail.15,20–23 To the best of our knowledge, no studies have purely reported the use of lengthening with implantable IM devices for post-traumatic LLD.
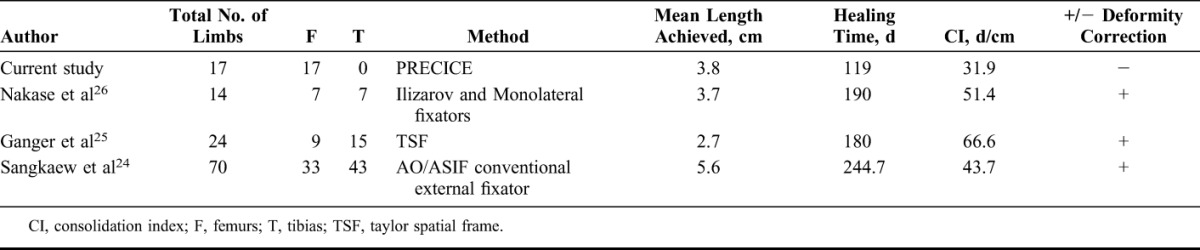
Previous literature describing post-traumatic lower limb lengthening with different methods of external fixation has shown various results regarding the consolidation time (Table 2). Sangkaew24 evaluated patients who underwent lengthening with or without deformity correction (76 post-traumatic lower limb segments; 33 femurs and 43 tibias) using the AO/ASIF conventional external fixator. At a distraction rate of 1 mm in 1 step on alternate days (1 mm/48 hours), he reported an average bone healing time of 244.7 days (range, 60–836 days) with an average new bone formation of 5.6 cm (range, 1–17 cm). Ganger et al25 assessed 24 post-traumatic lower limb segments (9 femurs and 15 tibias) undergoing lengthening +/− deformity correction using the Taylor Spatial Frame (TSF; Smith and Nephew, TN). With the mean amount of lengthening of 2.7 cm (range, 3–6.1 cm), they reported a mean time for bone healing of 180 days (range, 63–318 days). Similarly, Nakase et al26 achieved mean lengthening of 3.7 cm (range, 1.5–12 cm) in patients treated using external fixators for post-traumatic epiphyseal growth arrest. They reported the mean healing index of 190 days (range, 112–355 days). In the literature, there is a direct relationship between the amount of lengthening and the healing time. As more lengthening is achieved, longer healing time of the regenerate and soft-tissue complications should be expected.11 In this study, all of our patients were treated with the PRECICE lengthening nail and had a mean lengthening of 3.8 cm (range, 2.3–6 cm). The mean bone healing time was 119 days (range, 57–209 days). Our mean total consolidation index was less than the previous studies (Table 2). This may be attributed in part to the senior authors' technique of performing multiple drill holes at the osteotomy site before reaming. This enables IM reamings to exit and surround the osteotomy site, acting as pre-positioned bone graft. However, our study included only femurs, so it might be difficult to compare our faster healing times to other lengthening devices in the literature if they included tibias, which may heal more slowly.
TABLE 2.
Healing Index in the Literature
PRECICE nail breakage has been reported in a case report.27 Other complications of failure to distract (nail related) and premature consolidation (not nail related) had been reported in another study of 17 femurs that underwent lengthening with the PRECICE nail.15 Tiefenboeck et al,28 in their study had 7 of 10 patients (70%) with complications post-lengthening with the PRECICE nail; 3 of these were nail failure and breakage. In our series, 3 segments encountered major complications, none of which were implant related. As part of the treatment for complex post-traumatic cases, many patients underwent previous surgeries that may contribute to our complications. One of our complications was premature consolidation of the femur (Fig. 2), which might be anticipated during the process of lengthening regardless of the device, particularly in multiply operated limbs.29–31 This case had femoral shortening post-femoral shaft fracture (healed after distal femur internal fixation) and femoral neck fracture (healed in varus after internal fixation by screws). We intended to use trochanteric entry to avoid unwanted stress through the femoral neck. At index surgery, bone corticotomy resulted in a medial butterfly fragment, which caused the osteotomy to tilt into varus. The unusually large surface area of this comminuted corticotomy led to rapid healing (premature consolidation). Re-osteotomy with correction of the deformity and nail exchange was then performed and lengthening was resumed successfully without further complications. The second complication was tibial nerve compression behind the medial malleolus, unrelated to the process of femoral lengthening but due to pressure from the healed ulcer due to the postoperative splint. This was resolved by tarsal tunnel decompression, without permanent sequelae.
External fixators have been associated with implant-related complications during lower limb lengthening of post-traumatic cases. Nakase et al26 in their series (n = 14 limbs; 7 femurs and 7 tibias) reported the complications of superficial pin tract infection (4 segments), deep infection (1 segment), secondary deformity in regenerate bone after lengthening (2 segments), and fracture after fixator removal (1 segment). Song et al10 in their series of femoral lengthening over nail reported 3 cases of deep infection and required early removal of the nail. Ganger et al25 in their series reported 36 implant-related complications. Of these, 32 were pin-tract infection, 3 were axial deviation, and 1 was late bowing after frame removal. Similarly, Jürgens et al,32 in their study on post-traumatic lower limb lengthening using the Ilizarov frame in 10 segments reported complications of 6 segments with pin tract infection (2 of which developed local osteomyelitis) and 1 segment with wire breakage.
Ilizarov's fundamental principles must still be followed even with internal lengthening. IM lengthening nails (particularly, the PRECICE IM limb lengthening system) avoid the common external-fixation-related complications due to the obvious absence of pin sites. Also, IM stability prevents postlengthening deformity and fractures. Specifically in femurs, IM fixation is much more comfortable than external fixation because of the soft-tissue considerations. Therefore, our preliminary results demonstrate that IM lengthening nails may be useful tools in our armamentarium for treatment of femoral post-traumatic injuries. No specific implant-related complications were observed in our cohort. However, further trials with bigger cohorts are warranted to assess the effectiveness of lengthening nails used in conjunction with acute angular/rotational correction. Furthermore, studies on larger cohorts and other long bones should be considered to confirm our results.
ACKNOWLEDGMENTS
The following companies supported our institution's annual course for orthopaedic surgeons: Acumed, Brainlab, DePuy Synthes, Integra, MHE Coalition, NuVasive, Orthofix, OrthoPediatrics, Smith & Nephew, Stryker, and Zimmer Biomet. The following companies supported our institution's nonprofit organization (the Save-A-Limb Fund), which provides financial assistance to our patients: Stryker, Metro Prosthetics, and CS Medical Supply. S. C. Standard: Royalties from NuVasive and Pega Medical; J. D. Conway: Research support from Medtronic Sofamor Danek, Kinetic Concepts, Inc., and CD Diagnostics. Royalties from University of Florida. Consultant for Biomet, DePuy Synthes, and Cerament; J. E. Herzenberg: Research support from NuVasive. Consultant for OrthoPediatrics, Orthofix, NuVasive, and Smith & Nephew. For the remaining authors, no conflicts of interest were declared. Study performed at Sinai Hospital, Baltimore, MD.
Footnotes
Presented in part at the Annual Meeting of Extremity War Injuries X, January 26–28, 2015, Washington, DC, and at the first ILLRS Meeting, November 4–7, 2015, Miami, FL.
Author disclosures are available in the Acknowledgment at the end of the article.
REFERENCES
- 1.Schep NW, van Lieshout EM, Patka P, et al. Long-term functional and quality of live assessment following post-traumatic distraction osteogenesis of the lower limb. Strateg Trauma Limb Reconstr. 2009;4:107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polyzois VD, Stathopoulos IP, Lampropoulou-Adamidou K, et al. Strategies for managing bone defects of the lower extremity. Clin Podiatr Med Surg. 2014;31:577–584. [DOI] [PubMed] [Google Scholar]
- 3.Adegbehingbe OO, Ojo OD, Abiola PO, et al. Distraction by a monotube fixator to achieve limb lengthening: predictive factors for tibia trauma. J Trauma Manag Outcomes. 2013;7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79:1243–1258. [DOI] [PubMed] [Google Scholar]
- 5.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 6.Jasiewicz B, Kacki W, Tesiorowski M, et al. Results of femoral lengthening over an intramedullary nail and external fixator [in Polish]. Chir Narzadow Ruchu Ortop Pol. 2008;73:177–183. [PubMed] [Google Scholar]
- 7.Kulkarni R, Singh N, Kulkarni GS, et al. Limb lengthening over plate. Indian J Orthop. 2012;46:339–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cha SM, Shin HD, Kim KC, et al. Plating after tibial lengthening: unilateral monoaxial external fixator and locking plate. J Pediatr Orthop B. 2013;22:571–576. [DOI] [PubMed] [Google Scholar]
- 9.Lan X, Zhang L, Tang P, et al. S-osteotomy with lengthening and then nailing compared with traditional Ilizarov method. Int Orthop. 2013;37:1995–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song HR, Oh CW, Mattoo R, et al. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop. 2005;76:245–252. [DOI] [PubMed] [Google Scholar]
- 11.Shyam AK, Song HR, An H, et al. The effect of distraction-resisting forces on the tibia during distraction osteogenesis. J Bone Joint Surg Am. 2009;91:1671–1682. [DOI] [PubMed] [Google Scholar]
- 12.El-Husseini TF, Ghaly NA, Mahran MA, et al. Comparison between lengthening over nail and conventional Ilizarov lengthening: a prospective randomized clinical study. Strateg Trauma Limb Reconstr. 2013;8:97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rozbruch SR, Birch JG, Dahl MT, et al. Motorized intramedullary nail for management of limb-length discrepancy and deformity. J Am Acad Or Surg. 2014;22:403–409. [DOI] [PubMed] [Google Scholar]
- 14.Shabtai L, Specht SC, Standard SC, et al. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472:3860–3868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirane YM, Fragomen AT, Rozbruch SR. Precision of the PRECICE internal bone lengthening nail. Clin Orthop Relat Res. 2014;472:3869–3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jordan CJ, Goldstein RY, McLaurin TM, et al. The evolution of the Ilizarov technique: part 1: the history of limb lengthening. Bull Hosp Jt Dis. 2013;71:89–95. [PubMed] [Google Scholar]
- 17.Goldstein RY, Jordan CJ, McLaurin TM, et al. The evolution of the Ilizarov technique: part 2: the principles of distraction osteosynthesis. Bull Hosp Jt Dis. 2013;71:96–103. [PubMed] [Google Scholar]
- 18.Papakostidis C, Bhandari M, Giannoudis PV. Distraction osteogenesis in the treatment of long bone defects of the lower limbs: effectiveness, complications and clinical results; a systematic review and meta-analysis. Bone Joint J. 2013;95:1673–1680. [DOI] [PubMed] [Google Scholar]
- 19.Pipitone PS, Rehman S. Management of traumatic bone loss in the lower extremity. Orthop Clin North Am. 2014;45:469–482. [DOI] [PubMed] [Google Scholar]
- 20.Al-Sayyad MJ. Lower limb lengthening and deformity correction using the Fitbone motorized nail system in the adolescent patient. J Pediatr Orthop B. 2012;21:131–136. [DOI] [PubMed] [Google Scholar]
- 21.Krieg AH, Lenze U, Speth BM, et al. Intramedullary leg lengthening with a motorized nail. Acta Orthop. 2011;82:344–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burghardt RD, Herzenberg JE, Specht SC, et al. Mechanical failure of the intramedullary skeletal kinetic distractor in limb lengthening. J Bone Joint Surg Br. 2011;93:639–643. [DOI] [PubMed] [Google Scholar]
- 23.Karakoyun O, Küçükkaya M, Sökücü S. Intramedullary skeletal kinetic distractor in lower extremity lengthening. Acta Orthop Traumatol Turc. 2014;48:307–312. [DOI] [PubMed] [Google Scholar]
- 24.Sangkaew C. Distraction osteogenesis for the treatment of post traumatic complications using a conventional external fixator. A novel technique. Injury. 2005;36:185–193. [DOI] [PubMed] [Google Scholar]
- 25.Ganger R, Radler C, Speigner B, et al. Correction of post-traumatic lower limb deformities using the Taylor spatial frame. Int Orthop. 2010;34:723–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakase T, Yasui N, Kawabata H, et al. Correction of deformity and shortening due to post traumatic epiphyseal arrest by distraction osteogenesis. Arch Orthop Trauma Surg. 2007;127:659–663. [DOI] [PubMed] [Google Scholar]
- 27.Tiefenböck TM, Wozasek GE. Unusual complication with an intramedullary lengthening device 15 months after implantation. Injury. 2015;46:2069–2072. [DOI] [PubMed] [Google Scholar]
- 28.Tiefenboeck TM, Zak L, Bukaty A, et al. Pitfalls in automatic limb lengthening - first results with an intramedullary lengthening device. Orthop Traumatol Surg Res. 2016;102:851–855. [DOI] [PubMed] [Google Scholar]
- 29.Lascombes P, Popkov D, Huber H, et al. Classification of complications after progressive long bone lengthening: proposal for a new classification. Orthop Traumatol Surg Res. 2012;98:629–637. [DOI] [PubMed] [Google Scholar]
- 30.Nogueira MP, Paley D, Bhave A, et al. Nerve lesions associated with limb-lengthening. J Bone Joint Surg Am. 2003;85:1502–1510. [DOI] [PubMed] [Google Scholar]
- 31.Kocaoglu M, Eralp L, Kilicoglu O, et al. Complications encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86:2406–2411. [DOI] [PubMed] [Google Scholar]
- 32.Jürgens C, Kortmann HR, Fink B, et al. Treatment of post-traumatic limb shortening [in German]. Unfallchirurg. 1992;95:551–555. [PubMed] [Google Scholar]