Abstract
Background
Preserving cognitive function is an important public health issue. We investigated whether dietary pattern associates with cognitive function in middle-age.
Methods
We studied 2435 participants in the community-based Coronary Artery Risk Development in Young Adults (CARDIA) study of black and white men and women aged 18–30 in 1985–86 (year 0, Y0). We hypothesized that a higher A Priori Diet Quality Score, measured at Y0 and Y20, is associated with better cognitive function measured at Y25. The diet score incorporated 46 food groups (each in servings/day) as the sum of quintile ranks of food groups rated beneficial, 0 for food groups rated neutral, and reversed quintile ranks for food groups rated adverse; higher score indicated better diet quality. Y25 cognitive testing included verbal memory (Rey Auditory-Verbal Learning Test (RAVLT)), psychomotor speed (Digit Symbol Substitution Test (DSST)) and executive function (Stroop).
Results
Per 10-unit higher diet score at Y20, the RAVLT was 0.32 words recalled higher, the DSST was 1.76 digits higher, and the Stroop was 1.00 seconds+errors lower (better performance) after adjusting for race, sex, age, clinic, and energy intake. Further adjustment for physical activity, smoking, education, and body mass index attenuated the association slightly. Diet score at Y0 and increase in diet score over 20 years were also positively associated with each cognitive test.
Conclusions
A higher quality dietary pattern was associated with better cognitive function 5 years and even 25 years later in apparently healthy middle-aged adults.
Keywords: Cohort study, epidemiology, middle age, diet pattern, cognitive tests
Introduction
Cognitive function declines with aging (1). With social, economic and health care development, by 2050, 22% of the world population is expected to be over 60 years old (2) and the prevalence of cognitive function impairment will likely increase worldwide. Cognitive impairment is linked with high risk of dementia and stroke, and is a major threat to independence in the elderly (3, 4). Therefore, understanding preservation of cognitive function throughout adulthood is an important public health issue.
Healthy dietary patterns have been associated with slower decline of cognitive function and lower risk of dementia or cognitive impairment in older adults (5–18). Higher adherence to a Mediterranean diet was associated with slower cognitive decline measured by mini–mental state examination (MMSE), but not with cognitive decline assessed by other cognitive tests or with risk for incident dementia (13). In another study of 732 subjects over 60 years old, adherence to a Mediterranean diet was not significantly associated with MMSE score (12). Recently, a cross-sectional study in middle-aged Caucasians found that a food pattern rich in fruits, vegetables, dried legume and fish associated with lower risk of cognitive deficit than other food patterns rich in processed meat, fried foods, sweetened desserts, and high-fat dairy products (19). However, no prospective study has assessed a healthy dietary pattern and cognitive function in middle-age. Primary prevention in young adulthood or middle age could postpone cognitive function decline. Given the discrepancy in previous studies and limited evidence in young and middle-aged adults, prospective studies investigating this association are needed.
The A Priori Diet Quality Score (20) represents a diet pattern that was inversely related to oxidative stress (21) and circulating cellular adhesion molecule concentration (22) in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Higher scores predicted lower total, cardiovascular disease, cancer, and other “inflammatory-related” mortality in the Iowa Women’s Health Study (23). We therefore assumed that it would also relate to cognitive function. Here we investigated the association between the A Priori Diet Quality Score and cognitive function among apparently healthy middle-aged CARDIA participants. We hypothesized that a higher diet quality score 5 years before or even 25 years before would be associated with better cognitive function at midlife. Prior studies in CARDIA showed that both greater subclinical atherosclerotic calcification and ideal cardiovascular health were associated with better cognitive function (24, 25). The findings of our study further expand our understanding of cognitive function in CARDIA.
Subjects and Methods
Study design
CARDIA is a multi-center longitudinal cohort study of cardiovascular risk factors in adults between 18 and 30 years old at enrollment (1985–1986, year 0 (Y0)). Recruitment was at random from the general population in Birmingham, AL, Chicago, IL, and Minneapolis, MN, and from Kaiser Permanente Medical Care Plan members in Oakland, CA. The full CARDIA sample (n=5,115) at baseline was balanced by age (45% 18–24 years old), race (52% African American; 48% white), sex (46% men), and education (40% completed ≤12 years) (26–28). The 7 follow-up examinations at Y2, Y5, Y7, Y10, Y15, Y20 and Y25 had 91%, 86%, 81%, 79%, 74%, 72% and 72% of the surviving cohort returning, respectively. Of 3122 participants who attended Y0, Y20 and Y25 exams, 2573 assessed diet at Y0 and Y20 and measured cognitive function at Y25. 2435 participants without missing covariate values were analyzed (figure 1).
Figure 1.
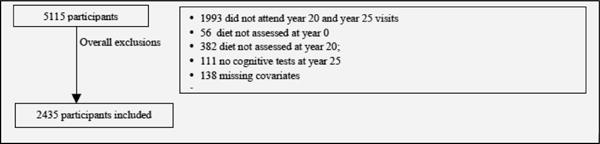
Flow chart: sample for the primary analyses
Dietary Pattern Assessment
Diet was assessed at Y0 and Y20 by using the interviewer administered CARDIA Diet History(29). The A Priori Diet Quality Score was derived from 46 foods groups as previously described (20–22, 30) (computational details in Online supplementary text and supplementary Tables 1 and 2). The score is based on classification of foods groups according to hypothesized health effects as beneficial (n=20, for example fruit, vegetables, legumes, low fat dairy products, fish, poultry, coffee, tea and moderate amount of alcoholic drinks), adverse (n = 13, for example fried foods, high fat meat, salty snacks, desserts, high fat dairy products, and soft drinks), or neutral (n = 13, for example lean meat, shellfish, potato, eggs, chocolate, fruit juices and diet beverages). Food groups considered beneficial or adverse were categorized into quintiles, and study participants received a score of 0–4 for each group reflecting increasing consumption. When non-consumption was common, nonconsumers were coded 0 and consumers were split into quartiles with scores from 1 to 4. The A Priori Diet Quality Score was the sum of category scores 0–4 for the beneficial food groups plus scores in reverse order (4–0) for adverse food groups (neutral food groups score 0). Higher score indicates better diet quality (theoretical maximum=132). A one-unit change in the score was a change of one category of one food group in the presumed beneficial direction. To study change in diet score, we used the cutoffs of food group categories as determined at Y0, which were then applied to dietary data at Y0 and Y20 (20, 21).
Cognitive function assessment
Cognitive function was measured at Y25. 1) The Rey Auditory Verbal Learning Test (RAVLT) assesses the ability to memorize and to retrieve words (verbal memory) (31). The number of words correctly recalled after the long delay (10 min) was used in the analyses. A higher number of words recalled (range 0 to 15) indicated better performance. 2) The Digit Symbol Substitution Test (DSST) assesses psychomotor speed, sustained attention, and working memory(32). A higher number of digits correctly substituted (range 0 to 133) indicated better performance. 3) The Stroop Test evaluates executive function by assessing the ability to view complex visual stimuli and to respond to one dimension while suppressing the response to another dimension (33). The test was scored by the time to correctly state ink color (e.g., yellow) of color words (e.g., the word blue) plus number of errors; thus, a higher score (seconds plus errors) indicated worse performance.
At Y2, two tests (reverse star tracing and the Atari Breakout video game) were conducted to elicit reactive blood pressure; although not intended as cognitive tests, these tests involve general cognitive agility. 1) In star-tracing, subjects traced the outline of a star from a reversed image displayed in a mirror while staying within narrow limits, with the stylus always on the apparatus. If subjects moved out of the limits of the star, an error was scored automatically. The participants drew forward stars as quickly as possible with the fewest possible errors. Total stars completed over three minutes and number of errors were recorded and constituted a Y2 cognitive score. The cognitive task of reversing an image and eye-hand coordination resembles the task in the Stroop test. 2) The Atari Breakout video game tests eye-hand coordination and psychomotor skill. Video game performance is considered an objective alternative psychomotor test closely related to Wechsler Adult Intelligence Scale executive intelligence score and Stroop test score(34–36). The average of up to 9 games completed within 3 minutes was used to compute the Y2 cognitive score.
Measurements of other variables
Age, race, sex, education levels, and cigarette smoking were obtained by self- and interviewer-administered questionnaires at each clinic visit (27, 37). Physical activity was measured at each examination by an interviewer-based questionnaire, and the frequency and intensity of 13 activities were used to calculate “Exercise Units” (38,39). Body weight was measured using a balance beam scale and height using a vertically mounted metal centimeter ruler and a metal carpenter’s square. Body mass index (BMI) was weight(kg)/height(m)2. Seated blood pressure was the average of the last two of three measurements after 5 minutes rest (27). Blood glucose and total cholesterol were measured by standard procedures (27). Diabetes diagnosis was fasting glucose level ≥126 mg/dL, self-report of antidiabetic medication, or a 2-h postload glucose ≥200 mg/dL (the last at Y10 and Y20 only) (40). Apolipoprotein E4 genotype was measured by the modified method of Kamboh et al. (41).
Statistical Analysis
Statistical analyses used SAS 9.2 (SAS Institute Inc., Cary, NC). Multiple linear regressions modeled the associations of Y0 and Y20 diet score with cognitive function tests at Y25. Age, race, sex, clinic, energy intake, physical activity, smoking, maximum education attained through Y25, BMI, blood pressure, total cholesterol, and diabetes were included in the models as potential confounders. A sensitivity analysis also adjusted for apolipoprotein E4 phenotype, which was assayed at CARDIA year 7 (n = 2176). Interactions between diet score and race, sex, and education were assessed by adding cross-product terms. A composite cognitive function score at Y2 was computed by averaging the 3 Z scores for the average Atari Breakout game score, the number of stars completed, and the negative of the number of errors in star tracing. A composite cognitive function score at Y25 was the average of the 3 Z scores for the average number of words recalled in RAVLT, digits correctly substituted in DSST, and negative of Stroop test score (details in Online Supplementary Table 3). The correlation coefficient between the two composite cognitive scores measured 23 years apart was 0.31. The Y2 composite cognitive function score was included as a covariate to adjust for baseline cognitive function. Statistical testing was two-sided with type I error =0.05.
Results
The 2435 participants had average age 25 at Y0 and 45 at Y20. Among them 403 (16.6%) were black men, 649 (26.7%) were black women, 639 (26.2%) were white men, and 744 (30.6%) were white women. The cohort was apparently healthy in terms of Y0 lifestyle and clinical measures (Table 1). Correlation between RAVLT and DSST was 0.3, between RAVLT and Stroop test was −0.3, and between DSST and Stroop test was −0.5.
Table 1.
A Priori Dietary Quality Score, cognitive function tests, and baseline characteristics (N=2435), CARDIA
| Mean(SD)/% | |
|---|---|
| Baseline (Year 0) Characteristics | |
| Age (years) | 25.2(3.6) |
| Black (%) | 43.2% |
| Women (%) | 57.2% |
| Energy intake (1000 * kcal/d) | 2.7(1.2) |
| Physical activity score (exercise units) | 420.4(293.5) |
| Smoking status | |
| Never smoker (%) | 62.3% |
| Former smoker (%) | 14.4% |
| Current smoker (%) | 23.3% |
| Maximum education attained through Year 25 (years in school) | 15.9(2.5) |
| BMI (kg/m2) | 24.3(4.7) |
| Hypertension (%) | 3.4% |
| Total cholesterol (mg/dl) | 177.3(32.7) |
| Diabetes (%) | 0.4% |
| A Priori Diet Quality Score | |
| Year 0 | 64.0 (13.2) |
| Year 20 | 71.1(12.7) |
| Year 20 – Year 0 | 7.0(11.5) |
| Year 25 Cognitive Function | |
| Rey Auditory-Verbal Learning Test (Words correctly recalled) | 8.6(3.2) |
| Digit Symbol Substitution Test (Digits correctly substituted) | 71.1(15.7) |
| Stroop Test(Seconds + errors to correctly name colors) | 43.6(12.0) |
Per 10-unit higher diet score at Y20, 0.32 (SE=0.05, P<0.0001) more words were correctly recalled on the RAVLT, 1.76 (SE=0.26, P<0.0001) more digits were correctly substituted in DSST, and 1.00 (SE=0.20, P<0.0001) lower score was obtained on the Stroop test at Y25, after accounting for race, sex, age, study center, and energy intake (Table 1, model 1). Further adjustment for physical activity, smoking, maximum education attained through Y25 (Table 1, model 2), and subsequently for BMI, blood pressure, total cholesterol, and diabetes (Table 1, model 3) attenuated the results slightly. The difference in model 3 between the 4th and 1st quartile of Y20 diet score corresponds to 23.7%, 12.9%, and 8.7% of a sample SD for the RAVLT, DSST, and Stroop test scores, respectively (also see Online Supplementary Table 3 for results for the composite year 25 cognitive score). Further adjustment for apolipoprotein E4 (per 10-unit higher diet score at Y20, 0.22 for RAVLT, 0.76 for DSST and −0.65 for the Stroop test, all P <0.05, N=2176) yielded similar findings. The three cognitive tests were more closely associated with diet assessed at Y20 (5 years earlier) than at Y0 (25 years earlier, 0.32 vs 0.29 for RAVLT, 1.76 vs 1.41 for DSST and −1.00 vs −0.73 for the Stroop test) (Table 1, model 1). Analysis of quartiles of diet score at Y20 (cutpoints: 62, 71, 81) showed monotonic improvement in the cognitive tests in all three models (P<0.05), while quartiles of diet score at Y0 showed monotonic improvements in all three models for RAVLT and DSST (P<0.05) but not for Stroop test. No significant interactions were identified between Y0 and Y20 diet scores and race or sex (all P>0.05 with df=1 for diet-race and diet-sex interactions). In an exploratory analysis, we found that the association between diet score and DSST performance tended to be of a smaller magnitude in participants who were college graduates or received graduate level education than in those with less than a college degree (P for interaction = 0.04 at Y0 and 0.01 at Y20). Education did not modify the relation between diet pattern and either RAVLT or Stroop test scores (P for interaction >0.05). A sensitivity analysis altered the A Priori Diet Quality Score by adding chocolate to the list of beneficially-rated foods; findings were similar to those presented here.
In addition, a 10-unit higher Y0 diet score was associated with 5% SD higher Y2 cognitive function Z score after adjusting for race, sex, age, study center, and energy intake (P=0.004). However the association lost its significance after further adjustment for educational attainment. Additional adjustment for Y2 cognitive function Z score in the analysis of Y0 diet score predicting Y25 cognitive test scores yielded similar magnitude of associations between Y0 diet score and performance in the three tests as is reported in Table 2.
Table 2.
Prospective association between Y0 and Y20 A Priori Diet Quality Score and Y25 cognitive function, N=2435
| RAVLT (Words) | DSST (Digits) | Stroop
Test (Seconds+Errors) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Slope¶ | SE | P | Slope | SE | P | Slope | SE | P | |
| Year 0 | |||||||||
| Diet Score(10 units) | |||||||||
| Model* | 0.29 | 0.06 | <0.0001 | 1.41 | 0.27 | <0.0001 | −0.73 | 0.21 | 0.0006 |
| Model 2† | 0.18 | 0.06 | 0.002 | 0.55 | 0.26 | 0.04 | −0.34 | 0.22 | 0.12 |
| Model 3‡ | 0.16 | 0.06 | 0.004 | 0.46 | 0.26 | 0.08 | −0.25 | 0.22 | 0.25 |
| Year 20 | |||||||||
| Diet Score(10 units) | |||||||||
| Model 1 | 0.32 | 0.05 | <0.0001 | 1.76 | 0.26 | <0.0001 | −1.00 | 0.20 | <0.0001 |
| Model 2 | 0.21 | 0.06 | 0.0002 | 0.83 | 0.26 | 0.002 | −0.62 | 0.21 | 0.004 |
| Model 3 | 0.21 | 0.06 | 0.0003 | 0.82 | 0.26 | 0.002 | −0.58 | 0.22 | 0.007 |
| Year 20–Year 0 | |||||||||
| Diet Score(10 units) | |||||||||
| Model 1 | 0.23 | 0.06 | <0.0001 | 1.42 | 0.29 | <0.0001 | −0.85 | 0.23 | 0.0002 |
| Model 2 | 0.16 | 0.06 | 0.008 | 0.70 | 0.29 | 0.01 | −0.57 | 0.23 | 0.01 |
| Model 3 | 0.16 | 0.06 | 0.01 | 0.70 | 0.29 | 0.01 | −0.55 | 0.23 | 0.02 |
“Slope” is the difference in the indicated cognitive function test score per 10 units of the A Priori Diet Quality Score;
Model 1 adjusted for age, race, sex, center of clinic visit, and energy intake; for change in A Priori Diet Quality Score over 20 years, the baseline score was a covariate;
Model 2 further adjusted for physical activity, smoking, and maximum education attained through Y25;
Model 3 further adjusted for body mass index, blood pressure, total cholesterol, and diabetes.
Furthermore, change in the A Priori Diet Quality Score from Y0 to Y20 was also associated with Y25 cognitive function tests. Each 10 unit increase in diet score over 20 years was associated with 0.24 (SE=0.06, P<0.0001) more words correctly recalled on the RAVLT, 1.40 (SE=0.29, P<0.0001) more digits correctly substituted on the DSST, and an 0.85 (SE=0.23, P=0.0002) lower Stroop test score at Y25, after accounting for race, sex, age, center of clinic visit, energy intake, and Y0 diet score (Table 2). Further adjustment attenuated the associations. The difference in model 3 between the 4th quartile and 1st quartile of the change of diet score over 20 years corresponds to 11.8%, 11.9%, and 10.4% of the sample SD of the test score in the RAVLT, DSST, and Stroop test, respectively. Analysis across quartiles of the change of the A Priori Diet Quality Score from Y0 to Y20 (cutpoints: 0, 7, 15) yielded significant monotonic gradation for the DSST and Stroop test (P<0.05), but not for the RAVLT (P>0.05).
Discussion
In the current study, higher A Priori Diet Quality Score at average age 45 years, and even at average age 25 years, was positively associated with better performance in cognitive function tests, including RAVLT, DSST, and Stroop test assessed at average age 50 years. The improvement of diet score over 20 years was associated with all three cognitive function tests. Furthermore, the more recent diet score tended to be more strongly associated with cognitive function assessed in middle-age. These findings support a role for diets favoring, for example, phytochemical-rich plant foods, low fat dairy products, fish, poultry, and less processed foods in preventing cognitive declines in middle age.
Our results are consistent with those of recent studies showing that a healthy dietary pattern which includes higher intake of fruit, vegetables, fish, nuts and legumes, and lower intake of meats, sweets and high fat dairy is related to better cognitive function, slower deterioration of cognitive function, and lower risk of dementia or cognitive impairment in subjects older than 65 years old (5–16, 18). In addition, in a cross-sectional study of 4693 Caucasian adults aged 35–55 years, a “whole food pattern”, a diet rich in fruit, vegetables, and fish, was associated with lower odds of cognitive deficit compared to a ‘processed food’ pattern, a diet rich in processed meat, chocolate, sweeteners, desserts, fried food, refined grains, and high fat dairy products (19). Though different approaches have been used to define a healthy dietary pattern throughout the literature, including Mediterranean Diet (9–11), DASH diet (17), healthy diet indicator (6, 7), and whole food pattern (19), healthy dietary constituents are generally similar across studies. Higher intake of fruit, vegetables, fish, nuts and legumes and lower intake of meats, high fat dairy and sweets are generally considered to be part of a healthy dietary pattern.
There are few studies of improvements in dietary pattern and subsequent cognitive function. In a randomized trial of 124 sedentary and overweight or obese participants with prehypertension or hypertension, the DASH diet alone for 4 months resulted in improved psychomotor speed measured by a battery of cognitive tests, including DSST and Stroop test, than usual diet control(17). Our observational findings of a positive association between the improvement of diet over 20 years and cognitive function 5 years after the second diet assessment bolster the above findings, cautioning that baseline and followup cognitive function tests differed in our study.
We have shown in prior CARDIA studies that higher dietary score is associated with less oxidative stress and lower concentrations of circulating cellular adhesion molecules (21, 22), which could mean that the vasculature throughout the body is healthier with high diet score. In the Iowa Women’s Health Study, a study of post-menopausal women with mean age of 61, this diet score was inversely associated with total death including CVD death and chronic inflammatory related death (23), therefore those with higher diet score were less vulnerable from CVD and chronic inflammation. CARDIA has shown that ideal cardiovascular health was associated with better cognitive function (25). Therefore, a better diet score, which tends to preserve overall cardiovascular health may help to preserve cognitive function at an older age, may also help to preserve cognitive function in middle age. In CARDIA, women, whites, and those who received higher education tended to have higher diet scores, although this sociodemographic discrepancy tended to attenuate over years (20).
Given the large, community-based sample, our findings generalize to young to middle-aged U.S. whites and African Americans. Our findings are important for understanding the underlying mechanism of the development of cognitive function in early and middle adulthood given 25 years of follow-up and A Priori Diet Quality Score assessed at two examinations 20 years apart. Compared to previous prospective studies in the elderly(9–11), it is unlikely that dietary choice at average ages 25 and 45 were influenced by subclinical cognitive impairment. On the other hand, several limitations of this proposed study should be noted. One limitation is that we could not completely control for baseline of the Y25 cognitive function measures. Y2 reverse star tracing and the Atari Breakout video game were not intended initially as cognitive tests though they seem to measure cognitive function. The absence of a true baseline cognitive function measure made it difficult to fully assess the temporality of the association between dietary pattern and cognitive function. Future CARDIA examinations will be needed to evaluate the temporality of this association. The absence of association between Y0 diet and the Y2 cognitive Z score is of interest in itself. Diet may be associated with aspects of cognitive function assessed in Y25, but unassociated with the ones captured by reverse star tracing and the Atari Breakout video game. However, this seems unlikely, because speed of processing and executive function, which were assessed in Y25, seem to be involved in the Y2 measures. More likely is that diet is not related to cognitive function in people of average age 27 years, and that the loss of cognitive function associated with diet observed by average age 50 reflects problems that accumulate over many years. Another limitation, as in all observational studies, is potential residual confounding due to unmeasured or unknown confounders. However, CARDIA collected information on a wide range of variables, limiting the potential for residual confounding.
In conclusion, we found that a higher quality dietary pattern measured by the A Priori Diet Quality Score was associated with better cognitive function 5 years and even 25 years later independent of other factors among apparently healthy middle-aged adults. Furthermore, dietary pattern improvement over 20 years was also associated with better cognitive function 5 years later. Maintaining or improving diet over the lifecourse may have the potential to prevent or at least delay future cognitive decline in older adulthood.
Supplementary Material
Acknowledgments
NZ, DRJ, LMS designed research; NZ and DRJ analyzed the data, NZ wrote the paper; NZ, DRJ, KAM, KH, LL, JPR, KY, SS, RAW, LMS had primary responsibility for final content. All authors read and approved the final manuscript.
Funding Support: The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute and the Intramural Research Program of the National Institute on Aging, as well as by a grant (R01-HL-053560).
Footnotes
Conflict of interest: Dr. Jacobs is a consultant for the California Walnut Commission. Dr. Yaffe reports grants from NIH, Alzheimer’s Association, Bright Focus Foundation, DOD, California Department of Public Health, personal fees from Takeda Pharmaceuticals, other from NIA, Beeson, personal fees from Novartis, outside the submitted work. The other authors have nothing to disclose.
Ethical standards: The institutional review boards for the protection of human subjects at each participating site approved the study, and written informed consent was obtained from all participants.
References
- 1.Smith R, Betancourt L, Sun Y. Molecular endocrinology and physiology of the aging central nervous system. Endocr Rev. 2005;26:203–250. doi: 10.1210/er.2002-0017. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Populations Divisions. Population aging and development. 2009:82. Updated. ESA/P/WP/212. [Google Scholar]
- 3.Gussekloo J, de Craen A, van Exel E, Bootsma-van der Wiel A, Westendorp R. Causes and consequences of cognitive decline in the very elderly the Leiden 85-plus study. Ned Tijdschr Geneeskd. 2004;148:979–983. [PubMed] [Google Scholar]
- 4.Ferrucci L, Guralnik JM, Salive ME, Pahor M, Corti MC, Baroni A, Havlik RJ. Cognitive impairment and risk of stroke in the older population. J Am Geriatr Soc. 1996;44:237–241. doi: 10.1111/j.1532-5415.1996.tb00908.x. [DOI] [PubMed] [Google Scholar]
- 5.Gu Y, Scarmeas N. Dietary patterns in Alzheimer’s disease and cognitive aging. Current Alzheimer Research. 2011;8:510–519. doi: 10.2174/156720511796391836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huijbregts PP, Feskens EJ, Räsänen L, Fidanza F, Alberti-Fidanza A, Nissinen A, Giampaoli S, Kromhout D. Dietary patterns and cognitive function in elderly men in Finland, Italy and the Netherlands. Eur J Clin Nutr. 1998;52:826–831. doi: 10.1038/sj.ejcn.1600654. [DOI] [PubMed] [Google Scholar]
- 7.Correa Leite M, Nicolosi A, Cristina S, Hauser W, Nappi G. Nutrition and cognitive deficit in the elderly: A population study. Eur J Clin Nutr. 2001;55:1053–1058. doi: 10.1038/sj.ejcn.1601270. [DOI] [PubMed] [Google Scholar]
- 8.Wengreen H, Neilson C, Munger R, Corcoran C. Diet quality is associated with better cognitive test performance among aging men and women. J Nutr. 2009;139:1944–1949. doi: 10.3945/jn.109.106427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scarmeas N, Luchsinger JA, Schupf N, Brickman AM, Cosentino S, Tang MX, Stern Y. Physical activity, diet, and risk of Alzheimer disease. JAMA. 2009;302:627–637. doi: 10.1001/jama.2009.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scarmeas N, Stern Y, Mayeux R, Manly J, Schupf N, Luchsinger J. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66:216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scarmeas N, Stern Y, Mayeux R, Luchsinger J. Mediterranean diet, Alzheimer disease, and vascular mediation. Arch Neurol. 2006;63:1709–1717. doi: 10.1001/archneur.63.12.noc60109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Psaltopoulou T, Kyrozis A, Stathopoulos P, Trichopoulos D, Vassilopoulos D, Trichopoulou A. Diet, physical activity and cognitive impairment among elders: The EPIC-Greece cohort (European Prospective Investigation into Cancer and Nutrition) Public Health Nutr. 2008;11:1054–1062. doi: 10.1017/S1368980007001607. [DOI] [PubMed] [Google Scholar]
- 13.Féart C, Samieri C, Rondeau V, Amieva H, Portet F, Dartigues JF, Scarmeas N, Barberger-Gateau P. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302:638–648. doi: 10.1001/jama.2009.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barberger-Gateau P, Raffaitin C, Letenneur L, Berr C, Tzourio C, Dartigues JF, Alpérovitch A. Dietary patterns and risk of dementia: The three-city cohort study. Neurology. 2007;69:1921–1930. doi: 10.1212/01.wnl.0000278116.37320.52. [DOI] [PubMed] [Google Scholar]
- 15.Samieri C, Jutand M, Feart C, Capuron L, Letenneur L, Barberger-Gateau P. Dietary patterns derived by hybrid clustering method in older people: Association with cognition, mood, and self-rated health. J Am Diet Assoc. 2008;108:1461–1471. doi: 10.1016/j.jada.2008.06.437. [DOI] [PubMed] [Google Scholar]
- 16.Gu Y, Nieves J, Stern Y, Luchsinger J, Scarmeas N. Food combination and Alzheimer disease risk: A protective diet. Arch Neurol. 2010;67:699–706. doi: 10.1001/archneurol.2010.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith PJ, Blumenthal JA, Babyak MA, Craighead L, Welsh-Bohmer KA, Browndyke JN, Strauman TA, Sherwood A. Effects of the dietary approaches to stop hypertension diet, exercise, and caloric restriction on neurocognition in overweight adults with high blood pressure. Hypertension. 2010;55:1331–1338. doi: 10.1161/HYPERTENSIONAHA.109.146795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan R, Chan D, Woo J. A cross sectional study to examine the association between dietary patterns and cognitive impairment in older Chinese people in Hong Kong. J Nutr Health Aging. 2013;17:757–65. doi: 10.1007/s12603-013-0348-5. [DOI] [PubMed] [Google Scholar]
- 19.Akbaraly T, Singh Manoux A, Marmot M, Brunner E. Education attenuates the association between dietary patterns and cognition. Dement Geriatr Cogn Disord. 2009;27:147–154. doi: 10.1159/000199235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sijtsma FP, Meyer KA, Steffen LM, Shikany JM, Van Horn L, Harnack L, Kromhout D, Jacobs DR., Jr Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: The Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr. 2012;95:580–586. doi: 10.3945/ajcn.111.020719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer KA, Sijtsma FP, Nettleton JA, Steffen LM, Van Horn L, Shikany JM, Gross MD, Mursu J, Traber MG, Jacobs DR., Jr Dietary patterns are associated with plasma F(2)-isoprostanes in an observational cohort study of adults. Free Radic Biol Med. 2013;57:201–9. doi: 10.1016/j.freeradbiomed.2012.08.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sijtsma FP, Meyer KA, Steffen LM, Van Horn L, Shikany JM, Odegaard AO, Gross MD, Kromhout D, Jacobs DR., Jr Diet quality and markers of endothelial function: The CARDIA study. Nutr Metab Cardiovasc Dis. 2014 Jan 17; doi: 10.1016/j.numecd.2013.12.010. pii: S0939-4753(14)00003-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mursu J, Steffen L, Meyer K, Duprez D, Jacobs D. Diet quality indices and mortality in postmenopausal women: The Iowa Women’s Health Study. Am J Clin Nutr. 2013;98:444–53. doi: 10.3945/ajcn.112.055681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reis JP, Launer LJ, Terry JG, Loria CM, Zeki Al Hazzouri A, Sidney S, Yaffe K, Jacobs DR, Jr, Whitlow CT, Zhu N, Carr JJ. Subclinical atherosclerotic calcification and cognitive functioning in middle-aged adults: the CARDIA study. Atherosclerosis. 2013;231:72–77. doi: 10.1016/j.atherosclerosis.2013.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reis JP, Loria CM, Launer LJ, Sidney S, Liu K, Jacobs DR, Jr, Zhu N, Lloyd-Jones DM, He K, Yaffe K. Cardiovascular health through young adulthood and cognitive functioning in midlife. Ann Neurol. 2013;73:170–179. doi: 10.1002/ana.23836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cutter GR, Burke GL, Dyer AR, Friedman GD, Hilner JE, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Manolio TA, et al. Cardiovascular risk factors in young adults. the CARDIA baseline monograph. Control Clin Trials. 1991;12(1 Suppl):1S–77S. doi: 10.1016/0197-2456(91)90002-4. [DOI] [PubMed] [Google Scholar]
- 27.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. CARDIA: Study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 28.Hughes GH, Cutter G, Donahue R, Friedman GD, Hulley S, Hunkeler E, Jacobs DR, Jr, Liu K, Orden S, Pirie P, et al. Recruitment in the coronary artery disease risk development in young adults (CARDIA) study. Control Clin Trials. 1987;8(4 Suppl):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 29.McDonald A, Van Horn L, Slattery M, Hilner J, Bragg C, Caan B, Jacobs D, Jr, Liu K, Hubert H, Gernhofer N, et al. The CARDIA dietary history: Development, implementation, and evaluation. J Am Diet Assoc. 1991;91:1104–1112. [PubMed] [Google Scholar]
- 30.Jacobs D, Tapsell L. Food synergy: The key to a healthy diet. Proc Nutr Soc. 2013;72:200–6. doi: 10.1017/S0029665112003011. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt M. Rey auditory verbal learning test: A handbook. Psychological Services. 1996 [Google Scholar]
- 32.Wechsler D. Wechsler adult intelligence scale-III (WAIS-III) Psychological Corporation. 1997 [Google Scholar]
- 33.Stroop J. Studies of interference in serial verbal reaction. J Exp Psychol. 1935;18:643. [Google Scholar]
- 34.Jones MB. Video games as psychological tests. Simulation & Gaming. 1984;15:131. [Google Scholar]
- 35.Lawrence V, Houghton S, Douglas G, Durkin K, Whiting K, Tannock R. Executive function and ADHD: A comparison of children’s performance during neuropsychological testing and real-world activities. Journal of attention disorders. 2004;7:137–149. doi: 10.1177/108705470400700302. [DOI] [PubMed] [Google Scholar]
- 36.Samoilovich S, Riccitelli C, Schiel A, Siedi A. Attitude of schizophrenics to computer videogames. Psychopathology. 1992;25:117–119. doi: 10.1159/000284761. [DOI] [PubMed] [Google Scholar]
- 37.Wagenknecht LE, Perkins LL, Cutter GR, Sidney S, Burke GL, Manolio TA, Jacobs DR, Jr, Liu KA, Friedman GD, Hughes GH, et al. Cigarette smoking behavior is strongly related to educational status: The CARDIA study. Prev Med. 1990;19:158–169. doi: 10.1016/0091-7435(90)90017-e. [DOI] [PubMed] [Google Scholar]
- 38.Jacobs DR, Hahn L, Haskell WL, Pirie P, Sidney S. Validity and reliability of short physical activity history: CARDIA study and the minnesota heart health program. J Cardiopulmonary Rehabil. 1989;9:448–459. doi: 10.1097/00008483-198911000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sidney S, Jacobs DR, Jr, Haskell WL, Armstrong MA, Dimicco A, Oberman A, Savage PJ, Slattery ML, Sternfeld B, Van Horn L. Comparison of two methods of assessing physical activity in the coronary artery risk development in young adults (CARDIA) study. Am J Epidemiol. 1991;133:1231–1245. doi: 10.1093/oxfordjournals.aje.a115835. [DOI] [PubMed] [Google Scholar]
- 40.Carnethon MR, Sternfeld B, Schreiner PJ, Jacobs DR, Jr, Lewis CE, Liu K, Sidney S. Association of 20-year changes in cardiorespiratory fitness with incident type 2 diabetes: The coronary artery risk development in young adults (CARDIA) fitness study. Diabetes Care. 2009;32:1284–1288. doi: 10.2337/dc08-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamboh MI, Ferrell RE, Kottke B. Genetic studies of human apolipoproteins. V. A novel rapid procedure to screen apolipoprotein E polymorphism. J Lipid Res. 1988;29:1535–1543. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


