Abstract
Background
Diagnosis of rectal evacuation disorders (RED) is currently based on anorectal manometry and evacuation tests in specialized laboratories; we recently showed higher rectal gas volume (RGV) and maximum rectal gas transaxial area (MRGTA) measured on abdominal and pelvic computed tomography (CT) in patients with documented RED.
Aim
To obtain cut-off values of RGV, MRGTA and rectal area on scout film (RASF) to differentiate constipated patients with RED from those without RED, based on anorectal manometry (ARM), balloon expulsion test (BET), and colon transit test.
Methods
We identified 118 constipated patients (65 with RED) with prior record of CT. Using standard CT software, we used a variable region of interest (ROI) program to measure RGV, MRTGA and RASF, as previously described. We constructed ROC curves based on different values, and we estimated AUC, specificity and positive predictive value (PPV) to detect RED in patients with constipation.
Key Results
ROCs of the models to predict RED showed AUC 0.751 for RGV and 0.737 for MRGTA (both p<0.001), and 0.623 for RASF (p=0.029). At specificity of 90%, RGV of 30mL had a PPV 77.3%, MRGTA of 10cm2 had a PPV 75.0%, and RFAS of 9cm2 had a PPV of 68.8% for identifying constipated patients with RED.
Conclusions and Inferences
Rectal gas measurements on abdominal imaging may indicate RED in patients with constipation. At ~90% specificity for RED, RGV of 20 or 30mL or MRGTA of 10cm2 on CT have PPV ~75%, and RASF of >9cm2 has PPV of ~69%.
Keywords: radiograph, colonic transit, specificity, area
Abbreviated abstract
Diagnosis of rectal evacuation disorders (RED) is currently based on anorectal manometry and evacuation tests in specialized laboratories; we recently showed higher rectal gas volume (RGV) and maximum rectal gas transaxial area (MRGTA) measured on abdominal and pelvic computer tomography (CT) in patients with documented RED. Our aim was to obtain cut-off values of RGV, MRGTA and rectal area on scout film to differentiate constipated patients with RED from those without RED, based on anorectal manometry, balloon expulsion test, and colon transit test. Rectal gas measurements on abdominal imaging may indicate RED in patients with constipation.
INTRODUCTION
Rectal evacuation disorders (REDs) account for approximately one-third of patients presenting with constipation in gastroenterology care (1). A recent population-based study showed that defecatory disorders are relatively common in the community, with the overall age of 19.3 per 100,000 person-years and the sex-adjusted incidence rate being 5-fold higher in women than in men (2). The most effective therapeutic approach to refractory constipation with RED is biofeedback therapy or pelvic floor retraining (3). To avoid laxative overuse in constipated patients with RED and to optimize treatment in these patients, an accurate diagnosis for RED is needed. Currently, the diagnosis of RED is based on anorectal manometry and evacuation tests (balloon, barium or MR defecography), which are not generally available in internal medicine or gastroenterology practices. Unfortunately, there is also considerable disagreement among tests used in the diagnosis of RED (4), and also lack of standardization of the balloon expulsion test.
Therefore, in addition to careful clinical evaluation (5), including digital rectal examination which is best for dyssynergic defecation (6), it would be helpful to develop an easily accessible diagnostic tool with high specificity to select the patients with suspected RED for referral for specialized tests to confirm the diagnosis. There are several clinical pointers in the history and examination that can be used, such as 75% sensitivity of RED to identify dyssynergic defecation (6). Therefore, there is need for a test that can corroborate the clinical impression and support referral for specialized anorectal testing. One test that is often performed to exclude other diseases is abdominal and pelvic computerized tomography (CT).
We recently showed that, using abdomen and pelvis CT, the rectal gas volume (RGV) and maximal rectal gas transaxial area (MRGTA) were significantly greater in constipated patients with RED than in those without RED (7).
In the current study, our aim was to obtain the cut-off values of RGV and MRGTA on CT to differentiate constipated patients with RED from those without RED.
MATERIALS AND METHODS
Participant Data
We used the previously published data of 118 patients (102 females) with constipation evaluated by a single experienced gastroenterologist over 20 years. The patients’ mean age was 42.9 ± 16.2 years and BMI was 22.9 ± 3.9 kg/m2. These patients are in a cumulated cohort of over 1500 patients that has been fully characterized elsewhere (1, 8–9); less than 8% of patients in this cohort had undergone CT scans related to the constipation, and the CTs were performed (usually at the referring centers) for exclusion of organic diseases.
The patients had undergone anorectal manometry (ARM), balloon expulsion test (BET), and colon transit test, and they also had record of abdominal and pelvic CT (7). Three subgroups were identified: RED (n=65), slow transit (STC, n=17) and normal transit (NTC, n=38) constipation, based on the totality of the evidence by clinical findings and results of laboratory or radiological investigations.
Measurements of Rectal Gas
Using standard CT software, we used a variable region of interest (ROI) program on each cross-sectional CT image that contained rectum to measure the area of gas in each slice and summated the volumes for the entire rectal gas: RGV (mL)=Σ (area of ROI on each slice X thickness of each slice). The area of ROI was automatically computed using Quick Query radiographs and photographs, Electronic Analysis and Display Station (QREADs version 5.7.2). We standardized the vertical extent of rectal gas from the transaxial slice at the lower margin on the pubic symphysis to slice at the entry to the lower pelvis, that is, the lower margin of the sacroiliac joints (Figure 1). We also recorded the largest area shown on the transaxial slices of each patient as MRGTA and area of rectal gas (vertical) on the 2-dimensional abdominal film [scout film (RASF)] which is included in the standard CT imaging.
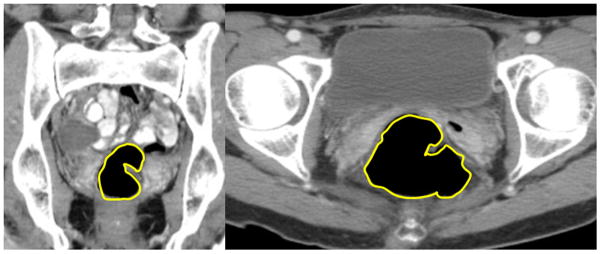
Figure 1.
Coronal image (left panel) and cross-sectional image on CT (right panel) from a 44 year-old female with rectal evacuation disorder. The rectal gas volume was 77.5mL and maximum rectal gas area was 22.2cm2.
Statistical Analysis
To assess the ability of RGV and MRGTA to predict RED, we tested the receiver operating characteristics (ROC) curve and estimated the area under the ROC curve (AUC); in addition, the specificity, sensitivity, positive predictive value (PPV) and negative predictive value (NPV) of different RGVs (10 to 50mL), MRGTAs (5 to 15cm2) and area of rectal gas on scout films (8 to 10cm2) were used to identify volume and area values that would have 90% specificity to predict, with at least 75% certainty (PPV), the presence of RED in patients with constipation. We selected optimization of specificity (>90%) over sensitivity because of the costs associated with specialized anorectal manometry and imaging (e.g. MRI) tests and, therefore, the need for high PPV and high specificity of the preliminary evaluation to avoid unnecessary costs that might be associated with selection of high sensitivity with low specificity.
RESULTS
We previously showed overall group differences between constipated patients with RED compared to non-RED for RGV, MRGTA and RASF, and the differences applied to comparisons of RED with both normal transit and slow transit constipation for RGV and MRGTA (both p<0.001) and RASF (p=0.031) (7). An example of the retained gas in the lower rectum is illustrated in Figure 1.
Receiver Operating Characteristic Curves
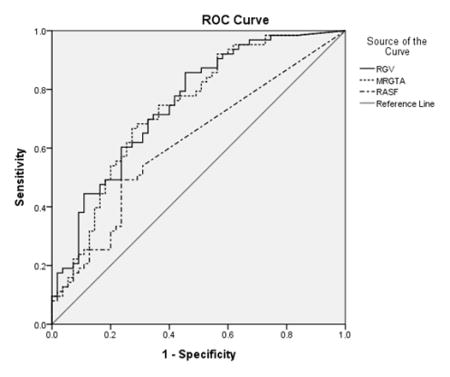
The ROC of the model of RGV for predicting RED showed AUC of 0.751 (95% CI 0.663–0.838, p<0.001, Figure 2). Similarly, the ROC of the model of MRGTA showed AUC of 0.737 (95% CI 0.651–0.83, p<0.001, Figure 2). The ROC of the model of rectal gas area on the scout film showed AUC of 0.623 (p=0.029, 95% CI 0.516~0.718, Figure 2).
Figure 2.
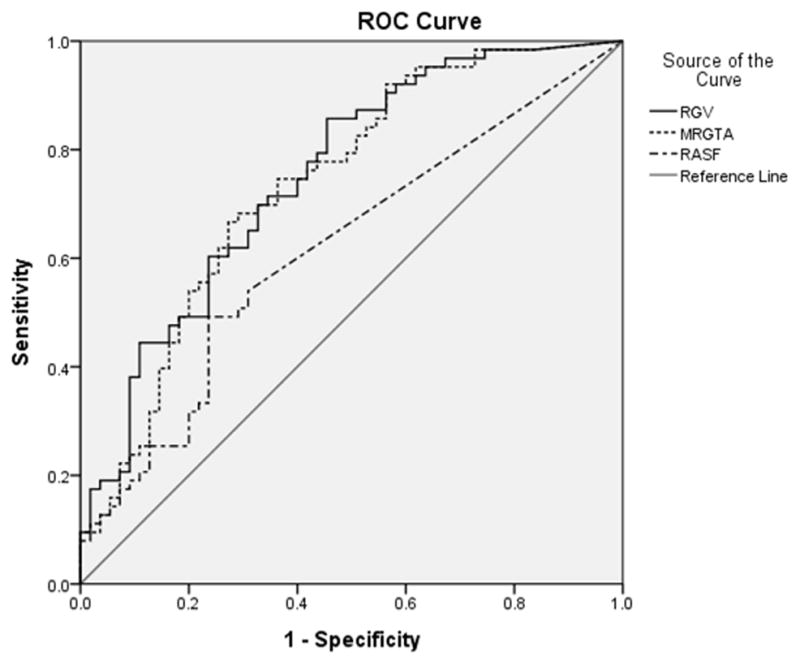
ROC curve of rectal gas volume, maximal rectal gas area, and area of rectal gas (vertical) on the 2-dimensional abdominal film (scout) to identify a rectal evacuation disorder. Note the two approaches have similar performance characteristics. RGV, rectal gas volume; MRGTA, maximum rectal gas transaxial area; RGA on scout, area of rectal gas on the 2-dimensional abdominal film (scout)
Cut-off Values for RGV and MRGTA with 90% Specificity for RED
We selected the cut-off values for RGV and MRGTA to achieve approximately 90% specificity to differentiate constipated patients with RED from those without RED on CT. Table 1 show the estimated sensitivity, specificity, PPV, NPV, and odds ratio for RGV, MRGTA, and rectal gas area on the scout film using the different cut-off values. For example, the cut-off values of 20 and 30mL for RGV had PPVs of 80.0% and 77.3% respectively, the MRGTA of 10cm2 had PPV of 75.0%, and the rectal gas area on scout film of 9cm2 had PPV of 68.8% for RED at about the same degree of specificity. Among these measurements, the RGV of 20mL was the most sensitive.
Table 1.
Diagnostic Accuracy According to Variable Cut-off Values for Rectal Gas Volume and Rectal Gas Maximum Area CT Images for Predicting Rectal Evacuation Disorders
| Cut-off value | Sensitivity | Specificity | PPV | NPV | OR (95% CI) |
|---|---|---|---|---|---|
| RGV>50mL | 17.5% | 96.4% | 84.6% | 50.5% | 5.6 (1.2~26.5) |
| RGV>40mL | 20.6% | 92.7% | 76.5% | 50.5% | 3.3 (1.0~10.9) |
| RGV>30mL | 27.0% | 90.9% | 77.3% | 52.8% | 3.7 (1.3~10.8) |
| RGV>20mL | 38.1% | 89.1% | 80.0% | 55.7% | 5.0 (1.9~13.5) |
| RGV>10mL | 54.0% | 76.4% | 72.3% | 59.2% | 3.8 (1.7~8.4) |
| MRGTA>15cm2 | 15.9% | 94.6% | 76.9% | 79.5% | 3.3 (0.9~12.6) |
| MRGTA>10cm2 | 24.6% | 90.9% | 75.0% | 52.1% | 3.1 (1.1~9.3) |
| MRGTA>5cm2 | 54.0% | 80.0% | 76.6% | 60.3% | 4.7 (2.1~10.7) |
| RGA on scout>8cm2 | 20.6% | 59.1% | 68.4% | 49.5% | 2.1 (0.75~6.0) |
| RGA on scout>9cm2 | 17.5% | 92.3% | 68.8% | 53.6% | 2.1 (0.7~6.5) |
| RGA on scout>10cm2 | 17.5% | 90.9% | 58.8% | 49.0% | 2.1 (0.7~6.5) |
RGV, rectal gas volume on CT; MRGTA, maximal rectal gas transaxial area on CT; RGA on scout, area of rectal gas on the 2-dimensional abdominal film (scout); PPV, positive predictive value; NPV, negative predictive value; OR, odd ratio; CI, confidence interval
DISCUSSION
Our study shows that an RGV of 20 or 30mL and an MRGTA of 10cm2 have positive predictive values of ≥75% at ~90% specificity for RED in constipated patients. These data complement our previous study (7), as we have identified the cut-off values that have high specificity and PPV to select patients with likelihood to suffer RED and, therefore, to pursue other physiologic studies to confirm RED.
A carefully performed digital rectal examination by a highly experienced expert is a good screening test, with 75% sensitivity and 87% specificity (6). However, it is operator dependent and even gastroenterologists fail to perform the rectal examination for a variety of reasons (10).
Among diagnostic tests, the balloon expulsion test (BET) is considered a useful screening test for RED (11), as it is the best simple assessment among functional studies to assess defecatory function in patients with constipation. Minguez et al. showed a high specificity of 89% and NPV of 97% for BET to identify constipated patients without pelvic floor dysfunction (12), suggesting that BET could be used as a ‘rule out’ screening test (13). However, in other studies and in clinical practice, it has been observed that many patients with dyssynergic defecation are able to expel the balloon by compensation for their impaired anal relaxation using a strong Valsalva maneuver that raises intraabdominal or intrarectal pressure and results in expulsion of the balloon. Therefore, normal BET does not always exclude a defecation disorder. In fact, a recent study showed the incomplete concordance between measurements on high resolution manometry or MRI defecography and balloon expulsion test (14). In addition, functional studies to appraise defecatory function, such as defecography using barium or MR, anorectal manometry (conventional or high resolution) and EMG, are usually available only in specialized laboratories of referral centers. Therefore, the availability of a technique to identify patients who should undergo further testing to conclusively diagnose RED is highly desirable.
Several radiologic studies such as plain abdominal x-ray with or without radiopaque markers, colonic transit by scintigraphy, and abdominopelvic CT are performed in patients with constipation (11. Among these modalities, abdominopelvic CT is commonly used to exclude organic problems such as an obstructing mass or stricture in patients presenting with constipation, or it may have been undertaken in different clinics for evaluation of many abdominopelvic organs, as in patients presenting with abdominal pain to clinics specializing in gastroenterology, nephrology, urology and gynecology. Previously, we showed that RGV on abdomen CT was greater in RED than in non-RED patients with constipation (7). We used the area of ROI on each cross-sectional CT image computed automatically by a software program available in standard CT equipment. This program was very simple and easily accessible for use by clinicians or radiologists, with good inter-observer and intra-observer reliability (7).
In this study, we estimated the cut-off values with high specificity and high PPV for RGV and MRGTA as well as the area on abdominal scout film, and we focused on high specificity because we perceived the need for a ‘rule-in’ screening test (13) with a ~10% likelihood of false positive rate in patients with RGV >20 mL or MRGTA>10 cm2 or RASF >9cm2 Therefore, if physicians detect entrapped rectal gas on CT or abdominal radiograph in patients with constipation, we recommend further clinical assessment by detailed history (5) and digital rectal examination to seek signs for RED and to seek to confirm the diagnosis with more detailed functional studies. Given that the negative predictive values are ~50% and sensitivities are ~25 to 35%, the cut-off values for RGV and MRGTA or RASF cannot be used as diagnostic tests for RED; similarly, RGV or MRGTA or RASF below the suggested cut-off values do not exclude RED.
In the future, we plan to perform prospective validation of rectal gas volume for screening of RED. Since our prior study (7) demonstrated validity of rectal area on the scout film of the CT scan to differentiate RED from non-RED constipation and the current analysis shows the rectal gas area of 9cm2 may indicate RED, we recommend prospective validation of plain abdominal and/or pelvic radiograph instead of abdominopelvic CT, given the radiation exposure and cost of abdominopelvic CT (15). Given the lack of standardization of BET methodology and variable sensitivity and specificity of that test, we anticipate that, with further prospective validation, the measurement of rectal gas area on a plain abdominal and/or pelvic radiograph will become a useful screening test for RED in patients with constipation.
KEY POINTS.
Diagnosis of rectal evacuation disorders (RED) requires specialized laboratory testing; assessment of rectal gas on abdominal imaging provides numerical indicators of likelihood of RED in patients with constipation
Our aim was to obtain cut-off values of rectal gas volume (RGV), maximum rectal gas transaxial area (MRGTA) and rectal area on scout films (RASF) to differentiate constipated patients with RED from those without RED.
In 118 constipated patients (65 with RED) with prior record of abdominopelvic CT, we used a variable region of interest (ROI) program to measure RGV, MRGTA and RASF.
Rectal gas measurements on abdominal imaging may indicate RED in patients with constipation. At ~90% specificity for RED, RGV of 20 or 30mL or MRGTA of 10cm2 on CT have PPV ~75%, and RASF of >9cm2 has PPV of ~69%.
Acknowledgments
Funding: Dr. Camilleri is supported by grant RO1-DK92179 from National Institutes of Health.
Competing interests: The authors have no competing interests.
Authors’ contributions:
Seon-Young Park: data retrieval from electronic medical records, authorship
Disha Khemani: data retrieval from electronic medical records, authorship
Andrés Acosta: data interpretation, authorship
Deborah Eckert: medical management of patients with senior investigator, clinical data verification
Michael Camilleri: concept, design, interpretation, authorship of manuscript
References
- 1.Nullens S, Nelsen T, Camilleri M, Burton D, Eckert D, Iturrino J, Vazquez-Roque M, Zinsmeister AR. Regional colon transit in patients with dys-synergic defaecation or slow transit in patients with constipation. Gut. 2012;61:1132–9. doi: 10.1136/gutjnl-2011-301181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noelting J, Eaton JE, Choung RS, Zinsmeister AR, Locke GR, 3rd, Bharucha AE. The incidence rate and characteristics of clinically diagnosed defecatory disorders in the community. Neurogastroenterol Motil. 2016;28:1690–7. doi: 10.1111/nmo.12868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bharucha AE, Rao SS. An update on anorectal disorders for gastroenterologists. Gastroenterology. 2014;146:37–45. doi: 10.1053/j.gastro.2013.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palit S, Thin N, Knowles CH, Lunniss PJ, Bharucha AE, Scott SM. Diagnostic disagreement between tests of evacuatory function: a prospective study of 100 constipated patients. Neurogastroenterol Motil. 2016;28:1589–98. doi: 10.1111/nmo.12859. [DOI] [PubMed] [Google Scholar]
- 5.Lembo T, Camilleri M. Chronic constipation. N Engl J Med. 2003;349:1360–8. doi: 10.1056/NEJMra020995. [DOI] [PubMed] [Google Scholar]
- 6.Tantiphlachiva K, Rao P, Attaluri A, Rao SS. Digital rectal examination is a useful tool for identifying patients with dyssynergia. Clin Gastroenterol Hepatol. 2010;8:955–60. doi: 10.1016/j.cgh.2010.06.031. [DOI] [PubMed] [Google Scholar]
- 7.Park S-Y, Khemani D, Nelson AD, Eckert D, Camilleri M. Rectal gas volume measured by computerized tomography identifies evacuation disorders in patients with constipation. Clin Gastroenterol Hepatol. 2016 Nov 14; doi: 10.1016/j.cgh.2016.11.013. pii: S1542-3565(16)31052-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shin A, Camilleri M, Nadeau A, Nullens S, Rhee JC, Jeong ID, Burton DD. Interpretation of overall colonic transit in defecation disorders in males and females. Neurogastroenterol Motil. 2013;25:502–8. doi: 10.1111/nmo.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park SY, Burton D, Busciglio I, Eckert D, Camilleri M. Regional colonic transit pattern does not conclusively identify evacuation disorders in constipated patients with delayed colonic transit. J Neurogastroenterol Motil. 2017;23:92–100. doi: 10.5056/jnm16066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong RK, Drossman DA, Bharucha AE, Rao SS, Wald A, Morris CB, Oxentenko AS, Ravi K, Van Handel DM, Edwards H, Hu Y, Bangdiwala S. The digital rectal examination: a multicenter survey of physicians’ and students’ perceptions and practice patterns. Am J Gastroenterol. 2012;107:1157–63. doi: 10.1038/ajg.2012.23. [DOI] [PubMed] [Google Scholar]
- 11.Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A. Functional anorectal disorders. Gastroenterology. 2016 Mar 25; doi: 10.1053/j.gastro.2016.02.009. pii: S0016-5085(16)00175-X. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minguez M, Herreros B, Sanchiz V, Hernandez V, Almela P, Añon R, Mora F, Benages A. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology. 2004;126:57–62. doi: 10.1053/j.gastro.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 13.Florkowski CM. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: communicating the performance of diagnostic tests. Clin Biochem Rev. 2008;29(Suppl 1):S83–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Prichard DO, Lee T, Parthasarathy G, Fletcher JG, Zinsmeister AR, Bharucha AE. High-resolution anorectal manometry for identifying defecatory disorders and rectal structural abnormalities in women. Clin Gastroenterol Hepatol. 2016 Oct 5; doi: 10.1016/j.cgh.2016.09.154. pii: S1542-3565(16)30866-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231:393–8. doi: 10.1148/radiol.2312030767. [DOI] [PubMed] [Google Scholar]