Abstract
For sputum analysis, the transfer of inflammatory cells from liquefied sputum samples to a culture medium or buffer solution is a critical step because it removes the inflammatory cells from the presence of residual dithiothreitol (DTT), a reagent that reduces cell viability and interferes with further sputum analyses. In this work, we report an acoustofluidic platform for transferring inflammatory cells using standing surface acoustic waves (SSAW). In particular, we exploit the acoustic radiation force generated from a SSAW field to actively transfer inflammatory cells from a solution containing residual DTT to a buffer solution. The viability and integrity of the inflammatory cells are maintained during the acoustofluidic-based cell transfer process. Our acoustofluidic technique removes residual DTT generated in sputum liquefaction and facilitates immunophenotyping of major inflammatory cells from sputum samples. It enables cell transfer in a continuous flow, which aids the development of an automated, integrated system for on-chip sputum processing and analysis.
The analysis of human sputum samples, the mucus within the airways of the lungs, is critical for the diagnosis and personalized treatment of pulmonary diseases such as tuberculosis, lung cancer, and asthma.1–3 For example, it has been increasingly recognized that the pathogenesis and clinical characteristics of asthma are heterogeneous, such that new therapeutic approaches may only be successful if they are targeted in a personalized fashion to individuals whose asthma is mediated by the targeted pathway.4 By analyzing the different cell populations found in sputum, researchers have identified the distinct immunological phenotypes associated with the disease.5 Identifying these phenotypes has led to hopes of developing individually tailored therapeutic treatments that will more effectively target the mechanisms unique to each phenotype.
Standard procedure for sputum liquefaction calls for the mixture of sputum samples with dithiothreitol (DTT), a strong reducing agent that decreases cell viability and interferes with further sputum analyses.6–8 Therefore, the inflammatory cells have to be transferred to a culture medium or buffer solution in order to avoid the negative effects of DTT on downstream sputum analysis.
Conventionally this cell transfer step is realized through centrifugation, which has several drawbacks. Centrifuges are bulky and sometimes expensive. They are often not suitable for resource-limited regions, where point-of-care diagnostics of pulmonary diseases are needed. In addition, in these centrifugation-based conventional sputum processing/analysis assays, sputum samples need to be handled manually by the operator, often in open air, and run through several instruments. This presents significant biosafety concerns to the operator. This also hinders the integration with continuous-flow components toward a fully automated sputum processing/analysis system. Moreover, the manual transfer of fluid upon centrifugation is prone to interoperator variability. With these drawbacks, there is a pressing demand for a biosafe, biocompatible, low-cost, automated, point-of-care platform to transfer the inflammatory cells from liquefied sputum samples to a culture medium or buffer solution in continuous flow.
With the advantages of low cost, miniaturization, and automation,9–13 microfluidics is suited to fulfill this unmet demand. Several microfluidic platforms for sputum liquefaction14 and analysis15–18 have already been demonstrated. However, the microfluidic transfer of inflammatory cells from liquefied sputum samples has not yet been demonstrated. Although various microfluidic techniques have been developed for the transfer of cells across flow streams,19–35 none of these techniques has been validated in transferring inflammatory cells from human sputum samples.
In this work, we demonstrate the first microfluidic platform for the transfer of inflammatory cells from liquefied human sputum samples. This cell transfer device is built upon our acoustofluidic (i.e., the fusion of acoustics and microfluidics) based cell manipulation platform.36–40 It features a tilted alignment between a microchannel and interdigital transducers (IDTs), which generate a standing surface acoustic wave (SSAW) field.38–40 Inflammatory cells present in liquefied human sputum samples are thereby transferred from the residual DTT solution to the buffer solution when SSAW is applied. This acoustofluidic cell transfer process decreases the concentration of DTT in sputum samples by 93% and thereby avoids the adverse effects of DTT on sputum analysis. Results from live/dead and histological staining show that our acoustofluidic device preserves the viability and integrity of transferred inflammatory cells, demonstrating the biocompatibility of our acoustofluidic-based inflammatory cell transfer platform. Moreover, flow cytometry analysis shows that the removal of residual DTT from liquefied sputum samples by our acoustofluidic approach yields better antibody labeling and accurate identification of major inflammatory cells. With the advantages of high biocompatibility, high biosafety, low cost, miniaturization, automation, and ease of in-line integration, our SSAW-based acoustofluidic platform is an excellent candidate for the development of an automated and fully integrated sputum processing/analysis system.41
WORKING MECHANISM
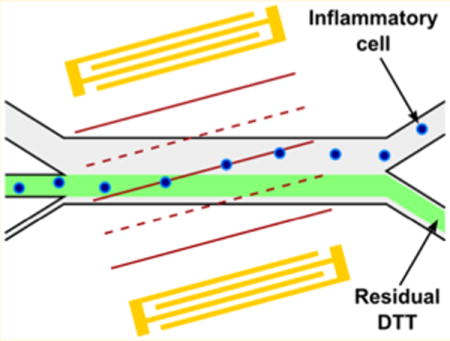
The working mechanism of our acoustofluidic device is shown in Figure 1. Our device (Figure 1, inset) is fabricated by bonding a polydimethylsiloxane (PDMS) microchannel with a pair of IDTs on a piezoelectric substrate. The microchannel is aligned with the IDTs at a tilt angle of 15°.40 When the IDTs are excited by radio frequency (RF) signals, two identical surface acoustic waves (SAWs) are generated and propagate in opposite directions. The interference between the waves establishes a SSAW field inside the microchannel. Because of the tilted alignment, periodically distributed pressure nodes and antinodes are formed at an angle relative to the flow direction. When the liquefied sputum sample flows into the SSAW field, inflammatory cells present in the sample are subjected to an acoustic radiation force (Fr) and the Stokes drag force (Fd), which are expressed as42
| (1) |
| (2) |
| (3) |
where p0, Vc, λ, k, x, ρc, ρf, βc, βf, η, Rc, and ur are acoustic pressure, volume of the cell, SAW wavelength, wave vector, distance from a pressure node, density of the cell, density of the fluid, compressibility of the cell, compressibility of the fluid, viscosity of the fluid, radius of the cell, and relative velocity of the cell, respectively. Equation 2 calculates the acoustic contrast factor (ϕ) of the cell.
Figure 1.
Schematic of our acoustofluidic device for transferring inflammatory cells from liquefied sputum samples to a buffer solution using SSAW. Inset: a photograph of our acoustofluidic device.
Inflammatory cells present in the liquefied sputum sample are expected to have a positive acoustic contrast factor based on our previous work.40,43–45 In our experiment, we observed that the inflammatory cells moved toward pressure nodes in the SSAW field, confirming their positive acoustic contrast factor. Because of the angle between the pressure nodes and the flow direction, inflammatory cells that pass through the SSAW field deviate from the flow due to the combination of the acoustic radiation force and the Stokes drag force. As a result, inflammatory cells are successfully transferred from the liquefied sputum to the buffer solution and are collected at the upper outlet.
MATERIALS AND METHODS
Device Fabrication
Figure 1 (inset) is a photograph of our acoustofluidic-based inflammatory cell transfer device. For the fabrication of IDTs, two layers of chrome and gold (Cr/Au, 50 Å/500 Å) were deposited upon a photoresist-patterned lithium niobate (LiNbO3) wafer (128° Y-cut, 500 μm thick, and double-side polished) using an e-beam evaporator (RC0021, Semicore, U.S.A.). The pair of IDTs with a period of 200 μm was formed by a lift-off procedure. The PDMS microchannel was fabricated by standard soft-lithography using SU-8 photoresist. The height and width of the microchannel were 75 μm and 1 mm, respectively. A Harris Uni-Core 0.75 mm punch was used to drill holes for inlets and outlets. The PDMS microchannel and the LiNbO3 substrate were bonded together after 3 min of plasma treatment (PDC001, Harrick Plasma, U.S.A.) and were incubated overnight at 65 °C before use.
Sample Preparation
Human sputum samples were collected at the National Institutes of Health (NIH) from an asthmatic patient who provided informed consent to participate in the Institutional Review Board (protocol 99-H-0076) of the National Heart, Lung, and Blood Institute. After collection, sputum samples were transported on ice to The Pennsylvania State University. Upon arrival, the sputum sample was mixed with 0.1% DTT (Sputolysin reagent, Cat# 560000, EMD Millipore, USA) at a 1:4 ratio, vortexed for 30 s, and incubated at room temperature for 15 min. After incubation, the sample was filtered through a sterile cell strainer of mesh size 100 μm (Cat# 22363549, Fisher Scientific, U.S.A.). The filtered sample was centrifuged at 800 rpm for 5 min. After centrifugation, the pelleted cells with residual DTT were resuspended for the cell transfer experiment in 1 mL of phosphate-buffered saline (PBS) supplemented with 1% bovine serum albumin (BSA), 0.5% Pluronic F-68 (PF-68), and 2.5 mM EDTA.
Experimental Setup
The acoustofluidic cell transfer experiment was conducted on the stage of an inverted microscope (Eclipse Ti–U, Nikon, Japan). The IDTs were excited using an RF signal function generator (E4422B, Agilent, U.S.A.) and a power amplifier (100A250A, Amplifier Research, U.S.A.). The liquefied sputum sample and a PBS buffer (1% BSA, 0.5% PF-68, 2.5 mM EDTA) were injected into the center inlet and two sheath flow inlets using 1 mL syringes (MFR# 102-ST1C, McKesson, U.S.A.) and polyethylene tubing (Cat# 598322, Harvard Apparatus, U.S.A.). To transfer inflammatory cells for flow cytometry analysis, PBS supplemented with 1% mouse serum was used as a sheath flow. Flow rates were controlled by syringe pumps (neMESYS, cetoni GmbH, Germany). A fast camera (SA4, Photron, Japan) was connected to the microscope for video acquisition.
Cell Count and DTT Quantification
Cell concentrations of sputum samples before and after acoustofluidic-based inflammatory cell transfer were counted by hemocytometer. Specifically, 10 μL of initial liquefied sputum sample was processed in our acoustofluidic device and 50 μL of sample was collected from the upper outlet after cell transfer (processing time ∼ 10 min). After three repeated sample collections, the total number of cells collected in each 50 μL sample and the number of cells in 10 μL of initial liquefied sputum sample were measured using a hemocytometer. Cell recovery rate was calculated as the percentage of cells successfully transferred and collected through the upper outlet. DTT concentrations of sputum samples before and after acoustofluidic-based inflammatory cell transfer were quantified using a commercial DTT assay kit (Cat# DTT200, ProFoldin, U.S.A.): (1) 100 μL of DTT solutions from 100 to 0 μM were prepared in the wells of a 96-well plate (Cat# 07–200–565, Corning, U.S.A.) through 2-fold serial dilution; (2) 100 μL of 100× diluted sputum samples were added into the wells; (3) 25 μL of Dye C55 was added into each well; (4) After incubation at room temperature for 10 min, the fluorescence intensity at 535 nm (excitation at 485 nm) of each well was measured using a plate reader (Infinite 200 PRO, Tecan, Switzerland); (5) A linear standard curve was generated, and the original concentrations of DTT within sputum samples were interpolated.
Cell Viability
Cell viability was assessed using live/dead staining. Samples were stained with Calcein-AM (Cat# C3100MP, Life Technologies, U.S.A.) to identify live cells, and propidium iodide (Cat# P4864, Sigma-Aldrich, U.S.A.) to identify dead cells. After staining, samples were examined by fluorescence microscopy to calculate the percentage of live cells.
Modified Wright–Giemsa Staining
Sputum samples were added to the two chambers of a Shandon Double Cytofunnel (Cat# 5991039, Thermo Scientific, U.S.A.) assembled on Shandon Double Cytoslides (Cat# 5991055, Thermo Scientific, U.S.A.) and were centrifuged at 600 rpm for 10 min in a cytocentrifuge (Cytospin 3, Thermo Scientific, U.S.A.). After centrifugation, the slide was air-dried and stained with a Kwik-Diff staining kit (Cat# 9990700, Thermo Scientific, U.S.A.): (1) 10 dips in reagent 1 (fixative, green); (2) 5 min in reagent 2 (eosin, red); (3) 2 dips in reagent 3 (methylene blue, blue); (4) rinsed with deionized water. After staining, the slide was examined under an inverted microscope (Eclipse Ti–U, Nikon, Japan). Staining results were captured using a digital single-lens reflex (DSLR) camera (D3S, Nikon, Japan) connected to the microscope. A differential cell count was performed (200–250 cells in total) to calculate the percentage of major inflammatory cells (eosinophils and neutrophils) in the sputum sample.
Flow Cytometry
To label the inflammatory cells, 5 μL of Alexa Fluor 488 antihuman CD45 antibody (Cat# 304019, BioLegend, U.S.A.) and 5 μL of PE antihuman CD15 (SSEA-1) antibody (Cat# 301905, BioLegend, U.S.A.) were added to 100 μL of sputum sample before and after cell transfer, and incubated at room temperature for 30 min. Another 100 μL of liquefied sputum sample was also incubated without antibodies and used as a nonstained control. After incubation, the three samples were washed with 900 μL of PBS, fixed with 4% paraformaldehyde (Cat# sc-281692, Santa Cruz Biotechnology, U.S.A.), resuspended in 500 μL of PBS, and examined using a commercial flow cytometer (FC500, Beckman Coulter, U.S.A.). The flow cytometry results were analyzed using commercial software (FlowJo, LLC, U.S.A.).
Statistical Analysis
Data were presented as group means ± standard deviations (SD). Welch two-sample t tests were conducted. A p-value of less than 0.05 was considered statistically significant.
RESULTS AND DISCUSSION
Transfer of Inflammatory Cells Using SSAW
We first validated the successful transfer of inflammatory cells from liquefied sputum samples using our acoustofluidic device. Each sample was injected into the center inlet at a flow rate of 1 μL/min, and PBS buffer was injected into the upper and lower inlets at flow rates of 5 and 4 μL/min, respectively. When the SSAW was not applied, all of the inflammatory cells along with the residual DTT solution exited through the lower outlet, as shown in Figure 2a and Video S1 (Supporting Information). In order to transfer inflammatory cells from residual DTT solution to PBS buffer, we applied RF signals (19.54 MHz, 34.0 Vpp) to the IDTs. Based on our preliminary results, 34.0 Vpp was the optimized input voltage for our acoustofluidic cell transfer devices with current design. As shown in Figure 2b and Video S2 (Supporting Information), most of the inflammatory cells were transferred to the PBS buffer and collected through the upper outlet when the SSAW was applied. We observed that a small fraction of cells was difficult to transfer, even when we increased the input voltage. We collected three samples from the upper outlet after cell transfer and calculated the cell recovery rate to be 83.9 ± 5.1%.
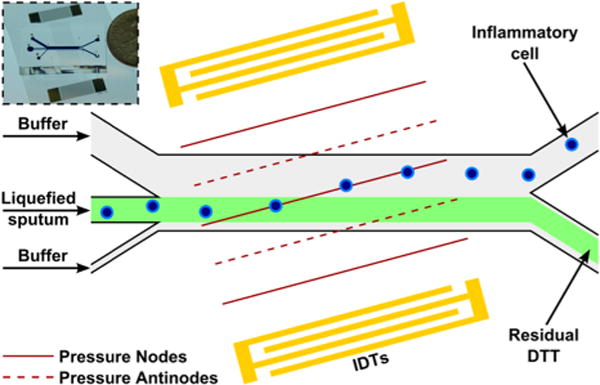
Figure 2.
(a, b) Stacked micrographs showing the transfer of inflammatory cells using SSAW. (a) When the SSAW was off, inflammatory cells exited through the lower outlet in residual DTT solution; (b) When the SSAW was on, most of the inflammatory cells were transferred to the PBS buffer and collected through the upper outlet. Scale bar = 200 μm. (c) DTT concentrations before and after the cell transfer (n = 3). ***p-value < 0.001.
To characterize the removal of residual DTT through acoustofluidic cell transfer, we quantified DTT concentrations of sputum samples before and after cell transfer. As shown in Figure 2c, the DTT concentration before acoustofluidic cell transfer was 573.1 ± 37.1 μM and decreased by 93% to 40.0 ± 14.9 μM after acoustofluidic cell transfer (p-value = 0.0004, two-sample t test). These results demonstrate that our acoustofluidic-based inflammatory cell transfer device removes residual DTT used for sputum liquefaction, which may affect cell viability and further cellular analysis.6–8 To further reduce the amount of DTT diffused into the upper outlet, we can increase the flow rate of the upper sheath flow and decrease the flow rate of the lower sheath flow to locate the sample flow away from the centerline of the channel. Such optimization of our platform will be further explored in the development of the integrated sputum processing and analysis instrument.
Cell Viability and Morphology
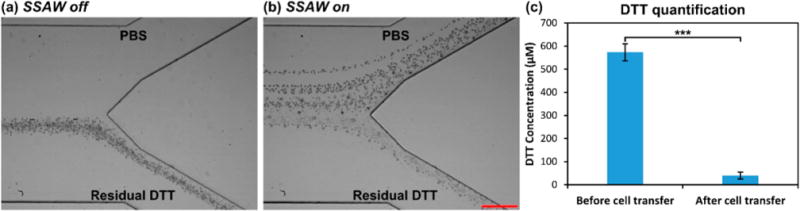
After demonstrating the successful transfer of inflammatory cells using our acoustofluidic device, we evaluated the effect of cell transfer on cell viability. We first checked the liquefied sputum sample and found the cell viability to be 41.5%. The relatively low cell viability could stem from prolonged storage of sputum samples after collection due to transportation delay (>4 h). Four samples of inflammatory cells were collected through the upper outlet after cell transfer. As a positive control, four samples of inflammatory cells were collected through the lower outlet when the SSAW was not applied. The cell viability of each sample was quantified and normalized to that of the original liquefied sputum sample. As shown in Figure 3, normalized cell viabilities of positive control samples and samples after acoustofluidic cell transfer were 92.1 ± 12.9% and 87.1 ± 8.9%, respectively (n = 4, p-value = 0.5498, two-sample t test). Therefore, exposure to SSAW during cell transfer did not affect the viability of inflammatory cells in sputum samples. It is worth noting that our acoustofluidic cell transfer removes cells from the presence of DTT. This might help preserve the viability of the cells if there is any damage of the cells induced by the DTT.6
Figure 3.
Comparison of normalized cell viabilities between the positive control samples and the sputum samples after acoustofluidic cell transfer (n = 4). N.S.: not significant (p-value > 0.05).
To examine if exposure to SSAW during cell transfer compromised cell integrity, transferred cells were stained with modified Wright–Giemsa stain to inspect cell morphology and identify different inflammatory cell types. Samples collected through the lower inlet without SSAW applied were used as a positive control. As shown in Figure 4, the appearance of stained cells after transfer appeared similar to that of the positive control group. We identified major inflammatory cells common to sputum samples from asthmatic patients (e.g., eosinophils and neutrophils), as well as other cell types (e.g., macrophages and oral squamous cells). From a differential cell count, the percentages of major inflammatory cells (eosinophils and neutrophils) for the positive control and after acoustofluidic cell transfer were 27.6% and 29.5%, respectively. The modified Wright–Giemsa staining results indicate that our acoustofluidic-based inflammatory cell transfer device preserves cell integrity and is compatible with histological staining, which is commonly used in clinical diagnostics of pulmonary diseases.
Figure 4.
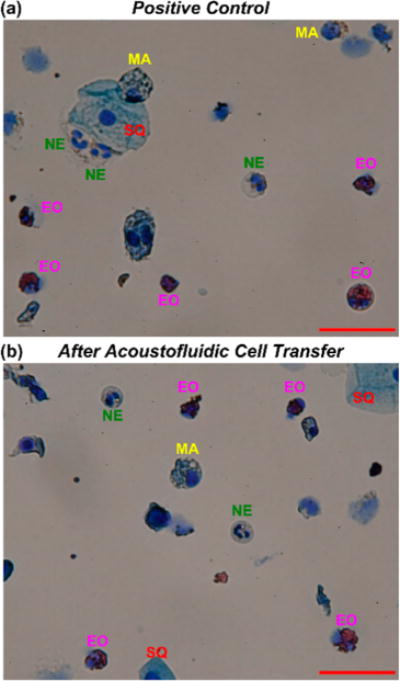
Modified Wright-Giemsa staining results of (a) the positive control group and (b) the sputum sample after acoustofluidic cell transfer. EO: eosinophil; NE: neutrophil; MA: macrophage; SQ: oral squamous cell. Scale bar = 50 μm.
Flow Cytometry Analysis
Since identification of major inflammatory cells using flow cytometry is a crucial step in immunophenotyping of sputum samples, we examined the effect of acoustofluidic-based cell transfer on flow cytometry analysis. Inflammatory cells in liquefied sputum samples were transferred using SSAW. Flow cytometry analysis was conducted on nonstained sputum sample, sputum sample before cell transfer, and sputum sample after cell transfer. The nonstained sputum sample was used to set the gates for CD45+ and CD15+ cells (Figure 5a,b). Fluorescence signals of CD45 and CD15 in the sputum sample before acoustofluidic cell transfer (Figure 5d,e) were weaker than after acoustofluidic cell transfer (Figure 5g,h). This is attributed to the inactivation of antibodies by residual DTT.46 The calculated percentages of CD45+/CD15+ cells in sputum samples before and after cell transfer were 11.9% and 29.9%, respectively, which correspond to copopulation of eosinophils and neutrophils in two samples. Compared to the results obtained from a differential cell count (27.6 and 29.5%), the percentage of CD45+/CD15+ cells in the sputum sample before cell transfer was underestimated. We quantified the percentage of copopulation of eosinophils and neutrophils more accurately after cell transfer (Figure 5i). Our flow cytometry results justify the necessity of the acoustofluidic cell transfer step after sputum liquefaction for identification of major inflammatory cells per flow cytometry.
Figure 5.
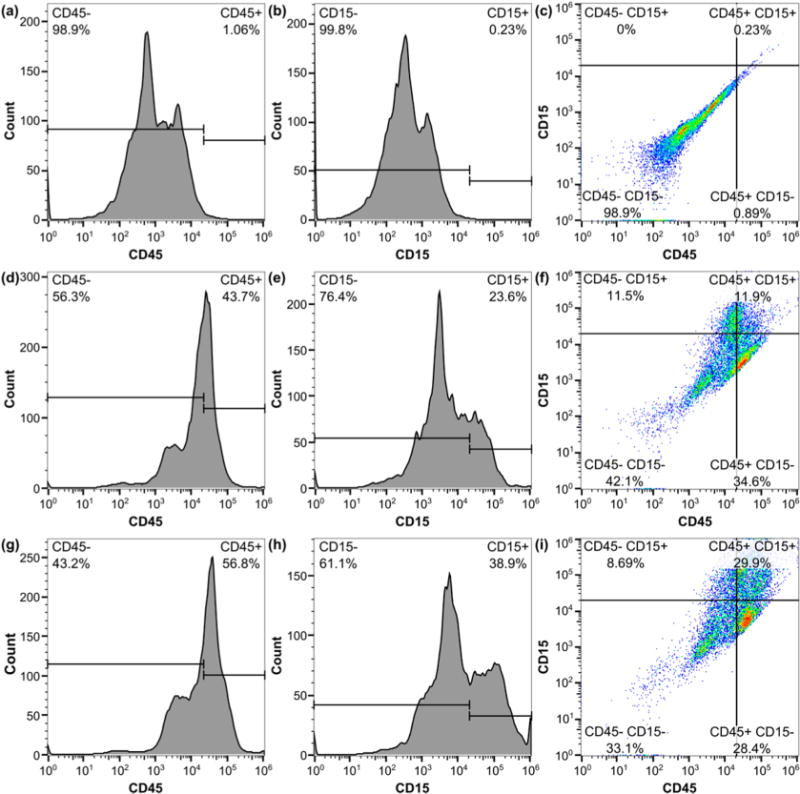
Flow cytometry results of (a–c) nonstained sputum sample; (d–f) sputum sample before acoustofluidic cell transfer; and (g–i) sputum sample after acoustofluidic cell transfer. The nonstained sputum sample was used to set the gates for CD45+ and CD15+ cells. The calculated percentages of CD45+/CD15+ cells (eosinophils and neutrophils) in sputum samples before and after cell transfer were 11.9 and 29.9%, respectively.
CONCLUSIONS
We have demonstrated an acoustofluidic device that transfers inflammatory cells from liquefied sputum samples by SSAW. Our device preserves the viability and integrity of transferred inflammatory cells. In addition, by removing residual DTT utilized during sputum liquefaction, our acoustofluidic-based inflammatory cell transfer device yields more accurate immunophenotyping results per flow cytometry analysis. The increased accuracy is valuable for identifying inflammatory lung cells from human sputum samples. Compared with conventional centrifugation methods, our acoustofluidic-based approach offers advantages such as high biocompatibility, high biosafety, low cost, and miniaturization. In this work, vortex mixing was used for sputum liquefaction and a manual wash step was implemented in sample preparation to preconcentrate the liquefied sputum sample. In our future work, we will incorporate our recently developed acoustofluidic sputum liquefier to get rid of the off-chip sample preparation steps.14 In addition, an on-chip flow cytometry unit47–49 will be incorporated to realize an automated, fully integrated device for point-of-care diagnostics and personalized treatment of asthma and other pulmonary diseases. We envision that the realization of such platforms could have significant impact on diagnosis and therapeutics of asthma and other pulmonary diseases.
Supplementary Material
Acknowledgments
We thank Dr. Zhiwei Xie from Prof. Jiang Yang’s group for microplate fluorescence measurements. This research was supported by the American Asthma Foundation (AAF) Scholar Award, National Institutes of Health (1R01AI120560-01), and the NHLBI Division of Intramural Research. S.L. and C.E.C. were funded in part by Grant AI45818 from NIAID, NIH. Components of this work were conducted at the Penn State node of the NSF-funded National Nanotechnology Infrastructure Network (NNIN).
Footnotes
Supporting Information
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acs.anal-chem.5b03383.
Video captions (PDF).
Supplementary video S1 shows that all of the inflammatory cells exited through the lower outlet when the SSAW was off (AVI).
Supplementary video S2 shows that most of the inflammatory cells were transferred and collected through the upper outlet when the SSAW was on (AVI).
Notes
The authors declare no competing financial interest.
References
- 1.Mase SR, Ramsay A, Ng V, Henry M, Hopewell PC, Cunningham J, Urbanczik R, Perkins MD, Aziz MA, Pai M. Int J Tuberc Lung Dis. 2007;11(5):485–495. [PubMed] [Google Scholar]
- 2.McNerney R, Maeurer M, Abubakar I, Marais B, McHugh TD, Ford N, Weyer K, Lawn S, Grobusch MP, Memish Z, Squire SB, Pantaleo G, Chakaya J, Casenghi M, Migliori GB, Mwaba P, Zijenah L, Hoelscher M, Cox H, Swaminathan S, Kim PS, Schito M, Harari A, Bates M, Schwank S, O’Grady J, Pletschette M, Ditui L, Atun R, Zumla A. J Infect Dis. 2012;205(Suppl 2):S147–S158. doi: 10.1093/infdis/jir860. [DOI] [PubMed] [Google Scholar]
- 3.Simpson JL, Scott R, Boyle MJ, Gibson PG. Respirology. 2006;11(1):54–61. doi: 10.1111/j.1440-1843.2006.00784.x. [DOI] [PubMed] [Google Scholar]
- 4.Wenzel SE. Lancet. 2006;368:804–813. doi: 10.1016/S0140-6736(06)69290-8. [DOI] [PubMed] [Google Scholar]
- 5.Vidal S, Bellido-Casado J, Granel C, Crespo A, Plaza V, Juárez C. Immunobiology. 2012;217(7):692–697. doi: 10.1016/j.imbio.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Tartier L, McCarey YL, Biaglow JE, Kochevar IE, Held KD. Cell Death Differ. 2000;7(10):1002–1010. doi: 10.1038/sj.cdd.4400726. [DOI] [PubMed] [Google Scholar]
- 7.Woolhouse IS, Bayley DL, Stockley RA. Thorax. 2002;57(8):667–671. doi: 10.1136/thorax.57.8.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beier J, Beeh KM, Kornmann O, Buhl R. J Lab Clin Med. 2004;144(1):38–44. doi: 10.1016/j.lab.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Kim HS, Devarenne TP, Han A. Lab Chip. 2015;15(11):2467–2475. doi: 10.1039/c4lc01316f. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Z, Xu J, Hong B, Chen X. Lab Chip. 2014;14(14):2576–2584. doi: 10.1039/c4lc00301b. [DOI] [PubMed] [Google Scholar]
- 11.Wang H, Kim J, Jayaraman A, Han A. Biomed Microdevices. 2014;16(6):887–896. doi: 10.1007/s10544-014-9893-x. [DOI] [PubMed] [Google Scholar]
- 12.Rane TD, Zec HC, Wang T-H. Anal Chem. 2015;87(3):1950–1956. doi: 10.1021/ac504330x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu X, Samuelson DR, Xu Y, Zhang H, Wang S, Rasco BA, Xu J, Konkel ME. Anal Chem. 2013;85(4):2320–2327. doi: 10.1021/ac303279u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang P-H, Ren L, Nama N, Li S, Li P, Yao X, Cuento RA, Wei C-H, Chen Y, Xie Y, Nawaz AA, Alevy YG, Holtzman MJ, McCoy JP, Levine SJ, Huang TJ. Lab Chip. 2015;15(15):3125–3131. doi: 10.1039/c5lc00539f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liong M, Fernandez-Suarez M, Issadore D, Min C, Tassa C, Reiner T, Fortune SM, Toner M, Lee H, Weissleder R. Bioconjugate Chem. 2011;22(12):2390–2394. doi: 10.1021/bc200490r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim J-H, Yeo W-H, Shu Z, Soelberg SD, Inoue S, Kalyanasundaram D, Ludwig J, Furlong CE, Riley JJ, Weigel KM, Cangelosi GA, Oh K, Lee K-H, Gao D, Chung J-H. Lab Chip. 2012;12(8):1437–1440. doi: 10.1039/c2lc21131a. [DOI] [PubMed] [Google Scholar]
- 17.Fang X, Chen H, Xu L, Jiang X, Wu W, Kong J. Lab Chip. 2012;12(8):1495–1499. doi: 10.1039/c2lc40055c. [DOI] [PubMed] [Google Scholar]
- 18.Hung LY, Huang TB, Tsai YC, Yeh CS, Lei HY, Lee GB. Biomed Microdevices. 2013;15(3):539–551. doi: 10.1007/s10544-013-9753-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park S, Zhang Y, Wang T-H, Yang S. Lab Chip. 2011;11(17):2893–2900. doi: 10.1039/c1lc20307j. [DOI] [PubMed] [Google Scholar]
- 20.Lee G-B, Wu H-C, Yang P-F, Mai JD. Lab Chip. 2014;14(15):2837–2843. doi: 10.1039/c4lc00466c. [DOI] [PubMed] [Google Scholar]
- 21.Sochol RD, Li S, Lee LP, Lin L. Lab Chip. 2012;12(20):4168–4177. doi: 10.1039/c2lc40610a. [DOI] [PubMed] [Google Scholar]
- 22.Chiang Y-Y, West J. Lab Chip. 2013;13(6):1031–1034. doi: 10.1039/c3lc41297k. [DOI] [PubMed] [Google Scholar]
- 23.Kantak C, Beyer S, Yobas L, Bansal T, Trau D. Lab Chip. 2011;11(6):1030–1035. doi: 10.1039/c0lc00381f. [DOI] [PubMed] [Google Scholar]
- 24.Tarn MD, Lopez-Martinez MJ, Pamme N. Anal Bioanal Chem. 2014;406(1):139–161. doi: 10.1007/s00216-013-7363-6. [DOI] [PubMed] [Google Scholar]
- 25.Peyman SA, Iles A, Pamme N. Chem Commun. 2008;(10):1220–1222. doi: 10.1039/b716532c. [DOI] [PubMed] [Google Scholar]
- 26.Tornay R, Braschler T, Demierre N, Steitz B, Finka A, Hofmann H, Hubbell JA, Renaud P. Lab Chip. 2008;8(2):267–273. doi: 10.1039/b713776a. [DOI] [PubMed] [Google Scholar]
- 27.Gossett DR, Tse HTK, Dudani JS, Goda K, Woods TA, Graves SW, Di Carlo D. Small. 2012;8(17):2757–2764. doi: 10.1002/smll.201200588. [DOI] [PubMed] [Google Scholar]
- 28.Yamada M, Kobayashi J, Yamato M, Seki M, Okano T. Lab Chip. 2008;8(5):772–778. doi: 10.1039/b718281c. [DOI] [PubMed] [Google Scholar]
- 29.Hawkes JJ, Barber RW, Emerson DR, Coakley WT. Lab Chip. 2004;4(5):446–452. doi: 10.1039/b408045a. [DOI] [PubMed] [Google Scholar]
- 30.Morton KJ, Loutherback K, Inglis DW, Tsui OK, Sturm JC, Chou SY, Austin RH. Lab Chip. 2008;8(9):1448–1453. doi: 10.1039/b805614e. [DOI] [PubMed] [Google Scholar]
- 31.Augustsson P, Åberg LB, Swärd-Nilsson A-MK, Laurell T. Microchim Acta. 2009;164(3–4):269–277. [Google Scholar]
- 32.VanDelinder V, Groisman A. Anal Chem. 2007;79(5):2023–2030. doi: 10.1021/ac061659b. [DOI] [PubMed] [Google Scholar]
- 33.Toyama K, Yamada M, Seki M. Biomed Microdevices. 2012;14(4):751–757. doi: 10.1007/s10544-012-9653-8. [DOI] [PubMed] [Google Scholar]
- 34.Petersson F, Nilsson A, Jönsson H, Laurell T. Anal Chem. 2005;77(5):1216–1221. doi: 10.1021/ac048394q. [DOI] [PubMed] [Google Scholar]
- 35.Sollier E, Amini H, Go DE, Sandoz PA, Owsley K, Di Carlo D. Microfluid Nanofluid. 2015;19(1):53–65. [Google Scholar]
- 36.Shi J, Huang H, Stratton Z, Huang Y, Huang TJ. Lab Chip. 2009;9(23):3354–3359. doi: 10.1039/b915113c. [DOI] [PubMed] [Google Scholar]
- 37.Ding X, Lin S-CS, Lapsley MI, Li S, Guo X, Chan CY, Chiang I-K, Wang L, McCoy JP, Huang TJ. Lab Chip. 2012;12(21):4228–4831. doi: 10.1039/c2lc40751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ding X, Peng Z, Lin S-CS, Geri M, Li S, Li P, Chen Y, Dao M, Suresh S, Huang TJ. Proc Natl Acad Sci U S A. 2014;111:12992–12997. doi: 10.1073/pnas.1413325111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li P, Mao Z, Peng Z, Zhou L, Chen Y, Huang P, Truica CI, Drabick JJ, El-Deiry WS, Dao M, Suresh S, Huang TJ. Proc Natl Acad Sci U S A. 2015;112(16):4970–4975. doi: 10.1073/pnas.1504484112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li S, Ding X, Mao Z, Chen Y, Nama N, Guo F, Li P, Wang L, Cameron CE, Huang TJ. Lab Chip. 2015;15(1):331–338. doi: 10.1039/c4lc00903g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Friend J, Yeo LY. Rev Mod Phys. 2011;83(2):647–704. [Google Scholar]
- 42.Yosioka K, Kawasima Y. Acustica. 1955;5:167–173. [Google Scholar]
- 43.Guo F, Li P, French JB, Mao Z, Zhao H, Li S, Nama N, Fick JR, Benkovic SJ, Huang TJ. Proc Natl Acad Sci U S A. 2015;112(1):43–48. doi: 10.1073/pnas.1422068112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ding X, Lin S-CS, Kiraly B, Yue H, Li S, Chiang I-K, Shi J, Benkovic SJ, Huang TJ. Proc Natl Acad Sci U S A. 2012;109(28):11105–11109. doi: 10.1073/pnas.1209288109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ding X, Li P, Lin S-CS, Stratton ZS, Nama N, Guo F, Slotcavage D, Mao X, Shi J, Costanzo F, Huang TJ. Lab Chip. 2013;13(18):3626–3649. doi: 10.1039/c3lc50361e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Okuno T, Kondelis N. J Clin Pathol. 1978;31(12):1152–1155. doi: 10.1136/jcp.31.12.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen Y, Nawaz AA, Zhao Y, Huang P-H, McCoy JP, Levine SJ, Wang L, Huang TJ. Lab Chip. 2014;14(5):916–923. doi: 10.1039/c3lc51139a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mao X, Nawaz AA, Lin S-CS, Lapsley MI, Zhao Y, McCoy JP, El-Deiry WS, Huang TJ. Biomicrofluidics. 2012;6(2):024113. doi: 10.1063/1.3701566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nawaz AA, Chen Y, Nama N, Nissly RH, Ren L, Ozcelik A, Wang L, McCoy JP, Levine SJ, Huang TJ. Anal Chem. 2015;87(24):12051–12058. doi: 10.1021/acs.analchem.5b02398. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


