Abstract
Background
A recent randomised controlled trial (RCT) of acupuncture as a treatment for irritable bowel syndrome (IBS) demonstrated sustained benefits over a period of 12 months post-randomisation.
Aim
To extend the trial follow-up to evaluate the effects of acupuncture at 24 months post-randomisation.
Methods
Patients in primary care with ongoing IBS were recruited to a two-arm pragmatic RCT of acupuncture for IBS. Participants were randomised to the offer of up to 10 weekly sessions of acupuncture plus usual care (n=116 patients) or to continue with usual care alone (n=117). The primary outcome was the self-reported IBS symptom severity score (IBS SSS) measured at 24 months post-randomisation. Analysis was by intention-to-treat using an unstructured multivariate linear model incorporating all repeated measures.
Results
The overall response rate was 61%. The adjusted difference in mean IBS SSS at 24 months was −18.28 (95% CI −40.95 to 4.40) in favour of the acupuncture arm. Differences at earlier time points estimated from the multivariate model were: −27.27 (−47.69 to −6.86) at 3 months; −23.69 (−45.17 to −2.21) at 6 months; −24.09 (−45.59 to −2.59) at 9 months; and −23.06 (−44.52 to −1.59) at 12 months.
Conclusions
There were no statistically significant differences between the acupuncture and usual care groups in IBS SSS at 24 months post-randomisation, and the point estimate for the mean difference was approximately 80% of the size of the statistically significant results seen at 6, 9 and 12 months.
Trial registration number
ISRCTN08827905.
Keywords: ACUPUNCTURE, PRIMARY CARE, GASTROENTEROLOGY)
Introduction
In response to the limited evidence on acupuncture as a treatment for patients with irritable bowel syndrome (IBS), as detailed in a Cochrane review,1 we previously conducted a pragmatic randomised controlled trial (RCT) to evaluate the clinical effectiveness and cost-effectiveness of acupuncture for this condition.2 3 We found that, for patients recruited from primary care who were diagnosed with IBS with an average duration of 13 years, acupuncture was associated with a clinical reduction in symptoms at 3 months post-randomisation when compared to usual care alone, and that the effect largely persisted up to 12 months post-randomisation.2
We know from a previous trial of acupuncture for low back pain that statistically significant benefits might be observed at 24 months post-randomisation.4 Such long-term benefits are hypothesised to be associated with the acupuncture-specific interactions designed to engage patients in their recovery process by making, for example, lifestyle changes indicated by their traditional acupuncture diagnosis.5 Similarly, in the aforementioned trial of acupuncture for IBS, the acupuncturists provided lifestyle advice to 68% of their patients.6
In the light of uncertainty regarding whether clinical benefits in IBS lasted beyond 12 months, our aim was to extend the project and conduct a longer-term follow-up at 24 months post-randomisation.
Methods
Design
The methods for the full-scale trial are reported elsewhere.2 In summary, 233 adults with IBS symptoms scoring at least 100 on the IBS symptom severity scale (IBS SSS) were recruited from primary care to a parallel-arm RCT examining the clinical effectiveness and cost-effectiveness of acupuncture as an adjunct to usual care for IBS. The patients were recruited from November 2008 to June 2009. The trial was prospectively registered (ISRCTN08827905) and received approval from the York NHS Research Ethics Committee (08/H1311/66) in 2008.
Randomisation and interventions
Patients were randomly allocated to receive up to 10 weekly individualised sessions of acupuncture plus usual care (n=116) or to continue with usual care alone (n=117). The random allocation sequence was computer-generated by an independent data manager in the York Trials Unit. Those allocated to the acupuncture group were offered up to 10 sessions. Patients who attended at least one session completed on average nine sessions, almost all of which were delivered weekly in the first 3 months post-randomisation. Details of the traditional acupuncture diagnosis and treatment, including the acupuncture diagnosis-related lifestyle advice, have been published separately.6
Outcome measures
Initially we sent follow-up questionnaires by post to patients at 3, 6, 9, and 12 months post-randomisation. The main outcome measure was the IBS SSS, which is scored from 0 to 500 (<75=no IBS, 75–175=‘mild’ IBS, 175–300=‘moderate’ IBS, >300=‘severe’ IBS).7 Secondary outcomes included the IBS non-colonic symptom score (NCSS), which includes lethargy and tiredness, backache, and other symptoms,8 and the 12-item Short Form Health Survey (SF-12) physical component summary (PCS) and mental component summary (MCS) scores.9 In this extended follow-up study, the above outcomes were measured at a single additional time point (24 months post-randomisation).
Ethics approval and follow-up method
Approval for this project extension was obtained from the York NHS Research Ethics Committee (08/H1311/66). A letter was sent to all patients who had not withdrawn from the trial informing them of the new follow-up in June 2011. If letters were returned undelivered because the addressee had moved, we tried to make contact with the patient by phone to obtain his or her new postal address. A few weeks after the initial letter had been mailed out, the new follow-up questionnaire was posted to all patients who had not withdrawn from the trial and for whom we had addresses. Questionnaires were sent out on the same date to all participants. At the point we were able to commence follow-up, it had been 30 and 24 months since the first and last patients, respectively, had been recruited to the trial. If patients did not return the questionnaire, we did not send a reminder letter or seek to collect the outcomes over the phone. Return of the additional follow-up questionnaire from patients was taken to indicate implicit consent to take part.
Statistical analysis
We used Stata (V.12) to perform intention-to-treat statistical analysis of the IBS SSS measures using a two-sided 5% significance level. In our earlier paper2 we used standard analysis of covariance (ANCOVA) models to compare means in the two groups, adjusting for baseline levels separately at each follow-up time point. Here, in view of the fact that there was substantially more missing data at 24 months, we used a multivariate linear model to analyse simultaneously the data from all time points. The advantage of this approach is that it can take account of some of the biases that can be introduced by missing data. A properly specified multivariate model is unbiased under a ‘missing at random’ assumption whereas ANCOVA requires the stronger ‘missing completely at random’ assumption.10
This multivariate model has been described in detail by Molenberghs and Kenward11 and Carpenter and Kenward.12 In brief, the model treats the baseline and follow-up measures as correlated outcomes, enforcing a zero treatment effect at baseline, with an unstructured covariance matrix for the repeated measures. The model permits simultaneous estimation of treatment differences at all follow-up time-points, adjusted for baseline. It is evident from the findings of Lee13 that, in the absence of missing data, this approach gives identical point estimates and very similar standard errors to an ANCOVA model. It also allows measurements at the various time points (including baseline) to be correlated one with another, with no constraints on variance and covariance. White and Thompson have shown analytically and in simulations that this approach is the most statistically efficient method of dealing with partially missing baseline measurements in RCTs.14 Analogous analyses were performed for the secondary outcomes of IBS NCSS and SF-12 PCS and MCS scores.
Results
Recruitment and follow-up
The baseline characteristics of the 233 patients recruited to the trial are published elsewhere.2 In brief, the average age was 43 years, 19% were male, and they had experienced IBS for an average of 13 years. Follow-up rates are presented in table 1, which shows that complete non-missing IBS SSS data at 24 months were available for analysis in 61% of participants, comprising 68% (n=79) of the acupuncture group and 53% (n=62) of the usual care group.
Table 1.
Response rates at follow-up for acupuncture (n=116) and usual care (n=117)
| Month | Questionnaires returned (%) |
Non-missing IBS SSS data (%) |
||
|---|---|---|---|---|
| Acupuncture | Usual care | Acupuncture | Usual care | |
| 3 | 109 (94%) | 100 (85%) | 108 (93%) | 97 (83%) |
| 6 | 105 (91%) | 95 (81%) | 99 (85%) | 91 (78%) |
| 9 | 104 (90%) | 95 (81%) | 93 (80%) | 94 (80%) |
| 12 | 104 (90%) | 94 (80%) | 103 (89%) | 93 (79%) |
| 24 | 81 (70%) | 62 (53%) | 79 (68%) | 62 (53%) |
IBS SSS, irritable bowel syndrome symptom severity score.
Table 2 shows the mean baseline IBS SSS for those with and without available data at 24 months.
Table 2.
Baseline IBS SSS according to whether or not an IBS SSS score was obtained at 24 months
| 24 month score obtained—mean (SE) | 24 month score missing—mean (SE) | |
|---|---|---|
| Acupuncture group | 269.13 (8.79) n=78 | 302.92 (14.02) n=37 |
| Usual care group | 273.67 (8.73) n=61 | 281.27 (10.49) n=52 |
Of those providing follow-up data at 24 months, baseline IBS SSS data were available for 78 of 79 patients in the acupuncture group and 61 of 62 patients in the usual care group.
IBS SSS, irritable bowel syndrome symptom severity score.
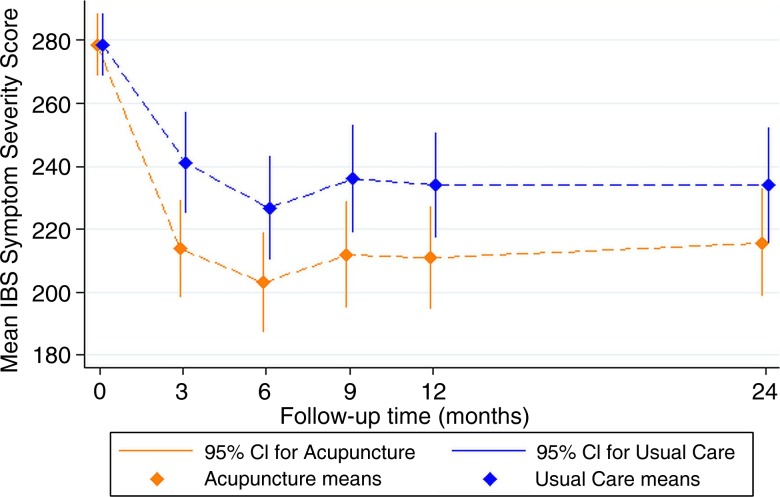
Results from the unstructured multivariate linear model analysis of IBS SSS, treating follow-up and baseline IBS SSS measures as correlated outcomes with only that of follow-up depending on treatment, are shown in table 3 and figure 1. Up to 12 months, this analysis gave results that were largely similar to the separate linear regression models used previously.2 The adjusted difference between the means at 24 months (−18.28, 95% CI −40.95 to 4.40) was not statistically significant, and the point estimate was around 20% smaller in magnitude than the mean differences of 23 to 24 points that were seen at 6, 9, and 12 months. A minor difference compared to our previous analysis was the finding of a statistically significant difference between acupuncture and usual care groups at 12 months (−23.06, 95% CI −44.52 to −1.59; p=0.035), which was previously only borderline significant (−21.33, 95% CI −43.66 to 1.00; p=0.061). The re-analysis of all available data under a missing at random assumption resulted in a slightly larger treatment effect that was more precisely estimated, as demonstrated by the tighter confidence interval.
Table 3.
Primary outcome measure (IBS SSS scores) between baseline and 24-month follow-up, and between-group differences (n=233)
| IBS SSS | Baseline mean (95% CI) | Month 3 mean (95% CI) | Month 6 mean (95% CI) | Month 9 mean (95% CI) | Month 12 mean (95% CI) | Month 24 mean (95% CI) |
|---|---|---|---|---|---|---|
| Acupuncture group (n=116) | 278.45 (268.54 to 288.35) | 213.71 (198.17 to 229.24) | 202.99 (186.97 to 219.01) | 211.86 (194.97 to 228.76) | 210.89 (194.70 to 227.08) | 215.62 (198.60 to 232.64) |
| Usual care group (n=117) | 240.98 (224.89 to 257.07) | 226.68 (210.20 to 243.16) | 235.96 (218.91 to 253.01) | 233.95 (217.24 to 250.65) | 233.90 (215.48 to 252.31) | |
| Between-group differences in means (acupuncture vs. usual care) | − | −27.27 (−47.69 to −6.86)* | −23.69 (−45.17 to −2.21)* | −24.09 (−45.59 to −2.59)* | −23.06 (−44.52 to −1.59)* | −18.28 (−40.95 to 4.40) |
Data are predicted means and 95% CIs from the unstructured multivariate linear model. At baseline there is only one predicted mean since the corresponding outcome does not depend on treatment.
*p<0.05.
IBS SSS, irritable bowel syndrome symptom severity score.
Figure 1.
Unstructured multivariate linear model predicted means and 95% CIs. IBS, irritable bowel syndrome.
Between-group differences for the IBS NCSS, SF-12 PCS and SF-12 MCS scores, derived using the unstructured multivariate linear model, are presented in table 4. Baseline and follow-up scores were treated as correlated outcomes, with only that of follow-up depending on treatment. There were no significant differences in outcome between the two groups with the single exception of the NCSS at 3 months.
Table 4.
Secondary outcome measures between baseline and 24-month follow-up, and between-group differences (n=233)
| Month 0 mean (95% CI) | Month 3 mean (95% CI) | Month 6 mean (95% CI) | Month 9 mean (95% CI) | Month 12 mean (95% CI) | Month 24 mean (95% CI) | |
|---|---|---|---|---|---|---|
| IBS NCSS | ||||||
| Acupuncture group (n=116) | 208.71 (198.94 to 218.47) | 178.78 (166.22 to 191.34) | 181.43 (168.41 to 194.46) | 187.12 (172.64 to 201.60) | 186.93 (173.07 to 200.79) | 178.11 (164.08 to 192.14) |
| Usual care group (n=117) | 193.42 (180.57 to 206.28) | 188.79 (175.45 to 202.13) | 189.81 (175.13 to 204.49) | 194.73 (180.44 to 209.03) | 188.16 (173.00 to 203.32) | |
| Between-group differences in means (acupuncture vs. usual care) | − | −14.64 (−28.91 to −0.38)* | −7.36 (−23.08 to 8.36) | −2.69 (−20.14 to 14.76) | −7.80 (−24.51 to 8.90) | −10.05 (−27.67 to 7.56) |
| SF-12 PCS score | ||||||
| Acupuncture group (n=116) | 43.38 (42.56 to 44.21) | 42.82 (41.78 to 43.86) | 43.11 (42.06 to 44.16) | 42.34 (41.29 to 43.39) | 42.09 (41.10 to 43.07) | 42.30 (41.21 to 43.39) |
| Usual care group (n=117) | 42.72 (41.59 to 43.84) | 42.14 (41.03 to 43.26) | 43.12 (42.01 to 44.22) | 42.15 (41.11 to 43.20) | 41.62 (40.43 to 42.81) | |
| Between-group differences in means (acupuncture vs. usual care) | − | 0.10 (−1.26 to 1.47) | 0.97 (−0.35 to 2.29) | −0.78 (−2.14 to 0.58) | −0.07 (−1.37 to 1.24) | 0.68 (−0.73 to 2.09) |
| SF-12 MCS score | ||||||
| Acupuncture group (n=116) | 44.08 (42.64 to 45.52) | 46.32 (44.39 to 48.25) | 46.02 (44.06 to 47.99) | 46.70 (44.72 to 48.69) | 46.39 (44.43 to 48.35) | 47.35 (45.39 to 49.30) |
| Usual care group (n=117) | 44.95 (42.84 to 47.05) | 44.91 (42.81 to 47.00) | 45.15 (43.07 to 47.22) | 45.98 (43.91 to 48.04) | 46.86 (44.71 to 49.00) | |
| Between-group differences in means (acupuncture vs. usual care) | − | 1.37 (−1.24 to 3.99) | 1.12 (−1.52 to 3.75) | 1.56 (−1.02 to 4.14) | 0.41 (−2.14 to 2.96) | 0.49 (−2.18 to 3.15) |
Data are predicted means and 95% CIs from the fitted model. At month 0 there is only one predicted mean for each measure since the corresponding outcome does not depend on treatment.
*p<0.05.
IBS NCSS, irritable bowel syndrome non-colonic symptom score; MCS, mental component summary; PCS, physical component summary; SF-12, 12-item Short Form Health Survey.
Discussion
Principal findings
In extending the collection of outcome data to 24 months, there were considerable missing data, with only 61% of participants providing complete IBS SSS data. Using an unstructured multivariate linear model to analyse data simultaneously from all time points, an approach which is more robust with regard to missing data than the separate complete case analysis method used previously, we did not observe a statistically significant difference in IBS symptom scores between the two groups at 24 months. Moreover, the point estimate of the size of the (non-significant) between-group difference was reduced by approximately 20% compared with that seen at 12 months, which was borderline statistically significant (p=0.061) in our original report2 and formally significant (p=0.035) after switching to an unstructured multivariate linear model herein—although it should be noted that the absolute change in p value and 95% confidence limits were small. The lack of a statistically significant treatment effect at 24 months could be due in part to the small size of the remaining sample and the concurrent, progressive reduction in IBS symptoms in the usual care group between 12 and 24 months. It is also noteworthy that the 68% of participants in the acupuncture group that provided data at 24 months had lower IBS SSS scores at baseline than the 32% who did not, and may not therefore be fully representative of the treatment group as a whole. Despite the fact that our approach to the statistical analysis controls for some of the biases that can result through missing data, it is still possible that this baseline difference between those with and without follow-up data at 24 months could have biased our results. As per our previously published analysis,2 we found little in the way of meaningful differences for any secondary outcomes measures—that is, non-colonic IBS symptoms and SF-12 physical and mental component scores.
Strengths and limitations
The major strength of this study is its long-term follow-up through to 24 months post-randomisation, a length of time that is unusual in studies of treatments for IBS. Moreover, our use of unstructured multivariate linear models (with baseline IBS SSS as a correlated outcome measure as opposed to a covariate) controls better for the potential biases that can arise due to missing data. This approach also led to a slightly more precise estimation of the treatment effects, as reflected in the somewhat tighter confidence intervals. We found that more patients in the usual care group failed to provide data at 24 months compared to the acupuncture group (47% vs 32%) and that the 68% of patients in the acupuncture group who did provide data at 24 months had a higher baseline IBS SSS than the 32% who did not. As such, those participants with extended follow-up may not be fully representative of the original groups as a whole, which could potentially introduce bias. These differences provide a rationale for the unstructured multivariate linear model as it relaxes the assumptions necessary for the treatment estimates to be unbiased.
The low response rate at 24 months is a major limitation, especially given that response rates at 3, 6, 9, and 12 months were relatively high, with questionnaires returned by ≥90% and ≥80% of the acupuncture and usual care groups, respectively.2 At 24 months, we only received follow-up questionnaires with complete data from 61% of participants across the two trial arms. This could be due in part to the fact that the long-term follow-up at 24 months was not part of the original trial design. Patients participating in the trial originally expected a 12-month commitment and may thus have been less willing to return a subsequent and additional questionnaire, given that they were not informed of this possibility at the time of initial consent. In some cases, we no longer had the current address for patients, as some had moved away since the point of last contact by the trial team for completion of the 12-month questionnaire.
As mentioned above, the loss to follow-up was not evenly split between groups, with only 53% of the usual care group submitting IBS SSS data at 24 months, compared to 68% in the acupuncture arm. The reason for this difference is unknown; however, the greater participation with regards to follow-up in the acupuncture group may reflect the enhanced engagement with the trial engendered by practitioner–patient interactions that only occurred in the acupuncture arm during the first 3 months of the trial. The difference in response rates illustrates the need for the multivariate model. The difference suggests that the ‘missing completely at random’ assumption necessary for simpler analyses to be unbiased is implausible here. Another limitation is that, after the end of the initial 12-month trial period, additional acupuncture treatments may have been received by some patients in either arm, and this could have influenced the results either way.
The results of the trial can only be generalised with caution. The patients recruited to the trial constituted people who had consulted their general practitioner in primary care, had been diagnosed as having IBS of an average duration of 13 years, and were continuing to experience IBS symptoms. The results we have presented are based on averages across this population. A consequence of the small sample size is that we were unable to conduct subgroup analyses—for example, comparing patients with more severe or less severe IBS.
Implications for research and practice
As previously acknowledged, the trial was not designed to establish the proportion of the overall benefit that might be associated with ‘non-specific effects’—for example, the generic benefits associated with consulting an empathetic acupuncture practitioner in a supportive environment. Our extension of the follow-up to 24 months provides further evidence that the benefits observed between 3 and 12 months post-randomisation are unlikely to be due to ‘non-specific effects’. External evidence to support this comes from a review of 27 RCTs of treatments for IBS, in which no individual trial demonstrated a placebo response at 12 months.15 That the IBS symptom scores are largely sustained between the end of treatment at 3 months through to 24 months suggests that the apparent benefits of acupuncture represent more than a simple placebo response. Longer-term effects are likely to be associated with the underlying physiological mechanisms of action, into which further research is required. Also potentially important over the longer term are the non-needling components of treatment that are acupuncture-specific, such as the explanations of the traditional acupuncture diagnosis and the active engagement of the patient in following lifestyle advice related to the diagnosis.2 6
In terms of future trial design, it would be useful to control for the extra time and attention that the patients in the acupuncture arm received. For example, this could be provided by an active control arm with an intervention perceived to be credible by patients that provides structural equivalence in terms of measurable non-specific treatment components. Possible active controls in trials of acupuncture for IBS might include hypnotherapy, cognitive behavioural therapy, relaxation, and/or nutritional guidance. Among a range of possible non-specific components that one might want to control for, clearly contact time is important, as well as the quality of attention provided by the practitioner. As an exemplar, in a previous study of acupuncture for depression,16 counselling was provided as an active control, contact time and empathy were assessed using the consultation and relational empathy (CARE) measure,17 and these variables were included in the analysis comparing acupuncture with counselling.
Conclusion
There were no significant differences between the acupuncture and usual care groups at 24 months post-randomisation, and the point estimate for the mean difference was reduced by approximately 20% compared to the previous time point of 12 months. Using analytical methods that are more robust to the effects of missing data, we found statistically significant differences favouring acupuncture at 12 months, which only represented a statistical tendency in our previous analysis. The lack of a statistically significant difference at 24 months may be associated, at least in part, with the progressive improvement observed within the usual care group, combined with the increased loss to follow-up over time.
Acknowledgments
Acknowledgements are due to Janet Eldred and the team that conducted the trial, namely J Martin Bland, Karen Bloor, Sally Brabyn, Arthur Ricky Kang'ombe, Mei-See Man, Tracy Stuardi, David Torgerson, Ian Watt and Peter Whorwell.
Footnotes
Contributors: This paper was conceived by HM and HT. Data were collected by HT. Statistical analysis was conducted by DA, CF, CH and HB. The first draft of the manuscript was prepared by HM. All authors approved the final manuscript.
Funding: This article presents independent research commissioned by the UK National Institute for Health Research (NIHR) Research for Patient Benefit programme (PB-PG-0407-13241).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: York NHS Research Ethics Committee (08/H1311/66) .
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data available for sharing on application to the lead author.
References
- 1.Lim B, Manheimer E, Lao L, et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2006:18:CD005111 10.1002/14651858.CD005111.pub2 [DOI] [PubMed] [Google Scholar]
- 2.MacPherson H, Tilbrook H, Bland JM, et al. Acupuncture for irritable bowel syndrome: primary care based pragmatic randomised controlled trial. BMC Gastroenterol 2012;12:150 10.1186/1471-230X-12-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stamuli E, Bloor K, MacPherson H, et al. Cost-effectiveness of acupuncture for irritable bowel syndrome: findings from an economic evaluation conducted alongside a pragmatic randomised controlled trial in primary care. BMC Gastroenterol 2012;12:149 10.1186/1471-230X-12-149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas KJ, MacPherson H, Thorpe L, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ 2006;333:623–6. 10.1136/bmj.38878.907361.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacPherson H, Thomas K. Self-help advice as a process integral to traditional acupuncture care: implications for trial design. Complement Ther Med 2008;16:101–6. 10.1016/j.ctim.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 6.Stuardi T, MacPherson H. Acupuncture for irritable bowel syndrome: diagnosis and treatment of patients in a pragmatic trial. J Altern Complement Med 2012;18:1021–7. 10.1089/acm.2011.0670 [DOI] [PubMed] [Google Scholar]
- 7.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. [DOI] [PubMed] [Google Scholar]
- 8.Atkinson W, Sheldon TA, Shaath N, et al. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomised controlled trial. Gut 2004;53:1459–64. 10.1136/gut.2003.037697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 10.Rubin DB. Inference and missing data. Biometrika 1976;63:581–92. 10.1093/biomet/63.3.581 [DOI] [Google Scholar]
- 11.Molenberghs G, Kenward MG. Missing data in clinical studies. Wiley, 2007:526 ISBN: 978-0-470-84981-1. [Google Scholar]
- 12.Carpenter JR, Kenward MG. Missing data in randomised controlled trials—a practical guide. Birmingham: National Institute for Health Research, Publication RM03/JH17/MK 2008. http://www.missingdata.org.uk [Google Scholar]
- 13.Lee Y-H. A note on Rao's reduction of Potthof and Roy's generalized linear model. Biometrika 1974;61: 349–51. 10.1093/biomet/61.2.349 [DOI] [Google Scholar]
- 14.White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993–1007. 10.1002/sim.1981 [DOI] [PubMed] [Google Scholar]
- 15.Spiller RC. Problems and challenges in the design of irritable bowel syndrome clinical trials: experience from published trials. Am J Med 1999;107:91S–97S. 10.1016/S0002-9343(99)00086-8 [DOI] [PubMed] [Google Scholar]
- 16.MacPherson H, Richmond S, Bland M, et al. Acupuncture and counselling for depression in primary care: a randomised controlled trial. PLoS Med 2013;10:e1001518 10.1371/journal.pmed.1001518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mercer SW, McConnachie A, Maxwell M, et al. Relevance and performance of the consultation and relational empathy (CARE) measure in general practice. Fam Pract 2005;22:328–34. 10.1093/fampra/cmh730 [DOI] [PubMed] [Google Scholar]