Abstract
Objective
A systematic review of factors that might be associated with, or influence, clinical recovery from sport-related concussion. Clinical recovery was defined functionally as a return to normal activities, including school and sports, following injury.
Design
Systematic review.
Data sources
PubMed, PsycINFO, MEDLINE, CINAHL, Cochrane Library, EMBASE, SPORTDiscus, Scopus and Web of Science.
Eligibility criteria for selecting studies
Studies published by June of 2016 that addressed clinical recovery from concussion.
Results
A total of 7617 articles were identified using the search strategy, and 101 articles were included. There are major methodological differences across the studies. Many different clinical outcomes were measured, such as symptoms, cognition, balance, return to school and return to sports, although symptom outcomes were the most frequently measured. The most consistent predictor of slower recovery from concussion is the severity of a person’s acute and subacute symptoms. The development of subacute problems with headaches or depression is likely a risk factor for persistent symptoms lasting greater than a month. Those with a preinjury history of mental health problems appear to be at greater risk for having persistent symptoms. Those with attention deficit hyperactivity disorder (ADHD) or learning disabilities do not appear to be at substantially greater risk. There is some evidence that the teenage years, particularly high school, might be the most vulnerable time period for having persistent symptoms—with greater risk for girls than boys.
Conclusion
The literature on clinical recovery from sport-related concussion has grown dramatically, is mostly mixed, but some factors have emerged as being related to outcome.
Keywords: Concussion, sex differences, outcome, moderators, age, sports
Introduction
Concussions can have large adverse effects on cognitive functioning and balance in the first 24 hours following injury.1 2 Injured athletes report diverse physical, cognitive and emotional symptoms during the first week following injury,1 2 and a greater number and severity of symptoms after a concussion are predictors of a slower recovery.3–6 There is tremendous interest in identifying factors that might influence outcome from sport-related concussion.1 7–18
For most injured athletes, cognitive deficits,11 19 balance20 21 and symptoms21 improve rapidly during the first 2 weeks following injury. The return to play timeframe is often reported to be within 10 days.20 22–26 However, this tends to be based on group-level findings only, not clinical outcomes from individual athletes, and group statistical analyses can obscure subgroup results and individual differences. Some athletes might return to play while still symptomatic,27 28 well before clinical recovery. During the past 10 years, there has also been accumulating evidence suggesting that a sizeable minority of high school and collegiate athletes take much longer than 10 days to clinically recover and return to sports.29–31
The longer recovery times might partially reflect changes in the medical management of concussion,32 33 with adoption of the gradual return to play recommendations from the Concussion in Sport Group statements from the conferences in Prague34 and Zurich.35 36 These return to play recommendations include no same-day return to play and a sequential progression through a series of steps prior to medical clearance for return to sports. In contrast, from 1995 to 1997, 31% of concussed high school and collegiate athletes returned to play during the same game that they sustained a concussion.28 Those sustaining grade 1 concussions returned on average 4 days following injury and those sustaining grade 2 concussions returned, on average, 8 days following injury.28
However, the translation of the Prague and Zurich return-to-play recommendations into clinical practice has likely been gradual. There is clear evidence that from 2005 to 2008 many concussed high school athletes in the USA were returned to play prematurely, in a manner not consistent with the practice recommendations.37 Studies conducted in the past few years seem to reflect a change in clinical management. For example, in a study conducted between 2012 and 2014, of the 1429 concussions reported among youth, high school and college-level athletes, 3.1% returned to play within 24 hours of injury.38
At present, it is reasonable to conclude that the large majority of injured athletes recover, from a clinical perspective, within the first month following injury.39–43 Neurobiological recovery might extend beyond clinical recovery in some athletes.44–47 Clinicians know that some student athletes report persistent symptoms for many months following injury, there can be multiple causes for those symptoms and those individuals are more likely to be included in studies conducted at specialty clinics.48 49
A range of preinjury individual differences, initial injury severity indicators, acute clinical effects or subacute clinical effects or comorbidities might influence outcome from concussion. Genetics,50 sex differences,1 16 18 51–53 younger age,1 7 12 38 54 neurodevelopmental factors such as attention deficit hyperactivity disorder (ADHD)55 56 or learning disability,57 personal57 or family history of migraine,58 or a personal14 58 or family history of mental health problems58 might also be predictors or effect modifiers of clinical recovery from concussion. Having a past concussion is a risk factor for having a future concussion,59 and having multiple past concussions is associated with having more physical, cognitive and emotional symptoms prior to participation in a sporting season.60 61 There have been inconsistent findings regarding whether specific injury severity characteristics, such as loss of consciousness, retrograde amnesia or post-traumatic amnesia, are associated with greater acute effects or prolonged recovery.5 15 56 62 Numerous postinjury clinical factors, such as the initial severity of cognitive deficits,4 63 64 the development of post-traumatic headaches or migraines,5 65 experiencing dizziness,48 66 difficulties with oculomotor functioning48 and experiencing symptoms of depression,67 have also been associated with worse outcomes after concussion.
There is a need to synthesise evidence regarding the relationship between demographic and clinical preinjury, injury-related and postinjury factors and clinical recovery after concussion. Therefore, this systematic review will assess numerous factors that might be considered intermediary, effect modifying, predictor or confounding variables in relation to clinical recovery from concussion. Clinical recovery is defined functionally as a return to normal activities, including school and sports, following injury. Operationally, it encompasses a resolution of postconcussive symptoms and a return to clinically normal balance and cognitive functioning.
Methods
The review protocol was prospectively registered in the PROSPERO database for systematic reviews (protocol ID: CRD42016041479). The broad initial review questions provided by the scientific leadership committee of the Concussion in Sport Group were: (1) What are the key modifiers of concussion outcomes? (2) What factors are associated with a poorer prognosis or future risk following concussion? (3) How do we best quantify the role of these modifiers? (4) How many concussions are too many? (5) How do sex differences impact concussion management? Given the breadth of the initial questions, we narrowed the focus of this review to predictors of clinical outcome.
We defined outcome as ‘clinical recovery and return to activities and sports’. We examined different types of predictor variables. Effect modification occurs when the magnitude of the effect of concussion on clinical recovery (ie, the association) differs depending on the level of a third variable (ie, the effect modifier variable). Intermediary variables are factors involved in the causal pathway between exposure (injury) and outcome (clinical recovery). Confounding variables are factors independently associated with the outcome (clinical recovery), and independently associated with the exposure (concussion), but they are not involved in the causal pathway between exposure and outcome. Confounding variables have a bidirectional association with both the exposure (concussion) and the outcome (clinical recovery).
Search strategy
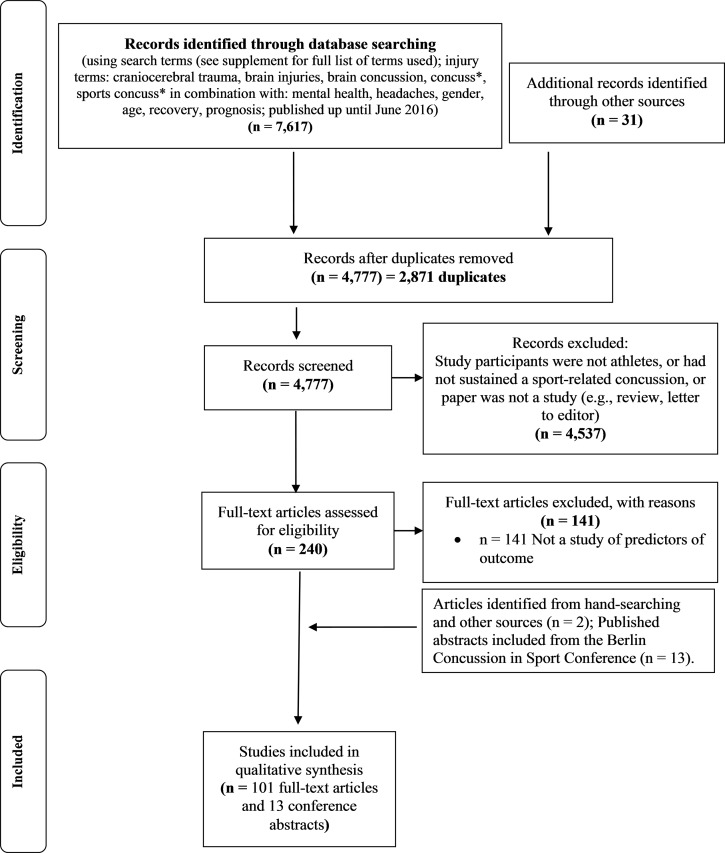
Articles were retrieved via online database searching, hand-searching reference lists and performing cited reference searches (see figure 1). We searched PubMed, PsycINFO, MEDLINE, CINAHL, Cochrane Library, EMBASE, SPORTDiscus, Scopus and Web of Science for articles published in English, from database inception to June 2016. Two general categories relating to (1) sport and athlete-related terms and (2) brain concussion-related terms were used as key search terms (refer to PROSPERO online registration (protocol ID: CRD42016041479), or see the online supplementary table, at the end of the table, for the specific search terms used). The search strategy initially included terms relating to imaging and biomarkers. However, after the search, these neuroimaging studies (as well as the results of serum biomarker studies) were determined to be beyond the scope of this review. The reference lists of articles retrieved for inclusion in the review were hand searched to identify other relevant articles. Key articles retrieved via online databases and through hand-searching reference lists were also used for further searches using the Web of Science Cited Reference function.
Figure 1.
Systematic literature search.
bjsports-2017-097729supp001.docx (57KB, docx)
Article selection
Two reviewers conducted the initial screening of the titles and abstracts of articles identified in the search. We included articles that examined factors that may be associated with outcome from concussion and were conducted with humans. We excluded articles that addressed acute outcome in the initial days following injury, but did not address clinical recovery time or risk for persistent symptoms. Where there was uncertainty about whether a study should be included based on the review of the title and abstract, the full article was retrieved. To supplement the electronic database search, we examined the reference lists from previously published reviews and systematic reviews and the published abstracts that were presented as posters and oral presentations at the Fifth Conference on Concussion in Sport in Berlin in October of 2016.
Data extraction
For the included articles, all authors participated in the extraction of the first author, year of publication, the PubMed identification number, number of participants, proportion of female participants, age, setting, clinical outcome, predictors that were significant, predictors that were not significant and the period for assessing the clinical outcome. The level of evidence was rated using the Oxford Classification for Evidence-Based Medicine. Two or three reviewers independently extracted data from and rated each article. A third reviewer was sometimes needed to resolve discrepancies. Studies were sorted based on the specific predictor variables that were analysed.
Results
We found 7617 articles in the database search (figure 1). After duplicates were removed, 4777 were screened further by title and abstract for eligibility. Of the 4777 articles, 4537 were excluded on the basis that they did not examine athletes who had sustained a sports concussion, or the citation was not an original study (ie, the citation was a review article, editorial, letter to the editor or commentary). The PDFs of 240 articles were retrieved and reviewed. We included 101 articles and 13 abstracts from the Berlin Concussion in Sport Conference for review (figure 1). In the online supplementary table and in boxes 1–3, we report variables that had a significant independent association with outcome. There were major methodological differences across the studies (see online supplementary table). Some of these differences are listed below.
Research designs were diverse, including retrospective, prospective, case–control, inception cohort and epidemiological studies.
Many different clinical outcomes were measured, including symptoms, cognition, balance, return to school and return to sports.
There was considerable variability in when outcomes were measured.
The setting in which the study was conducted also likely influenced outcomes; recovery times were faster in studies conducted in educational institutions21 53 compared with emergency departments57 68 or specialty clinics.69
Box 1. Preinjury characteristics associated with recovery.
Younger age:
Yes: Chermann81; Field82; Terwilliger83; Covassin84; Majerske85; Pellman86; Zuckerman71
No: Lau87; Hang30; McDevitt88; Nelson21; Asplund89; Chrisman75; Vargas74; Morgan58; Meehan42; Meehan90; Meehan6; McCrea91; Lee70; Baker92; Greenhill93; Nelson78; Corwin48; Preiss-Farzanegan94; Heyer80; Kontos67; Kriz77; Miller56, Ellis95; Gibson96
Female sex:
Yes: Baker31; Berz97; Henry29, Kostyun79; Bock49; Zuckerman98; Covassin84; Covassin73; Covassin53; Majerske85; Colvin99; Eisenberg68; Ellis95; Miller56; Preiss-Farzanegan(in adults)94; Heyer80; Zemek57
No: Chermann81; Moor100; Hang30; Nelson21; Mayers101; Asplund89; Black72; Chrisman75; Zuckerman102; Zuckerman103; Vargas74; Terwilliger83; Morgan58; Frommer52; Baker92; McDevitt88; Nelson78; Lax104; Ono105; Preiss-Farzanegan (in children/adolescents)94; Covassin106; Kontos67; Wasserman41; Yang107; Meehan90; Gibson96; Meehan6
Race (non-white):
No: McDevitt88; Asplund89; Morgan58; Yang107; Eisenberg68
Genetics:
No: McDevitt109
Prior concussions:
Yes: Hang30; Nelson21; Guskiewicz110; Castile39; Chrisman (football only)75; Zuckerman102; Morgan58; Covassin111; Kerr112; Colvin99; Meehan (binary)6; Meehan113; Miller56; Wasserman41; Slobounov114; Benson115; Corwin48; Bruce116; Eisenberg (if <1 year ago)68; Zemek57
No: Asken117; Barlow69; Moor100; Brown118; Lau87; Mautner55; McDevitt88; Vargas74; Terwilliger83; McCrea91; Meehan (number of injuries)6; Erlanger119; Majerske85; Baker92; Ellis95; Field82; Makdissi120; Pellman86; Gibson96; Heyer80; Miller56
ADHD:
Yes: Miller56
No: Asken117; Lau87; Mautner55; Hang30; Terwilliger83; Morgan58; Nelson78; Miller56; Eisenberg68; Zemek57
Learning disability:
Yes: Zemek57
No: Asken117; Lau87; Hang30; Asplund89; Morgan58; Nelson78; Eisenberg68
Prior psychiatric history:
Yes: Asken117; Morgan58; Eisenberg68; Ellis95; Yang107; Corwin48; Zemek57
No: Terwilliger83
Family psychiatric history:
No: None
Migraine (preinjury personal history):
Yes: Zemek57
No: Lau87; McDevitt88; Morgan58; Ellis95; Nelson78; Miller56; Eisenberg68; Meehan90; Meehan6
Family history of migraine:
Yes: Morgan58
Headache history:
Yes: Register-Mihalik121; Heyer80; Meehan6
No: Terwilliger83; Lau87; Nelson78; Meehan90
Note: First author and reference citation. Five studies by Iverson63 and Lau and colleagues (refs. 4, 66, 64 and 87) used the same cohort of football players and thus findings relating to specific predictors in boxes 1-3 are represented by only one of these five studies.
Box 2. Injury severity characteristics associated with recovery.
Loss of consciousness:
Yes: Chermann81; Pellman122; Guskiewicz110; Asplund89; McCrea91; Miller56; Benson115; Heyer80; Zemek57
No: Brown118; Guskiewicz123; Hinton-Bayre124; Nelson21; Bock49; Corwin48; Zuckerman102; Terwilliger83; Morgan58; Erlanger119; Lau4; McCrea25; Ellis95; Makdissi120; McDevitt88; Nelson78; Merritt5; Meehan6; Gibson96; Chrisman75; Collins 125; Meehan90
Post-traumatic amnesia/‘amnesia’:
Yes: Benson115; Chrisman75 (males only); Guskiewicz110; Heyer80; McCrea91; Lovell126; Collins125; Meehan6; Zuckerman102
No: Brown118; Guskiewicz123; Hinton-Bayre124; Nelson21; Asplund89; Bock49; Terwilliger83; Meehan90; Lau66; McCrea25; Ellis95; Makdissi120; Nelson (2016)78; Merritt5; Eisenberg68; Gibson96
Retrograde amnesia:
Yes: Asplund89; McCrea91; Zuckerman102; Nelson78; Pellman122
No: Lau66; Merritt5; Heyer80; Collins125; Nelson78;
Delayed removal from play/or additional head trauma:
Yes: Asken117; Terwilliger83; Heyer80
No: None
Note: First author and reference citation.
Box 3. Acute clinical characteristics associated with recovery.
Greater acute/subacute symptoms:
Yes: Chermann81; Brown118*; Hang30; Resch127; Castile39; Chrisman75; Zuckerman102; Meehan6*; Meehan*90; McCrea91; Benson115; Ellis95*; Greenhill93; Makdissi120; Nelson78; Merritt5; Heyer80; Iverson63; Collie128; Pellman122; Zemek57
No: Barlow69*; Moor100*; Morgan58
Acute headache:
Yes: Asplund89; Register-Mihalik129; Kontos130; Mihalik131; Benson115; Merritt5; Mihalik65 (acute ‘migraine’); Register-Mihalik121; Lau4; Zemek57
No: Mihalik65 (acute ‘headache’); Chrisman75
Acute dizziness:
Yes: Lau66; Erlanger119; Corwin48; Zemek57
No: McDevitt88; Benson115; Merritt5; Chrisman75; Pellman122; Makdissi120
Poor initial balance (objective):
Yes: Zemek57
No: Barlow69; McDevitt88; Nelson78; Lau66
Acute neuropsychological deficits:
No: Barlow69; Hang30; Nelson78; Pellman26
Note: First author and reference citation. *Some of these studies included both acute and subacute time periods, with most subjects being in the subacute time period.
Summary of relationship between clinical recovery after concussion and preinjury, injury-related and postinjury factors
We extracted statistically significant predictors as well as predictors that were not significantly different (see online supplementary table). Some studies examined single variables, such as age70 71 or sex.31 52 72 73 Most studies, however, examined multiple variables. In the online supplementary table and in boxes 1–3, we report variables that had a significant independent association with outcome. It is important to appreciate that when multivariable analyses are conducted, many univariate significant findings drop out.56 57 68 For example, Zemek and colleagues found 47 variables that were independently associated with persistent symptoms after 1 month, but in multivariable analyses only nine remained significant predictors.57
Numerous studies have reported that younger age is associated with worse outcome, whereas many have not (see box 1). Age effects were examined statistically in different ways across the studies. Moreover, some studies reporting no age effects sometimes had fairly restricted age ranges.74–77 There were, however, large studies that did not find meaningful age effects.21 78 Prior studies have usually shown a gradient effect, with professional athletes returning to sports faster than collegiate athletes, then followed by high school athletes. Some recent studies have not shown a difference in recovery time between high school and collegiate athletes, however.21 78 Many studies have reported an association between female sex and worse clinical outcome (see box 1). A comparable number of studies have not reported significant sex differences in outcomes. However, large-scale observational studies indicate that girls and young women are at greater risk for having symptoms that persist for more than a month.57 79 80
Many studies have found an association between prior concussions and worse clinical outcome, but it is interesting to note that a greater number of studies have not found this association (box 1). Several studies have examined the association between mental health history and outcome, with nearly all showing an association with worse outcome. Most research to date does not support an association between ADHD or learning disabilities and clinical outcome. Nearly all studies do not show an association between a personal history of migraine and worse clinical outcomes (box 1). However, one large multisite prospective study reported that a history of migraine was associated with risk for symptoms lasting more than 4 weeks.57 There was consistent evidence that acute and subacute postinjury headaches were associated with worse clinical outcomes (box 3).
Some studies have reported that loss of consciousness is associated with worse clinical outcome, but most have not (box 2). Similarly, some studies have reported that ‘amnesia’ and post-traumatic amnesia are associated with worse clinical outcomes after concussion, but most studies have reported negative findings (box 2). There was strong evidence of a relationship between acute or subacute symptom burden and worse clinical outcome, although a few studies have not found this association (box 3).
Discussion
Most children, adolescents and young adults who experience a sport-related concussion will recover, from a clinical perspective, within 1 month.39 41–43 132 However, it is important to appreciate that the subgroup of children and adolescents who are taken to the emergency department following a sport-related concussion is at much greater risk for symptoms lasting beyond a month.57 68 In a multisite Canadian study, 30% of these children and adolescents reported persistent symptoms after 4 weeks.57 Both within and beyond the first month following injury, it is well understood in research and clinical practice that there are individual differences in recovery trajectories. In general, the literature is complex, mixed and difficult to interpret definitively.
Six key considerations when interpreting this review
There are baseline (preinjury) differences in student athletes’ experiences with, and reporting of, concussion-like symptoms, and these baseline differences can complicate our understanding of the relationships between predictors and clinical outcome. Prior to injury, girls and young women report more symptoms than boys and young men in most studies.10 60 People with pre-existing developmental or health problems, such as ADHD,60 133–135 learning problems,60 134 135 a history of mental health60 or substance abuse problems,60 a history of treatment for headaches61 or migraines,60 or multiple prior concussions60 61 129 report more symptoms than people who do not have these conditions.
Student athletes with ADHD 133 136–139 or learning problems136 have a greater lifetime history of concussion, and individuals with a prior history of concussion are at increased risk for a future concussion.59 There might be important interactions between neurodevelopmental problems, multiple prior concussions and clinical recovery from a future concussion. In large-scale multivariate analyses of baseline preseason symptom reporting in adolescents, past concussion history is a significant predictor of baseline symptoms, but the magnitude of its relationship to symptom reporting is less than the factors such as ADHD, past mental health problems and a personal history of migraine.60 61
Student athletes with no known developmental or health problems, and no prior history of concussion, also report some non-specific concussion-like symptoms in their daily lives.60 These symptoms can be related to stress,140 depression,141 insufficient sleep141–143 and a variety of other factors.
The results for nearly all the potential predictors are mixed, and for the most-often studied predictors (eg, age, sex and prior concussion history) there are many studies that do not show a significant association. The quality of included studies was variable, and the methodologies varied considerably, and this might influence the strength of evidence. We suggest not simply relying on a summary count of the number of studies in boxes 1–3 that showed an association versus not, because the studies varied tremendously in when and how they measured outcomes, in sample sizes and statistical power, sport population representativeness and methodological quality (see online supplementary table for details regarding the methodological differences in these studies).
Extracting non-significant findings from empirical studies can be difficult because authors often emphasise significant findings and do not always report negative findings. It was not always clear whether a predictor was statistically examined and whether it was a negative finding. Therefore, it is likely that the number of negative findings presented in the boxes is an underestimate (ie, there is a risk for publication bias).
Many past studies on the topic of predictors examine athletes only in the first 1–2 weeks following injury. In recent years, there have been quite a few studies that have examined predictors of those who are slow to recover and have persistent symptoms beyond a month.
Relationship between age and clinical recovery
Age is one of the most frequently studied preinjury demographic and health factors that might be related to outcome. There is some, but not definitive, support for a gradient age and level of play effect with clinical recovery being fastest in professional athletes, followed by college athletes, followed by high school athletes. In a large prospective multicentre study57 of children and adolescents presenting to the emergency department, the rates of those having persistent symptoms beyond 4 weeks, stratified by age group, were as follows: 5–7=17.9%, 8–12=26.3% and 13–17=39.9%. This suggests that the teenage and high school years might represent the greatest age period of vulnerability for slow recovery. However, younger children have less ability to conceptualise and verbalise their symptoms—whereas teenagers have an emerging ability to think more abstractly and they have a greater vocabulary for symptoms—so part of the difference in symptom rates might actually reflect developmental differences in how children and adolescents experience and report symptoms. Adolescents might also be more vulnerable to the social psychological effects of having sustained a sport-related concussion or have different motivational factors influencing their recovery. More research in these areas is needed.
Relationship between sex and clinical recovery
The literature on recovery time and persistent symptoms is mixed, but overall supports that females, on average, take longer to recover—and they are more likely to have symptoms that persist for more than a month.49 56 57 68 Sex differences, such as differences in neck strength,144–147 injury biomechanics148 and injury rates149 in females compared with males, and the fact that women report more symptoms, as a group, both before and after sustaining an injury,10 might help to account for this finding.
Relationship between history of concussion and clinical recovery
Prior history of concussions was not related to clinical outcome after concussion in most studies. However, because prior history of concussion is a risk factor for future concussions,59 prior concussions are associated with greater preinjury symptom reporting in some athletes,60 61 and some large-scale studies show an association between concussion history and increased risk for symptoms lasting more than 4 weeks,48 56 57 we consider concussion history an important variable. More research is needed to determine whether the risk for future concussion is greater primarily in those who had slower recovery from a past concussion.57
Relationship between neurodevelopmental disorders, mental health, migraine and clinical recovery
Children with neurodevelopmental disorders, such as ADHD and learning disabilities, have a greater lifetime history of concussion,136 150 perform more poorly, as a group, on neuropsychological testing134 135 139 and report more concussion-like symptoms in their daily lives,60 133–135 in the absence of injury. The literature to date suggests that those with ADHD or learning problems may have different baseline scores on symptom and neurocognitive measures but they are not clearly at greater risk for worse outcome or slow recovery following injury.
Preinjury mental health problems,58 particularly depression,57 68 are a risk factor for persistent symptoms in a small number of studies. A preinjury history of migraine was not related to outcome in most studies, but it was related in one large multicentre, prospective, well-powered study.57 Studies typically rely on self-reported headache history on a questionnaire, and many adolescents and young adults might have difficulty differentiating ‘headache’ from ‘migraine’, which could contribute to the mixed findings. Acute and subacute postinjury headaches of any type are a risk factor for persistent symptoms in some studies. Therefore, having a history of migraine might confer increased risk for slower recovery, but more research is needed to definitively establish this association.
Relationship between surrogate measures of injury severity and clinical recovery
There is a long-standing interest in whether injury severity factors, such as loss of consciousness, retrograde amnesia and post-traumatic amnesia, are related to clinical outcome. The literature is mixed regarding these variables. Most concussions are not demarcated by loss of consciousness,42 and loss of consciousness is not a strong predictor of outcome in most studies. Therefore, we consider it a weak predictor. Post-traumatic amnesia was not related to outcome in most studies. Retrograde amnesia has more consistently been associated with short-term outcome15 than loss of consciousness and post-traumatic amnesia, but fewer studies show an association between retrograde amnesia and slower recovery time.89 91 102
The initial injury severity indicators are less important than the early clinical consequences (ie, symptom burden) of the injury. Many studies have illustrated that greater severity of acute and subacute symptoms following injury are associated with slower recovery (see box 3). A small number of studies indicate that greater acute cognitive deficits are associated with slower recovery.63 119 These are intuitive findings because greater acute cognitive impairment likely reflects greater adverse effects of injury on neurobiology, and greater acute symptom reporting likely reflects the combined effects of neurobiology, adverse acute psychological reactions and greater preinjury propensity towards experiencing symptoms.
Limitations
This systematic review has several methodological limitations. First, we did not rate risk of bias or the methodological quality of the articles. We simply extracted details regarding the methodology, results and rated the level of evidence (online supplementary table). Second, there is a potential for publication bias in our conclusions because we only reviewed published articles; studies with negative findings are less likely to be published. Third, there is potential for language bias influencing our conclusions because we only included English language articles. Fourth, we could not pool data across studies and meta-analyse individual predictors or multiple predictors in combination. Finally, conducting a best evidence synthesis would have allowed us to better weight the quality of evidence when making overall summary statements about the relationship between individual predictor variables and clinical recovery.
Conclusions
The strongest and most consistent predictor of slower recovery from concussion was greater severity of a person’s acute and subacute symptoms following injury. Having a low-level of symptoms in the first day or two following injury was a favourable prognostic indicator. The development of subacute problems with headaches or depression are likely risk factors for persistent symptoms lasting greater than a month. Children, adolescents and young adults with a preinjury history of mental health problems or migraine headaches appear to be at somewhat greater risk for having symptoms greater than 1 month. Those with ADHD or learning disabilities might require more careful planning and intervention regarding returning to school, but they do not appear to be at substantially greater risk for persistent symptoms beyond a month. The teenage years, particularly high school, might be the most vulnerable time for having persistent symptoms—with greater risk for girls than boys.
What is already known?
Concussions can have large adverse effects on cognitive functioning and balance in the first 24 hours following injury.
Athletes report diverse physical, cognitive and emotional symptoms acutely and subacutely.
A greater number and severity of symptoms after a concussion are predictors of a slower recovery in some studies.
A large percentage of injured athletes recover clinically within 10 days, and the large majority appear to recover within 1 month.
Injury severity characteristics, such as loss of consciousness, retrograde amnesia and post-traumatic amnesia are not consistent or strong predictors of recovery time in some studies.
What are the new findings?
For the majority of predictors, the literature is mixed with positive and negative findings.
Preinjury mental health problems and prior concussions appear to be risk factors for persistent symptoms.
Greater acute and subacute symptoms are a consistent predictor of worse clinical outcome.
The teenage years might be a particularly vulnerable time for having persistent symptoms—with greater risk for girls than boys.
Footnotes
Contributors: GLI and AJG wrote the first draft of the review. All authors participated in conceptualising the review, designing the search terms, reviewing the literature and extracting data from articles, reviewing drafts of the manuscript and approving the final draft for submission.
Competing interests: GLI has been reimbursed by the government, professional scientific bodies and commercial organisations for discussing or presenting research relating to mild TBI and sport-related concussion at meetings, scientific conferences and symposiums. He has a clinical and consulting practice in forensic neuropsychology involving individuals who have sustained mild TBIs (including professional athletes). He has been a principal investigator and coinvestigator on federal and industry grants on topics relating to mild traumatic brain injury, neuropsychological assessment and depression. He has received consulting fees from pharmaceutical companies. He receives royalties for books and one neuropsychological test. He has received research funding from several test publishing companies, including ImPACT Applications, Inc., CNS Vital Signs and Psychological Assessment Resources (PAR, Inc.). He acknowledges unrestricted philanthropic support from the Mooney-Reed Charitable Foundation and ImPACT Applications, Inc. He previously served as a contractor in the area of TBI research through General Dynamics for the Defense and Veterans Brain Injury Center within the US Department of Defense. He receives salary support for chairing the Brain and Behavior committee for the Harvard Integrated Program to Protect and Improve the Health of NFLPA Members. AJG has a clinical practice in neuropsychology involving individuals who have sustained sport-related concussion (including current and former athletes). He has operated as a contracted concussion consultant to the Australian Rugby Union (ARU) from July 2016. He has received travel funding from the Australian Football League (AFL) to present at the Concussion in Football Conference in 2013. Previous grant funding includes the NSW Sporting Injuries Committee, the Brain Foundation (Australia), and the Hunter Medical Research Institute (HMRI), supported by Jennie Thomas. He is currently funded through the HMRI, supported by Anne Greaves, and the University of Newcastle’s Priority Research Centre for Stroke and Brain Injury. JLP is an employee of Monash University and Epworth Healthcare and conducts a private practice conducting assessments for forensic purposes. She has received funding from the Rehaklinik Bellikon and Suvacare to present on the management of concussion in Zurich in 2013. She frequently presents on TBI-related topics at brain injury conferences and has received funding from the International Neuropsychological Society, the International Brain Injury Association and World Federation of NeuroRehabilitation, Federation of European Neuropsychological Societies, British Psychological Society, Norwegian Neuropsychological Society and various hospitals to do this. She has received grant support from the National Health and Medical Research Council, Institute for Safety Compensation and Recovery Research, Victorian Neurotrauma Initiative, the Australian Research Council, the William Buckland Foundation, Epworth Research Institute and Monash University for studies involving people with traumatic brain injury. AKS is a full-time employee of the Vanderbilt University Medical Center. He is an unpaid consulting neurosurgeon to the NHL Nashville Predators, the MiLB Nashville Sounds, Vanderbilt University athletics and Mississippi State University athletics. He serves as unpaid member of the Medical Committee for the International Equestrian Foundation (FEI) and on the NCAA Concussion Protocol Committee. He is section editor (unpaid) for Sports and Rehabilitation for the journal Neurosurgery. He also receives compensation to serve as Unaffiliated Neurotrauma Consultant for the National Football League. He receives no direct grant or research support for concussion research. DKB is a full-time employee of the University of Virginia School of Medicine. Clinically, she evaluates primarily high school and collegiate athletes who have sustained sports concussions. She is a member of the Concussion Committee for the National/Women’s Basketball Association (NBA/WNBA) and is president of the Sports Neuropsychology Society, but receives no compensation for either activity. She has received grant support towards her salary on sports concussion-related research from the US Department of Defense, NIH/NHLBI and the National Athletic Trainers Association Research and Education Foundation. She has received speaking honoraria for scientific presentations on sports concussion. GSS is a full-time employee of the Vanderbilt University Medical Center. He is a consulting neuropsychologist for the NHL Nashville Predators, NFL Tennessee Titans, University of Tennessee Athletics and Tennessee Tech Athletics, with all fees paid to institution. He is also a member of the ImPACT Scientific Advisory Board and receives expense reimbursements for attendance at board meetings. He has received speaking honoraria for presentations at scientific meetings related to concussion in sports. He receives some grant support from the Department of Defense (non-TBI related).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Dougan BK, Horswill MS, Geffen GM. Athletes' age, sex, and years of education moderate the acute neuropsychological impact of sports-related concussion: a meta-analysis. J Int Neuropsychol Soc 2014;20:64–80. 10.1017/S1355617712001464 [DOI] [PubMed] [Google Scholar]
- 2. Broglio SP, Puetz TW. The effect of sport concussion on neurocognitive function, self-report symptoms and postural control : a meta-analysis. Sports Med 2008;38:53–67. 10.2165/00007256-200838010-00005 [DOI] [PubMed] [Google Scholar]
- 3. Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med 2013;47:15–26. 10.1136/bjsports-2012-091941 [DOI] [PubMed] [Google Scholar]
- 4. Lau B, Lovell MR, Collins MW, et al. Neurocognitive and symptom predictors of recovery in high school Athletes. Clin J Sport Med 2009;19:216–21. 10.1097/JSM.0b013e31819d6edb [DOI] [PubMed] [Google Scholar]
- 5. Merritt VC, Rabinowitz AR, Arnett PA. Injury-related predictors of symptom severity following sports-related concussion. J Clin Exp Neuropsychol 2015;37:265–75. 10.1080/13803395.2015.1004303 [DOI] [PubMed] [Google Scholar]
- 6. Meehan WP, Mannix R, Monuteaux MC, et al. Early symptom burden predicts recovery after sport-related concussion. Neurology 2014;83:2204–10. 10.1212/WNL.0000000000001073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Foley C, Gregory A, Solomon G. Young age as a modifying factor in sports concussion management: what is the evidence? Curr Sports Med Rep 2014;13:390–4. 10.1249/JSR.0000000000000104 [DOI] [PubMed] [Google Scholar]
- 8. Scopaz KA, Hatzenbuehler JR. Risk modifiers for concussion and prolonged recovery. Sports Health 2013;5:537–41. 10.1177/1941738112473059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Makdissi M, Davis G, Jordan B, et al. Revisiting the modifiers: how should the evaluation and management of acute concussions differ in specific groups? Br J Sports Med 2013;47:314–20. 10.1136/bjsports-2013-092256 [DOI] [PubMed] [Google Scholar]
- 10. Brown DA, Elsass JA, Miller AJ, et al. Differences in Symptom Reporting between Males and Females at Baseline and after a Sports-Related concussion: a systematic review and Meta-Analysis. Sports Med 2015;45:1027–40. 10.1007/s40279-015-0335-6 [DOI] [PubMed] [Google Scholar]
- 11. Williams RM, Puetz TW, Giza CC, et al. Concussion recovery time among high school and collegiate Athletes: a systematic review and meta-analysis. Sports Med 2015;45:893–903. 10.1007/s40279-015-0325-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cancelliere C, Hincapié CA, Keightley M, et al. Systematic review of prognosis and return to play after sport concussion: results of the International Collaboration on Mild traumatic brain Injury Prognosis. Arch Phys Med Rehabil 2014;95:S210–29. 10.1016/j.apmr.2013.06.035 [DOI] [PubMed] [Google Scholar]
- 13. Karr JE, Areshenkoff CN, Garcia-Barrera MA. The neuropsychological outcomes of concussion: a systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology 2014;28:321–36. 10.1037/neu0000037 [DOI] [PubMed] [Google Scholar]
- 14. Solomon GS, Kuhn AW, Zuckerman SL. Depression as a modifying factor in Sport-Related concussion: a critical review of the Literature. Phys Sportsmed 2016;44:14–19. 10.1080/00913847.2016.1121091 [DOI] [PubMed] [Google Scholar]
- 15. Dougan BK, Horswill MS, Geffen GM. Do injury characteristics predict the severity of acute neuropsychological deficits following sports-related concussion? A meta-analysis. J Int Neuropsychol Soc 2014;20:81–7. 10.1017/S1355617713001288 [DOI] [PubMed] [Google Scholar]
- 16. Dick RW. Is there a gender difference in concussion incidence and outcomes? Br J Sports Med 2009;43(Suppl 1):i46–50. 10.1136/bjsm.2009.058172 [DOI] [PubMed] [Google Scholar]
- 17. Shim J, Smith DH, Van Lunen BL. On-field signs and symptoms associated with recovery duration after concussion in high school and college Athletes: a critically appraised topic. J Sport Rehabil 2015;24:72–6. 10.1123/jsr.2013-0058 [DOI] [PubMed] [Google Scholar]
- 18. Brook EM, Luo X, Curry EJ, et al. A heads up on concussions: are there sex-related differences? Phys Sportsmed 2016;44:20–8. 10.1080/00913847.2016.1142834 [DOI] [PubMed] [Google Scholar]
- 19. Kontos AP, Braithwaite R, Dakan S, et al. Computerized neurocognitive testing within 1 week of sport-related concussion: meta-analytic review and analysis of moderating factors. J Int Neuropsychol Soc 2014;20:324–32. 10.1017/S1355617713001471 [DOI] [PubMed] [Google Scholar]
- 20. McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA 2003;290:2556–63. 10.1001/jama.290.19.2556 [DOI] [PubMed] [Google Scholar]
- 21. Nelson LD, Guskiewicz KM, Barr WB, et al. Age differences in Recovery after Sport-Related Concussion: a comparison of High School and Collegiate Athletes. J Athl Train 2016;51:142–52. 10.4085/1062-6050-51.4.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bleiberg J, Cernich AN, Cameron K, et al. Duration of cognitive impairment after sports concussion. Neurosurgery 2004;54:1073–80. 10.1227/01.NEU.0000118820.33396.6A [DOI] [PubMed] [Google Scholar]
- 23. Lovell MR, Collins MW, Iverson GL, et al. Grade 1 or "ding" concussions in high school athletes. Am J Sports Med 2004;32:47–54. 10.1177/0363546503260723 [DOI] [PubMed] [Google Scholar]
- 24. Macciocchi SN, Barth JT, Alves W, et al. Neuropsychological functioning and recovery after mild head injury in collegiate Athletes. Neurosurgery 1996;39:510–4. [PubMed] [Google Scholar]
- 25. McCrea M, Kelly JP, Randolph C, et al. Immediate neurocognitive effects of concussion. Neurosurgery 2002;50:1032–40. [DOI] [PubMed] [Google Scholar]
- 26. Pellman EJ, Lovell MR, Viano DC, et al. Concussion in professional football: neuropsychological testing--part 6. Neurosurgery 2004;55:1290–305. 10.1227/01.NEU.0000149244.97560.91 [DOI] [PubMed] [Google Scholar]
- 27. McCrea M, Guskiewicz K, Randolph C, et al. Effects of a symptom-free waiting period on clinical outcome and risk of reinjury after sport-related concussion. Neurosurgery 2009;65:876–83. 10.1227/01.NEU.0000350155.89800.00 [DOI] [PubMed] [Google Scholar]
- 28. Guskiewicz KM, Weaver NL, Padua DA, et al. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med 2000;28:643–50. 10.1177/03635465000280050401 [DOI] [PubMed] [Google Scholar]
- 29. Henry LC, Elbin RJ, Collins MW, et al. Examining Recovery Trajectories after Sport-Related Concussion with a Multimodal Clinical Assessment Approach. Neurosurgery 2016;78:232–41. 10.1227/NEU.0000000000001041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hang B, Babcock L, Hornung R, et al. Can Computerized Neuropsychological Testing in the Emergency Department Predict Recovery for Young Athletes with Concussions? Pediatr Emerg Care 2015;31:688–93. 10.1097/PEC.0000000000000438 [DOI] [PubMed] [Google Scholar]
- 31. Baker JG, Leddy JJ, Darling SR, et al. Gender differences in Recovery from Sports-Related Concussion in Adolescents. Clin Pediatr 2016;55:771–5. 10.1177/0009922815606417 [DOI] [PubMed] [Google Scholar]
- 32. Pfaller AY, Nelson LD, Apps JN, et al. Frequency and Outcomes of a Symptom-Free Waiting Period After Sport-Related Concussion. Am J Sports Med 2016;44:2941–6. 10.1177/0363546516651821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. LaRoche AA, Nelson LD, Connelly PK, et al. Sport-Related Concussion Reporting and State legislative effects. Clin J Sport Med 2016;26:33–9. 10.1097/JSM.0000000000000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McCrory P. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med 2005;39:i78–86. 10.1136/bjsm.2005.018614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McCrory P, Meeuwisse W, Johnston K, et al. Consensus Statement on Concussion in Sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br J Sports Med 2009;43(Suppl 1):i76–84. 10.1136/bjsm.2009.058248 [DOI] [PubMed] [Google Scholar]
- 36. McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med 2013;47:250–8. 10.1136/bjsports-2013-092313 [DOI] [PubMed] [Google Scholar]
- 37. Yard EE, Comstock RD. Compliance with return to play guidelines following concussion in US high school Athletes, 2005-2008. Brain Inj 2009;23:888–98. 10.1080/02699050903283171 [DOI] [PubMed] [Google Scholar]
- 38. Kerr ZY, Zuckerman SL, Wasserman EB, et al. Concussion Symptoms and return to play Time in Youth, High School, and College American Football Athletes. JAMA Pediatr 2016;170:647–53. 10.1001/jamapediatrics.2016.0073 [DOI] [PubMed] [Google Scholar]
- 39. Castile L, Collins CL, McIlvain NM, et al. The epidemiology of new versus recurrent sports concussions among high school Athletes, 2005-2010. Br J Sports Med 2012;46:603–10. 10.1136/bjsports-2011-090115 [DOI] [PubMed] [Google Scholar]
- 40. Marar M, McIlvain NM, Fields SK, et al. Epidemiology of concussions among United States high school Athletes in 20 sports. Am J Sports Med 2012;40:747–55. 10.1177/0363546511435626 [DOI] [PubMed] [Google Scholar]
- 41. Wasserman EB, Kerr ZY, Zuckerman SL, et al. Epidemiology of Sports-Related Concussions in National Collegiate Athletic Association Athletes from 2009-2010 to 2013-2014: symptom prevalence, Symptom Resolution Time, and Return-to-Play Time. Am J Sports Med 2016;44:226–33. 10.1177/0363546515610537 [DOI] [PubMed] [Google Scholar]
- 42. Meehan WP, d'Hemecourt P, Comstock RD. High school concussions in the 2008-2009 academic year: mechanism, symptoms, and management. Am J Sports Med 2010;38:2405–9. 10.1177/0363546510376737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McKeon JM, Livingston SC, Reed A, et al. Trends in concussion return-to-play timelines among high school Athletes from 2007 through 2009. J Athl Train 2013;48:836–43. 10.4085/1062-6050-48.6.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vagnozzi R, Signoretti S, Floris R, et al. Decrease in N-acetylaspartate following concussion may be coupled to decrease in creatine. J Head Trauma Rehabil 2013;28:284–92. 10.1097/HTR.0b013e3182795045 [DOI] [PubMed] [Google Scholar]
- 45. Vagnozzi R, Signoretti S, Cristofori L, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain 2010;133:3232–42. 10.1093/brain/awq200 [DOI] [PubMed] [Google Scholar]
- 46. Wright AD, Jarrett M, Vavasour I, et al. Myelin Water Fraction is transiently reduced after a single mild traumatic brain Injury--A prospective Cohort Study in Collegiate hockey players. PLoS One 2016;11:e0150215 10.1371/journal.pone.0150215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wang Y, Nelson LD, LaRoche AA, et al. Cerebral blood flow alterations in acute Sports-Related concussion. J Neurotrauma 2015;10:1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Corwin DJ, Zonfrillo MR, Master CL, et al. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. J Pediatr 2014;165:1207–15. 10.1016/j.jpeds.2014.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bock S, Grim R, Barron TF, et al. Factors associated with delayed recovery in Athletes with concussion treated at a pediatric neurology concussion clinic. Childs Nerv Syst 2015;31:2111–6. 10.1007/s00381-015-2846-8 [DOI] [PubMed] [Google Scholar]
- 50. Merritt VC, Arnett PA, Apolipoprotein E. Apolipoprotein E (APOE) ϵ4 allele is associated with increased Symptom Reporting following Sports Concussion. J Int Neuropsychol Soc 2016;22:89–94. 10.1017/S1355617715001022 [DOI] [PubMed] [Google Scholar]
- 51. Stone S, Lee B, Garrison JC, et al. Sex Differences in Time to Return-to-Play Progression After Sport-Related Concussion. Sports Health 2016. (Epub ahead of print: 3 Oct 2016). 10.1177/1941738116672184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Frommer LJ, Gurka KK, Cross KM, et al. Sex differences in concussion symptoms of high school Athletes. J Athl Train 2011;46:76–84. 10.4085/1062-6050-46.1.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Covassin T, Moran R, Elbin RJ. Sex differences in reported concussion Injury Rates and Time loss from participation: an Update of the National Collegiate Athletic Association Injury Surveillance Program from 2004-2005 through 2008-2009. J Athl Train 2016;51:189–94. 10.4085/1062-6050-51.3.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Covassin T, Elbin RJ, Harris W, et al. The role of age and sex in symptoms, neurocognitive performance, and postural stability in Athletes after concussion. Am J Sports Med 2012;40:1303–12. 10.1177/0363546512444554 [DOI] [PubMed] [Google Scholar]
- 55. Mautner K, Sussman WI, Axtman M, et al. Relationship of attention deficit hyperactivity disorder and Postconcussion Recovery in Youth Athletes. Clin J Sport Med 2015;25:355–60. 10.1097/JSM.0000000000000151 [DOI] [PubMed] [Google Scholar]
- 56. Miller JH, Gill C, Kuhn EN, et al. Predictors of delayed recovery following pediatric sports-related concussion: a case-control study. J Neurosurg Pediatr 2016;17:491–6. 10.3171/2015.8.PEDS14332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for Persistent Postconcussion Symptoms among Children with Acute concussion in the ED. JAMA 2016;315:1014–25. 10.1001/jama.2016.1203 [DOI] [PubMed] [Google Scholar]
- 58. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports-related concussion in young Athletes: a matched case-control study. J Neurosurg Pediatr 2015;15:589–98. 10.3171/2014.10.PEDS14356 [DOI] [PubMed] [Google Scholar]
- 59. Abrahams S, Fie SM, Patricios J, et al. Risk factors for sports concussion: an evidence-based systematic review. Br J Sports Med 2014;48:91–7. 10.1136/bjsports-2013-092734 [DOI] [PubMed] [Google Scholar]
- 60. Iverson GL, Silverberg ND, Mannix R, et al. Factors associated with Concussion-like Symptom Reporting in High School Athletes. JAMA Pediatr 2015;169:1132–40. 10.1001/jamapediatrics.2015.2374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Brooks BL, Mannix R, Maxwell B, et al. Multiple Past Concussions in High School Football Players: are there differences in cognitive functioning and Symptom Reporting? Am J Sports Med 2016;44:3243–51. 10.1177/0363546516655095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Collins MW, Iverson GL, Lovell MR, et al. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med 2003;13:222–9. 10.1097/00042752-200307000-00005 [DOI] [PubMed] [Google Scholar]
- 63. Iverson G. Predicting slow recovery from sport-related concussion: the new simple-complex distinction. Clin J Sport Med 2007;17:31–7. 10.1097/JSM.0b013e3180305e4d [DOI] [PubMed] [Google Scholar]
- 64. Lau BC, Collins MW, Lovell MR. Sensitivity and specificity of subacute computerized neurocognitive testing and symptom evaluation in predicting outcomes after sports-related concussion. Am J Sports Med 2011;39:1209–16. 10.1177/0363546510392016 [DOI] [PubMed] [Google Scholar]
- 65. Mihalik JP, Register-Mihalik J, Kerr ZY, et al. Recovery of posttraumatic migraine characteristics in patients after mild traumatic brain injury. Am J Sports Med 2013;41:1490–6. 10.1177/0363546513487982 [DOI] [PubMed] [Google Scholar]
- 66. Lau BC, Kontos AP, Collins MW, et al. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players? Am J Sports Med 2011;39:2311–8. 10.1177/0363546511410655 [DOI] [PubMed] [Google Scholar]
- 67. Kontos AP, Covassin T, Elbin RJ, et al. Depression and neurocognitive performance after concussion among male and female high school and collegiate Athletes. Arch Phys Med Rehabil 2012;93:1751–6. 10.1016/j.apmr.2012.03.032 [DOI] [PubMed] [Google Scholar]
- 68. Eisenberg MA, Andrea J, Meehan W, et al. Time interval between concussions and symptom duration. Pediatrics 2013;132:8–17. 10.1542/peds.2013-0432 [DOI] [PubMed] [Google Scholar]
- 69. Barlow M, Schlabach D, Peiffer J, et al. Differences in change scores and the predictive validity of three commonly used measures following concussion in the middle school and high school aged population. Int J Sports Phys Ther 2011;6:150–7. [PMC free article] [PubMed] [Google Scholar]
- 70. Lee YM, Odom MJ, Zuckerman SL, et al. Does age affect symptom recovery after sports-related concussion? A study of high school and college Athletes. J Neurosurg Pediatr 2013;12:537–44. 10.3171/2013.7.PEDS12572 [DOI] [PubMed] [Google Scholar]
- 71. Zuckerman SL, Lee YM, Odom MJ, et al. Recovery from sports-related concussion: days to return to neurocognitive baseline in adolescents versus young adults. Surg Neurol Int 2012;3:130 10.4103/2152-7806.102945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Black AM, Sergio LE, Macpherson AK. The Epidemiology of Concussions: number and Nature of Concussions and Time to Recovery among female and male canadian Varsity Athletes 2008 to 2011. Clin J Sport Med 2017;27:1–5. 10.1097/JSM.0000000000000308 [DOI] [PubMed] [Google Scholar]
- 73. Covassin T, Elbin RJ, Bleecker A, et al. Are there differences in neurocognitive function and symptoms between male and female soccer players after concussions? Am J Sports Med 2013;41:2890–5. 10.1177/0363546513509962 [DOI] [PubMed] [Google Scholar]
- 74. Vargas G, Rabinowitz A, Meyer J, et al. Predictors and prevalence of postconcussion depression symptoms in collegiate Athletes. J Athl Train 2015;50:250–5. 10.4085/1062-6050-50.3.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Chrisman SP, Rivara FP, Schiff MA, et al. Risk factors for concussive symptoms 1 week or longer in high school Athletes. Brain Inj 2013;27:1–9. 10.3109/02699052.2012.722251 [DOI] [PubMed] [Google Scholar]
- 76. Lau BC, Collins MW, Lovell MR. Cutoff scores in neurocognitive testing and symptom clusters that predict protracted recovery from concussions in high school Athletes. Neurosurgery 2012;70:371–9. 10.1227/NEU.0b013e31823150f0 [DOI] [PubMed] [Google Scholar]
- 77. Kriz PK, Stein C, Kent J, et al. Physical maturity and Concussion Symptom Duration among Adolescent Ice hockey players. J Pediatr 2016;171:234–9. 10.1016/j.jpeds.2015.12.006 [DOI] [PubMed] [Google Scholar]
- 78. Nelson LD, Tarima S, LaRoche AA, et al. Preinjury somatization symptoms contribute to clinical recovery after sport-related concussion. Neurology 2016;86:1856–63. 10.1212/WNL.0000000000002679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kostyun RO, Hafeez I. Protracted recovery from a concussion: a focus on gender and treatment interventions in an adolescent population. Sports Health 2015;7:52–7. 10.1177/1941738114555075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Heyer GL, Schaffer CE, Rose SC, et al. Specific factors influence Postconcussion Symptom Duration among Youth referred to a Sports Concussion Clinic. J Pediatr 2016;174:33–8. 10.1016/j.jpeds.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 81. Chermann JF, Klouche S, Savigny A, et al. Return to rugby after brain concussion: a prospective study in 35 high level rugby players. Asian J Sports Med 2014;5:e24042 10.5812/asjsm.24042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Field M, Collins MW, Lovell MR, et al. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate Athletes. J Pediatr 2003;142:546–53. 10.1067/mpd.2003.190 [DOI] [PubMed] [Google Scholar]
- 83. Terwilliger VK, Pratson L, Vaughan CG, et al. Additional Post-Concussion Impact exposure May Affect Recovery in Adolescent Athletes. J Neurotrauma 2016;33:761–5. 10.1089/neu.2015.4082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Covassin T, Elbin RJ, Harris W, et al. The role of age and sex in symptoms, neurocognitive performance, and postural stability in Athletes after concussion. Am J Sports Med 2012;40:1303–12. 10.1177/0363546512444554 [DOI] [PubMed] [Google Scholar]
- 85. Majerske CW, Mihalik JP, Ren D, et al. Concussion in sports: postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train 2008;43:265–74. 10.4085/1062-6050-43.3.265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Pellman EJ, Lovell MR, Viano DC, et al. Concussion in Professional Football: recovery of NFL and High School Athletes assessed by Computerized Neuropsychological Testing-Part 12. Neurosurgery 2006;58:263–74. 10.1227/01.NEU.0000200272.56192.62 [DOI] [PubMed] [Google Scholar]
- 87. Lau BC, Collins MW, Lovell MR. Cutoff scores in neurocognitive testing and symptom clusters that predict protracted recovery from concussions in high school athletes. Neurosurgery 2012;70:371–9. 10.1227/NEU.0b013e31823150f0 [DOI] [PubMed] [Google Scholar]
- 88. McDevitt J, Tierney RT, Phillips J, et al. Association between GRIN2A promoter polymorphism and recovery from concussion. Brain Inj 2015;29:1674–81. 10.3109/02699052.2015.1075252 [DOI] [PubMed] [Google Scholar]
- 89. Asplund CA, McKeag DB, Olsen CH. Sport-related concussion: factors associated with prolonged return to play. Clin J Sport Med 2004;14:339–43. [DOI] [PubMed] [Google Scholar]
- 90. Meehan WP, Mannix RC, Stracciolini A, et al. Symptom severity predicts prolonged recovery after sport-related concussion, but age and amnesia do not. J Pediatr 2013;163:721–5. 10.1016/j.jpeds.2013.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. McCrea M, Guskiewicz K, Randolph C, et al. Incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college Athletes. J Int Neuropsychol Soc 2013;19:22–33. 10.1017/S1355617712000872 [DOI] [PubMed] [Google Scholar]
- 92. Baker JG, Leddy JJ, Darling SR, et al. Factors associated with problems for adolescents returning to the Classroom after Sport-Related Concussion. Clin Pediatr 2015;54:961–8. 10.1177/0009922815588820 [DOI] [PubMed] [Google Scholar]
- 93. Greenhill DA, Navo P, Zhao H, et al. Inadequate Helmet Fit increases Concussion Severity in American High School Football Players. Sports Health 2016;8:238–43. 10.1177/1941738116639027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Preiss-Farzanegan SJ, Chapman B, Wong TM, et al. The relationship between gender and postconcussion symptoms after sport-related mild traumatic brain injury. Pm R 2009;1:245–53. 10.1016/j.pmrj.2009.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Ellis MJ, Ritchie LJ, Koltek M, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr 2015;16:709–18. 10.3171/2015.5.PEDS15220 [DOI] [PubMed] [Google Scholar]
- 96. Gibson S, Nigrovic LE, O'Brien M, et al. The effect of recommending cognitive rest on recovery from sport-related concussion. Brain Inj 2013;27:839–42. 10.3109/02699052.2013.775494 [DOI] [PubMed] [Google Scholar]
- 97. Berz K, Divine J, Foss KB, et al. Sex-specific differences in the severity of symptoms and recovery rate following sports-related concussion in young Athletes. Phys Sportsmed 2013;41:58–63. 10.3810/psm.2013.05.2015 [DOI] [PubMed] [Google Scholar]
- 98. Zuckerman SL, Apple RP, Odom MJ, et al. Effect of sex on symptoms and return to baseline in sport-related concussion. J Neurosurg Pediatr 2014;13:72–81. 10.3171/2013.9.PEDS13257 [DOI] [PubMed] [Google Scholar]
- 99. Colvin AC, Mullen J, Lovell MR, et al. The role of concussion history and gender in recovery from soccer-related concussion. Am J Sports Med 2009;37:1699–704. 10.1177/0363546509332497 [DOI] [PubMed] [Google Scholar]
- 100. Moor HM, Eisenhauer RC, Killian KD, et al. The relationship between adherence behaviors and recovery time in adolescents after a sports-related concussion: an observational study. Int J Sports Phys Ther 2015;10:225–33. [PMC free article] [PubMed] [Google Scholar]
- 101. Mayers LB. Outcomes of sport-related concussion among college Athletes. J Neuropsychiatry Clin Neurosci 2013;25:115–9. 10.1176/appi.neuropsych.11120374 [DOI] [PubMed] [Google Scholar]
- 102. Zuckerman SL, Yengo-Kahn AM, Buckley TA, et al. Predictors of postconcussion syndrome in collegiate student-athletes. Neurosurg Focus 2016;40:E13 10.3171/2016.1.FOCUS15593 [DOI] [PubMed] [Google Scholar]
- 103. Zuckerman SL, Solomon GS, Forbes JA, et al. Response to acute concussive injury in soccer players: is gender a modifying factor? J Neurosurg Pediatr 2012;10:504–10. 10.3171/2012.8.PEDS12139 [DOI] [PubMed] [Google Scholar]
- 104. Lax ID, Paniccia M, Agnihotri S, et al. Developmental and gender influences on executive function following concussion in youth hockey players. Brain Inj 2015;29:1409–19. 10.3109/02699052.2015.1043344 [DOI] [PubMed] [Google Scholar]
- 105. Ono KE, Burns TG, Bearden DJ, et al. Sex-Based differences as a predictor of Recovery Trajectories in Young Athletes after a Sports-Related concussion. Am J Sports Med 2016;44:748–52. 10.1177/0363546515617746 [DOI] [PubMed] [Google Scholar]
- 106. Covassin T, Schatz P, Swanik CB. Sex differences in neuropsychological function and post-concussion symptoms of concussed collegiate Athletes. Neurosurgery 2007;61:345–51. 10.1227/01.NEU.0000279972.95060.CB [DOI] [PubMed] [Google Scholar]
- 107. Yang J, Peek-Asa C, Covassin T, et al. Post-concussion symptoms of depression and anxiety in division I collegiate Athletes. Dev Neuropsychol 2015;40:18–23. 10.1080/87565641.2014.973499 [DOI] [PubMed] [Google Scholar]
- 108. Kontos AP, Elbin RJ, Covassin T, et al. Exploring differences in computerized neurocognitive concussion testing between african american and white Athletes. Arch Clin Neuropsychol 2010;25:734–44. 10.1093/arclin/acq068 [DOI] [PubMed] [Google Scholar]
- 109. McDevitt JK, Tierney RT, Mansell JL, et al. Neuronal structural protein polymorphism and concussion in college Athletes. Brain Inj 2011;25:1108–13. 10.3109/02699052.2011.607790 [DOI] [PubMed] [Google Scholar]
- 110. Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA 2003;290:2549–55. 10.1001/jama.290.19.2549 [DOI] [PubMed] [Google Scholar]
- 111. Covassin T, Moran R, Wilhelm K. Concussion symptoms and neurocognitive performance of high school and college athletes who incur multiple concussions. Am J Sports Med 2013;41:2885–9. 10.1177/0363546513499230 [DOI] [PubMed] [Google Scholar]
- 112. Kerr ZY, DeFreese JD, Marshall SW. Current Physical and Mental Health of Former Collegiate Athletes. Orthop J Sports Med 2014;2:1–9. 10.1177/2325967114544107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Meehan WP, Mannix RC, O'Brien MJ, et al. The prevalence of undiagnosed concussions in athletes. Clin J Sport Med 2013;23:339–42. 10.1097/JSM.0b013e318291d3b3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Slobounov S, Slobounov E, Sebastianelli W, et al. Differential rate of recovery in athletes after first and second concussion episodes. Neurosurgery 2007;61:338–44. 10.1227/01.NEU.0000280001.03578.FF [DOI] [PubMed] [Google Scholar]
- 115. Benson BW, Meeuwisse WH, Rizos J, et al. A prospective study of concussions among National hockey League players during regular season games: the NHL-NHLPA Concussion Program. CMAJ 2011;183:905–11. 10.1503/cmaj.092190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Bruce JM, Echemendia RJ. Concussion history predicts self-reported symptoms before and following a concussive event. Neurology 2004;63:1516–8. 10.1212/01.WNL.0000142088.32204.82 [DOI] [PubMed] [Google Scholar]
- 117. Asken BM, McCrea MA, Clugston JR, et al. "Playing Through It": Delayed Reporting and Removal From Athletic Activity After Concussion Predicts Prolonged Recovery. J Athl Train 2016;51:329–35. 10.4085/1062-6050-51.5.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Brown NJ, Mannix RC, O'Brien MJ, et al. Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics 2014;133:e299–304. 10.1542/peds.2013-2125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Erlanger D, Kaushik T, Cantu R, et al. Symptom-based assessment of the severity of a concussion. J Neurosurg 2003;98:477–84. 10.3171/jns.2003.98.3.0477 [DOI] [PubMed] [Google Scholar]
- 120. Makdissi M, Darby D, Maruff P, et al. Natural history of concussion in sport: markers of severity and implications for management. Am J Sports Med 2010;38:464–71. 10.1177/0363546509349491 [DOI] [PubMed] [Google Scholar]
- 121. Register-Mihalik J, Guskiewicz KM, Mann JD, et al. The effects of headache on clinical measures of neurocognitive function. Clin J Sport Med 2007;17:282–8. 10.1097/JSM.0b013e31804ca68a [DOI] [PubMed] [Google Scholar]
- 122. Pellman EJ, Viano DC, Casson IR, et al. Concussion in professional football: injuries involving 7 or more days out--Part 5. Neurosurgery 2004;55:1100–19. 10.1227/01.NEU.0000147063.12873.F5 [DOI] [PubMed] [Google Scholar]
- 123. Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after Concussion in Collegiate Athletes. J Athl Train 2001;36:263–73. [PMC free article] [PubMed] [Google Scholar]
- 124. Hinton-Bayre AD, Geffen G. Severity of sports-related concussion and neuropsychological test performance. Neurology 2002;59:1068–70. 10.1212/WNL.59.7.1068 [DOI] [PubMed] [Google Scholar]
- 125. Collins MW, Field M, Lovell MR, et al. Relationship between postconcussion headache and neuropsychological test performance in high school Athletes. Am J Sports Med 2003;31:168–73. 10.1177/03635465030310020301 [DOI] [PubMed] [Google Scholar]
- 126. Lovell MR, Collins MW, Iverson GL, et al. Recovery from mild concussion in high school Athletes. J Neurosurg 2003;98:296–301. 10.3171/jns.2003.98.2.0296 [DOI] [PubMed] [Google Scholar]
- 127. Resch JE, Brown CN, Macciocchi SN, et al. A preliminary formula to predict timing of Symptom Resolution for Collegiate Athletes diagnosed with Sport Concussion. J Athl Train 2015;50:1292–8. 10.4085/1062-6050-50.12.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Collie A, Makdissi M, Maruff P, et al. Cognition in the days following concussion: comparison of symptomatic versus asymptomatic Athletes. J Neurol Neurosurg Psychiatry 2006;77:241–5. 10.1136/jnnp.2005.073155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Register-Mihalik JK, Mihalik JP, Guskiewicz KM. Association between Previous Concussion history and Symptom Endorsement during Preseason Baseline Testing in High School and Collegiate Athletes. Sports Health 2009;1:61–5. 10.1177/1941738108325920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Kontos AP, Elbin RJ, Newcomer Appaneal R, et al. A comparison of coping responses among high school and college athletes with concussion, orthopedic injuries, and healthy controls. Res Sports Med 2013;21:367–79. 10.1080/15438627.2013.825801 [DOI] [PubMed] [Google Scholar]
- 131. Mihalik JP, Stump JE, Collins MW, et al. Posttraumatic migraine characteristics in Athletes following sports-related concussion. J Neurosurg 2005;102:850–5. 10.3171/jns.2005.102.5.0850 [DOI] [PubMed] [Google Scholar]
- 132. Marar M, McIlvain NM, Fields SK, et al. Epidemiology of concussions among United States high school Athletes in 20 sports. Am J Sports Med 2012;40:747–55. 10.1177/0363546511435626 [DOI] [PubMed] [Google Scholar]
- 133. Nelson LD, Guskiewicz KM, Marshall SW, et al. Multiple Self-Reported Concussions are more prevalent in Athletes with ADHD and Learning Disability. Clin J Sport Med 2016;26:120–7. 10.1097/JSM.0000000000000207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Zuckerman SL, Lee YM, Odom MJ, et al. Baseline neurocognitive scores in Athletes with attention deficit-spectrum disorders and/or learning disability. J Neurosurg Pediatr 2013;12:103–9. 10.3171/2013.5.PEDS12524 [DOI] [PubMed] [Google Scholar]
- 135. Elbin RJ, Kontos AP, Kegel N, et al. Individual and combined effects of LD and ADHD on computerized neurocognitive concussion test performance: evidence for separate norms. Arch Clin Neuropsychol 2013;28:476–84. 10.1093/arclin/act024 [DOI] [PubMed] [Google Scholar]
- 136. Iverson GL, Wojtowicz M, Brooks BL, et al. High School Athletes With ADHD and Learning Difficulties Have a Greater Lifetime Concussion History. J Atten Disord 2016. (Epub ahead of print: 18 Jul 2016). 10.1177/1087054716657410 [DOI] [PubMed] [Google Scholar]
- 137. Iverson GL, Atkins JE, Zafonte R, et al. Concussion History in Adolescent Athletes with Attention-Deficit Hyperactivity Disorder. J Neurotrauma 2016;33:2077–80. 10.1089/neu.2014.3424 [DOI] [PubMed] [Google Scholar]
- 138. Alosco ML, Fedor AF, Gunstad J. Attention deficit hyperactivity disorder as a risk factor for concussions in NCAA division-I Athletes. Brain Inj 2014;28:472–4. 10.3109/02699052.2014.887145 [DOI] [PubMed] [Google Scholar]
- 139. Salinas CM, Dean P, LoGalbo A, et al. Attention-Deficit hyperactivity disorder status and Baseline Neurocognitive Performance in High School Athletes. Appl Neuropsychol Child 2016;5:264–72. 10.1080/21622965.2015.1052814 [DOI] [PubMed] [Google Scholar]
- 140. Edmed S, Sullivan K. Depression, anxiety, and stress as predictors of postconcussion-like symptoms in a non-clinical sample. Psychiatry Res 2012;200:41–5. 10.1016/j.psychres.2012.05.022 [DOI] [PubMed] [Google Scholar]
- 141. Covassin T, Elbin RJ, Larson E, et al. Sex and age differences in depression and baseline sport-related concussion neurocognitive performance and symptoms. Clin J Sport Med 2012;22:98–104. 10.1097/JSM.0b013e31823403d2 [DOI] [PubMed] [Google Scholar]
- 142. McClure DJ, Zuckerman SL, Kutscher SJ, et al. Baseline neurocognitive testing in sports-related concussions: the importance of a prior night's sleep. Am J Sports Med 2014;42:472–8. 10.1177/0363546513510389 [DOI] [PubMed] [Google Scholar]
- 143. Mihalik JP, Lengas E, Register-Mihalik JK, et al. The effects of sleep quality and sleep quantity on concussion baseline assessment. Clin J Sport Med 2013;23:343–8. 10.1097/JSM.0b013e318295a834 [DOI] [PubMed] [Google Scholar]
- 144. Eckner JT, Oh YK, Joshi MS, et al. Effect of neck muscle strength and anticipatory cervical muscle activation on the kinematic response of the head to impulsive loads. Am J Sports Med 2014;42:566–76. 10.1177/0363546513517869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Tierney RT, Sitler MR, Swanik CB, et al. Gender differences in head-neck segment dynamic stabilization during head acceleration. Med Sci Sports Exerc 2005;37:272–9. 10.1249/01.MSS.0000152734.47516.AA [DOI] [PubMed] [Google Scholar]
- 146. Collins CL, Fletcher EN, Fields SK, et al. Neck strength: a protective factor reducing risk for concussion in high school sports. J Prim Prev 2014;35:309–19. 10.1007/s10935-014-0355-2 [DOI] [PubMed] [Google Scholar]
- 147. Hrysomallis C. Neck Muscular Strength, Training, Performance and Sport Injury Risk: A Review. Sports Med 2016;46:1111–24. 10.1007/s40279-016-0490-4 [DOI] [PubMed] [Google Scholar]
- 148. Wilcox BJ, Beckwith JG, Greenwald RM, et al. Head impact exposure in male and female collegiate ice hockey players. J Biomech 2014;47:109–14. 10.1016/j.jbiomech.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Dick RW. Is there a gender difference in concussion incidence and outcomes? Br J Sports Med 2009;43(Suppl 1):i46–50. 10.1136/bjsm.2009.058172 [DOI] [PubMed] [Google Scholar]
- 150. Iverson GL, Atkins JE, Zafonte R, et al. Concussion History in Adolescent Athletes with Attention-Deficit Hyperactivity Disorder. J Neurotrauma 2016;33:2077–80. 10.1089/neu.2014.3424 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2017-097729supp001.docx (57KB, docx)