Abstract
Background
Coronary artery calcification (CAC) is a predictor of cardiovascular events and plaque burden and is closely associated with chronic inflammation. Interleukin (IL)-37 is a newly discovered member of the IL-1 family and is considered an anti-inflammatory cytokine. Our recent study on mice indicated that IL-37 could attenuate atherosclerosis and vascular calcification, which suggests that IL-37 could be associated with the development of atherosclerosis and related diseases. The aim of this study was to investigate if IL-37 plays a role in the progression of CAC in patients.
Methods
Two hundred participants with suspected cardiovascular disease were recruited. The levels of plasma IL-37, osteoprotegerin (OPG), hypersensitive C-reactive protein (hsCRP) together with other biochemical parameters were measured, and a coronary calcium assessment was carried out by multi-detector row CT. A score of < 10 AU (Agatston units) denotes an absence of CAC, a score of 11–100 AU denotes mild CAC, 101–400 denotes moderate CAC, and > 400 AU denotes severe CAC.
Results
Our initial data showed that there were no apparent differences in plasma IL-37 levels among patients with or without mild or moderate CAC. However, IL-37 levels were significantly increased in patients with severe CAC (P < 0.001). Similar results were observed for plasma OPG and hsCRP levels. When IL-37 levels in patients with severe calcification were compared with that in all of the other non-severe CAC groups, it became apparent that there was a significant positive correlation between IL-37 level and severe CAC (r = 0.360, P < 0.001; OR = 1.033) using Spearman's correlation and binary logistic regression analysis.
Conclusions
This study demonstrates that the anti-inflammatory cytokine IL-37 is associated with high coronary calcium levels, suggesting that IL-37 expression may be caused by the activation of inflammation and that IL-37 might become a predictor of severe CAC in the future, which requires further investigation.
Keywords: Coronary artery calcification, High-sensitivity C-reactive protein, Interleukin-37, Osteoprotegerin
1. Introduction
Coronary artery calcification (CAC) is a pathological deposition of minerals that can occur with either atherosclerosis or arteriosclerosis and has been used as a predictor of cardiovascular events and plaque burden.[1] From a clinical point of view, the amount of CAC is associated with the total atherosclerotic plaque burden and therefore can serve as a measure of subclinical atherosclerosis.[2] Furthermore, CAC scores also reflect the long-term impact of elevated cardiovascular disease (CVD) risk factors and can be used to predict the future risk of CVD events.[3]
For several decades, vascular calcification has been a known consequence of ageing. Recent studies have confirmed that vascular calcification is an actively regulated process and shares many features with bone development and metabolism;[4] the process is also closely related with chronic inflammation.[5] Macrophages, lymphocytes, and dendritic cells infiltrate the plaque and release cytokines that regulate calcification.[6] Perivascular adipose,[7] and systemic inflammation[8] may also contribute to both neointimal and medial calcification. The newly discovered interleukin-1 (IL-1) family member IL-37 is an anti-inflammatory cytokine.[9],[10] Our study has recently shown that in animal models, IL-37 plays a protective role in the development of vascular calcification and atherosclerosis.[11] We have also demonstrated that the levels of IL-37 were substantially increased in patients with acute coronary syndrome (ACS).[12] The increase of IL-37 may be induced in an inflammatory context.
Calcification typically follows the development of atherosclerotic lesions while inflammation is involved in the progression of arterial calcification; therefore, it is likely that inflammation-related cytokine IL-37 is involved in the progression of CAC. In the present study, we measured the levels of IL-37 in patients with suspected coronary artery disease (CAD) and compared their IL-37 levels with their CAC severity. Osteoprotegerin (OPG) is a well-known inhibitory factor of vascular calcification and we have, in the past, observed a positive correlation between IL-37 and OPG in an animal model.[11] Additionally, high-sensitivity C-reactive protein (hs-CRP) is known as a non-specific marker of inflammation. Therefore, we here additionally assessed and compared the plasma levels of OPG and hs-CRP in patients.
2. Methods
2.1. Study design
Two hundred consecutive patients with suspected CAD who have undergone coronary calcium assessment by multi-detector row CT were recruited from July 2013 to July 2015. Indications for the calcium scan included risk stratification purposes in individuals with an enhanced likelihood for future CAD events as based on traditional risk factors or individuals with atypical chest pain. We excluded participants who had any of the following conditions: (1) older than 80 years of age; (2) a history of percutaneous coronary intervention and/or coronary artery bypass grafting; (3) a history of atrial fibrillation; and (4) had ACS within the last three months.
After providing written informed consent, the patients were asked to complete a brief questionnaire. Atherogenic risk factors of the patients were assessed, and the criteria for diabetes, hypertension and hyperlipidaemia were based on a physician's diagnosis. The study was approved by the institutional ethics committee for human subjects.
2.2. Blood sample test
Fasting blood samples were collected in the morning immediately before performing the CT scan and were stored at 4°C for less than 4 h before processing. The samples were collected into sodium heparin Vacutainers (Becton-Dickinson). Blood was centrifuged for 15 min at 2000 × g, and the serum was stored at −80 °C until the assays were performed.
The levels of total cholesterol, high- and low-density lipoprotein, cholesterol, total triglycerides, creatinine, uric acid, alkaline phosphatase, phosphorous, calcium, and fasting blood-glucose at baseline were measured in the central laboratory of Beijing Anzhen Hospital.
2.3. Detection of IL-37, OPG and CRP levels by ELISA
The concentrations of plasma IL-37, OPG, and hs-CRP were measured by an enzyme-linked immunosorbent assay (ELISA) according to instructions provided by the manufacturers (IL-37: Adipogen AG, Liestal, Switzerland; OPG: MBL, Nagoya, Japan; and hs-CRP: Siemens Healthcare, Tarrytown, New York). All samples were measured in duplicate.
2.4. CAC assessment
All patients were in normal sinus rhythm and were capable of a breath hold that was sufficient for computed tomographic angiography (CTA). Coronary calcium lesions were measured, and the total Agatston score (CAC score) was determined by summing the individual lesion scores from each of the four main coronary arteries (left main, left anterior descending, circumflex and right).[13] We used the classification system proposed by Rumberger, et al.[14] We initially classified the participants into four groups according to CAC scores: a score < 10 (Agatston unit, AU) denotes an absence of CAC, a score of 11–100 AU denotes mild CAC, a score of 101–400 denotes moderate CAC, and a score of > 400 AU denotes severe CAC. For further analysis, the study cohort was divided into two groups based on calcium scores: the severe (> 400 AU) and non-severe (< 400 AU) CAC patient groups.
2.5. Statistical analysis
All data were presented as mean ± SD. When comparing only two groups, Student's t-test was used. For comparisons involving three or more groups, one-way ANOVA followed by Neuman-Keuls post hoc test was used. Pearson Chi-Square test (exact Fisher's test) was used for the comparison of proportions. Spearman's correlation and binary logistic regression analysis were used to calculate the correlations between the plasma biomarker levels, other measured parameters and the level of CAC. In all tests, a value of P < 0.05 was considered to be statistically significant. The SPSS statistical software (version 17.01) was used for all calculations.
3. Results
3.1. Baseline characteristics of the study participants
Two hundred patients were enrolled in this study, and based on the severity of their CAC as determined by the Agatston scores, we divided the participants into four groups with fifty in each group, as described in the Methods section. Table 1 shows the blood sample characteristics of participants in the four groups. We found that patients with higher CAC scores were more likely to be elderly. Within the atherogenic risk factors, diabetes and hypertension were related to higher CAC score, while other factors such as hyperlipidaemia, smoking, family history of cardiovascular disease were not. We also found that participants who had a greater number of atherogenic risk factors were more likely to have higher CAC scores than those who had a lower number of risk factors (Table 1).
Table 1. Clinical characteristics of participants.
| Variables | CAC, AU |
P | |||
| < 10 (n = 50) | 11 to 100 (n = 50) | 101 to 400 (n = 50) | > 400 (n = 50) | ||
| Age, yrs | 57.52 ± 8.37 | 60.96 ± 8.76 | 62.56 ± 9.20 | 63.04 ± 10.54 | 0.0141 |
| Male sex, % | 52 | 68 | 64 | 76 | 0.086 |
| BMI, kg/m2 | 25.45 ± 3.53 | 26.08 ± 3.14 | 25.60 ± 3.06 | 25.53 ± 3.59 | 0.790 |
| Atherogenic risk factors | |||||
| Diabetes, % | 14 | 32 | 39 | 38 | 0.0232 |
| Hypertension, % | 42 | 56 | 68 | 66 | 0.0343 |
| Hyperlipidaemia, % | 42 | 50 | 46 | 56 | 0.543 |
| *Smoking, % | 28 | 40 | 42 | 46 | 0.286 |
| Family history | 16 | 20 | 24 | 20 | 0.801 |
| *Number of risk factors | 1.42 | 1.98 | 2.22 | 2.28 | < 0.0014 |
| Biochemical variables | |||||
| TC, mmol/L | 4.44 ± 1.04 | 4.71 ± 0.96 | 4.61 ± 1.04 | 4.64 ± 0.99 | 0.584 |
| HDL-C, mmol/L | 1.16 ± 0.29 | 1.04 ± 0.28 | 1.00 ± 0.19 | 1.05 ± 0.24 | 0.014 |
| LDL-C, mmol/L | 2.74 ± 0.79 | 3.11 ± 0.78 | 3.06 ± 0.99 | 2.98 ± 0.98 | 0.157 |
| TG, mmol/L | 1.75 ± 1.24 | 1.71 ± 1.10 | 1.88 ± 1.06 | 1.84 ± 1.24 | 0.875 |
| Creatinine, mmol/L | 68.5 ± 14.1 | 75.4 ± 19.2 | 77.2 ± 16.4 | 78.4 ± 19.6 | 0.23 |
| UA, mmol/L | 325.9 ± 83.7 | 335.8 ± 94.0 | 355.7 ± 68.1 | 329.48 ± 93.6 | 0.309 |
| ALP, mmol/L | 80.1 ± 21.8 | 82.9 ± 20.3 | 79.3 ± 19.0 | 84.8 ± 22.3 | 0.532 |
| Phosphorous, mmol/L | 1.24 ± 0.17 | 1.24 ± 0.21 | 1.18 ± 0.24 | 1.17 ± 0.20 | 0.126 |
| Calcium, mmol/L | 2.33 ± 0.12 | 2.31 ± 0.10 | 2.32 ± 0.13 | 2.29 ± 0.09 | 0.249 |
| FBG, mmol/L | 5.52 ± 1.24 | 6.46 ± 1.98 | 6.24 ± 1.99 | 6.72 ± 2.42 | 0.018 |
Data are expressed as the mean ± SD or %. *Including current and former smoking. 1Patients with higher CAC score were more likely to be elderly (P < 0.05); 2Diabetes and 3hypertension were associated with higher CAC scores (P < 0.05); 4A greater number of atherogenic risk factors correlated with higher CAC scores (P < 0.05). Higher FBG was associated with a higher CAC score (P < 0.05). AU: Agatston unit; ALP: alkaline phosphatase; CAC: coronary artery calcification; FBG: fasting blood glucose; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; TC: total cholesterol; TG: total triglycerides; UA: uric acid.
Moreover, participants with higher CAC scores tended to have higher fasting blood-glucose but lower high-density lipoprotein cholesterol levels (Table 1). However, there were no significant differences in gender (P = 0.086), body mass index and levels of other general serum biochemical parameters, including total cholesterol, low-density lipoprotein cholesterol, total triglycerides, creatinine, uric acid, alkaline phosphatase, phosphorous and calcium, among these four groups.
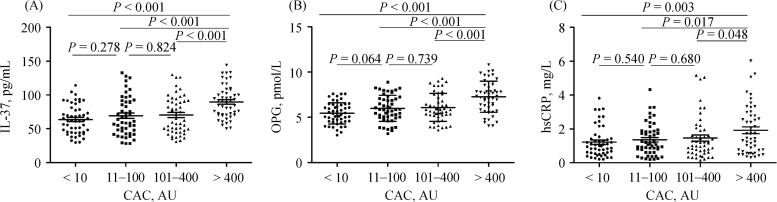
3.2. Plasma levels of IL-37, OPG and hs-CRP
As shown in Table 2 and Figure 1A, our data showed that there were no apparent differences in plasma IL-37 levels among patients in the first three groups (without CAC and with mild and moderate CAC). However, plasma IL-37 levels were significantly increased in patients with severe CAC (CAC scores > 400 AU, P < 0.001, Figure 1A). Interestingly, similar results were obtained for plasma OPG and hs-CRP (Table 2, and Figure 1B and 1C, respectively); OPG and hs-CRP levels were increased only in patients with severe CAC, and there were no apparent differences in OPG and hs-CRP levels among patients with or without mild or moderate CAC.
Table 2. Plasma IL-37, OPG and hs-CRP stratified by groups of patients with four levels of CAC and traditional risk factors.
| n | IL-37 | OPG | hs-CRP | |
| CAC, AU | ||||
| < 10 | 50 | 63.65 ± 21.45* | 5.44 ± 1.18* | 1.22 ± 0.90* |
| 11–100 | 50 | 69.18 ± 28.46* | 5.99 ± 1.45* | 1.37 ± 0.95* |
| 101–400 | 50 | 70.31 ± 27.40* | 6.09 ± 1.54* | 1.46 ± 1.25* |
| > 400 | 50 | 89.67 ± 23.84* | 7.27 ± 1.72* | 1.92 ± 1.44* |
| Male | 130 | 75.34 ± 27.64 | 6.39 ± 1.71 | 1.49 ± 1.21 |
| Female | 70 | 69.23 ± 25.80 | 5.86 ± 1.37 | 1.50 ± 1.11 |
| Diabetes | 62 | 75.68 ± 25.96 | 6.36 ± 1.71 | 1.52 ± 1.05 |
| Non-diabetes | 138 | 72.09 ± 27.63 | 6.13 ± 1.58 | 1.48 ± 1.23 |
| Hypertension | 116 | 74.79 ± 26.51 | 6.28 ± 1.67 | 1.62 ± 1.23 |
| Normotension | 84 | 71.02 ± 27.91 | 6.08 ± 1.55 | 1.32 ± 1.08 |
| Smoking | 79 | 74.81 ± 27.40 | 6.36 ± 1.73 | 1.51 ± 1.15 |
| Non-smoking | 121 | 72.16 ± 26.98 | 6.09 ± 1.54 | 1.48 ± 1.20 |
Data are presented as mean ± SD. *P < 0.05 among the four groups. There were no apparent differences in IL-37, OPG and hs-CRP levels among patients in the first three groups (without CAC, and with mild and moderate CAC). The main difference was between severe CAC and the other groups. AU: Agatston unit; CAC: coronary artery calcification; hs-CRP: high-sensitivity C-reactive protein; IL: interleukin; OPG: osteoprotegerin.
Figure 1. One-way ANOVA analysis of IL-37, OPG and hs-CRP levels according to CAC scores.
A score < 10: absence of CAC; 11–100 AU: mild CAC; 101–400 AU: moderate CAC; and > 400 AU: severe CAC. There were no apparent differences in IL-37, OPG and hs-CRP levels among patients in the first three groups (without CAC, with mild and moderate CAC). The main difference was between severe CAC and the other groups. AU: Agatston unit; CAC: coronary artery calcification; hs-CRP: high-sensitivity C-reactive protein; IL: interleukin; OPG: osteoprotegerin.
Based on these results, for the purpose of further statistical analysis, participants were regrouped into two categories: the severe calcification (CAC scores > 400 AU, n = 50) and non-severe calcification (CAC scores ≤ 400 AU, n = 150) groups. Based on the new grouping, Spearman's correlation and binary logistic regression analysis were carried out and revealed a significant positive correlation between IL–37 and severe CAC (r = 0.360, P < 0.001, OR = 1.033, Table 3). Moreover, we found a significant positive correlation between OPG and severe CAC (r = 0.355, P < 0.001, OR = 1.805, Table 3) as well. A similar relationship was observed between hs-CRP and severe CAC (r = 0.168, P < 0.001, OR = 1.465, Table 3). In addition, we also found that the number of risk factors was positively correlated with severe CAC (r = 0.141, P < 0.001, Table 3). However, there were no significant differences in the plasma levels of IL-37, OPG and hs-CRP when considering gender or the risk factors for diabetes, hypertension, and smoking (Table 2).
Table 3. Analysis of distinct biomarkers, traditional risk factors and severe CAC levels.
| Variables | Spearman's correlation coefficient (r) | Binary logistic regression analysis, OR (95% CI) |
| Age | 0.133 | |
| Male sex | 0.133 | |
| Diabetes | 0.087 | |
| Hypertension | 0.094 | |
| Number of risk factors | 0.141* | |
| HDL, mmol/L | −0.017 | |
| FBG, mmol/L | 0.094 | |
| IL-37 | 0.360* | 1.033 (1.019−1.047) |
| OPG | 0.355* | 1.805 (1.432−2.276) |
| hs-CRP | 0.168* | 1.465 (1.128−1.902) |
*P < 0.05. There is a significant positive correlation between the number of risk factors and severe CAC (P < 0.001); between IL–37 and severe CAC (P < 0.001); between OPG and severe CAC (P < 0.001); and between hs-CRP and severe CAC (P < 0.001). CAC: coronary artery calcification; FBG: fasting blood glucose; HDL: high-density lipoprotein; hs-CRP: high-sensitivity C-reactive protein; IL: interleukin; OPG: osteoprotegerin.
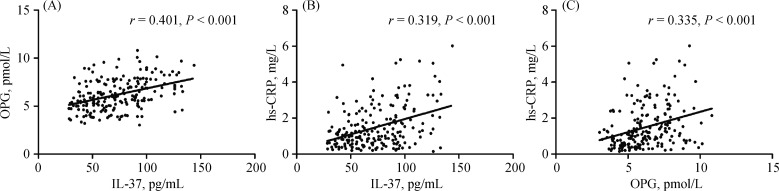
3.3. Associations among IL-37, OPG and hs-CRP
We used the Spearman's linear correlation coefficient to determine the relationship among the levels of these three plasma biomarkers. A positive correlation between IL-37 and OPG was determined (r = 0.401, P < 0.001, Figure 2A). The result further confirmed that the effect of IL-37 is closely related with the increase of OPG, which was observed in our recent animal study.[18] There was also a positive relationship between IL-37 and hs-CRP (r = 0.319, P < 0.001, Figure 2B) and between OPG and hs-CRP (r = 0.335, P < 0.001, Figure 2C) in the participating patients.
Figure 2. Correlation analysis plot.
(A): IL-37 and OPG; (B): IL-37 and hs-CRP; and (C) OPG and hs-CRP. There was a positive relationship between IL-37 and OPG (r = 0.401, P < 0.001), between IL-37 and hs-CRP (r = 0.319, P < 0.001), and between OPG and hs-CRP (r = 0.335, P < 0.001). hs-CRP: high-sensitivity C-reactive protein; IL: interleukin; OPG: osteoprotegerin.
4. Discussion
This is the first study to assess the relationship between the plasma IL-37 level in patients and the degree of CAC. In our study, no apparent difference in IL-37 levels was found in plasma among patients in the first three groups (with or without mild or moderate CAC). A significant increase in IL-37 level was observed only in the severe CAC group. For statistical analysis, the patients were regrouped, and a significant positive correlation between IL-37 and severe CAC was revealed. We also showed that the levels of plasma OPG and hs-CRP were increased in patients with severe CAC, and both were positively correlated with the level of IL-37. Although the sample size was relatively small and the implications are not yet clear, these interesting results may suggest that the elevated IL-37 expression could be the outcome of the activation of inflammation and may be related to the increase of OPG as shown in our recent animal study.[11]
Our study used CAC scores to assess the calcium content in the coronary arteries. Some studies have verified that CAC scores can be used to predict cardiac events.[15] We can speculate that the levels of plasma IL-37 might be associated with the risk of cardiac events. IL-37 is present in several organs and tissues, including the heart, brain, kidney, bone marrow and testis. Evidence has shown that IL-37 plays a protective role in inflammatory and autoimmune diseases in animal models via the suppression of pro-inflammatory cytokine generation and the activation of macrophage and dendritic cells.[10] Recently, Boraschi, et al.,[9] found that IL-37 was expressed in the foam-like cells of the atherosclerotic coronary and carotid artery plaques, suggesting that IL-37 is related to the process of atherosclerosis.[16] Recently, our study has shown that IL-37 can attenuate not only atherosclerosis but also vascular calcification in mice.[11] Although all of these studies point to the involvement of IL-37 in human atherosclerotic disease, the understanding of IL-37 in the disease process is rather limited. IL-37 is expressed at low levels in peripheral blood mononuclear cells (PBMCs) and dendritic cells (DCs) and is up-regulated in an inducible manner. After treatment with phorbol myristoyl acetate, the mRNA expression of IL-37 was increased 2-fold in PBMCs and 4.5-fold in DCs.[17] In addition, IL-37 is induced mainly in an inflammatory context. IL-1β, IL-18, TNF-α, IFN-γ, and TGF-β can increase IL-37 synthesis.[18] Recently, we have demonstrated that the levels of the anti-inflammatory cytokine IL-37 were dramatically increased in ACS patients,[12] which may be due to an excessive inflammatory response. In the present study, we found that the level of IL-37 was positively correlated with high CAC levels, suggesting that IL-37 expression may be caused by the activation of inflammation. We also found that the levels of IL-37 were positively correlated with OPG and hs-CRP. Therefore, we concluded that IL-37 is expressed in low levels in healthy persons but may be regulated by inflammatory stimuli and cytokines such as OPG and hs-CRP.
OPG is a soluble member of the TNF receptor superfamily.[19],[20] Elevated serum OPG levels have been shown to be independently associated with prevalent coronary plaques, aortic plaques, CAC and peripheral vascular disease,[21],[22] as well as the increased risk of cardiovascular events.[23],[24] Although a clear association between higher circulating OPG levels and vascular disease has been observed, whether this is the cause or the outcome remains to be defined. However, the evidence from animal models suggests that OPG may be protective against vascular calcification.[11],[25] It is therefore possible that the OPG elevation observed in humans with vascular disease may have occurred, in part, due to a local compensatory response to atherosclerosis. Our recent work demonstrated a significant increase of plasma OPG levels in IL-37 treated mice.[11] When an anti-OPG antibody was administered, the protective effect of IL-37 in mice with vascular calcification was significantly reduced. In the present study, the plasma OPG level was apparently increased in patients with severe CAC and was positively related with IL-37. These results suggest that OPG could become a predictor of the presence and severity of CAC. Moreover, the levels of circulating OPG may also affect IL-37 expression.
We additionally assessed the hs-CRP levels in plasma and found that hs-CRP was increased in patients with high levels of CAC. CRP is associated with CHD, which was reported over 60 years ago.[26] The possible mechanistic role of CRP in plaque deposition is highly complex, exerting pro-atherogenic effects in many cells that are involved in atherosclerosis.[27] The Multi-Ethnic Study of Atherosclerosis showed a weak association of the three inflammatory biomarkers (CRP, IL-6, and fibrinogen) with CAC presence and burden,[28] which is in line with the present study. We found that hs-CRP, which is more sensitive than CRP, was positively correlated with plasma IL-37 levels, confirming the possible relationship between IL-37 expression and inflammatory stimuli.
In conclusion, in the present study, we showed for the first time that the plasma level of IL-37 was increased in patients with high coronary calcium levels. This may be associated with the activation of inflammation and other relevant factors such as OPG or hs-CRP. Recent reports have indicated that IL-37 uses IL-1R8 for its anti-inflammatory properties,[29] and that IL-37 inhibits NF-kB activation while increasing the anti-inflammatory IL-10 level.[30] Although a clear association among the three cytokines (IL-37, OPG and hs-CRP) and CAC has been observed in the present study, the mechanism remains to be defined and requires further investigation. However, it is reasonable to hypothesize that IL-37 might become a predictor of severe calcification in future, which requires further investigation.
Acknowledgments
This work was supported by the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZYLX201303), the National Key Clinical Speciality Construction Project (2013–2014), and the “Beijing Municipal Administration of Hospitals” Ascent Plan (DFL20150601). The authors declare that there are no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
- 1.Budoff MJ, Hokanson JE, Nasir K, et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging. 2010;3:1229–1236. doi: 10.1016/j.jcmg.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 2.Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 3.Keelan PC, Bielak LF, Ashai K, et al. Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation. 2001;104:412–417. doi: 10.1161/hc2901.093112. [DOI] [PubMed] [Google Scholar]
- 4.Johnson RC, Leopold JA, Loscalzo J. Vascular calcification pathobiological mechanisms and clinical implications. Circ Res. 2006;99:1044–1059. doi: 10.1161/01.RES.0000249379.55535.21. [DOI] [PubMed] [Google Scholar]
- 5.Abdelbaky A, Corsini E, Figueroa AL, et al. Focal arterial inflammation precedes subsequent calcification in the same location a longitudinal FDG-PET/CT Study. Circ Cardiovasc Imaging. 2013;6:747–754. doi: 10.1161/CIRCIMAGING.113.000382. [DOI] [PubMed] [Google Scholar]
- 6.Li H, Hong S, Zheng Y, et al. Cross talk between the bone and immune systems: osteoclasts function as antigen-presenting cells and activate CD4+ and CD8+ T cells. Blood. 2010;116:210–217. doi: 10.1182/blood-2009-11-255026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takaoka M, Nagata D, Kihara S, et al. Periadventitial adipose tissue plays a critical role in vascular remodeling. Circ Res. 2009;105:906–911. doi: 10.1161/CIRCRESAHA.109.199653. [DOI] [PubMed] [Google Scholar]
- 8.Shroff RC, McNair R, Figg N, et al. Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation. 2008;118:1748–1757. doi: 10.1161/CIRCULATIONAHA.108.783738. [DOI] [PubMed] [Google Scholar]
- 9.Boraschi D, Lucchesi D, Hainzl S, et al. IL-37: a new anti-inflammatory cytokine of the IL-1 family. Eur Cytokine Netw. 2011;22:127–147. doi: 10.1684/ecn.2011.0288. [DOI] [PubMed] [Google Scholar]
- 10.Nold MF, Nold-Petry CA, Zepp JA, et al. IL-37 is a fundamental inhibitor of innate immunity. Nat Immunol. 2010;11:1014–1022. doi: 10.1038/ni.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chai M, Ji Q, Zhang H, et al. The protective effect of interleukin-37 on vascular calcification and atherosclerosis in apolipoprotein E-deficient mice of diabetes. J Interferon Cytokine Res. 2015;35:530–539. doi: 10.1089/jir.2014.0212. [DOI] [PubMed] [Google Scholar]
- 12.Ji Q, Zeng Q, Huang Y, et al. Elevated plasma IL-37, IL-18, and IL-18BP concentrations in patients with acute coronary syndrome. Mediators Inflamm. 2014;2014:165742. doi: 10.1155/2014/165742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 14.Rumberger JA, Brundage BH, Rader DJ, et al. Electron beam computed tomographic coronary calcium scanning: a review and guidelines for use in asymptomatic persons. Mayo Clin Proc. 1999;74:243–252. doi: 10.4065/74.3.243. [DOI] [PubMed] [Google Scholar]
- 15.Church TS, Levine BD, McGuire DK, et al. Coronary artery calcium score, risk factors, and incident coronary heart disease events. Atherosclerosis. 2007;190:224–231. doi: 10.1016/j.atherosclerosis.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Boyle JJ. Macrophage activation in atherosclerosis: pathogenesis and pharmacology of plaque rupture. Curr Vasc Pharmacol. 2005;3:63–68. doi: 10.2174/1570161052773861. [DOI] [PubMed] [Google Scholar]
- 17.Pan G, Risser P, Mao W, et al. IL-1H, an interleukin 1-related protein that binds IL-18 receptor/IL-1Rrp. Cytokine. 2001;13:1–7. doi: 10.1006/cyto.2000.0799. [DOI] [PubMed] [Google Scholar]
- 18.Nold MF, Nold-Petry CA, Zepp JA, et al. IL-37 is a fundamental inhibitor of innate immunity. Nat Immunol. 2010;11:1014–1022. doi: 10.1038/ni.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collin-Osdoby P. Regulation of vascular calcification by osteoclast regulatory factors RANKL and osteoprotegerin. Circ Res. 2004;95:1046–1057. doi: 10.1161/01.RES.0000149165.99974.12. [DOI] [PubMed] [Google Scholar]
- 20.Schoppet M, Preissner KT, Hofbauer LC. RANK ligand and osteoprotegerin: paracrine regulators of bone metabolism and vascular function. Arterioscler Thromb Vasc Biol. 2002;22:549–553. doi: 10.1161/01.atv.0000012303.37971.da. [DOI] [PubMed] [Google Scholar]
- 21.Jono S, Ikari Y, Shioi A, et al. Serum osteoprotegerin levels are associated with presence and severity of coronary artery disease. Circulation. 2002;106:1192–1194. doi: 10.1161/01.cir.0000031524.49139.29. [DOI] [PubMed] [Google Scholar]
- 22.Abedin M, Omland T, Ueland T, et al. Relation of osteoprotegerin to coronary calcium and aortic plaque (from the Dallas Heart Study) Am J Cardiol. 2007;99:513–518. doi: 10.1016/j.amjcard.2006.08.064. [DOI] [PubMed] [Google Scholar]
- 23.Ueland T, Jemtland R, Godang K, et al. Prognostic value of osteoprotegerin in heart failure after acute myocardial infarction. J Am Coll Cardiol. 2004;44:1970–1976. doi: 10.1016/j.jacc.2004.06.076. [DOI] [PubMed] [Google Scholar]
- 24.Kiechl S, Schett G, Wenning G, et al. Osteoprotegerin is a risk factor for progressive atherosclerosis and cardiovascular disease. Circulation. 2004;109:2175–2180. doi: 10.1161/01.CIR.0000127957.43874.BB. [DOI] [PubMed] [Google Scholar]
- 25.Bucay N, Sarosi I, Dunstan CR, et al. Osteoprotegerin-deficient mice develop early-onset osteoporosis and arterial calcification. Genes Dev. 1998;12:1260–1268. doi: 10.1101/gad.12.9.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuller LH, Tracy RP, Shaten J, et al. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996;144:537–547. doi: 10.1093/oxfordjournals.aje.a008963. [DOI] [PubMed] [Google Scholar]
- 27.Zhang YX, Cliff WJ, Schoefl GI, et al. Coronary C-reactive protein distribution: its relation to development of atherosclerosis. Atherosclerosis. 1999;145:375–379. doi: 10.1016/s0021-9150(99)00105-7. [DOI] [PubMed] [Google Scholar]
- 28.Jenny NS, Brown ER, Detrano R, et al. Associations of inflammatory markers with coronary artery calcification: results from the multi-ethnic study of atherosclerosis. Atherosclerosis. 2010;209:226–229. doi: 10.1016/j.atherosclerosis.2009.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li S, Neff CP, Barber K, et al. Extracellular forms of IL-37 inhibit innate inflammation in vitro and in vivo but require the IL-1 family decoy receptor IL-1R8. Proc Natl Acad Sci USA. 2015;112:2497–2502. doi: 10.1073/pnas.1424626112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu B, Meng K, Ji Q, et al. Interleukin-37 ameliorates myocardial ischaemia/reperfusion injury in mice. Clin Exp Immunol. 2014;176:438–451. doi: 10.1111/cei.12284. [DOI] [PMC free article] [PubMed] [Google Scholar]