Abstract
Rationale: Extracorporeal life support (ECLS) for acute respiratory failure has increased as a result of technological advancements and promising results from recent studies as compared with historical trials.
Objectives: Systematically review the effect of ECLS compared with mechanical ventilation on mortality, length of stay, and adverse events in respiratory failure.
Methods: Data sources included were MEDLINE, EMBASE, and CENTRAL (through to October 2013). Any randomized controlled trial (RCT) or observational study comparing ECLS to mechanical ventilation in adults was used. Two authors independently abstracted the data. Our primary outcome was mortality. Secondary outcomes included intensive care unit length of stay, hospital length of stay, and adverse events. A sensitivity analysis was performed restricted to RCTs and quasi-RCTs, and a number of predefined subgroups were identified to explore heterogeneity.
Measurements and Main Results: Ten studies (four RCTs, six observational studies, 1,248 patients) were included. There was no significant difference in hospital mortality with ECLS as compared with mechanical ventilation (risk ratio [RR], 1.02; 95% confidence interval [CI], 0.79–1.33; I2 = 77%). When restricted to venovenous ECLS studies of randomized trials and quasi-randomized trials (three studies; 504 patients), there was a decrease in mortality with ECLS compared with mechanical ventilation (RR, 0.64; 95% CI, 0.51–0.79; I2 = 15%). There were insufficient study-level data to evaluate most secondary outcomes. Bleeding was significantly greater in the ECLS group (RR, 11.44; 95% CI, 3.11–42.06; I2 = 0%). In the H1N1 subgroup (three studies; 364 patients), ECLS was associated with significantly lower hospital mortality (RR, 0.62; 95% CI, 0.45–0.8; I2 = 25%).
Conclusions: ECLS was not associated with a mortality benefit in patients with acute respiratory failure. However, a significant mortality benefit was seen when restricted to higher-quality studies of venovenous ECLS. Patients with H1N1–acute respiratory distress syndrome represent a subgroup that may benefit from ECLS. Future studies are needed to confirm the efficacy of ECLS as well as the optimal configuration, indications, and timing for adult patients with respiratory failure.
Keywords: critical care, extracorporeal life support, intensive care units, respiratory distress syndrome, adult, systematic review
Acute respiratory failure (ARF) is a common reason for admission to an intensive care unit (ICU) and the need for mechanical ventilation. Acute respiratory distress syndrome (ARDS) is a severe form of hypoxemic ARF, with bilateral infiltrates consistent with pulmonary edema on chest radiography that is not primarily due to a cardiogenic etiology (1). Mortality from ARDS is high (30–40%), with most deaths resulting from multiorgan failure and sepsis (1). Limited pharmacologic therapy has proven effective in ARDS; however, management is focused primarily on supportive care with mechanical ventilation (2, 3). Currently, lung-protective pressure- and volume-limited ventilatory strategies aimed at mitigating ventilator-associated lung injury have become the standard of care (2). Clinical trials evaluating the use of higher positive end-expiratory pressure, recruitment maneuvers, high-frequency oscillatory ventilation, and prone positioning to further optimize lung protection in patients with ARDS have yielded variable results (4–11).
Despite the use of lung-protective ventilation, a number of patients with ARDS may develop refractory hypoxemia and/or hypercapnia or may not be able to achieve adequate gas exchange without using injurious levels of ventilatory support. Extracorporeal life support (ECLS) provides an alternative means of supporting patients with severe ARDS by alleviating the need for high airway pressures and allowing lung “rest” with “ultra”–lung-protective ventilation (e.g., tidal volumes < 4 ml/kg predicted body weight). During the H1N1 pandemic, a surge in ECLS use in highly selected patients yielded promising results, leading to a resurgence of interest in its use for severe ARDS. The recently completed Conventional ventilatory support versus Extracorporeal membrane oxygenation for Severe Adult Respiratory failure (CESAR) trial and a systematic review of ECLS for the H1N1 cohort further strengthened its potential role as rescue therapy in ARDS (12, 13). However, poor outcomes from historical trials and conflicting results from recent reports have tempered the recent enthusiasm for its use and have reestablished clinical equipoise for ECLS in patients with ARDS (14, 15).
Given the limited number of patients enrolled in previous studies, conflicting results, and the recent improvements in ECLS technology, indications, and associated complications, we performed a systematic review and metaanalysis of studies comparing ECLS to mechanical ventilation in patients with ARF.
Methods
Search Strategy
We electronically searched MEDLINE, EMBASE, and CENTRAL (from inception to October 1, 2013) to identify randomized controlled trials (RCTs) and observational studies of ECLS compared with mechanical ventilation for ARF. Our search combined Medical Subject Headings (or appropriate controlled vocabulary) and keywords for extracorporeal life support and ARF (see Figure E1 in the online supplement). There were no language or date restrictions applied.
Study Selection
Two reviewers (L.M. and T.T.) independently reviewed all studies for inclusion, extracted potentially relevant studies, and determined study eligibility. Full texts were retrieved and reviewed for both definite and potentially eligible studies (L.M., T.T., A.W.). Any disagreements were resolved by overall group consensus (L.M., T.T., A.W., E.F.). We included studies that: enrolled patients with ARF older than 1 month of age (population), received ECLS (intervention), were compared with patients receiving mechanical ventilation (comparison), and reported mortality as an outcome.
Data Extraction and Study Quality
A custom-designed, Excel spreadsheet (Microsoft Corporation, Redmond, WA) was used to store independently abstracted (L.M. and T.T.) data on study design, patient characteristics, ECLS configuration, indication and timing, details on ventilation, and study outcomes. Disagreements were resolved by group consensus. All studies were assessed for evidence of bias using the Cochrane Collaboration risk of bias instrument including assessment for random sequence generation, allocation concealment, blinding of personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting. We assessed study quality using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) assessment, including evidence of outcomes and adverse events (16, 17).
Outcomes
Our primary outcome of interest was hospital mortality. In the event that it was not provided, we used ICU mortality. Secondary outcomes included mortality at other time points (i.e., 6 months) and ICU and hospital length of stay (LOS). Adverse events included the incidence of major bleeding (e.g., hemorrhagic shock, major gastrointestinal bleeding, intracerebral hemorrhage), barotrauma, sepsis, and ECLS-associated complications (e.g., limb ischemia, circuit clot, air embolism).
Statistical Analysis
Dichotomous outcomes were reported using risk ratios (RR) and their 95% confidence intervals (CIs). For continuous outcomes, the standardized difference in means was evaluated. Heterogeneity among studies was determined by calculating the I2 statistic, with high heterogeneity being classified as greater than 75%, moderate between 50 and 74%, and low less than 25%. Study-level data were pooled using a random-effects model; in the presence of low heterogeneity (I2 < 25%), a fixed-effects model was used for a more precise estimate of effect. To assess reporting bias, we examined funnel plots of treatment effect versus study precision. We assumed a more liberal level of statistical significance to indicate possible publication bias (P < 0.10) given the low statistical power of these tests. All statistical analyses were performed using RevMan 5.2 (Cochrane Collaboration, Oxford, UK).
Sensitivity and Subgroup Analysis
We conducted a sensitivity analysis, restricted to studies with good methodological quality (i.e., RCTs and quasi-RCTs). A quasi-RCT was determined to be any observational study that performed a matched cohort analysis using propensity scores (18). We decided a priori to repeat the sensitivity analysis using studies evaluating venovenous exctracorporeal membrane oxygenation (ECMO) only, studies in which lung-protective ventilation was adopted in the ECLS and control arms, and studies using different matching strategies to determine the control cohort.
Subgroup analysis performed on all studies defined a priori included: younger adult age (18–40 yr), studies using lung-protective ventilation, etiology of ARF (patients with H1N1-associated ARDS, studies in which > 50% of the cases of ARDS were due to pneumonia), early initiation of ECLS (within 7 d of ARDS onset), severity of ARDS (i.e., PaO2/FiO2 < 50), and predominant use of venovenous ECMO.
Results
Literature Search
The electronic database search retrieved 2,145 citations, of which 131 full texts were retrieved for further adjudication (Figure E2). Ten studies fulfilled the inclusion criteria, including four RCTs (19–22) and six observational studies (14, 23–27). No pediatric trials met the inclusion criteria, and, therefore, only adult patients were included in all analyses. There was near-perfect agreement on study inclusion (kappa statistic = 1.00) of the observational studies; two were propensity score–matched cohort studies and were considered quasi-RCT for the purposes of analysis (14, 23). There was no evidence of significant publication bias (Figure E3).
Study Characteristics and Methodological Quality
In the 10 included studies (1,248 patients), 496 patients received ECLS (Table 1). There was substantial qualitative heterogeneity among the trials. The studies used a combination of venoarterial ECMO, venovenous ECMO, and extracorporeal CO2 removal (ECCO2R) with a predominance of venovenous ECMO for ARF in the more recent trials. Three studies (364 patients) were composed primarily of H1N1-associated ARDS. The number of days before initiation of ECLS was variable (range, 0.5–13 d), with more recent studies initiating ECLS earlier. Protocolized ventilation for the ECLS arms was outlined in eight studies, and protocolized management in the control arms was present in seven studies. Adherence to a lung-protective ventilatory strategy in the control arms of studies after 2000 was not always maintained or reported (Table 1). Finally, mortality rates in the ECLS group were highly variable in the included studies (range, 24–90%), with the highest mortality rates reported in the earliest studies.
Table 1.
Baseline characteristics of patients and risk of bias
| Author (Study Design) | Total No. Patients (ECLS) | Average Age (yr) | ICU Type (country) | Days pre ECLS and Type | Severity of ARDS (P/F Ratio) in ECLS Group | Severity of ARDS (P/F Ratio) in Control Group | Cause of ARF | Lung-Protective Ventilation ECMO Arm | Lung-Protective Ventilation Control Arm | Risk of Bias* |
|---|---|---|---|---|---|---|---|---|---|---|
| Zapol 1979 (RCT) | 90 (42) | 42 | N/A (US) | 9.6, VA | 50/80† | 50/80† | Pneumonia, other | No | No | Low |
| Morris 1994 (RCT) | 40 (21) | 36 | N/A (US) | N/A, ECCO2R | 63 | 64 | Pneumonia, other | No‡ | No | Low |
| Lewandowski 1997 (Obs) | 122 (49) | 32 | Surgical (Germany) | 13, VV | 67 | 86 | Pneumonia, nonpulmonary sepsis, aspiration, polytrauma, other | N/A | Yes (PP) | High |
| Mols 2000 (Obs) | 245 (62) | 40 | Medical (Germany) | 10, VV | 96 | 126 | Pneumonia, nonpulmonary sepsis, aspiration, polytrauma, transfusion | Yes (PP) | Yes (PP) | High |
| Beiderlinden 2006 (Obs) | 150 (32) | 42 | Medical (Germany) | 5, VV | 63 | 100 | Pneumonia | Yes | N/A | High |
| Roch 2010 (Obs) | 18 (6) | 52 | Medical (France) | 0.5, VV (6), VA (3) | 52 | 96 | H1N1 | Yes | Yes | High |
| Peek 2009 (RCT) | 180 (90, 68§) | 40 | Medical (UK) | 1.5, VV | 76 | 75 | Pneumonia, polytrauma, other | Yes (PP) | Yes (PP) | Low |
| Noah 2011 (Obs) | 150 (75) | 37 | Medical, surgical, cardiovascular (UK) | 4, VV | 55 | 55 | H1N1 | Yes | N/A | Low |
| Pham 2013 (Obs) | 196 (98)∥ | 41 | Medical (France) | 2, VV (107), VA (16) | 62 | 62 | H1N1 | Yes | Yes | Low |
| Bein 2013 (RCT) | 79 (40) | 49 | Medical (Germany, Austria) | 1, ECCO2R | 152 | 168 | Pneumonia, sepsis, massive transfusion, trauma | Yes (3 ml/kg) | Yes | Low |
Definition of abbreviations: ARDS = acute respiratory distress syndrome; ARF = acute respiratory failure; ECCO2R = extracorporeal CO2 removal; ECLS = extracorporeal life support; ICU = intensive care unit; Obs = observational study; N/A = not available; P/F = PaO2/FiO2; PP = only plateau pressure limits outlined; RCT = randomized controlled trial; VA = venoarterial; VV = venovenous.
See online supplement.
P/F of 50 reflects criteria for early enrolment and P/F of 80 reflects criteria for late enrolment.
Low-frequency positive pressure ventilation strategy used.
Number of patients in ECLS group who actually received ECLS.
Using GenMatch Matching cohort.
The level of bias was analyzed using the Cochrane Collaboration risk of bias instrument (Table E1). The four RCTs (19–22) and two quasi-RCTs (14, 23) had an overall low risk of bias, whereas the observational studies tended to have sicker patients in the ECLS group, thus limiting the ability to compare the two modalities among a similar group of patients.
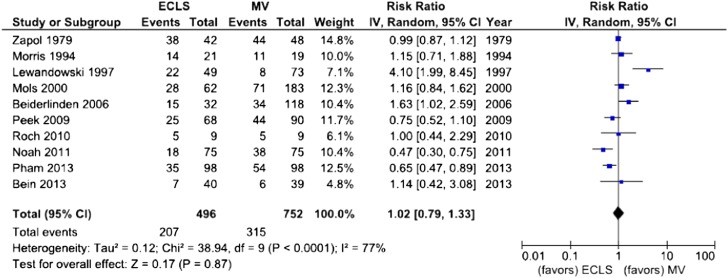
Hospital Mortality
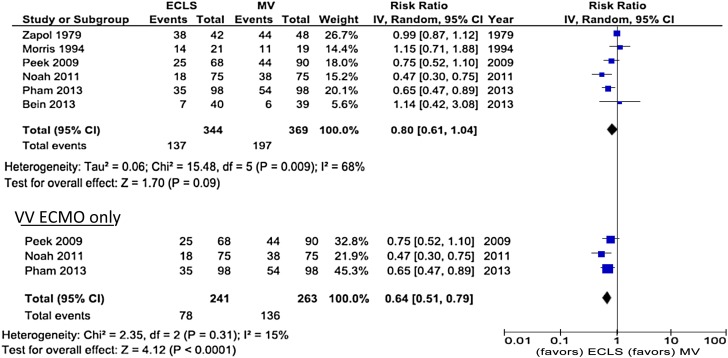
Hospital mortality was reported in 10 studies (1,248 patients, 496 ECLS), with a composite endpoint of in-hospital mortality and 6-month mortality (21) and ICU mortality (14) reported in two studies (Table 2) (12, 14). There was no difference in hospital mortality between ECLS and conventional mechanical ventilation (RR, 1.02; 95% CI, 0.79–1.33; I2 = 77%) (Figure 1). When restricted to RCTs and quasi-RCTs (713 patients, 344 ECLS), there was also no difference in mortality (RR, 0.80; 95% CI, 0.61–1.04; I2 = 68%); however, when analyzing the use of venovenous ECLS among the higher-quality studies (504 patients, 263 ECLS), mortality was significantly lower with ECLS (RR, 0.64; 95% CI, 0.51–0.79; I2 = 15%) (Figure 2). Moreover, the results of the sensitivity analysis were similar when limited to studies using lung-protective ventilation (four studies) (RR, 0.53; 95% CI, 0.53–0.80; I2 = 17%) (Figure E4A). We repeated the analysis using the per-protocol analysis and intention-to-treat analysis for the CESAR study, for which the results remained statistically significant. We chose to use GenMatch for the studies involving propensity score matching techniques, given that it reflected the most inclusive cohort of patients undergoing ECLS; however, when changed to the more conservative Réseau Européen de recherche en Ventilation Artificielle (REVA) matching technique for the Pham trial the results were not significant (RR, 0.90; 95% CI, 0.69–1.16; I2 = 61%) (Figure E4B) (14). The strength of the evidence is summarized in Table 2 using the GRADE assessment tool.
Table 2.
Summary of outcomes and Grading of Recommendations Assessment, Development, and Evaluation Evidence assessment
| Outcomes | No. of Studies | Total No. Included in Analysis | Evidence Assessment (GRADE) | RR (95% CI) | P Value |
|---|---|---|---|---|---|
| Primary outcome | |||||
| In-hospital mortality | 10* | 1,248 | Mod | 1.02 (0.79 to 1.33) | 0.87 |
| Secondary outcomes | |||||
| LOS ICU | 6† | 162 | Low | 8.65 (−9.72 to 27.01) | 0.36 |
| Sensitivity analysis | |||||
| In-hospital mortality RCT, quasi-RCT | 6 | 713 | Mod-High | 0.80 (0.61 to 1.04) | 0.09 |
| In-hospital mortality RCT, quasi-RCT VV ECLS | 3 | 504 | Mod-High | 0.64 (0.51 to 0.79) | <0.0001 |
| In-hospital mortality RCT, quasi-RCT REVA match Pham‡ | 6 | 621 | Mod-High | 0.90 (0.69 to 1.16) | 0.40 |
| In-hospital mortality RCT, quasi-RCT lung-protective ventilation‡ | 4 | 583 | Mod-High | 0.65 (0.53 to 0.80) | <0.0001 |
| Subgroup analysis, in-hospital mortality | |||||
| H1N1 | 3 | 364 | Mod-High | 0.62 (0.45 to 0.84) | 0.002 |
| Lung-protective ventilation | 6 | 773 | Mod-High | 0.82 (0.57 to 1.18) | 0.29 |
| >50% ARDS due to pneumonia | 8 | 1,069 | Mod | 0.91 (0.72 to 1.14) | 0.40 |
| Age < 40 yr | 5 | 737 | Mod | 1.08 (0.64 to 1.82) | 0.77 |
| ECLS within 1st wk | 6 | 773 | Mod | 0.82 (0.57 to 1.18) | 0.29 |
| Very severe ARDS (average PF < 50) | 2 | 168 | Mod | 0.63 (0.31 to 1.30) | 0.21 |
| VV ECMO | 7 | 1,061 | Mod | 1.03 (0.98 to 1.57) | 0.87 |
| Adverse events | |||||
| Adverse events: bleeding | 5 | 429 | Low-Mod | 11.44 (3.11 to 42.06) | 0.0002 |
| Adverse events: barotrauma | 2 | 162 | Mod | 1.46 (1.21 to 1.76) | < 0.0001 |
| Adverse events: sepsis | 3 | 333 | Low-Mod | 1.63 (0.82 to 3.26) | 0.16 |
Definition of abbreviations: ARDS = acute respiratory distress syndrome; CI = confidence interval; ECLS = extracorporeal life support; GRADE = Grading of Recommendations Assessment, Development, and Evaluation; ICU = intensive care unit; LOS = length of stay; PF = PaO2/FiO2; Mod = moderate; RCT = randomized controlled trial; REVA = Réseau Européen de recherche en Ventilation Artificielle; RR = risk ratio; VV = venovenous.
Peek included composite endpoint of in-hospital and <6-month mortality.
Only two studies had complete data including SDs to accurately combine in metaanalysis.
See online supplement.
Figure 1.
In-hospital mortality. Forest plot showing pooled analysis of four randomized controlled trials and six observational studies comparing extracorporeal life support (ECLS) to conventional mechanical ventilation (MV). In this analysis the GenMatch data were used for Pham and Noah and the per-protocol analysis was used for Peek (see Figure E1 for REVA matching for Pham). Using a random effects model: risk ratio, 1.02; 95% confidence interval (CI), 0.79–1.33; I2 = 77%; P = 0.87. Given the significant heterogeneity, refer to the sensitivity analysis performed (Figure 2).
Figure 2.
In-hospital mortality sensitivity analysis (randomized controlled trial, quasi-randomized controlled trial, and venovenous extracorporeal membrane oxygenation [VV ECMO] only). Forest plot showing pooled analysis of six higher-quality studies. In this analysis, the GenMatch data were used for Pham and Noah and the per-protocol analysis for Peek (see Figure E1 for REVA matching). Using a random effects model: risk ratio, 0.80; 95% confidence interval (CI), 0.61–1.04; I2 = 68%; P = 0.09. The analysis was then further limited to studies in which the predominant ECLS modality was VV ECMO. Using a fixed effects model: risk ratio, 0.64; 95% CI, 0.51–0.79; I2 = 15%; P < 0.0001.
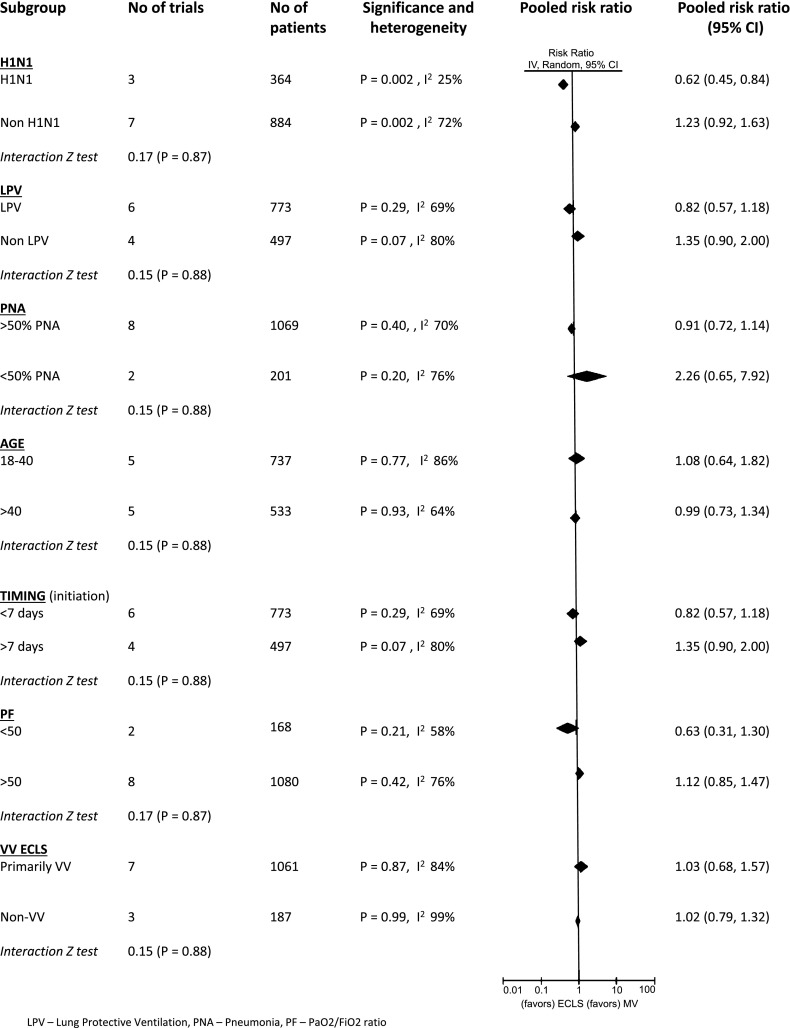
Subgroup Analysis
To explore the heterogeneity of in-hospital mortality among studies, we performed a number of predefined subgroup analyses (Figure 3). ECLS was associated with significantly lower mortality in patients with H1N1-associated ARDS (RR, 0.62; 95% CI, 0.45–0.8; I2 = 25%). There were no significant differences between ECLS and mechanical ventilation among the other subgroups examined.
Figure 3.
Subgroup analysis. Summary of the subgroups of interest and an assessment of interaction. The H1N1 subgroup demonstrated a significant mortality benefit from ECLS using a random effects model: risk ratio, 0.62; 95% confidence interval (CI), 0.45–0.84; I2 = 25%; P = 0.002. LPV = lung-protective ventilation; PF = PaO2/FiO2 ratio; PNA = pneumonia.
Secondary Outcomes
We intended to carry out an analysis of 6-month mortality, ICU and hospital LOS, and duration of mechanical ventilation. Unfortunately, study-level data were available only for a limited analysis of ICU length of stay. Although six studies (635 patients) reported on ICU length of stay, only three studies (202 patients) provided sufficient data for a pooled analysis. Patients on ECLS had a longer ICU length of stay, but this was not statistically significant (mean difference, 8.05; 95% CI, −2.45 to 18.54; I2 = 85%) (Figure E5)
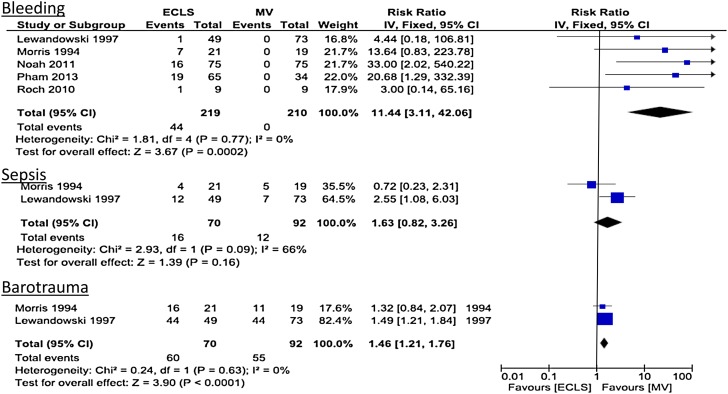
Adverse Events
We aimed to analyze the incidence of bleeding, barotrauma, sepsis and circuit-associated complications. Unfortunately, reporting and definitions of adverse events were often absent or, if present, heterogeneous among the studies (Figure 4). There were insufficient study-level data on circuit-associated complications to perform a pooled analysis. Regarding bleeding, the rates of bleeding were higher in the ECLS groups, with bleeding events seen in 21% of cases across five studies (RR, 11.44; 95% CI, 3.11–42.06; I2 = 0%). Life-threatening bleeding was reported in two studies only (Figure E4B) (RR, 2.78; 95% CI, 0.46–16.77; I2 = 0%). Limited data existed on the incidence of barotrauma, which was found to be higher in the ECLS group (RR, 1.46; 95% CI, 1.21–1.76; I2 = 0%). However, all of these studies that reported on this outcome were conducted in studies that did not use lung-protective ventilation. The incidence of sepsis was not different between the groups (RR, 1.63; 95% CI, 0.82–3.26; I2 = 66%).
Figure 4.
Adverse events. Pooled analysis using a fixed effects model for adverse events (bleeding, sepsis, and barotrauma). Of note, barotrauma reports were from studies before the lung-protective ventilation era. CI = confidence interval; ECLS = extracorporeal life support; MV = mechanical ventilation.
Discussion
Our systematic review and metaanalysis of 10 studies, including 1,248 patients, revealed no significant difference in in-hospital mortality in adult patients with ARF treated with ECLS. However, when limited to higher-quality studies involving venovenous ECLS, there was a significant reduction in in-hospital mortality with ECLS as compared with mechanical ventilation. Moreover, the subgroup of patients with H1N1-associated ARDS also derived a significant mortality benefit from ECLS. Few studies reported on longer-term mortality, length of stay, and adverse events associated with ECLS. Bleeding was found to be the major adverse event associated with ECLS. Interestingly, barotrauma was higher among the ECLS group; however, this was a limited assessment due to significant heterogeneity and before the lung-protective ventilation era.
Historic enthusiasm for ECLS was tempered in the early decades of its use due to a significant amount of bleeding, high incidence of circuit-associated complications, and poor patient outcomes. Small sample sizes and important limitations in study design (e.g., lack of randomization and selection bias of the sickest cohort undergoing ECLS in the early observational studies) have led to variable, and often disappointing, results. More recent trials have been characterized by earlier initiation in patients with severe, infectious-induced ARDS, with more advanced technology requiring less intense anticoagulation and fewer circuit-associated complications (28).
Five previous systematic reviews have evaluated ECLS in a descriptive fashion (13, 29–32). A recent review by Zangrillo and colleagues pooled ICU and hospital mortality from eight observational studies of ECLS use during H1N1 and estimated an overall in-hospital mortality of 28% (95% CI, 18–37%; I2 = 64%) (13) Zangrillo and colleagues more recently performed a review characterizing complications and outcome of all types of extracorporeal membrane oxygenation (with a predominance of venoarterial ECLS) and discovered a high incidence of renal failure, pneumonia, and sepsis (31). Zampieri and colleagues evaluated the use of ECLS for respiratory failure but limited their analysis to case-control studies and RCTs (32).
Our analysis was expanded to include observational studies, enabling us to perform a number of subgroup analyses in our evaluation (32). To our knowledge, our metaanalysis includes the largest cohort of the use of ECLS for patients with ARF to date evaluating hospital mortality for ECLS as compared with conventional mechanical ventilation. Furthermore, this is the first systematic review of primarily ECLS for respiratory failure that attempts to characterize adverse events. Unfortunately, the major limitation that existed was that there was a paucity of data on adverse events, and studies that included them lacked detailed definitions. However, recognition of this deficit can highlight the importance of prospectively characterizing and reporting these adverse events in future clinical trials.
The management of patients with severe ARDS has been hampered by a paucity of interventions leading to meaningful survival benefit (6, 11). Our inclusion of both observational studies and RCTs allowed for a more robust assessment of the potential impact of ECLS on ARF. Our sensitivity analysis, restricted to higher-quality studies, demonstrated a significant mortality benefit with the use of ECLS for severe ARDS compared with mechanical ventilation. Moreover, our study suggests ECLS may confer a survival benefit in younger patients with severe ARDS from a viral etiology (e.g., H1N1). Finally, our other predefined subgroups also suggest that patients with other infectious etiologies, early initiation of ECLS, and severe ARDS are other patient population for which ECLS merits future evaluation.
These results highlight the significant impact that ECLS may have on survival. If confirmed in a large RCT, ECLS would be one of the few interventions in ARDS that confers a mortality benefit (2, 3, 11). The ongoing, multicenter RCT, Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome (EOLIA; ClinicalTrials.gov NCT01470703) is investigating the use of venovenous ECMO for severe ARDS compared with conventional mechanical ventilation. This study will help further address the questions surrounding indications, timing of initiation, type of ARDS, and spectrum of adverse events associated with ECLS.
Another potential role of ECLS in the armamentarium for ARDS may be extracorporeal carbon dioxide removal (ECCO2R) (33, 34). In a post hoc analysis of a recent RCT comparing “ultra”–lung-protective ventilation (3 ml/kg predicted body weight) combined with ECCO2R, as compared with conventional lung-protective ventilation, was associated with increased ventilator-free days in the most severe cohort of patients with ARDS (22). The ability of ECCO2R to facilitate a further reduction in Vts is intriguing in light of recent data suggesting a dose–response of lower Vts with long-term mortality in patients with ARDS. The efficacy of ECCO2R in patients with ARDS requires confirmation in a rigorous clinical trial.
The results of our metaanalysis are heavily influenced by the CESAR trial, and important questions remain, including whether ECLS itself or transfer to an ECLS-capable center is the primary mechanism leading to the survival benefit seen in our sensitivity analysis (35, 36). Lack of protocolized ventilation in the control arm resulted in only 70% of patients receiving lung-protective ventilation (compared with 93% of the ECLS arm), and only 76% of the group referred for ECLS underwent treatment with ECLS. In an attempt to address the effect of being at a “center of excellence,” Noah and colleagues performed a sensitivity analysis only evaluating control patients from ECLS centers during which the results were upheld; however, this was a small number of patients (23). Furthermore, patients with H1N1-associated severe ARDS treated with conventional mechanical ventilation had comparable mortality to similar patients who were treated with ECLS (14, 23, 37). These deficiencies highlight the importance of the ongoing EOLIA study, in which the control arm will received protocolized ventilatory management of ARDS modeled on the “maximal pulmonary recruitment” group from the ExPRESS trial (38) using assist-controlled ventilatory mode, a Vt set at 6 ml/kg of ideal body weight, and positive end-expiratory pressure set to not exceed a plateau pressure of 28 to 30 cm H2O.
Our study has a number of important limitations. First, given temporal changes in critical care practice and ECLS technology, as well as differences in study inclusion criteria and design, we observed substantial heterogeneity in our results. However, our methodological approach was to incorporate the entire body of evidence (39) and perform a priori subgroup and sensitivity analyses to address heterogeneity. Results drawn from an extremely limited number studies do not allow for confidence in the consistency of the results. ECLS technology has changed over time. However, we were unable to identify a specific transition point to more “modern ECLS.” To address temporal changes in critical care and ECLS practices, we performed multiple subgroup and sensitivity analyses, including studies using venovenous ECLS and/or lung-protective ventilation strategies. Second, we included a number of observational studies, which may be more subject to bias than randomized trials. However, limiting our metaanalysis to the four available RCTs alone, two of which were conducted more than 20 years ago, may not reflect contemporary ECLS and critical care practices. Moreover, observational studies may be more likely to report data on adverse events, and the results of recent observational studies reported conflicting results, such that a pooled analysis was essential. We assessed the potential for bias from the observational studies and performed a number of sensitivity analyses restricted to studies with higher methodological quality.
Conclusions
ECLS was not associated with a mortality benefit in patients with ARF. However, a significant mortality benefit was seen when restricted to higher-quality studies of venovenous ECMO. Moreover, a potential benefit of ECLS was apparent in the subgroup of patients with H1N1. This study highlights the limited number of high-quality studies that currently exist evaluating the use of ECLS for respiratory failure and the significant heterogeneity that currently exists among the studies. Further studies are needed to confirm the efficacy of ECLS as well as the optimal configuration, indications, and timing. Results from the ongoing EOLIA trial may help to define the role ECLS in the therapeutic armamentarium for patients with severe ARDS.
Footnotes
Author Contributions: L.M. was involved in the study design, creation of search strategy, review of the search results and selection of relevant articles, data extraction, and statistical analysis, and was the primary author of the manuscript. T.T. was involved in the study design, creation of search strategy, review of the search results and selection of relevant articles, and data extraction and reviewed the manuscript in its draft forms and provided feedback on the final manuscript. A.W. was involved in an update of the search strategy and data collection. He reviewed and edited the manuscript. E.F. was involved in the conception and hypothesis of the research study. He supervised the study design and search strategy. He addressed any questions or conflicts that arose in study inclusion, and he supervised the statistical analysis and provided feedback on the creation of the manuscript.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 2.The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 3.Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 4.Fan E, Wilcox ME, Brower RG, Stewart TE, Mehta S, Lapinsky SE, Meade MO, Ferguson ND. Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med. 2008;178:1156–1163. doi: 10.1164/rccm.200802-335OC. [DOI] [PubMed] [Google Scholar]
- 5.Sud S, Sud M, Friedrich JO, Meade MO, Ferguson ND, Wunsch H, Adhikari NK. High frequency oscillation in patients with acute lung injury and acute respiratory distress syndrome (ARDS): systematic review and meta-analysis. BMJ. 2010;340:c2327. doi: 10.1136/bmj.c2327. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson ND, Slutsky AS, Meade MO. High-frequency oscillation for ARDS. N Engl J Med. 2013;368:2233–2234. doi: 10.1056/NEJMc1304344. [DOI] [PubMed] [Google Scholar]
- 7.Young D, Lamb SE, Shah S, MacKenzie I, Tunnicliffe W, Lall R, Rowan K, Cuthbertson BH. High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med. 2013;368:806–813. doi: 10.1056/NEJMoa1215716. [DOI] [PubMed] [Google Scholar]
- 8.Dasenbrook EC, Needham DM, Brower RG, Fan E. Higher PEEP in patients with acute lung injury: a systematic review and meta-analysis. Respir Care. 2011;56:568–575. doi: 10.4187/respcare.01011. [DOI] [PubMed] [Google Scholar]
- 9.Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865–873. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 10.Abroug F, Ouanes-Besbes L, Dachraoui F, Ouanes I, Brochard L. An updated study-level meta-analysis of randomised controlled trials on proning in ARDS and acute lung injury. Crit Care. 2011;15:R6. doi: 10.1186/cc9403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 12.Peek GJ, Moore HM, Moore N, Sosnowski AW, Firmin RK. Extracorporeal membrane oxygenation for adult respiratory failure. Chest. 1997;112:759–764. doi: 10.1378/chest.112.3.759. [DOI] [PubMed] [Google Scholar]
- 13.Zangrillo A, Biondi-Zoccai G, Landoni G, Frati G, Patroniti N, Pesenti A, Pappalardo F. Extracorporeal membrane oxygenation (ECMO) in patients with H1N1 influenza infection: a systematic review and meta-analysis including 8 studies and 266 patients receiving ECMO. Crit Care. 2013;17:R30. doi: 10.1186/cc12512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pham T, Combes A, Roze H, Chevret S, Mercat A, Roch A, Mourvillier B, Ara-Somohano C, Bastien O, Zogheib E, et al. Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med. 2013;187:276–285. doi: 10.1164/rccm.201205-0815OC. [DOI] [PubMed] [Google Scholar]
- 15.Cooper DJ, Hodgson CL. Extracorporeal membrane oxygenation rescue for H1N1 acute respiratory distress syndrome: equipoise regained. Am J Respir Crit Care Med. 2013;187:224–226. doi: 10.1164/rccm.201211-2052ED. [DOI] [PubMed] [Google Scholar]
- 16.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 17.Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, Alderson P, Glasziou P, Falck-Ytter Y, Schunemann HJ. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011;64:395–400. doi: 10.1016/j.jclinepi.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Harris AD, McGregor JC, Perencevich EN, Furuno JP, Zhu J, Peterson DE, Finkelstein J. The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inform Assoc. 2006;13:16–23. doi: 10.1197/jamia.M1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zapol WM, Snider MT, Hill JD. Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA. 1979;242:2193–2196. doi: 10.1001/jama.242.20.2193. [DOI] [PubMed] [Google Scholar]
- 20.Morris AH, Wallace CJ, Menlove RL, Clemmer TP, Orme JF, Jr, Weaver LK, Dean NC, Thomas F, East TD, Pace NL, et al. Randomized clinical trial of pressure-controlled inverse ratio ventilation and extracorporeal CO2 removal for adult respiratory distress syndrome. Am J Respir Crit Care Med. 1994;149:295–305. doi: 10.1164/ajrccm.149.2.8306022. [DOI] [PubMed] [Google Scholar]
- 21.Peek M, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, Hibbert CL, Truesdale A, Clemens F, Cooper N, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 22.Bein T, Weber-Carstens S, Goldmann A, Muller T, Staudinger T, Brederlau J, Muellenbach R, Dembinski R, Graf BM, Wewalka M, et al. Lower tidal volume strategy (3 ml/kg) combined with extracorporeal CO2 removal versus ‘conventional’ protective ventilation (6 ml/kg) in severe ARDS: The prospective randomized Xtravent-study. Intensive Care Med. 2013;39:847–856. doi: 10.1007/s00134-012-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, Sadique MZ, Sekhon JS, McAuley DF, Firmin RK, et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1) JAMA. 2011;306:1659–1668. doi: 10.1001/jama.2011.1471. [DOI] [PubMed] [Google Scholar]
- 24.Lewandowski K, Rossaint R, Pappert D, Gerlach H, Slama KJ, Weidemann H, Frey DJ, Hoffmann O, Keske U, Falke KJ. High survival rate in 122 ARDS patients managed according to a clinical algorithm including extracorporeal membrane oxygenation. Intensive Care Med. 1997;23:819–835. doi: 10.1007/s001340050418. [DOI] [PubMed] [Google Scholar]
- 25.Mols G, Loop T, Geiger K, Farthmann E. Benzing A. Extracorporeal membrane oxygenation: a ten-year experience. Am J Surg. 2000;180:144–154. doi: 10.1016/s0002-9610(00)00432-3. [DOI] [PubMed] [Google Scholar]
- 26.Beiderlinden M, Eikermann M, Boes T, Breitfeld C, Peters J. Treatment of severe acute respiratory distress syndrome: role of extracorporeal gas exchange. Intensive Care Med. 2006;32:1627–1631. doi: 10.1007/s00134-006-0262-y. [DOI] [PubMed] [Google Scholar]
- 27.Roch A, Lepaul-Ercole R, Grisoli D, Bessereau J, Brissy O, Castanier M, Dizier S, Forel JM, Guervilly C, Gariboldi V, et al. Extracorporeal membrane oxygenation for severe influenza A (H1N1) acute respiratory distress syndrome: a prospective observational comparative study. Intensive Care Med. 2010;36:1899–1905. doi: 10.1007/s00134-010-2021-3. [DOI] [PubMed] [Google Scholar]
- 28.Sidebotham D, Allen SJ, McGeorge A, Ibbott N, Willcox T. Venovenous extracorporeal membrane oxygenation in adults: practical aspects of circuits, cannulae, and procedures. J Cardiothorac Vasc Anesth. 2012;26:893–909. doi: 10.1053/j.jvca.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell MD, Mikkelsen ME, Umscheid CA, Lee I, Fuchs BD, Halpern SD. A systematic review to inform institutional decisions about the use of extracorporeal membrane oxygenation during the H1N1 influenza pandemic. Crit Care Med. 2010;38:1398–1404. doi: 10.1097/CCM.0b013e3181de45db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong I, Vuylsteke A. Use of extracorporeal life support to support patients with acute respiratory distress syndrome due to H1N1/2009 influenza and other respiratory infections. Perfusion. 2011;26:7–20. doi: 10.1177/0267659110383342. [DOI] [PubMed] [Google Scholar]
- 31.Zangrillo A, Landoni G, Biondi-Zoccai G, Greco M, Greco T, Frati G, Patroniti N, Antonelli M, Pesenti A, Pappalardo F. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit Care Resusc. 2013;15:172–178. [PubMed] [Google Scholar]
- 32.Zampieri FG, Mendes PV, Ranzani OT, Taniguchi LU, Pontes Azevedo LC, Vieira Costa EL, Park M. Extracorporeal membrane oxygenation for severe respiratory failure in adult patients: A systematic review and meta-analysis of current evidence. J Crit Care. 2013;28:998–1005. doi: 10.1016/j.jcrc.2013.07.047. [DOI] [PubMed] [Google Scholar]
- 33.Abrams DC, Brenner K, Burkart KM, Agerstrand CL, Thomashow BM, Bacchetta M, Brodie D. Pilot study of extracorporeal carbon dioxide removal to facilitate extubation and ambulation in exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10:307–314. doi: 10.1513/AnnalsATS.201301-021OC. [DOI] [PubMed] [Google Scholar]
- 34.Abrams D, Brodie D. Emerging indications for extracorporeal membrane oxygenation in adults with respiratory failure. Ann Am Thorac Soc. 2013;10:371–377. doi: 10.1513/AnnalsATS.201305-113OT. [DOI] [PubMed] [Google Scholar]
- 35.Jones A, Barrett N, Scales D, Beale R.Ventilatory support versus ECMO for severe adult respiratory failure Lancet 2010375550–551.author reply 1 [DOI] [PubMed] [Google Scholar]
- 36.Zwischenberger JB, Lynch JE. Will CESAR answer the adult ECMO debate? Lancet. 2009;374:1307–1308. doi: 10.1016/S0140-6736(09)61630-5. [DOI] [PubMed] [Google Scholar]
- 37.Checkley W. Extracorporeal membrane oxygenation as a first-line treatment strategy for ARDS: is the evidence sufficiently strong? JAMA. 2011;306:1703–1704. doi: 10.1001/jama.2011.1504. [DOI] [PubMed] [Google Scholar]
- 38.Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, Lefrant JY, Prat G, Richecoeur J, Nieszkowska A, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:646–655. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 39.Murad MH, Montori VM. Synthesizing evidence: shifting the focus from individual studies to the body of evidence. JAMA. 2013;309:2217–2218. doi: 10.1001/jama.2013.5616. [DOI] [PubMed] [Google Scholar]