Abstract
Objective: The aim of this study was to assess and regulate heat generation in the dental pulp cavity and circumambient temperature around a tooth during laser ablation with a femtosecond laser in a confined space. Background data: The automatic tooth preparing technique is one of the traditional oral clinical technology innovations. In this technique, a robot controlled an ultrashort pulse laser to automatically complete the three-dimensional teeth preparing in a confined space. The temperature control is the main measure for protecting the tooth nerve. Methods: Ten tooth specimens were irradiated with a femtosecond laser controlled by a robot in a confined space to generate 10 teeth preparation. During the process, four thermocouple sensors were used to record the pulp cavity and circumambient environment temperatures with or without air cooling. A statistical analysis of the temperatures was performed between the conditions with and without air cooling (p < 0.05). Results: The recordings showed that the temperature with air cooling was lower than that without air cooling and that the heat generated in the pulp cavity was lower than the threshold for dental pulp damage. Conclusions: These results indicate that femtosecond laser ablation with air cooling might be an appropriate method for automatic tooth preparing.
Keywords: : temperature measurement, temperature control, heat generation, tooth preparing, femtosecond laser
Introduction
To overcome the drawbacks of current manual tooth preparing techniques, such as poor accuracy, low efficiency, or even the inducement of iatrogenic injuries to the gums, lips, cheeks, and tongue, an automatic tooth preparing system for oral clinical operations was developed. By integrating robotics, computer-aided design, and medical laser technologies, the system can precisely control an ultrashort pulse laser (USPL) beam, which ablates tooth hard tissues, thus replacing conventional mechanical grinding equipment.1 However, the heat generated during the removal of dental hard tissues may lead to a temperature increase, causing painful sensations or damaging the dental tissues. The biological effect of heat generation is an important issue to evaluate before applying a novel technology in clinical practice, especially in the oral area.
Laser techniques have been used in dental treatments since 1960. Treatments that use such laser techniques include periodontal scaling,2 root canal sterilization,3 tooth bleaching,4 and surgical excisions of soft tissues.5 These treatments were developed because they have several advantages, namely that they are conservative,6 comfortable,7 have no mechanical vibration,8 exhibit fewer unpleasant sounds, and are less traumatic to patients.7,9
The Er:YAG laser has been researched in the past because of its microexplosion capability and as it produces minimal thermal damage during the mechanical ablation process, making it a promising replacement for conventional handpieces when performing effective enamel and dentin ablation. However, the ablation accuracy of this laser is too low for preparing the teeth.10–12
Recently, researches on short pulse durations have led to the development of high-tech laser devices with pulses that are in the order of microseconds or nanoseconds and of the so-called USPLs that have picosecond and femtosecond pulses.13,14 These laser pulses, which are amplified with energies of up to millijoules15 and are conveniently focused on the material's surface, allow thin layers to be ablated with excellent accuracy and reproducibility. This may result in much less collateral damage to the adjacent tissues compared to using other thermal, chemical, or mechanical processes.16,17 Such merits might make the USPL technology a good candidate for treating dental hard tissue with accurate preparation outlines and without causing thermal damage around the prepared cavities.
Heat generation has been examined by some foreign researchers during the ablation of dental hard tissue by an USPL. For instance, Braun et al.18 reported that heat generation could be observed when a picosecond laser was used to perform ablation of enamel and dentine specimens. The highest delta temperature values for enamel and dentin were about 67.0 and 13.6 K. Research by Marina Stella Bello-Silva et al. showed that USPLs may be suitable for cavity preparation in the dentin and enamel, since effective ablation and low temperature increases were observed. If adequate laser parameters are selected, this technique seems to be promising for promoting the use of laser-assisted minimally invasive approaches.
To our knowledge, no studies have investigated the heat generated by femtosecond lasers during dental hard tissue ablation in a confined space. This information is important, as too high temperature can damage the dental pulp and surrounding tissues. Consequently, the aim of the present in vitro study was to assess and regulate heat generation in the dental pulp cavity, as well as the circumambient temperature around a tooth during dental hard tissue ablation using a femtosecond laser in a confined space.
Materials and Methods
Automatic tooth preparing was performed with a robotic device that controlled a Yb:KYW diode-pumped, solid-state, thin-disk, femtosecond laser at 1025 nm, with a pulse width of <400 fs, repetition rate of 100 kHz, an average output power of 4.4 W, and a scan rate of 500 mm/s. The Jenoptik femtosecond laser system (JenLas® D2.fs, Jena, Germany) was used.
Ten mandibular intact first molars that were freshly extracted at Peking University Hospital of Stomatology were collected. The study was approved by the Bioethics Committee at the Stomatological Hospital of Peking University, Beijing, China (No. PKUSSIRB-201522044; Date: July 8, 2015). All experimental protocols were approved by the license committee. All experiments were performed in accordance with the approved guidelines and regulations. Patients were informed that extracted teeth would be used in this study and they provided informed consent permitting us to use the teeth. The experiment was performed at room temperature of 24°C.
Specimen preparation
An ultrasonic scaler was used to remove the dental calculus and soft tissues from the surface of the molars, which were then rinsed with physiological saline. The teeth were cut transversely along the cement-enamel separation using a diamond wire cutter (STX-202, Kejing Instrument Co., Ltd, Shenyang, China). The tooth crowns with the pulp cavities were stored in normal saline at 37°C until use.
Temperature recording
A thermocouple was embedded in the pulp cavity of one tooth with copper powder (Fig. 1a). The left mandibular first molar was removed from the standard artificial teeth model, and then the tooth with the thermocouple was fixed in the standard artificial teeth model (Fig. 1b). A tooth fixture was designed using reverse engineering software (Geomagic studio 2012; 3M), fabricated by Rapid Prototyping, and fit to the dental model with silicone rubber (Fig. 2). Then, the confined space was formed. Three additional thermocouples referred to as P1, P2, and P3 were fixed around the tooth in the confined space. Afterward, the laser beam was focused on the crown surface to complete the automatic process of preparing a tooth with the robotic device. Four thermocouples were separately connected to the Data logger Thermometer (TR-176c; Yuqing Technology Co., Ltd, Taiwan) to record the temperature during the ablation process in real time (Fig. 1c). The temperature was recorded once per 10 sec. Then, air cooling was used and the temperature was recorded at the four positions in the same order as before. We repeated the same experiment in the remaining nine teeth.
FIG. 1.
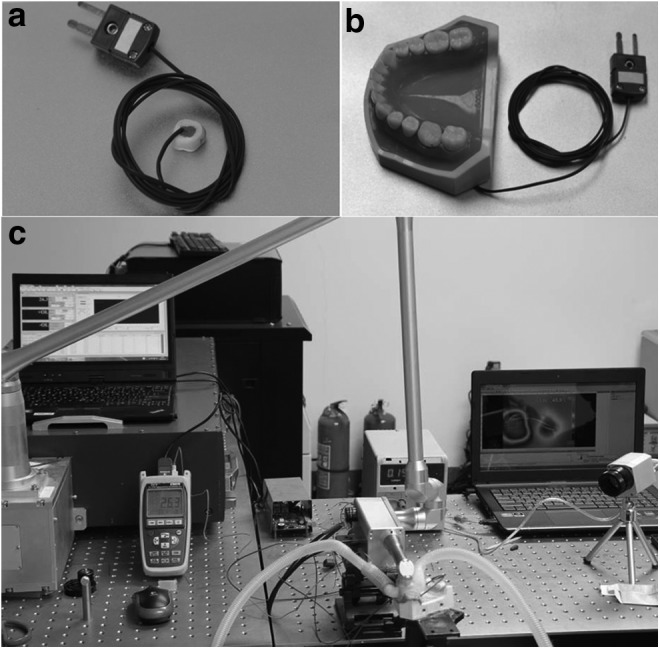
(a) The tooth with a thermocouple. (b) The tooth was fixed in the dental model. (c) The experimental platform.
FIG. 2.
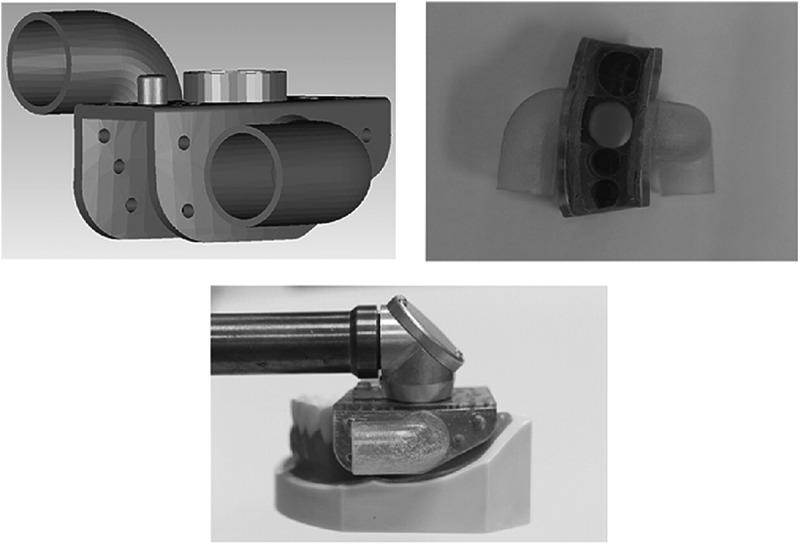
Physical prototype of the tooth fixture and the connections among the device, tooth fixture, and the target tooth.
Statistical analysis
The recorded data from 10 teeth were input into SPSS 19.0 software (IBM SPSS Inc., Chicago, IL). For each tooth, three temperature measurements (P1, P2, P3) of the ambient environment and the temperature of the pulp cavity were performed to minimize the impact of any individual conditions. Subsequently, the mean value of these three measurements was calculated as ambient environment for further statistical calculations so that one sample could be considered as one statistical unit. The measured data in the conditions with and without air cooling were analyzed using t-tests for independent samples and paired sample t-test. The differences of temperature in two conditions between 10 teeth were analyzed using one-way analysis of variance. A p value of <0.05 was considered statistically significant.
Results
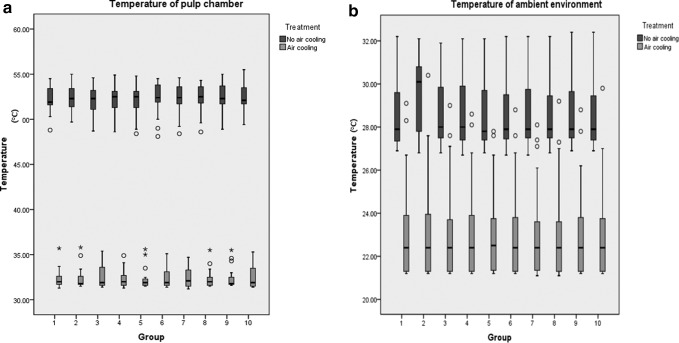
After average 22 min of ablation with the femtosecond laser, a tooth preparation of the tooth crown was generated (Fig. 3a, b). During the process of ablation, the temperature of the pulp cavity and the ambient environment increased steadily. There were no significant differences between temperatures of 10 teeth in two conditions. The temperature of pulp cavity without air cooling gradually increased, while temperatures with air cooling and that of ambient temperature were basically steady. And the temperature of the ambient environment was lower compared with the pulp cavity (Fig. 4). A significant difference in the temperature of the pulp cavity was observed between the conditions with and without air cooling (p < 0.05, Table 1). A significant difference between the conditions with and without air cooling was also found for the temperature of the ambient environment (p < 0.05, Table 2). Box plot diagrams show that under the air cooling condition, the temperatures of both the pulp cavity and ambient environment were lower than the temperatures in the condition without air cooling (Fig. 5).
FIG. 3.
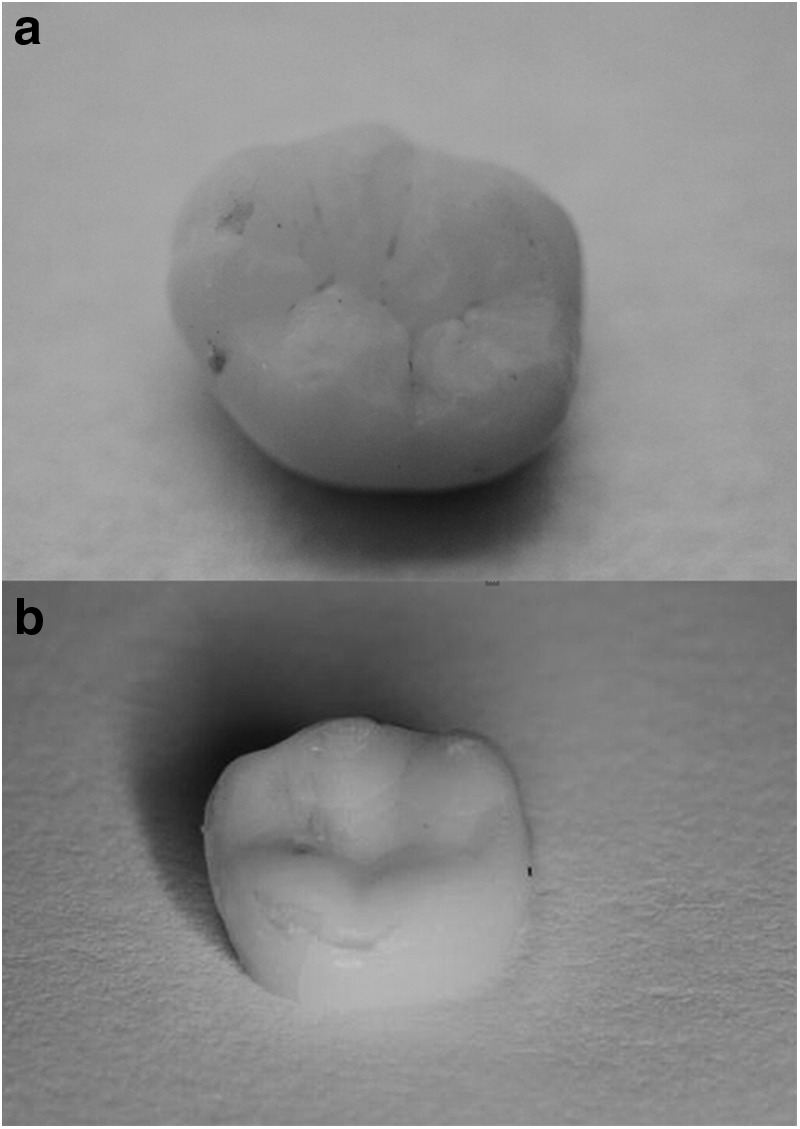
(a) The tooth crown before tooth preparing. (b) The tooth preparation after tooth preparing.
FIG. 4.
Temperatures of ambient environment and pulp cavity in two conditions.
Table 1.
The Statistical Analysis of Temperatures of the Pulp Chamber in the Two Conditions
| Condition | Temperature (°C) | t | p |
|---|---|---|---|
| Air cooling | 32.43 ± 1.56 | 129.85 | 0.00 |
| No air cooling | 52.31 ± 1.65 |
Table 2.
The Statistical Analysis of Temperatures of the Ambient Environment in the Two Conditions
| Condition | Temperature (°C) | t | p |
|---|---|---|---|
| Air cooling | 22.98 ± 1.88 | 53.35 | 0.00 |
| No air cooling | 28.53 ± 1.53 |
FIG. 5.
(a) Temperatures measured in the pulp chamber with or without air cooling. (b) Temperatures measured in the ambient environment with or without air cooling.
Conclusions
The experiment indicated that femtosecond laser ablation with air cooling might be an appropriate method for automatic tooth preparing. However, more researches were still needed to improve the accuracy and safety of the study.
Discussion
Lasers have been investigated as an option for ablating dental hard tissues. However, reports show that the use of laser systems can lead to charring, cracking, and damage of the enamel structures; moreover, lasers can cause excessive temperature increases in the pulp and surrounding tissues of up to 30°C.19 Typically, treatment with a conventional pulsed laser source leads to cracking and uncontrolled material removal, resulting in poor surface preparation.20 Several constraints and limitations in the dental applications of lasers, including the poor absorption by tooth structures induced by most high-power radiation lasers, significant excess heat deposition in the tooth, and the potential for intrapulpal damage, have led investigators to develop USPLs (pulse durations <10 ps) as a new method for ablating dental hard tissues.19 High-power pulses with durations that are shorter than the tissue thermal relaxation time are indicated to avoid thermal denaturation of the organic components of the tissues adjacent to the irradiated surfaces, thus the thermal damage induced by the femtosecond laser might be lower than the damage induced by other methods.21,22
Interactions of USPLs with dental hard tissues are based in the nonthermal aspects of the ablation process. When the laser irradiates the target tissue, it causes ionization and an electron avalanche in the superficial substrate within fractions of a second, which covers the ablation hydrodynamics, resulting in removal of the hard tissue. Then, the shockwave attenuates rapidly over a distance of a few microns, which is caused by the accompanying rarefaction wave. The rapidly ejected heated material removes most of the absorbed energy, and the air cooling promotes the ejection. Therefore, effective ablation is achieved, without causing thermal and mechanical damage in the remaining tooth.
According to the classical study by Zach and Cohen, the dental pulp is extremely sensitive to temperature variations and an increase of more than 5.6°C can result in pulp damage.23 The results of the present study suggest that the addition of air cooling during irradiation can reduce the temperature rise that may otherwise lead to thermal damage of the dental pulp tissue. The coordinates of the tooth fixture are registered with the coordinates of the tooth to ensure accurate ablation. With the help of the tooth fixture, the laser can be controlled to precisely ablate dental hard tissue in a confined space, thus avoiding to cause damage to the surrounding tissues with the laser. In this study, the temperature of the condition with air cooling was lower than the temperature of the condition without cooling, which indicates that air cooling is an effective way of reducing heat generation. Such findings suggest that the femtosecond laser may be an optional treatment for dental preparations given the lower temperatures it produces in the pulp cavity and on the tooth surface.
However, the femtosecond laser has some disadvantages and a number of unsolved problems, such as the cost of the device and the large size of the system due to the complexity of the device. In addition, with this technology, the treatment time is longer compared to that for traditional instruments, and different parameters should be set for teeth with varied calcification conditions. Further, articulated-arm delivery systems still result in energy loss. In the present study, the temperature of each point could not be measured simultaneously because of restrictions related to the experimental condition, thus the method used to obtain the temperature of the periodontal membrane and alveolar bone requires further study and development, and the long ablation times need to be reduced. For the enamel, ablation is better with the femtosecond laser independent of the output power used; however, studies should be performed to find an appropriate power that can satisfy both enamel and dentine ablation. Such experiments should be performed in an environment that simulates the oral temperature rather than room temperature. For these reasons, additional studies should be performed that investigate the ablation of hard dental tissues.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 81571023) and the National Natural Science Foundation of China (Grant No. 51475004).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Fusong Y, Yong W, Yaopeng Z, Yuchun S, Dangxiao W, Lyu P. An automatic tooth preparation technique: a preliminary study. An automatic tooth preparation technique: a preliminary study. Sci Rep 2016;6:25281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eberhard J, Ehlers H, Falk W, Açil Y, Albers H-K, Jepsen S. Efficacy of subgingival calculus removal with Er:YAG laser compared to mechanical debridement: an in situ study. J Clin Periodontol 2003;30:511–518 [DOI] [PubMed] [Google Scholar]
- 3.Sahar-Helft S, Sarp ASK, Stabholtz A, Gutkin V, Redenski I, Steinberg D. Comparison of positive-pressure, passive ultrasonic, and laser-activated irrigations on smear-layer removal from the root canal surface. Photomed Laser Surg 2015;33:129–135 [DOI] [PubMed] [Google Scholar]
- 4.Pleffken PR, Borges AB, Gonçalves SEDEP, Rocha Gomes Torres C. The effectiveness of low-intensity red laser for activating a bleaching gel and its effect in temperature of the bleaching gel and the dental pulp. J Esthet Restor Dent 2012;24:126–132 [DOI] [PubMed] [Google Scholar]
- 5.Genovese MD, Olivi G. Use of laser technology in orthodontics: hard and soft tissue laser treatments. Eur J Paediatr Dent 2010;11:44–48 [PubMed] [Google Scholar]
- 6.Yazici AR, Baseren M, Gorucu J. Clinical comparison of bur- and laser-prepared minimally invasive occlusal resin composite restorations: two-year follow-up. Oper Dent 2010;35:500–507 [DOI] [PubMed] [Google Scholar]
- 7.Keller U, Hibst R. Effects of Er:YAG laser in caries treatment: a clinical pilot study. Lasers Surg Med 1997;20:32–38 [DOI] [PubMed] [Google Scholar]
- 8.Braun A, Jepsen S, Deimling D, Ratka-Krüger P. Subjective intensity of pain during supportive periodontal treatment using a sonic scaler or an Er:YAG laser. J Clin Periodontol 2010;37:340–345 [DOI] [PubMed] [Google Scholar]
- 9.Wigdor H. Patients' perception of lasers in dentistry. Lasers Surg Med 1997;20:47–50 [DOI] [PubMed] [Google Scholar]
- 10.Keller U, Hibst R. Experimental studies of the application of the Er:YAG laser on dental hard substances: II. Light microscopic and SEM investigations. Lasers Surg Med 1989;9:345–351 [DOI] [PubMed] [Google Scholar]
- 11.Hibst R, Keller U. Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med 1989;9:338–344 [DOI] [PubMed] [Google Scholar]
- 12.Sonntag KD, Klitzman B, Burkes EJ, Hoke J, Moshonov J. Pulpal response to cavity preparation with the Er:YAG and Mark III free electron lasers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:695–702 [DOI] [PubMed] [Google Scholar]
- 13.Rode AV, Gamaly EG, Luther-Davies B, et al. Precision ablation of dental enamel using a subpicosecond pulsed laser. Aust Dent J 2003;48:233–239 [DOI] [PubMed] [Google Scholar]
- 14.Sheth KK, Staninec M, Sarma AV, Fried D. Selective targeting of protein, water, and mineral in dentin using UV and IR pulse lasers: the effect on the bond strength to composite restorative materials. Lasers Surg Med 2004;35:245–253 [DOI] [PubMed] [Google Scholar]
- 15.Strickland D, Mourou G. Compression of amplified chirped optical pulses. Opt Commun 1985;56:219–221 [Google Scholar]
- 16.Chichkov BN, Momma C, Nolte S, von Alvensleben F, Tünnermann A. Femtosecond, picosecond and nanosecond laser ablation of solids. Appl Phys A 1996;63:109–115 [Google Scholar]
- 17.Luengo MCL, Portillo M, Sánchez JM, et al. Evaluation of micromorphological changes in tooth enamel after mechanical and ultrafast laser preparation of surface cavities. Lasers Med Sci 2013;28:267–273 [DOI] [PubMed] [Google Scholar]
- 18.Braun A, Krillke RF, Frentzen M, Bourauel C, Stark H, Schelle F. Heat generation caused by ablation of dental hard tissues with an ultrashort pulse laser (USPL) system. Lasers Med Sci 2015;30:475–481 [DOI] [PubMed] [Google Scholar]
- 19.Keller U, Hibst R, Geurtsen W, et al. Erbium:YAG laser application in caries therapy. Evaluation of patient perception and acceptance. J Dent 1998;26:649–656 [DOI] [PubMed] [Google Scholar]
- 20.Dela Rosa A, Sarma AV, Le CQ, Jones RS, Fried D. Peripheral thermal and mechanical damage to dentin with microsecond and sub-microsecond 9.6 microm, 2.79 microm, and 0.355 microm laser pulses. Lasers Surg Med 2004;35:214–228 [DOI] [PubMed] [Google Scholar]
- 21.Sozzi M, Fornaini C, Cucinotta A, Merigo E, Vescovi P, Selleri S. Dental ablation with 1064 nm, 500 ps, Diode pumped solid state laser: a preliminary study. Laser Ther 2013;22:195–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Engelbach C, Dehn C, Bourauel C, Meister J, Frentzen M. Ablation of carious dental tissue using an ultrashort pulsed laser (USPL) system. Lasers Med Sci 2015;30:1427–1434 [DOI] [PubMed] [Google Scholar]
- 23.Zach L, Cohen G. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 1965;19:515–530 [DOI] [PubMed] [Google Scholar]