Abstract
Background
Epidural analgesia provides good pain control after many postoperative procedures, but it can lead to complications, has some contraindications, and occasionally fails. Intravenous lidocaine infusion has been suggested as an alternative. We assessed, in our clinical practice, the effects of perioperative intravenous lidocaine infusion compared with epidural analgesia for major abdominal surgery.
Methods
We conducted a retrospective review of patients who had received intravenous lidocaine (1 mg/kg per hour) perioperatively after a major abdominal surgery. We matched them with patients who had received epidural analgesia. We tested a joint hypothesis of noninferiority of lidocaine infusion to epidural analgesia in postoperative pain scores and opioid consumption. We assigned a noninferiority margin of 1 point (on an 11-point numerical rating scale) difference in pain and a ratio [mean (lidocaine) / mean (epidural)] of 1.2 in opioid consumption, respectively.
Results
Two hundred sixteen patients (108 in each group) were analyzed. Intravenous lidocaine was not inferior to epidural analgesia with respect to pain scores. Lidocaine infusion was inferior to epidural analgesia with respect to opioid consumption. Patients in the lidocaine group had fewer episodes of hypotension and less postoperative nausea and vomiting, pruritus, and urinary retention. Patients receiving lidocaine also had earlier urinary catheter removal and earlier first gastrointestinal function. Daily mental status assessment was similar between the 2 groups.
Conclusions
Patients who received systemic lidocaine infusions with the addition of PRN (as needed) opioids administered for breakthrough pain did not have clinically significant differences in pain scores on postoperative day 2 and beyond. Intravenous lidocaine infusion in major abdominal surgery was inferior to epidural analgesia with respect to opioid consumption. However, lidocaine was associated with improvements in several important aspects of recovery.
Major abdominal operations are painful, and epidural analgesia has been proposed as the criterion-standard analgesic modality after open abdominal surgery.1 Multiple meta-analyses1,2 comparing epidural analgesia with opioid-based patient-controlled analgesia (PCA) and continuous wound infiltration showed that epidural analgesia provides superior analgesia, faster return of gastrointestinal function, and lower incidence of pruritus. However, no difference was observed in the length of stay. Despite these benefits, epidural analgesia is not ideal in this population. It frequently causes hypotension that may result in excessive intravenous fluid administration,3 which is particularly deleterious after bowel surgery.1 It can also result in serious (although uncommon) complications such as epidural hematoma or abscess,4 and it has a relatively high failure rate.5 Furthermore, epidural analgesia is contraindicated in some patients.
Perioperative lidocaine infusion has been suggested as an alternative pain management modality in major abdominal surgeries. Multiple meta-analyses evaluating the efficacy of lidocaine infusion found lidocaine infusion to decrease postoperative pain intensity, reduce opioid consumption, facilitate gastrointestinal function, and shorten the length of hospital stay in comparison with placebo.6,7 Although there exist risks of neurological and cardiac toxicity, these were not substantiated in the trials.6,7
Although lidocaine infusion seems to be an effective pain management modality after major abdominal surgery,6,7 its effects in comparison with epidural analgesia has been investigated to a limited extent only. We previously reported a small randomized but unblinded trial in a population of patients who underwent bowel surgery and did not find statistically significant differences between groups in time to return of bowel function or hospital length of stay. The median pain score difference was not statistically significant. No statistically significant differences were found in pain scores for any specific postoperative day (POD) or in analgesic consumption.8
Nonetheless, in our institution and others, the use of perioperative lidocaine infusion has become popular because it is easily implemented and has fewer contraindications than epidural analgesia. We therefore had a substantial sample of clinical patients who could be compared with matched controls who received epidural analgesia. We hypothesized that perioperative lidocaine infusion would not be inferior in both postoperative pain scores and opioid consumptions to epidural analgesia.
METHODS
This is a retrospective review of patients who underwent major abdominal surgery at the University of Virginia and received either perioperative lidocaine infusion or epidural analgesia, during the period between October 2013 and October 2014. The departmental quality improvement committee approved the project. We intended to match patients who underwent major open abdominal surgery and received perioperative lidocaine infusion with those who had epidural analgesia by age (within 5 years), gender, and chronic preoperative use of opioids (for >1 month). We added the latter criterion anticipating it could alter postoperative analgesic requirements.
We assigned a noninferiority margin of 1-point (on an 11-point numerical rating scale) difference in pain and a ratio [mean (lidocaine) / mean (epidural)] of 1.2 in opioid consumption.9 Noninferiority is established when the lower bound of the 95% confidence interval (CI) does not cross the inferiority margin, whereas the comparison is rendered inconclusive if the 95% CI does cross the inferiority margin.10
We defined the primary outcomes as both postoperative pain scores and opioid consumption during the first 4 PODs or until patient discharge (whichever came first). We selected this relatively long period as our patients had major abdominal surgeries with fairly long length of stay. For the secondary outcomes, we studied the incidence of hypotension, postoperative nausea and vomiting (PONV), pruritus, and urinary retention, as well as the time to first ambulation, urinary catheter removal, return of gastrointestinal function, and hospital discharge. All patients who received intravenous lidocaine had been assessed daily for mental status changes and clinical manifestations of lidocaine toxicity.
Anesthetic and Analgesic Management
All patients had their surgery under general anesthesia with tracheal intubation. Typical anesthetic management included induction with propofol, intubation using rocuronium, and anesthetic maintenance using sevoflurane or desflurane. Muscle relaxant was reversed with neostigmine and glycopyrrolate. Patients typically received antiemetic prophylaxis with 4 mg ondansetron and occasionally dexamethasone. Intraoperative opioids were given at the discretion of the anesthesiologist.
Lidocaine infusions were typically started in the operating room at a rate of 2 to 3 mg/min. In the recovery room, the rate was decreased to 0.5 to 1 mg/min. The maximum rate used postoperatively was 1 mg/min.
Patients receiving epidural analgesia were infused 0.125% bupivacaine (except in gynecology cases where 0.0625% bupivacaine was used) with 10 μg/mL of hydromorphone at a rate of 8 mL/h. Epidural catheters were placed in the 9th or 10th thoracic intervertebral space. Lidocaine 1% to 2% could be given as a epidural bolus after emergence in order to provide rapid analgesia in the postanesthesia care unit (PACU), but then the infusion described above was run continuously with as few adjustments as possible. The time of starting the infusion was not standardized; however, for the majority of patients, it was initiated before incision.
All patients were routinely assessed by the nursing staff for pain scores every 4 hours using the 11-point numeric rating scale (NRS), where zero equals no pain and 10 equals the worst pain imaginable. The Acute Pain Service team, which consists of an anesthesiology attending, a resident, and a specialized pain nurse, visited the patients every morning after surgery. The team typically assessed the patient for the following: pain level (using NRS), functional level, nausea and vomiting, ability to tolerate clear liquids or current diet ordered, mental status, complaints of itching, and symptoms and signs of lidocaine toxicity (only in patients receiving lidocaine infusions).
The majority of the patients also received intravenous PCA. Opioid-naive patients received 0.1 to 0.2 mg hydromorphone per bolus, and opioid-tolerant patients received 0.3 to 0.4 mg hydromorphone per bolus; both groups had an 8-minute lockout. Patients who did not receive PCA were intravenously administered 0.5 to 1.0 mg hydromorphone every 1 hour PRN (as needed). Adjuvant pain medications administered to all patients included intravenous acetaminophen 1 g every 6 to 8 hours until the patient was able to take pills by mouth and then acetaminophen 625 mg every 6 hours. Once patients could take medications by mouth, oxycodone 5 to 10 mg was administered every 4 hours as needed. No gabapentinoids were used.
The selection of epidural analgesia versus lidocaine infusion was based on anesthesiologist and surgeon preference. There was a clear increase in the use of lidocaine infusions, and a concomitant decrease in epidural use, over time.
Data Collection and Synthesis
Pain scores were collected from the patient’s electronic chart over the predetermined time frame. If no pain score was reported at a specific time frame, we used the pain score reported within 2 hours before or after that point. Opioid consumption within the predetermined time frame was summed. All opioids were converted to morphine equivalent values using standardized formulas.11 Hypotension definition was not standardized to specific numbers; however, it was based on the clinical condition of each patient: any blood pressure that required adjusting or withholding pain management, with or without the need for fluid or vasopressor administration, was considered hypotension. Return of gastrointestinal function was defined as the first time the patient reported passing flatus or had bowel movement. Duration of hospital stay was calculated from the time the patient left the operating room until the discharge order was written. Similarly, times to ambulation, urinary catheter removal, and return of gastrointestinal function were calculated from the time the patient left the operating room. Patient satisfaction was assessed as a binary value (yes or no). Mental status was assessed and graded as follows: awake/alert, confused, somnolent, arouses with simulation, difficult to arouse, or unresponsive. Patients receiving lidocaine infusion were assessed daily for the following toxicity manifestations: numbness in face/mouth, dizziness, light headedness, confusion, ringing in ears, double vision, muscle twitching, seizure, arrhythmias, and numbness in arms or legs. Complications such as delirium, drug allergy, and falls were also documented by the nurses.
Sample Size Calculation
We tested a joint hypothesis of noninferiority of lidocaine infusion to epidural analgesia in postoperative pain scores and opioid consumption.9 Because these are both primary outcomes, the α error rate was each defined as 0.025. We used findings on POD1 from Swenson et al8 (a small randomized trial of intravenous lidocaine vs epidural analgesia conducted at our institute) to calculate our sample size. Theirmedian POD1 pain scores were 4.7 (interquartile range [IQR], 3.4–5.5) in the lidocaine group and 3.3 (IQR, 1.7–5.3) in the epidural group. Their median POD1 opioid consumption was 48 mg (IQR, 30–83 mg) in the lidocaine group and 57 mg (IQR, 27–100 mg) in the epidural group. We took the value of the median as a mean and calculated the SD as IQR /1.35. Minimum sample size required to detect a 1 -point difference in pain scores was computed with the following settings: 1-tailed t test, α = 0.025, power = 90%, and pooled SD of 2.15. Minimum sample size needed to detect a 20% difference in opioid consumption was computed with the following settings: α = 0.025, power = 90%, coefficient of variation = 0.94, with the largest clinically irrelevant percentage of the control mean to be detected to be 0.70. All sample size computations were conducted using R (R Foundation for Statistical Computing, Vienna, Austria). Results showed a minimum of 98 and 93 individuals (total = 196 and 186, respectively) are needed for the comparisons of pain scores and opioid consumption, respectively.
Statistical Analysis
We first evaluated the normality of the data using Shapiro-Wilk test and histograms. We reported the mean and SD for the normally distributed variables, and the median and 25th and 75th IQR for non-normally distributed variables.
For each patient, the primary outcome variables (postoperative pain scores and opioid consumption) were assessed at multiple time points after surgery. Taking into account the within individual and between-individual differences, we used mixed-effects models to examine the changes in the primary outcome variables. The use of a mixed-effects model has the advantage of accounting for nonnormality of data distribution, between-individual heterogeneity, and the presence of missing data.12
The general mixed-effects model takes the form of
where yij is the outcome variable, βn is the fixed-effect coefficients, xnij is the fixed-effect predictor for observation j in patient i, bin is the random-effect coefficients (assumed to be multivariate normally distributed), znij is the random-effect predictor, and εij is the error for observation j in patient i.
The mixed-effects model found to best fit the data is as follows:
where yij is the outcome variable (postoperative pain score or opioid consumption) for observation j in patient i; x1ij, x2ij, and x3ij are the linear time, quadratic time, and analgesia group (epidural vs lidocaine) fixed effects for observation j in patient i; bi0 is the random intercept for patient i; z1ij is the random slope for time; and εij is the error for observation j in patient i. This model suggests that the change in the outcome variable (postoperative pain score or opioid consumption) follows a nonlinear trend with time, with between-individual heterogeneity in patients’ initial postoperative pain scores and the rate of changes in postoperative pain scores across time.
For secondary outcome we used χ2 test or Fisher exact test to compare the incidence of each outcome. In our analyses, we used both SPSS Statistics for Windows, version 21.0 (IBM Corp, Armonk, New York), and the R programming language (R Foundation for Statistical Computing).
RESULTS
One hundred eight patients who received epidural analgesia were matched to 108 patients who received perioperative lidocaine infusion. Although we did not achieve perfect matching, there is no statistically significant difference in any of the demographic and matching criteria that determined a priori (Table 1). The majority of the patients underwent gynecologic or bowel surgery.
TABLE 1.
Demographic and Clinical Characteristics of the Patients
| Characteristics | Lidocaine Group (n = 108) | Epidural Group (n = 108) | P |
|---|---|---|---|
| Age,* y | 57.3 (14.8) | 58.2(13.7) | 0.706 |
| Sex† | |||
| Male | 39 | 49 | 0.439 |
| Female | 69 | 59 | 0.555 |
| Body mass index,‡ kg/m2 | 26.8 (23.1–30.7) | 27.2 (23.0–32.0) | 0.881 |
| Chronic preoperative opioid use† | 33 | 25 | 0.432 |
| Procedure anatomical site† | |||
| 1. Bladder/prostate | 8 | 6 | 0.808 |
| 2. Colorectal | 19 | 42 | 0.013 |
| 3. Gastric | 6 | 1 | 0.119 |
| 4. Gynecology | 27 | 16 | 0.171 |
| 5. Hepatobiliary | 11 | 3 | 0.052 |
| 6. Small bowel | 29 | 27 | 0.929 |
| 7. Spleen/pancreas | 6 | 5 | 1 |
Presented as mean (SD), P value from simple t test.
Presented as frequency, P value from χ2 or Fisher exact test.
Presented as median and (IQR), P value from Mann-Whitney U test.
Primary Outcomes
Taking into the account that the primary outcomes were assessed repeatedly over a period, mixed-effects models were fit to the data. Results from the mixed-effects models are shown in Table 2. The mean and 95% CIs for each of the primary outcome were derived from the mixed-effects models and were used in the subsequent inferiority analyses. The raw means and SEs of postoperative pain scores and postoperative opioid consumption are illustrated in Figures 1, A and B, respectively.
TABLE 2.
Effect of Epidural Versus Lidocaine on Pain Scores and Morphine Consumption Across Time
| Fixed Effects | Estimate | SE | t | P |
|---|---|---|---|---|
| Pain scores | ||||
| Intercept | 4.29 | 0.23 | 18.04 | <0.0001 |
| Time | −0.52 | 0.007 | −7.44 | <0.0001 |
| Time2 | 0.0004 | 0.00007 | 6.14 | <0.0001 |
| Group | 0.78 | 0.26 | 3.01 | 0.003 |
| Opioid consumption | ||||
| Intercept | 6.00 | 1.24 | 4.84 | <0.0001 |
| Time | 0.26 | 0.03 | 7.86 | <0.0001 |
| Time2 | −0.003 | 0.0003 | −8.86 | <0.0001 |
| Group | 5.77 | 1.50 | 3.84 | 0.0002 |
Linear mixed-effects models in which the intercept and the slope of time were estimated as random effects were fitted. Time2 is quadratic time.
FIGURE 1.
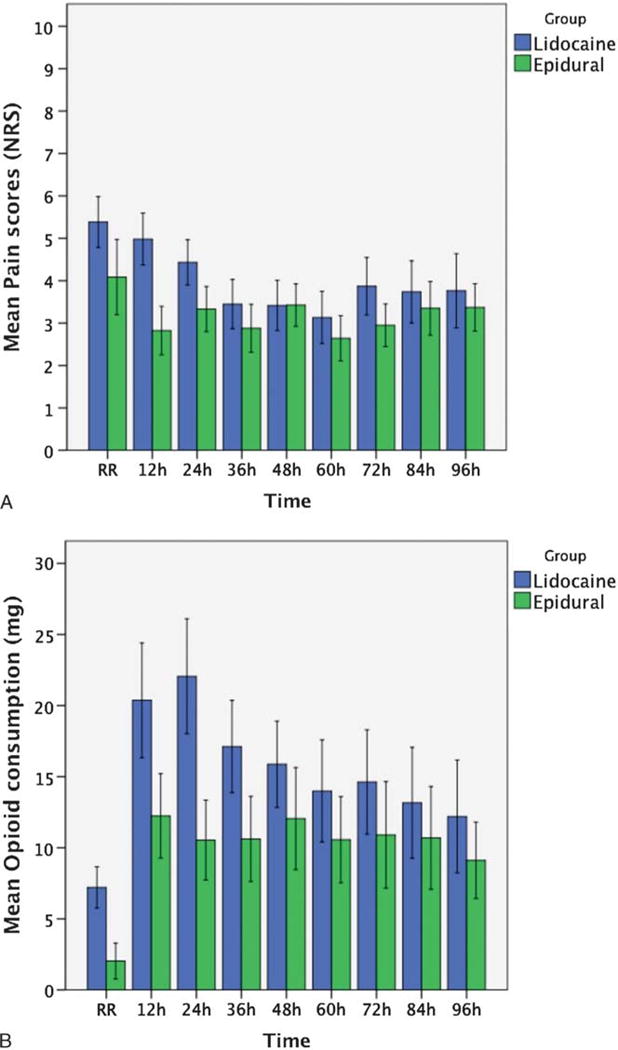
Mean and SE of (A) pain scores and (B) opioid consumption.
The noninferiority margin for pain score was set a priori as a 1-point difference (lidocaine – epidural) on the NRS pain scale. For the entire assessment period (96 hours), although the mean pain score difference between lidocaine infusion and epidural analgesia falls within the noninferiority region, the upper bound of the 95% CI extends beyond that of the 1-point noninferior margin. In other words, results were inconclusive regarding whether lidocaine infusion was inferior to epidural analgesia or not. The differences in postoperative pain scores on POD1 as well as POD2 to POD4 were also examined. For POD1, although the mean difference in pain scores is beyond the 1-point noninferior margin, the 95% CI extends beyond the noninferiority margin, rendering the results inconclusive. The mean difference in pain scores is less than 1 point for the remaining PODs, with 95% CIs within the noninferior margin; this indicates that lidocaine infusion is not inferior to epidural analgesia in pain scores on POD2 and beyond (Fig. 2A and Table 3).
FIGURE 2.
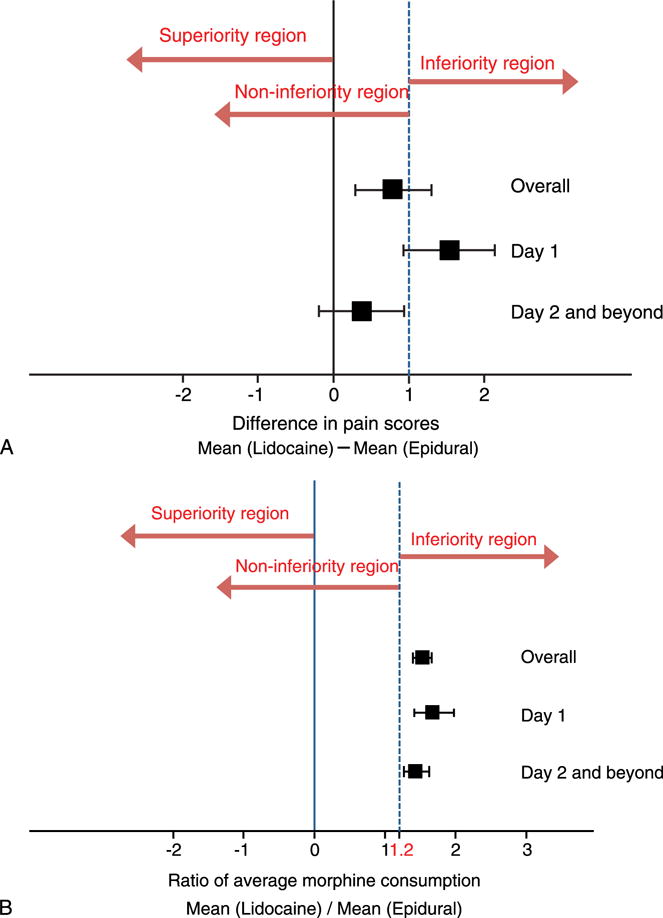
Noninferiority margins. The squares represent the mean, whereas the whiskers represent the 95% CI. A, Pain score: overall and POD1 were inconclusive, even though the mean of POD1 is beyond the inferiority margin, the lower bound of the 95% CI falls within the noninferiority margin. However, day 2 and beyond was noninferior, as the upper bound of the 95% CI did not cross the inferiority margin. B, Morphine consumption (ratio): overall inferior, day 1 inferior, day 2 and beyond inferior.
TABLE 3.
Difference in NRS Pain Scores and Opioid Consumption
| Difference in NRS Pain Scores | ||||
|---|---|---|---|---|
|
| ||||
| Lidocaine | Epidural | Mean Difference (Lidocaine − Epidural) (95% CI)* | Δ | |
| Overall | 4.09 (1.71) 3.95 [2.80, 5.34] |
3.18 (1.69) 2.96 [1.94, 4.17] |
0.78 (0.27–1.29) | 1 |
| Day 1 | 4.93 (1.22) 4.81 [4.10, 5.75] |
3.34 (1.39) 3.20 [2.33, 4.26] |
1.53 (0.92–2.14) | 1 |
| Day 2 and beyond | 3.51 (1.81) 3.35 [2.09, 4.92] |
3.10 (1.65) 2.91 [1.86, 4.25] |
0.35 (−0.21 to 0.91) | 1 |
|
| ||||
| Difference in Opioid Consumption | ||||
|
| ||||
| Lidocaine | Epidural | Ratio (Lidocaine / Epidural) (95% CI)† | Δ | |
|
| ||||
| Overall | 14.75 (10.13) 12.43 [8.13, 18.01] |
9.67 (10.09) 6.70 [2.98, 14.31] |
1.53 (1.40–1.66) | 1.2 |
| Day 1 | 15.56 (12.21) 13.73 [7.07, 19.13] |
9.26 (10.57) 6.52 [2.15, 12.46] |
1.68 (1.44–1.99) | 1.2 |
| Day 2 and beyond | 14.24 (12.21) 10.48 [6.60, 17.58] |
9.86 (11.51) 5.44 [1.29, 13.92] |
1.44 (1.28–1.64) | 1.2 |
Results presented in both mean (SD), and median [first, third IQR]. P < 0.025 is considered statistically significant.
Mixed-effects models were fitted to estimate the average NRS pain scores difference between the lidocaine and epidural groups across time.
Mixed-effects models were fitted to estimate the average morphine consumption ratio between the lidocaine and epidural groups across time.
A 1.2 ratio (lidocaine/epidural) of mean opioid consumption was set a priori as the noninferiority margin. For the entire duration of the assessment period (from PACU through 96 hours after surgery), as well as for POD1 and for POD2 to POD4, lidocaine infusion was found to be inferior to epidural analgesia in opioid consumption; patients receiving lidocaine infusions were administered more opioid than those receiving epidural infusions. The morphine equivalent consumption ratios, as well as the 95% CIs, fall beyond the noninferiority margin (Fig. 2B and Table 3).
Secondary Outcomes
Lidocaine infusion was associated with a lower incidence of hypotension (POD1 to POD3), PONV (POD2), pruritus (POD1 to POD4), and urinary retention (POD1 and POD2) than epidural analgesia. Time to urinary catheter removal and return of gastrointestinal function were also less in lidocaine patients. While there was a trend in the lidocaine group for earlier hospital discharge (by 24 hours), this trend did not reach statistical significance. Other comparisons and all statistics are summarized in Table 4. There was no statistically significant difference between the 2 groups in terms of daily mental status evaluation (Table 5). One patient in the lidocaine infusion group and 3 patients in the epidural group developed delirium. No allergic reactions or in-hospital falls in either group were reported.
TABLE 4.
Summary of the Secondary Outcomes
| Character/Incidence | Lidocaine Group | Epidural Group | P |
|---|---|---|---|
| Hypotension* | |||
| POD 1 | 4 (107), 3.7% | 28 (107), 26.1% | <0.0001 |
| POD 2 | 2 (99), 2% | 13 (104), 12.5% | 0.013 |
| POD 3 | 0 (60), 0% | 7 (93), 7.5% | 0.045 |
| POD 4 | 0 (35), 0% | 1 (71), 1.4% | 1 |
| Postoperative nausea and vomiting (PONV)* | |||
| POD 1 | 14 (107), 13% | 27 (107), 25.2% | 0.090 |
| POD 2 | 12 (99), 12.1% | 28 (103), 27.1% | 0.042 |
| POD 3 | 8 (60), 13.3% | 19 (91), 20.8% | 0.435 |
| POD 4 | 4 (35), 11.4% | 20 (70), 28.5% | 0.141 |
| Pruritus* | |||
| POD 1 | 3 (106), 2.8% | 38 (103), 27.1% | <0.0001 |
| POD 2 | 1 (99), 1% | 40 (103), 38.8% | <0.0001 |
| POD 3 | 1 (61), 1.6% | 32 (92), 34.7% | <0.0001 |
| POD 4 | 2 (35), 5.7% | 26 (70), 37.1% | 0.004 |
| Urine retention* | |||
| POD 1 | 3 (107), 2.8% | 7 (54), 12.9% | 0.035 |
| POD 2 | 3 (99), 3% | 9 (64), 14% | 0.029 |
| POD 3 | 3 (61), 4.9% | 5 (68), 7.3% | 0.723 |
| POD 4 | 1 (36), 2.7% | 2 (55), 3.6% | 1 |
| Patient pain management satisfaction (yes)* | |||
| POD 1 | 79 (107), 73.8% | 77 (102), 75.4% | 1 |
| POD 2 | 72 (99), 72.7% | 82 (102), 80.3% | 0.718 |
| POD 3 | 40 (58), 68.9% | 84 (91), 92.3% | 0.309 |
| POD 4 | 25 (34), 73.5% | 67 (70), 95.7% | 0.493 |
| Time for first ambulation,†‡h | 40 (22, 55) | 44 (26, 70) | 0.252 |
| Time for urinary catheter removal,†‡h | 26 (20, 58) | 50 (37, 96) | <0.0001 |
| Time for first return of bowel function,†‡h | 61 (41,85) | 84 (53, 107) | 0.019 |
| Duration of hospital stay,†‡h | 120 (75, 168) | 144 (102, 193) | 0.081 |
Presented as frequency, P value from χ2 or Fisher exact tests.
Presented as median and (IQR), P value from Mann-Whitney U test.
All these measurements calculated from the time the patient left the theater.
TABLE 5.
Comparisons of the Daily Mental Status Between Groups
| Mental Status Assessment | Lidocaine Group
|
Epidural Group
|
P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Day 1
|
Day 2
|
Day 3
|
Day 4
|
Day 1
|
Day 2
|
Day 3
|
Day 4
|
||
| (n = 107) | (n = 99) | (n = 60) | (n = 35) | (n = 105) | (n = 103) | (n = 92) | (n = 70) | ||
| Awake/Alert | 105 | 93 | 56 | 34 | 93 | 99 | 89 | 68 | 0.999 |
| Confused | 1 | 5 | 2 | 0 | 2 | 2 | 1 | 1 | 0.641 |
| Somnolent | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0.900 |
| Arouses with stimulation | 0 | 0 | 1 | 1 | 7 | 1 | 2 | 1 | 0.024 |
| Difficult to arouse | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0.142 |
| Unresponsive | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0.852 |
The majority (88.5%) of the lidocaine infusion was started at the beginning of surgery, with the remainder started at PACU discharge. The total amount of lidocaine infused was (in milligrams): median, 2550 (IQR, 1673–3597), or 2833 ± 168 (mean ± SE); the minimum was 540, and the maximum was 9168. Daily lidocaine toxicity assessments are summarized in Table 6.
TABLE 6.
Daily lidocaine Toxicity Assessment
| Day 1
|
Day 2
|
Day 3
|
Day 4
|
Total Events | |
|---|---|---|---|---|---|
| (n = 107) | (n = 99) | (n = 60) | (n = 35) | ||
| No manifestations | 103 | 93 | 55 | 33 | NA |
| Numbness in face/mouth | 3 | 2 | 0 | 0 | 5 |
| Dizziness | 0 | 0 | 1 | 0 | 1 |
| Light headed | 0 | 0 | 0 | 0 | 0 |
| Confusion | 0 | 2 | 3 | 2 | 7 |
| Ringing in ears | 0 | 2 | 0 | 0 | 2 |
| Double vision | 0 | 0 | 0 | 0 | 0 |
| Muscle twitching | 0 | 0 | 0 | 0 | 0 |
| Seizure | 0 | 0 | 0 | 0 | 0 |
| Arrhythmias | 1 | 0 | 0 | 0 | 1 |
| Numbness in extremity | 0 | 0 | 1 | 0 | 1 |
DISCUSSION
Our data indicate that intravenous lidocaine provides pain control that is noninferior for pain scores but inferior for opioid use, compared with epidural infusion. Although patients receiving intravenous lidocaine were administered more opioids, clinically significant adverse effects were reduced.
Pain scores in the cohort receiving intravenous lidocaine were noninferior to those in the group receiving epidural analgesia, although the noninferiority analysis was inconclusive for POD1. In clinical terms, pain scores during POD1 were 1.5 to 2 points higher in the lidocaine cohort as compared with the epidural cohort, suggesting that an additional mode of analgesia might be useful for this period. One attractive possibility is subarachnoid administration of a long-acting opioid at the time of surgery, which has been shown to be effective and has the appropriate duration of action.13 However, subarachnoid long-acting opioid can carry significant adverse effects such as delayed return of gastrointestinal movement, nausea, vomiting, and pruritus, which may overcome the benefits of systemic lidocaine. For the remainder of the assessment period (POD2 to POD4), intravenous lidocaine was noninferior to epidural analgesia with respect to pain scores. This pattern—modestly but nonsignificantly higher pain scores on POD1 and noninferior after that—was also noted in a small randomized trial we published previously.8 The trial included only subjects undergoing open-colon surgery. The previous study used a higher intravenous lidocaine rate than in the current comparison; similar epidural regimen was used. Results showed a 1.5-point difference (not statistically significant) in pain scores on POD1 in favor of epidural management and equivalent pain scores after that.
It seems remarkable that an intervention as simple as intravenous lidocaine could have an analgesic effect not inferior to that of epidural analgesia, yet several other trials in selected populations have reported similar benefits. Our previous trial in colorectal surgery was described previously.8 Kuo et al14 compared thoracic epidural analgesia to intravenous lidocaine and placebo (normal saline) in patients undergoing colonic surgery. They found the epidural group had better pain relief, lower opioid consumption, earlier return of gastrointestinal function, and less production of cytokines than intravenous lidocaine during 72 hours; however, the lidocaine group was better than the placebo group. The present report is, to our knowledge, the first in a general abdominal surgery population.
The analgesic mechanism of intravenous local anesthetics has not been well elucidated, although inflammatory modulating properties may likely play a role.15 It is likely that epidural analgesia works through the same mechanism to some extent, as intravenous lidocaine infusion rates are typically chosen to mimic local anesthetic plasma levels attained during epidural analgesia. It should also be realized that epidural therapy may not be as effective as we think, if only because of epidural failure rates and the need for reductions in epidural dosing because of hypotension (which happened in 25% of cases on POD1). This issue has been reviewed recently.16 Patients in the lidocaine cohort were administered more opioid than patients receiving epidural analgesia, approximately 5 mg morphine equivalent per day, on each of the PODs. It is possible that the increase in opioid consumption would have provided some additional analgesia. However, no between-group differences in opioid usage were observed in our previous study,8 and pain scores nonetheless were similar in both groups. Our patients typically had pain scores between 3 and 5; it is unclear if the beneficial effects of intravenous lidocaine would be as notable in patients with substantially higher pain ratings.
Importantly, the use of intravenous lidocaine was associated with significant reductions in a number of clinically relevant adverse effects associated with epidural analgesia. Hypotension necessitating changes in analgesic therapy (either holding or dose adjustment) occurred in approximately 25% of patients on POD1 and approximately 10% of patients on POD2 in the epidural analgesia cohort; it was virtually eliminated in the intravenous lidocaine group. Pruritus (probably resulting mainly from neuraxial opioid) was similarly almost eliminated. Nausea and vomiting were reduced by approximately 50%. This is of interest, as the intravenous lidocaine group received more opioid than did the epidural analgesia group. It may be related to the finding that gastrointestinal transit was restored earlier in those receiving intravenous lidocaine. The statistically significant difference in opioid consumption might not represent a clinical significance (eg, the difference was approximately 5 mg/d from POD2 and thereafter).
Maybe most important is the reduction in urinary retention. This well-known adverse effect of epidural therapy occurred in approximately 10% to 15% of patients in the epidural analgesia group and was reduced to approximately 3% in those receiving intravenous lidocaine. Urinary catheter removal happened after approximately 1 day in the intravenous lidocaine group and after 2 days in the epidural analgesia group. Considering the major risk of urinary tract infections induced by the presence of an indwelling catheter and the resulting current emphasis on early catheter removal,17 this is a very clinically relevant finding.
Probably as a result of 1 or more of these reductions in adverse effects, we observed a trend for patients receiving intravenous lidocaine to be discharged from the hospital earlier (by approximately 24 hours), although the trend did not reach statistical significance.
Our observations have some limitations. Because this study was based on clinical practice rather than a study design, results may be more clinically applicable; however, the nature of the study lacks the standardization of a clinical trial. For example, we observed variability in timing of epidural or lidocaine administration: the majority of lidocaine infusions were initiated intraoperatively, whereas the majority of epidural infusions were started near the end of the case. Such variability may have influenced the results. However, Møiniche et al,18 in a systematic review of approaches to preemptive analgesia, showed that timing of epidural therapy (ie, start at the beginning or at the end of the case) did not affect postoperative analgesia. For intravenous lidocaine, however, it is likely that intraoperative administration is a major factor in its postoperative effects, as studies comparing intravenous lidocaine infusions against placebo, despite widely varying postoperative infusion durations (from 2 hours19 to 48 hours20), have shown almost identical postoperative outcome effects. Furthermore, selection bias cannot be ruled out in our study. For example, hepatobiliary patients may have more frequently received systemic lidocaine because of the concern for coagulation derangements due to liver resections, and this may have significantly different degrees of the postoperative pain than other surgeries. It is our practice to use fixed epidural infusion rather than PCA; this also might have an effect on our outcomes. Finally, because this is not a randomized controlled trial, and there was a secular trend in replacing epidural analgesia for lidocaine, it is possible that other factors have influenced the observed outcomes.
There is no consensus as to appropriate inferiority margins for postoperative pain scores and opioid consumption. For instance, some studies used a 1.6-point difference in NRS score21,22 and 50% (ratio of 1.5) difference in opioid consumption,21,23 as the inferiority margins. If we had used these values, intravenously administered lidocaine would likely have been noninferior in all our comparisons. We adopted inferiority margins suggested by Mascha and Turan,9 because we felt these stricter margins would provide more confidence for the conclusion of noninferiority.
Our findings have implications for the development of Enhanced Recovery After Surgery protocols. These clinical pathways attempt to reduce opioid consumption and intravenous fluid administration and encourage oral intake and early ambulation.13 In most protocols, epidural analgesia is a key factor. However, epidural analgesia often results in increased fluid administration (because of hypotension) and decreased mobilization. In addition, the rate of failure and reductions in infusion rates required because of hypotension are issues of concern. Using intravenous lidocaine instead therefore appears an attractive option. Concerns that patients would be denied beneficial effects of epidural therapy on postoperative morbidities seem unwarranted based on the results of the MASTER trial,24 which showed only benefits on pain and respiratory end points. At our institution, the colorectal Enhanced Recovery After Surgery program now uses subarachnoid morphine administration before surgery and intravenous lidocaine thereafter, in addition to a variety of other modalities (nonopioid analgesic approaches, limits on intravenous fluids, early ambulation, etc). Results have been very positive, with a 2-day reduction in length of hospitalization as compared with historical controls (most of whom received epidural analgesia).13
In summary, our data indicate that after major abdominal surgery intravenous lidocaine provides pain control that is noninferior for pain scores but inferior for opioid use, compared with epidural infusion. Additional analgesia on POD1 should be considered. Importantly, a number of epidural-induced adverse effects are significantly reduced in incidence when intravenous lidocaine is used instead.
Acknowledgments
The authors thank Eric C. Ness, MD, and Aneesh P Goel, MD, for their participation in data collection.
Footnotes
An abstract was presented at the American Society of Regional Anesthesia and Pain Medicine, 40th Annual Meeting, Las Vegas, Nevada, May 2015.
The authors declare no conflict of interest.
References
- 1.Hughes MJ, Ventham NT, McNally S, Harrison E, Wigmore S. Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: a systematic review and meta-analysis. JAMA Surg. 2014;149:1224–1230. doi: 10.1001/jamasurg.2014.210. [DOI] [PubMed] [Google Scholar]
- 2.Werawatganon T, Charuluxananan S. WITHDRAWN: patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev. 2013:CD004088. doi: 10.1002/14651858.CD004088.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Low J, Johnston N, Morris C. Epidural analgesia: first do no harm. Anaesthesia. 2008;63:1–3. doi: 10.1111/j.1365-2044.2007.05407.x. [DOI] [PubMed] [Google Scholar]
- 4.Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990–1999. Anesthesiology. 2004;101:950–959. doi: 10.1097/00000542-200410000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: causes and management. Br J Anaesth. 2012;109:144–154. doi: 10.1093/bja/aes214. [DOI] [PubMed] [Google Scholar]
- 6.Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95:1331–1338. doi: 10.1002/bjs.6375. [DOI] [PubMed] [Google Scholar]
- 7.Sun Y, Li T, Wang N, Yun Y, Gan TJ. Perioperative systemic lidocaine for postoperative analgesia and recovery after abdominal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2012;55:1183–1194. doi: 10.1097/DCR.0b013e318259bcd8. [DOI] [PubMed] [Google Scholar]
- 8.Swenson BR, Gottschalk A, Wells LT, et al. Intravenous lidocaine is as effective as epidural bupivacaine in reducing ileus duration, hospital stay, and pain after open colon resection: a randomized clinical trial. Reg Anesth Pain Med. 2010;35:370–376. doi: 10.1097/AAP.0b013e3181e8d5da. [DOI] [PubMed] [Google Scholar]
- 9.Mascha EJ, Turan A. Joint hypothesis testing and gatekeeping procedures for studies with multiple endpoints. Anesth Analg. 2012;114:1304–1317. doi: 10.1213/ANE.0b013e3182504435. [DOI] [PubMed] [Google Scholar]
- 10.Head SJ, Kaul S, Bogers AJ, Kappetein AP. Non-inferiority study design: lessons to be learned from cardiovascular trials. Eur Heart J. 2012;33:1318–1324. doi: 10.1093/eurheartj/ehs099. [DOI] [PubMed] [Google Scholar]
- 11.Equivalent Opioid Calculator (EOC) Available at: http://clincalc.com/Opioids/. Accessed March 19, 2015.
- 12.Ma Y, Mazumdar M, Memtsoudis SG. Beyond repeated-measures analysis of variance: advanced statistical methods for the analysis of longitudinal data in anesthesia research. Reg Anesth Pain Med. 2012;37:99–105. doi: 10.1097/AAP.0b013e31823ebc74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thiele RH, Rea KM, Turrentine FE, et al. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015;220:430–443. doi: 10.1016/j.jamcollsurg.2014.12.042. [DOI] [PubMed] [Google Scholar]
- 14.Kuo CP, Jao SW, Chen KM, et al. Comparison of the effects of thoracic epidural analgesia and i.v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006;97:640–646. doi: 10.1093/bja/ael217. [DOI] [PubMed] [Google Scholar]
- 15.Hollmann MW, Durieux ME. Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology. 2000;93:858–875. doi: 10.1097/00000542-200009000-00038. [DOI] [PubMed] [Google Scholar]
- 16.Kooij FO, Schlack WS, Preckel B, Hollmann MW. Does regional analgesia for major surgery improve outcome? Focus on epidural analgesia. Anesth Analg. 2014;119:740–744. doi: 10.1213/ANE.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 17.Owen RM, Perez SD, Bornstein WA, Sweeney JF. Impact of surgical care improvement project inf-9 on postoperative urinary tract infections: do exemptions interfere with quality patient care? Arch Surg. 2012;147:946–953. doi: 10.1001/archsurg.2012.1485. [DOI] [PubMed] [Google Scholar]
- 18.Møiniche S, Kehlet H, Dahl JB. A qualitative and quantitative systematic review of preemptive analgesia for postoperative pain relief: the role of timing of analgesia. Anesthesiology. 2002;96:725–741. doi: 10.1097/00000542-200203000-00032. [DOI] [PubMed] [Google Scholar]
- 19.Groudine SB, Fisher HA, Kaufman RP, Jr, et al. Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg. 1998;86:235–239. doi: 10.1097/00000539-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Herroeder S, Pecher S, Schonherr ME, et al. Systemic lidocaine shortens length of hospital stay after colorectal surgery: a double-blinded, randomized, placebo-controlled trial. Ann Surg. 2007;246:192–200. doi: 10.1097/SLA.0b013e31805dac11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology. 2014;120:540–550. doi: 10.1097/ALN.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 22.Ilfeld BM, Mariano ER, Madison SJ, et al. Continuous femoral versus posterior lumbar plexus nerve blocks for analgesia after hip arthroplasty: a randomized, controlled study. Anesth Analg. 2011;113:897–903. doi: 10.1213/ANE.0b013e318212495b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen HW, Liu SS, Ware PD, Nairn CS, Owens BD. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg. 1998;87:93–97. doi: 10.1097/00000539-199807000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Rigg JR, Jamrozik K, Myles PS, et al. MASTER Anaethesia Trial Study Group Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet. 2002;359:1276–1282. doi: 10.1016/S0140-6736(02)08266-1. [DOI] [PubMed] [Google Scholar]


