Abstract
The number of hip arthroscopy procedures has significantly increased in the last several years, thereby necessitating individualized rehabilitation protocols for patients following hip arthroscopy. The purpose of this article is to review the literature on rehabilitation protocols for patients following hip arthroscopy and to describe a new protocol specifically designed for patients to return to running following hip arthroscopy. A search of PubMed was performed through October 2016 to locate studies of rehabilitation protocols for patients wishing to return to sport/general activity following hip arthroscopy. Patients at our institution who desired to return to running following hip arthroscopy underwent a set of return to running guidelines which are based on goal achievement within a three-phase system that begins with a walking program and finishes with return to distance running. Rehabilitation protocols for patients following hip arthroscopy frequently use a four-phase system in which Phase I focuses on regaining hip range of motion and protection of surgically repaired tissues, and Phase IV involves a pain-free return to sports. Rehabilitation protocols vary in timing in that some include a timeline with each phase taking a certain number of weeks while others are based on goal achievement. There is an overall lack of published outcomes based on patients adhering to various post-hip arthroscopy rehabilitation protocols.
INTRODUCTION
The number of hip arthroscopy procedures has significantly increased in the last several years [1] and, as such, has become a focus of several articles in the orthopedic and sports medicine literature. Coinciding with this procedural increase is an enhancement in arthroscopic technology, understanding of intra- and extra-articular pathologies of the hip, and means by which to return patients to their previous levels of activity following arthroscopic procedures.
Despite these recent advancements, a paucity of literature exists regarding specific and dedicated rehabilitation protocols following hip arthroscopy [2, 3]. This gap in the published literature can have a significant impact on patients, especially those who desire to return to higher demand sporting activity, such as professional or competitive recreational athletes.
Several rehabilitation protocols exist for patients following hip arthroscopy [4–9], some of which are specifically geared toward patients following treatment of femoroacetabular impingement (FAI) [4, 9] or acetabular labral tears [6]. The reported rehabilitation protocols frequently use a four-phase system. In the four-phase system, Phase I focuses on regaining hip range of motion and protection of surgically repaired tissues. Phase II focuses on progressing range of motion, improving neuromuscular control, and achieving independence in activities of daily living with minimal pain. In Phase III, patients should begin to restore muscular strength and become recreationally asymptomatic. Finally, Phase IV involves a pain-free return to sports.
While most surgeons allow return to sports between 12 and 20 weeks following hip arthroscopy, the exact return to sport guidelines vary depending on the procedure performed as well as the patient-specific sport. Rehabilitation protocols further vary in phases based on phase endpoint. Some promote a timeline in which each phase lasts a certain number of weeks, while others focus on progression based on goal achievement by the end of each phase. Each of these protocols is designed with the goal of returning patients to activity without symptoms or limitations. However, these rehabilitation programs are focused on returning patients to sports without any specificity as to which sport patients are returning. Furthermore, outcomes have not been published on patients whom were included in these rehabilitation programs. The currently published protocols also lack direction for return to specific high-impact sport activities such as running.
The purpose of this article is to review the literature on rehabilitation protocols for patients following hip arthroscopy and to describe a new protocol specifically designed for patients to return to running following arthroscopic hip surgery. Institution of a rehabilitation protocol clearly geared toward patients who are runners allows for more sport-specific training and patient-centred goals to be reached throughout the protocol. In addition, a sport-specific protocol allows physical therapists to pinpoint milestones and identify possible setbacks if a patient fails to progress at a certain step of the running progression program.
The aim of this program is to optimize the return to running with minimal setbacks by establishing a progressive stepwise program, and includes a dynamic warm-up, strengthening exercises, a plyometric/drill progression, and a return to running progression. Drills are meant to improve reactivity, recruitment, and control of the injured limb, as well as to create symmetrical movement patterns. This program builds off of previously published protocols and is the first to discuss specific modalities for a return to running following arthroscopic hip surgery.
BACKGROUND
The return to running program was initially developed to help patients who were attempting to return to running following hip surgery, though it can be used for any patient attempting to return to running following a lower extremity injury or surgery. This program was developed due to the high rate of recurrent pain or disability seen in our tertiary centre shortly after attempting to return to running. Furthermore, it has been our experience that many patients failed upon return to activity because they had been cleared to progress based on healing guidelines rather than functional achievements in terms of strength, gait, or pain. Most patients were attempting to resume running at a level they had run previously, and were unable to sustain or progress secondary to pain in joints, muscles, or compensating tissues. This program is also used with prehabilitation, though most participants are post-surgery after failing to improve with conservative treatments. Based on our experience of 3 years using this program, approximately 400 patients who have undergone hip labral repair, acetabular rim resection and/or femoral head osteochondroplasty for FAI have performed well using the protocol described below.
RUNNING PROGRESSION PROGRAM
The running progression program should be initiated approximately 3 months following surgery, although this may vary to some degree depending on individual patients and the procedure performed. Patients undergoing cartilage restoration procedures such as microfracture, microdrilling or cell therapy, or patients with underlying dysplasia or borderline dysplasia should start approximately 6 weeks later, as these patients are typically non-weight bearing for the first 6 postoperative weeks. While in the early stages of recovery, the program gives patients a realistic roadmap for progressive return so that they may work independently for a time at their own pace before returning to clinic for follow-up.
Patients should be provided with a few key points to remember throughout this program: (i) progress gradually, giving recovering tissue and joints time to adapt, (ii) avoid speed and hills in early progressions, (iii) start running on soft surface or treadmill before progressing to pavement/road, (iv) cross train especially in initial phases and (v) incorporate adequate recovery between runs. Throughout this progression, patients should continue to monitor their comfort level, as shown in Table I.
Table I.
Patients should continue to monitor their discomfort level throughout their training progress
| Acceptable: Continue to progress training | Unacceptable: Back off training |
|---|---|
| General muscle soreness | Pain that lasts for 2–3 days after a workout |
| Slight joint discomfort after workout or next day that resolves within 24 h | Pain that is evident at the beginning of a run/walk then becomes worse as run/walk continues |
| Slight stiffness at beginning of run or walk that dissipates after first 10 min | Pain that is keeping the patient awake at night |
| Pain that changes the patient’s stride |
The core principle of the running progression program is to carefully pass through therapeutic exercises while building upon a baseline level of fitness. This core program involves strength maintenance exercises and dynamic warm-up exercises which are performed coincident with progression through each phase.
The strength maintenance exercises are designed to keep certain muscles activated. The gluteal/hip complex, core and balance exercises all have demonstrated importance in lower extremity injuries [10, 11]. Starting with quick steps and ladders to keep the feet under the body, plyometrics improve muscle reaction and body control and are progressed in intensity and volume. Plyometrics for increasing maximal explosiveness are not performed as the protocol is intended for runners rather than explosive athletes such as football or basketball players. Video links are provided to the patients, and included instructions for the dynamic work-up routine as well as all three phases of the plyometrics program. These videos allow patients to progress through much of the rehabilitation protocol without constant assistance from a therapist.
Strength maintenance exercises
During this program, it is important to continue strengthening exercises provided by the physical therapist (Fig. 1; Table II). The side plank has been shown to activate the gluteus medius and external oblique abdominis muscles [12, 13], while single-limb squats have been shown to activate the gluteus medius and maximus [12, 14]. The remaining exercises may be more useful for training endurance or body stabilization during running.
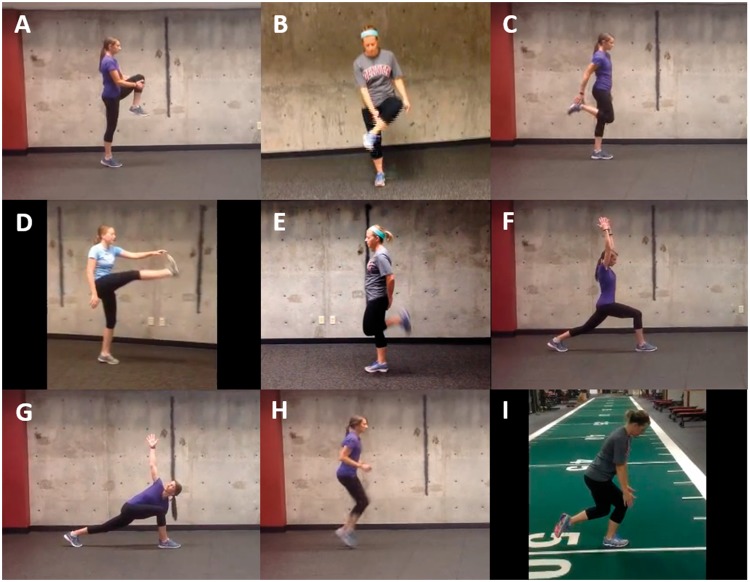
Fig. 1.
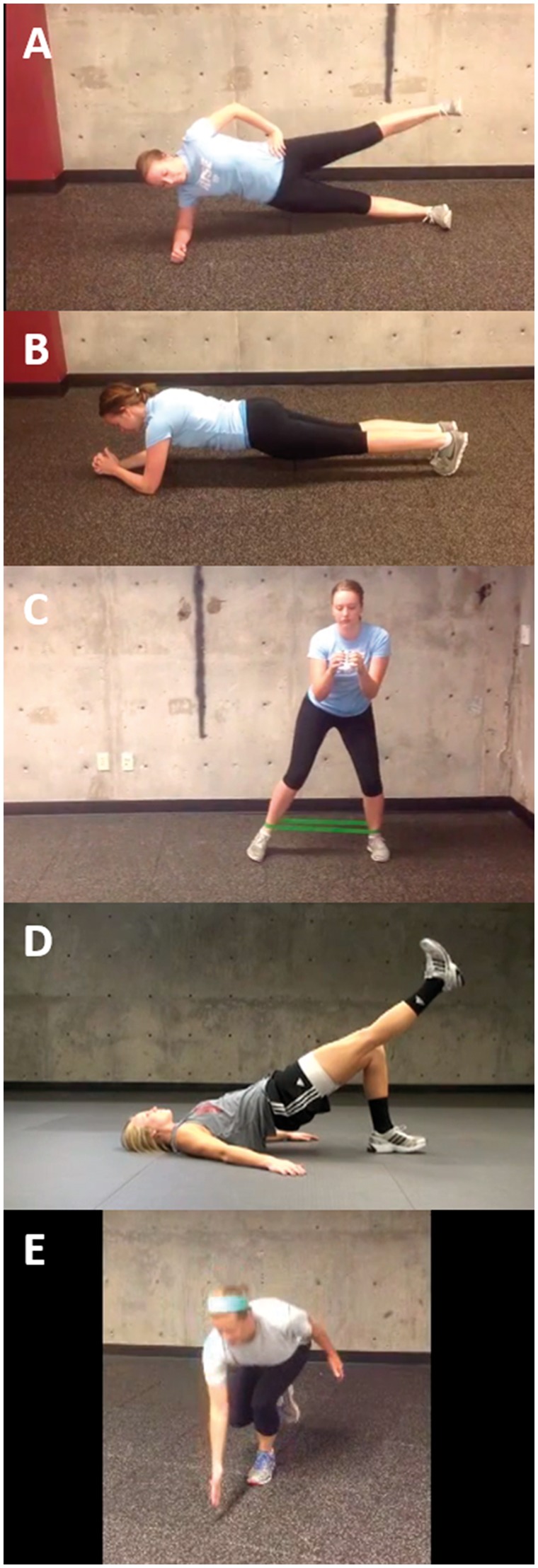
Strength maintenance exercises. (A) Side plank raises, (B) front planks, (C) band walks, (D) supine bridge and (E) single leg squat reach.
Table II.
Strength maintenance exercises
| Exercise | Video links |
|---|---|
| Side plank raises | https://youtu.be/x_F_xfiCZtA |
| Front planks | https://youtu.be/3_YvcCUitzQ |
| Band walks | https://youtu.be/baeAQXHvwhY |
| Supine bridge | https://youtu.be/WQrmXZDyLrU |
| Single leg squat reach | https://youtu.be/_R5ZbG-eYRM |
Dynamic warm-up
The purpose of this warm-up is to confirm that the muscles involved in running are warmed up and activated, and that the mobility necessary to run is available. Neuromuscular warm-up activities have been shown to prevent lower extremity injuries [11], and therefore it is very important for this warm-up to be performed prior to each workout or run (Fig. 2; Table III).
Fig. 2.
Dynamic warm-up.(A) Knee hug to calf raise, (B) in/out heel taps, (C) swing kicks, (D) soldier walks, (E) glute kicks, (F) walking lunges with reach and rotation, (G) lunge twist, (H) quick steps and (I) Single-leg mini-squat to calf raise.
Table III.
Dynamic warm-up
| Exercise | Repetitions | Video links |
|---|---|---|
| Knee hug to calf raise | 2 × 20 steps | https://youtu.be/RiYVoDjdbys |
| In/out heel taps | 2 × 20 steps | https://youtu.be/6lZT2tPZsmw |
| Swing kicks | 2 × 20 steps | https://youtu.be/0G6czNCrTXg |
| Soldier walks | 2 × 20 steps | https://youtu.be/hB3OsqYJuW8 |
| Glute kicks | 2 × 20 steps | https://youtu.be/H2OQ9v4k8g8 |
| Walking lunges with reach and rotation | 2 × 10 steps | https://youtu.be/0GO1ZsckaDk |
| Lunge twist | 2 × 10 steps | https://youtu.be/DVFwBCQQnHo |
| Quick steps |
|
https://youtu.be/BMLrzElmuNM |
| Single-leg mini-squat to calf raise | × 12 each leg | https://youtu.be/BqDe0lrGoas |
PHASES OF THE PROGRAM
Phase 1: Walking program
Patients should be able to walk 30 min pain-free at a fairly aggressive pace (at least 3.5 miles per hour). Patients should start on a treadmill before progressing to outdoor surfaces.
Phase II: Quick response and plyometric routine
Quick muscle response and plyometrics are initiated in this phase, progressing to about 500–600 foot contacts between one and two legs. Thus, if a runner has an average turnover of 170–180 strides/min, then running for 5–7 min would be required to reach the necessary 500–600 single-foot contacts. Plyometric training has been shown to reduce the energy cost of running when compared with dynamic weight training [15, 16]. Thus, successful completion of this phase is a good indicator that an athlete is ready to initiate the running program. Upon completion of the Level I plyometric program (Table IV), the walk/jog progression may be initiated if the following criteria have been met: (i) successful completion of Phase I and II, (ii) no pain with daily activities and (iii) walk without a limp.
Table IV.
Level I plyometric program
| Exercise | Repetitions | Video links |
|---|---|---|
| Ladders (40 ft) |
|
https://youtu.be/fK-4giDn9Wc |
| 2 foot line jumps Front/back with bounce | 3 × 12 | https://youtu.be/7cqjvO8yhUk |
| 2 foot dot hops | 3 × 3 rounds each way | https://youtu.be/zB6s32K_654 |
| Alternating hop/hold | 3 × 10 total jumps | https://youtu.be/f33-b-spZeo |
| Alternating 1 leg hops with bounce | 3 × 10 total jumps | https://youtu.be/hjxtS7t0_SU |
Walk/jog program
The goal of this program is for the patient to initiate and gradually progress their running volume without an increase in symptoms (Table V). It may be best for patients to begin the running program on a treadmill as this allows for more control of speed and distance. Patients should remember a few key points during this part of the program: (i) No hills or incline, (ii) no speed work, (iii) work on form and (iv) run every other day.
Table V.
Walk/jog progression
| Run interval (min) | Walk interval (min) | Repetitions | Total run time (min) | Total time spent (min) |
|---|---|---|---|---|
| 1 | 1 | × 7 | 7 | 14 |
| 2–3 | 1 | × 5 | 10–15 | 15–20 |
| 3–5 | 1 | 20 | 24+ | |
| Run until fatigue or form failure, then walk 1–2 min, then repeat for a total run time of 25–30 min | ||||
| Initiate running outdoors | ||||
| Jog every other day with a goal of reaching 30 consecutive min | ||||
Patients should end each run with a 3–5 min walk and mobility/stretching exercises. Patients should complete each step 2–3 times before progressing to the next step.
Depending on the patient’s athletic goals and the recommendations of the physical therapist, a patient may continue with Level II (Fig. 3; Table VI) and Level III (Fig. 4; Table VII) plyometric drills, as well as the return to distance running program (see below).
Fig. 3.
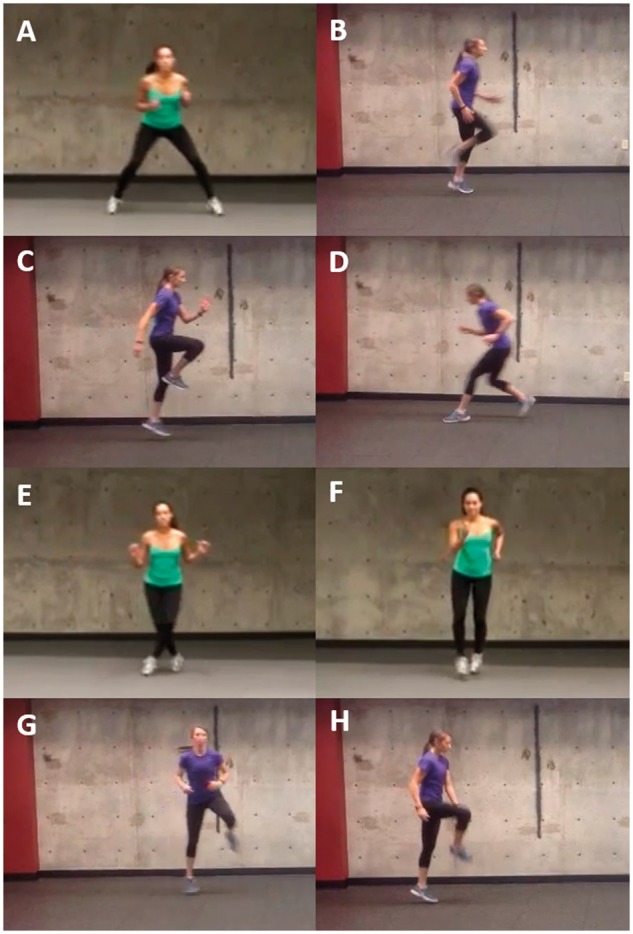
Level II plyometric program. (A) Lateral shuffles, (B) high knees, (C) forward/backward skips, (D) backpedal, (E) grapevine, (F) boxer shuffles, (G) Lateral skips and (H) tap skips.
Table VI.
Level II plyometric program
| Exercise | Video links |
|---|---|
| Lateral shuffles | http://youtu.be/IcTPmEF1apU |
| High knees | https://youtu.be/sUVnMWfl210 |
| Forward/backward skips | https://youtu.be/nPkXN_AhO6k |
| Backpedal | https://youtu.be/xkiPM47agQo |
| Grapevine | https://youtu.be/rQL7PJYu6nY |
| Boxer shuffles | https://youtu.be/ug1A8gfDzjo |
| Lateral skips | https://youtu.be/As1THjXMufs |
| Tap skips | https://youtu.be/JUOpDv4uPUM |
Fig. 4.
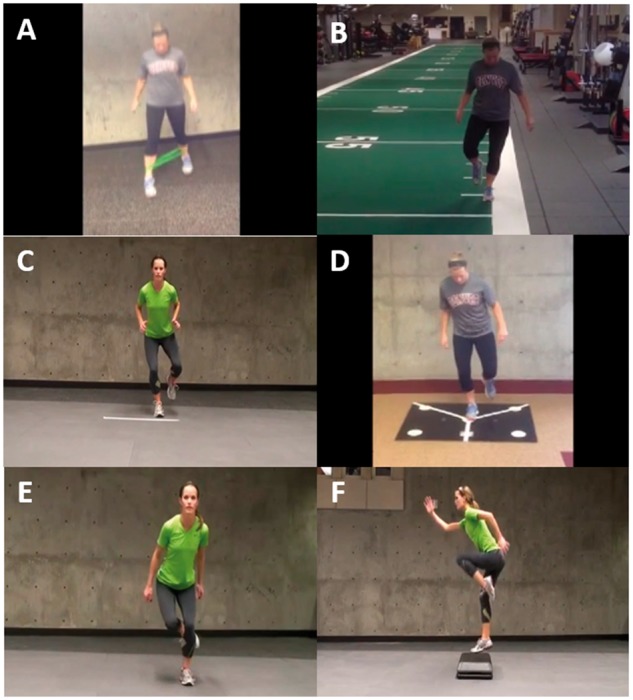
Level III plyometric program. (A) Matrix jacks, (B) 1 foot forward line hops, (C) 1 foot line hops with bounce, (D) 1 foot dot hops, (E) skater hops and (F) Box hoppers.
Table VII.
Level III plyometric program
| Exercise | Repetitions | Video links |
|---|---|---|
| Matrix jacks | 3 × 30 s | https://youtu.be/2LT9CbeAVfQ |
1 foot forward line hops
|
|
https://youtu.be/niv_fS0usGc |
1 foot line hops with bounce
|
|
https://www.youtube.com/watch?v=DALpKQE6zfs |
| 1 foot dot hops* | 2–3 × 3 each way | https://youtu.be/kQfms_RmTpo |
| Skater hops | 3 × 45–60 s | https://youtu.be/0I4ziA73p7w |
| Box hoppers | 3 × 12 | https://youtu.be/JdSVfzDfT0A |
| Jump rope |
|
R/L = right/left. *Patients should start with a pause, then progress to hot dots
Phase III: Return to distance running
During this last phase, it is important for patients to find their baseline. This is the distance the patient can run without pain and again 48 h later. Patients should find their baseline on a treadmill first as they will have more control over speed and distance. Patients should run for as long as they are comfortable and stop if running becomes painful. They should write down their distance, time and pace each time to track their progress. The goal in this phase is to find an appropriate distance and speed that does not increase pain symptoms. When patients feel comfortable on a treadmill, they may progress to straight-line running on level outdoor surfaces (e.g. sidewalks and running tracks).
Patients should still allow one day between each run, though at first they may take longer than a day depending on their comfort level. It is important during this phase for patients to only change one thing at a time (e.g. distance, speed, hills). This will allow the patient to identify the cause of a new source of pain. Finally, patients should progress gradually. Below are some progression guidelines for Phase III.
During weeks 1–2, patients should run 2–3 times per week, with two shorter runs between 50% and 60% of their baseline distance and one longer run at the baseline distance. During weeks 3–6, patients should run three times per week at their baseline level, with a rest day between each run. Patients should increase their distance by 10% each week. Starting in week 5, patients should reassess their baseline and increase running distance accordingly. Patients must monitor pain during and 24–48 h after increasing distance. It is important for patients to progress their weekly volume and long run distance by no more than 10% each week. Once their goal distance is reached, patients can then initiate speed or hill work. When initiating hill work, patients should be cautious of down hills.
The primary setback associated with this program is an inability to progress due to poor tissue adaptation. This may be a result of insufficient strength to progress through the program, or an inability of a patient’s tissue to adapt to load. It may also be that some patients attempt to skip steps of the program or do not allow sufficient recovery time after running.
By following this progression, it is much easier for the physical therapist to pinpoint where the failure to adapt occurs and the steps needed to address this failure in order to continue to progress to the desired activity level.
DISCUSSION
The purpose of this article is to review the literature on rehabilitation protocols for patients following hip arthroscopy and to describe a new protocol specifically designed for patients to return to running following arthroscopic hip surgery. Rather than specifying when patients may return to walking, plyometrics, distance running, et cetera, the proposed protocol allows for gradual activity progression based upon the comfort level of the patient and their ability to accomplish the prior protocol phase without injury or significant muscle soreness.
A number of prior publications have focused on rehabilitation protocols following hip arthroscopy, though most of these emphasize generalized return to sport, whereas our protocol is designed specifically for patients wishing to return to running. Voight et al. [8] performed a review on postoperative rehabilitation protocols for patients following hip arthroscopy, and although limited evidence-based data is available to support any one of these particular protocols, the authors did find that most protocols are divided into four general phases: (i) mobility and initial exercise, (ii) intermediate exercise and stabilization, (iii) advanced exercise and neuromotor control and (iv) return to activity. Similarly, Edelstein [17], Garrison [6] and Wahoff [9] reported on a four-phase rehabilitation protocol which was similar to those to which Voight has referred (Table VIII).
Table VIII.
Four-phase rehabilitation programs following hip arthroscopy
| Protocol | Edelstein et al. [17] | Garrison et al. [6] | Wahoff et al. [9] |
|---|---|---|---|
| Phase I | Phase I (the protective phase) | Initial exercise | Maximum protection and mobility |
| Time (weeks) |
|
1–4 | Varies based on progress |
| Goals |
|
|
|
| Phase II | Phase II | Intermediate exercise | Controlled stability |
| Time (weeks) |
|
5–7 | Varies based on progress |
| Goals | Achieve independence in daily activities with little or no discomfort | Continue progressing ROM and soft tissue flexibility |
|
| Phase III | Phase III | Advanced exercise | Strengthening |
| Time (weeks) |
|
8–12 | Varies based on progress |
| Goals | Become recreationally asymptomatic |
|
|
| Phase IV | Phase IV | Sports specific training | Return to sport |
| Time (weeks) |
|
12+ | Varies based on progress |
| Goals | Return to pain-free competitive state | Safe and effective return to competition or previous activity level |
|
ROM = range of motion
Edelstein’s post-hip arthroscopy rehabilitation protocol [17] begins with Phase I, which is known as the protective phase and entails weight-bearing and possibly range of motion restrictions depending on the procedure (Table VIII). Phase II focuses on achieving normal activities of daily living with little to no discomfort. During Phase III, patients are to become recreationally asymptomatic through strength building and core control. This is done through lunges, squats and box step-ups. Return to running may begin at 12 weeks postoperatively as long as the requirements of each phase are achieved. Finally, the goal of Phase IV is to return to sports pain-free without developing muscle breakdown or inflammatory responses. Similar to our suggestion of only changing one item at a time during the return to distance running phase, Edelstein suggests only manipulating one exercise variable per session during Phase IV, as this will reduce the chances of a setback.
Garrison et al. [6] reported specifically on rehabilitation following arthroscopy for acetabular labral tears. Similarly, this program consists of four phases (Table VIII). The intermediate exercises in Phase II include kneeling hip flexor stretches, seated resisted internal and external rotation, wall squats and single-leg bridging. Core strengthening exercises, typically with the use of an exercise ball, are a strong focus of Garrison’s Phase III.
Unlike the previous two rehabilitation protocols, Wahoff et al. [9] utilize a four-phase system that focuses on progress within each phase prior to advancement to the next phase (Table VIII). Timelines are not used in this protocol, which makes it similar to our return to running protocol. Wahoff encourages the use of a non-resistant stationary bicycle until a minimum of 6 weeks postoperatively. In addition, the authors discourage the use of a treadmill even through Phase III due to potential stress that the moving tread places on the anterior hip. From our experience, we believe that the advantages of treadmill use (precise speed and distance, soft surface and incline) outweigh the potential increase in hip stress.
Enseki et al. [5] restrict patients to partial weight bearing status for a minimum of 10 days postoperatively and up to 6 weeks following osteoplasty or hip microfracture procedures. Full passive range of motion is allowed by 2 weeks postoperatively for the majority of arthroscopic hip procedures. Before this time, excessive flexion or abduction may result in increased inflammation of the affected tissues. Return to jogging is allowed at 8–10 weeks following isolated arthroscopic procedures on the labrum. Competitive athletes may return to play at some point from 10 to 32 weeks postoperatively depending on the procedure as well as the sport.
Domb et al. [18] performed a study on return to sport following hip arthroscopy based on survey responses from 27 orthopaedic surgeons from high-volume hip arthroscopy centers. Seventy percent of the surgeons polled recommended waiting 12–20 weeks postoperatively before return to sport. Criteria for returning to sport included ability to run without pain (70% of hip arthroscopy centres), ability to jump without pain (59%), ability to reproduce all motions involved in the sport without pain (85%) and ability to perform a single-leg squat (19%). The majority of participating surgeons classified the following sports as high risk following hip arthroscopy: kickboxing, football, basketball and wrestling. Golf was the only major sport classified as low risk by more than half of the surgeons.
The purpose of this article was to review the literature on rehabilitation protocols for patients post-hip arthroscopy and to provide a novel protocol for return to running following hip arthroscopy. This program builds off of the background provided by previously described rehabilitation programs and proposes a functional rehabilitation program to improve results in a particular subset of patients. The novel program proposed here has been used with success in our institution; however, it has not been validated with long-term outcomes, and therefore should be treated as a guideline that can be altered according to individual needs.
CONCLUSIONS
In summary, this rehabilitation protocol is the first program specifically designed for patients who wish to return to running following hip arthroscopy/injury. Future studies should focus on obtaining short- and long-term outcomes based on patients who adhere to these rehabilitation guidelines as well as other published protocols for athletes returning to sports other than running to be able to draw comparisons and ultimately assess their effectiveness.
FUNDING
The authors report no funding for this study.
ACKNOWLEDGEMENTS
The authors would like to thank the models shown in Figs. 1–4 for volunteering their time.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Maradit Kremers H, Schilz R, Van Houten HK. et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty 2017; 32(3):750–5. [DOI] [PubMed] [Google Scholar]
- 2. Cheatham SW, Enseki KR, Kolber MJ.. Post-operative rehabilitation after hip arthroscopy: A search for the evidence. J Sport Rehabil 2015; 24:413–8. [DOI] [PubMed] [Google Scholar]
- 3. Grzybowski JS, Malloy P, Stegemann C. et al. Rehabilitation following hip arthroscopy—a systematic review. Front Surg 2015; 2:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Enseki KR, Martin R, Kelly BT.. Rehabilitation after arthroscopic decompression for femoroacetabular impingement. Clin Sports Med 2010; 29:247–55. [DOI] [PubMed] [Google Scholar]
- 5. Enseki KR, Martin RL, Draovitch P. et al. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther 2006; 36:516–25. [DOI] [PubMed] [Google Scholar]
- 6. Garrison JC, Osler MT, Singleton SB.. Rehabilitation after arthroscopy of an acetabular labral tear. N Am J Sports Phys Ther 2007; 2:241–50. [PMC free article] [PubMed] [Google Scholar]
- 7. Stalzer S, Wahoff M, Scanlan M.. Rehabilitation following hip arthroscopy. Clin Sports Med 2006; 25:337–57. [DOI] [PubMed] [Google Scholar]
- 8. Voight ML, Robinson K, Gill L, Griffin K.. Postoperative rehabilitation guidelines for hip arthroscopy in an active population. Sports Health 2010; 2:222–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wahoff M, Ryan M.. Rehabilitation after hip femoroacetabular impingement arthroscopy. Clin Sports Med 2011; 30:463–82. [DOI] [PubMed] [Google Scholar]
- 10. Geraci MC Jr, Brown W.. Evidence-based treatment of hip and pelvic injuries in runners. Phys Med Rehabil Clin N Am 2005; 16:711–47. [DOI] [PubMed] [Google Scholar]
- 11. Herman K, Barton C, Malliaras P, Morrissey D.. The effectiveness of neuromuscular warm-up strategies, that require no additional equipment, for preventing lower limb injuries during sports participation: a systematic review. BMC Med 2012; 10:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Distefano LJ, Blackburn JT, Marshall SW, Padua DA.. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther 2009; 39:532–40. [DOI] [PubMed] [Google Scholar]
- 13. Ekstrom RA, Donatelli RA, Carp KC.. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther 2007; 37:754–62. [DOI] [PubMed] [Google Scholar]
- 14. Krause DA, Jacobs RS, Pilger KE. et al. Electromyographic analysis of the gluteus medius in five weight-bearing exercises. J Strength Cond Res 2009; 23:2689–94. [DOI] [PubMed] [Google Scholar]
- 15. Berryman N, Maurel D, Bosquet L.. Effect of plyometric vs. dynamic weight training on the energy cost of running. J Strength Cond Res 2010; 24:1818–25. [DOI] [PubMed] [Google Scholar]
- 16. Bonacci J, Chapman A, Blanch P, Vicenzino B.. Neuromuscular adaptations to training, injury and passive interventions: implications for running economy. Sports Med 2009; 39:903–21. [DOI] [PubMed] [Google Scholar]
- 17. Edelstein J, Ranawat A, Enseki KR. et al. Post-operative guidelines following hip arthroscopy. Curr Rev Musculoskelet Med 2012; 5:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Domb BG, Stake CE, Finch NA, Cramer TL.. Return to sport after hip arthroscopy: aggregate recommendations from high-volume hip arthroscopy centers. Orthopedics 2014; 37:e902–5. [DOI] [PubMed] [Google Scholar]