Abstract
Femoral rotational malalignment is associated with pain and functional disability and may be a contributing factor to hip impingement as well as to instability. In general, the deformity can be addressed surgically by rotational osteotomy. However, the anatomic location of the deformity is debated. The goal of the present study was to narrow down the anatomic site of deformity using the lesser trochanter (LT) as an additional landmark. One hundred and eight patients underwent computer tomography (CT)-based rotational analysis of their lower extremities. Femoral torsion (FT) and LT torsion (LTT) were measured. The combined angle (CoA) between FT and LTT was calculated. Statistical evaluation was done by multiple regression analysis. Ninety-seven extremities were examined for FT and LTT. Average age was 41 years (SD = 16.9) with a range of 18–85 years. Mean values were 20° for FT (SD = 12.2) and −16° for LTT (SD = 11.3). Mean CoA was 37.2 (SD = 8.7). Statistical analysis reveals a strong linear relationship between FT and LTT (y=31+0.74x) and a weaker relationship between FT and CoA (y=31+0.24x). This study identifies the LT as a reliable landmark and shows a strong linear relationship between the orientation of the LT and the overall torsion of the femur below and above the LT with about two-thirds of torsional changes occurring distal to it. These results provide a considerable indication for a subtrochanteric osteotomy to address correction of femoral rotational deformity at its anatomical origin.
Level of Evidence: Level III, observational study.
INTRODUCTION
Femoro-acetabular impingement (FAI) has gained much attention since its initial description by Ganz et al. [1]. It is nowadays widely accepted as a major risk factor for degenerative hip arthritis. Characterized typically by groin pain it is caused by a pathological contact between the acetabular rim and the femoral head–neck junction, leading to specific cartilage damage [1, 2]. There are two separate mechanisms, the cam and pincer FAI. While these two types can appear separately, most patients present with a combination of both of them. However, more and more attention has been paid towards femoral torsion abnormalities as an additional structural feature of FAI [3]. Increased and decreased femoral torsion are both associated with degeneration of the hip joint [4, 5]. Valgus hips in combination with high antetorsion showed decreased external rotation and predispose to posterior extra-articular FAI as well as to antero-inferior subspine impingement [6]. The combination of increased femoral and acetabular anteversion has been suggested to compromise joint stability causing the femoral head to dislocate laterally and forward during gait [7]. Recent data show evidence for higher incidence of more anterior labral tears in patients with increased femoral antetorsion [8].
Femoral torsion is the twisting of femur between its proximal and distal end. Anatomically torsion is defined by the angle formed by a horizontal plane tangent to the posterior femoral condyles and a plane defined by the center of the femoral head and the axis through the femoral neck [9]. Numerous studies on the measurement of femoral torsion have been published with different methods [10–13]. Depending on the technique and methods significant differences may arise in the same femur [14].
The developmental change of femoral torsion is well documented based on numerous anatomic and clinical studies of infants and adolescents [15–18]. However, the spatial location of femoral twisting remains obscure, mainly because measurements only included an axis or plane through the proximal and distal ends of the femur. Therefore, femoral torsion could occur anywhere between the femoral neck and the femoral condyles: at the intertrochanteric region, the subtrochanteric region or even at both sites. The knowledge where the torsion occurs could be helpful for understanding the pathomechanisms leading to this deformity and also guide the surgeon where best to perform corrective osteotomy. The lesser trochanter (LT) is a distinct landmark between the distal and proximal femur. Its position follows a linear correlation with femoral antetorsion (FT) [19]. FT therefore can be subdivided into torsion that occurs above and below the LT.
The goal of the present study was to narrow down the anatomic site of deformity using LT as an additional landmark.
MATERIALS AND METHODS
Between 2010 and 2013, 146 patients (292 femora) underwent lower extremity rotational assessment with computer tomography (CT). Most common indications were gait disturbances, hip pain, patellar instability or post-operative follow-up. Extremities with ipsilateral fracture, arthroplasty or gross deformities were excluded from the study. Additional exclusion criteria were patients under 18 years as well as insufficient data from CT-scans.
All CT scans were performed by the radiology department of the Luzerner Kantonspital according to institutional protocols for the evaluation of rotational profile of the lower extremities. Patients were placed in the supine position with legs extended and 15° internally rotated. Images were obtained at 1 mm intervals scanning the hip (from the iliac crest down to the LT) and the knee (femoral condyles to proximal tibia) and the ankle (distal tibia to calcaneus). CT was performed with the same device (Somatom Sensation Flash, 2× 128 lines, Somatom Sensation Edge, 128 lines, Siemens AG, Erlangen, Germany) using picture archiving and communication system measurement tools (Phönix Merlin Software 5.0, Phönix PACS GmbH, Freiburg, Germany).
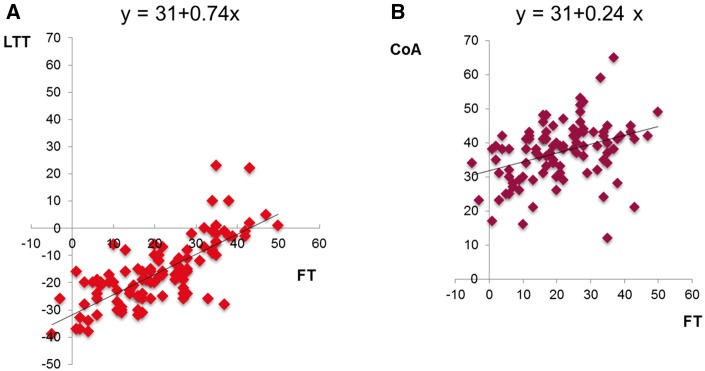
Femoral torsion (FT) and LT torsion (LTT) were measured as described below (Fig. 1). The difference between FT and LTT was calculated combined angle (CoA).
Fig. 1.
CT scans screen shots. Measurement of the left femoral antetorsion. Above section from axial view of base of femoral neck. Yellow circle indicates position of femoral head, yellow line marks femoral neck axis. Below axial view of the knee indicating the plane of the posterior femoral condyles.
Femoral torsion (FT)
Based on Murphy's study the femoral neck axis was determined between the center of the femoral head and the base of the femoral neck to remove any influence of the shape of the femoral neck. Therefore, two transverse (axial) images were required: one at the level of the femoral head center, the other at the base of the neck. Both centers at the head and at the femoral diaphysis at the base of the neck were defined. Both images were merged manually to execute measurements of the femoral neck axis.
To determine the axis of the femoral condyles, a slice through the most posterior aspects of the condyles was selected (Fig. 1).
The degree of femoral torsion was measured as the angle subtended by the femoral neck axis and the posterior bicondylar axis. Positive values represent antetorsion, while negative values describe femoral retrotorsion.
Lesser trochanter torsion (LTT)
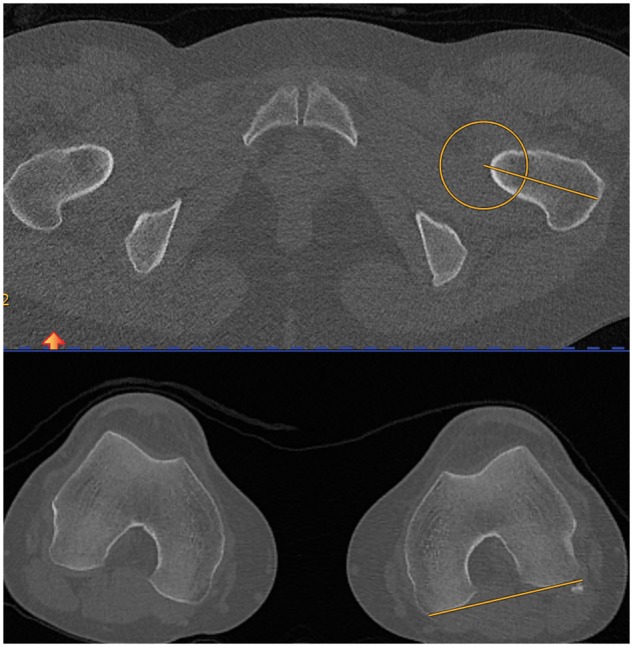
This parameter refers to the orientation of the LT with regard to the femoral shaft. It is measured according to Herzberg by defining an angle between a line bisecting the LT at its thickest cross-section in the middle and the base line of femoral condyles [19] (Fig. 2).
Fig. 2.
Schematic drawing demonstrates the measurement of femoral torsion (FT), lesser trochanter torsion (LTT) and combined angle (CoA). The dotted circle marks the center of the femoral neck axis at its base. Lesser trochanter is indicated by LT. FH, femoral head.
Combined angle (CoA)
This parameter is calculated by the difference between LTT and FT, which represents the angle between both planes. CoA is the angle between LTT and femoral neck axis and indicates supratrochanteric torsion. The LTT is the measure for intertrochanteric torsion. By comparing these two angles to overall FT the location of the torsion can be identified to occur above or below the LT (Fig. 2).
Interobserver variability assessment of both femoral antetorsion and trochanter minor torsion was performed in a randomly selected subset of 35 CT-scanned femora, which were carried out by the first two authors. Calculation has been done via interclass correlation (ICC, 95% limits of agreement).
Statistics
Statistical evaluation of radiologic parameters as well as of associations between femoral antetorsion and age, gender and side was carried out by multiple regression analysis (Software: R Version 3.1.2, R Foundation for Statistical Computing, Vienna, Austria).
The retrospective study is compliant with the ethical guidelines of our institution.
RESULTS
From the total of 292 femora (146) patients, 195 femora were excluded: 43 have had previous arthroplasty (24 hips and 19 knees), 47 were treated with some sort of osteosynthesis, 8 corrective osteotomies. Forty-four patients (88 femora) were under 18 years old, 3 patients (6 femora) exhibited gross deformity of their lower extremities. Three CT scans revealed insufficient data. After exclusion, our study cohort included 97 femora (75 patients, 29 males, 46 females).
Mean age was 41 years (SD 16.9) with a range of 18–85 years.
The mean value for FT was 20° for FT (SD = 12.2, range 1–50) and −16° for LTT (SD = 11.3, range −39 to 23). Mean CoA was 37° (SD 8.7, range 12–65).
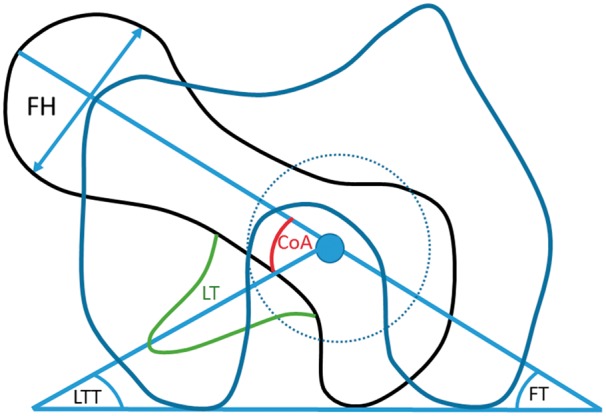
Linear regression analysis showed a linear relationship between FT and LTT (y = 31 + 0.74x) and between FT and CoA (y = 31 + 0.24x) (Fig. 3). The increase of LTT is approximately three times higher than of CoA (0.74 versus 0.24). Multiple regression analysis showed a significant association between FT and gender was observed as men had lower FT angles than women (15° and 24°, respectively, P values <0.001). In addition, an age-related correlation was observed. Older patients had lower FT values, with a decrease of 0.2° per year (P values <0.001). Measurements on left and right revealed no significant asymmetry.
Fig. 3.
Scatterplots below show linear regression analysis indicating a linear relationship between FT and LTT (y = 31 + 0.74x) (A) and between FT and CoA (y = 31 + 0.24x) (B). The increase of LTT is approximately three times higher than of CoA (0.74 versus 0.24).
Interobserver reliability was determined by ICC, which demonstrated a high amount of consistency between both observers: 0.92 for FT (CI 0.85; 0.96) and 0.92 for LT (CI 0.84; 0.96).
DISCUSSION
Femoral rotational malalignment is associated with pain and functional disability and may be a contributing factor to hip impingement as well as to instability [20].
Amidst general agreement about the influence of abnormal torsion on hip biomechanics, the anatomic location of the deformity is debated. This is mainly because current techniques of measuring femoral torsion measure the angle between the bicondylar plane and the femoral neck axis plane at the two extremes of the femur. This results in an overall torsion angle, which does not allow to allocate the location of the deformity. The position of the LT with respect to FT and CoA is a landmark to determine the location of the deformity. Our study shows, that both LTT and CoA show a linear correlation to FT. The increase of the LTT is three times higher than the increase of CoA. This indicates that with increasing FT, both torsion below and above the LT increase, but three times more at the subtrochanteric level.
Herzberg was the first to measure the LTT. His values are identical to the ones of this study and confirm a linear correlation between the position of the LT relative to the femur axis and the femoral antetorsion [19].
A recent study proposed a new method of measuring femoral rotation by adding a third axis, the intertrochanteric axis between the greater and the LT [21]. Using that technique, the authors were able to demonstrate that in high femoral torsion, the increase of femoral torsion was both above and below the LT and similar to our study, it was found that the torsion below the LT increased more than above. Another study in dysplastic hips showed that the deformity was between the isthmus of the femur and the LT [22].
Normal values of femoral torsion and he range of deviation may guide the surgeon in decision making and also help to identify the amount of correction that is needed. However, there is a wide range of mean values of femoral torsion, ranging from +9° to +31° [23–32]. This might be due to different imaging modalities (radiographs, CT, MRI) used to measure femoral antetorsion, but also due to different techniques of measuring antetorsion angle. The average femoral antetorsion in this present study is 20° (SD = 12.2), which is rather high. This may be explained by a selection bias of patients, where imaging was carried out for suspicion of abnormal femoral torsion and the method we used to define femoral antetorsion using the method of Murphy [26]. Murphy’s method, which was validated to replicate anatomic measurements, gives higher values than other measuring techniques [14, 33]. Considering possible relevant anatomic anomalies such as cam deformity that might distort the shape of the femoral neck, the advantage of Murphy’s method is that it is based on two planes, the femoral head and the base of the neck, which are unaffected by such deformities.
A relationship between demographic factors such as age and sex and femoral torsion is still debated. Decker found a significant negative correlation of age and antetorsion in women under the age of 20, whereas no correlation was shown between antetorsion and age for men and older women [28]. Similar findings support a sex-related correlation more recently [27]. Other studies could not establish any correlation between femoral antetorsion and patient demographics [8]. This study is consistent with above mentioned gender and age relationship. Results obtained from our population revealed higher femoral torsion angles for women and a decreasing age-dependent tendency. Finally, our data are completely indifferent regarding side differences.
Various surgical options for rotational osteotomies have been established, including the complete femur with three preferred locations: subtrochanteric, intertrochanteric and supracondylar. All results are reported to be similar [4, 34–38]. Selection method between these approaches are usually based on perioperative risks, healing tendencies, operation time, additional procedures that can possibly be combined with and the surgeon's preference among others. However, the location of the rotational deformity is usually neglected during decision-making. In general, rotational deformities of the femur are surgically addressed by derotational osteotomies. As a rule skeletal deformities are corrected at the alleged site of deformation. Thus, axial deviation is treated most effectively and muscle balances are left maximally unaffected.
Therefore, our results speak in favor of a subtrochanteric osteotomy. Which technique eventually is applied is of secondary interest. We prefer a lateral approach to the proximal femur with plating of the osteotomy, because it bears some advantages. Hardware application below the greater trochanter avoids interference with other procedures and can easily be combined with additional procedures such as surgical hip dislocation, hip arthroscopy etc. Subtrochanteric plating is associated with less greater trochanter pain and bursitis when compared with the intertrochanteric approach requiring a blade plate [39]. Also damage to the abductors cannot be underestimated in antegrade nailing with reduction in abduction strength and endurance, as well as functional impairment [40].
This study has a number of limitations. First, it is a radiological study and not a clinical one. Hence clinical aspects of anatomical deformities were not taken into account.
The second limitation is the study population, which is comprised of a pre-selected patient population which was referred to CT evaluation for various reasons. Hence, application of our findings to an asymptomatic population might be underpowered. However, a normal distribution could be documented suggesting representable values of the normal population.
In conclusion, this study identifies the LT as a reliable landmark and shows a strong linear relationship between the orientation of the LT and the overall torsion of the femur below and above the LT with about two thirds of torsional changes occurring distal to it. Therefore, our data provide a considerable indication for a subtrochanteric osteotomy to address correction of femoral rotational deformity at its anatomical origin.
ETHICAL APPROVAL
Our study involves human data, but the study does not require approval in our country. It is compliant with the ethical guidelines of our institution.
ACKNOWLEDGEMENTS
We thank Thomas Kaufmann, MD for his help with statistical analysis.
FUNDING
Relevant financial activities outside the submitted work (Mathys Ltd). There was no funding received to conduct and complete this study.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Ganz R, Parvizi J, Beck M. et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417:112–20. [DOI] [PubMed] [Google Scholar]
- 2. Beck M, Kalhor M, Leunig M. et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87:1012–8. [DOI] [PubMed] [Google Scholar]
- 3. Ricciardi BF, Fabricant PD, Fields KG. et al. What are the demographic and radiographic characteristics of patients with symptomatic extraarticular femoroacetabular impingement? Clin Orthop Relat Res 2015; 473:1299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reikeras O, Hoiseth A.. Femoral neck angles in osteoarthritis of the hip. Acta Orthop Scand 1982; 53:781–4. [DOI] [PubMed] [Google Scholar]
- 5. Tonnis D, Heinecke A.. Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritis. J Pediatr Orthop 1991; 11:419–31. [DOI] [PubMed] [Google Scholar]
- 6. Siebenrock KA, Steppacher SD, Haefeli PC. et al. Valgus hip with high antetorsion causes pain through posterior extraarticular FAI. Clin Orthop Relat Res 2013; 471:3774–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reikeras O, Bjerkreim I, Kolbenstvedt A.. Anteversion of the acetabulum in patients with idiopathic increased anteversion of the femoral neck. Acta Orthop Scand 1982; 53:847–52. [DOI] [PubMed] [Google Scholar]
- 8. Ejnisman L, Philippon MJ, Lertwanich P. et al. Relationship between femoral anteversion and findings in hips with femoroacetabular impingement. Orthopedics 2013; 36:e293–300. [DOI] [PubMed] [Google Scholar]
- 9. Billing L. Roentgen examination of the proximal femur end in children and adolescents; a standardized technique also suitable for determination of the collum-, anteversion-, and epiphyseal angles; a study of slipped epiphysis and coxa plana. Acta Radiol Suppl 1954; 110:1–80. [PubMed] [Google Scholar]
- 10. Abel MF, Sutherland DH, Wenger DR. et al. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop 1994; 14:48–53. [DOI] [PubMed] [Google Scholar]
- 11. Anda S, Terjesen T, Kvistad KA. et al. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr 1991; 15:115–20. [DOI] [PubMed] [Google Scholar]
- 12. Browning WH, Rosenkrantz H, Tarquinio T.. Computed tomography in congenital hip dislocation. The role of acetabular anteversion. J Bone Joint Surg Am 1982; 64:27–31. [PubMed] [Google Scholar]
- 13. Chevrot A, Hazebroucq V, Vallee C. et al. A criterion of validity of the X-ray computed tomographic measurement of femoral neck anteversion. Rev Chir Orthop Reparatrice Appar Mot 1991; 77:370–3. [PubMed] [Google Scholar]
- 14. Berryman F, Pynsent P, McBryde C.. A semi-automated method for measuring femoral shape to derive version and its comparison with existing methods. Int J Numer Method Biomed Eng 2014; 30:1314–25. [DOI] [PubMed] [Google Scholar]
- 15. Hamacher P, Roesler H.. Weightbearing diagrams in disorders of the hip (author's transl). Z Orthop Ihre Grenzgeb 1974; 112:176–86. [PubMed] [Google Scholar]
- 16. Pitkow RB. External rotation contracture of the extended hip. A common phenomenon of infancy obscuring femoral neck anteversion and the most frequent cause of out-toeing gait in children. Clin Orthop Relat Res 1975; 110:139–45. [PubMed] [Google Scholar]
- 17. Watanabe RS. Embryology of the human hip. Clin Orthop Relat Res 1974; 98:8–26. [DOI] [PubMed] [Google Scholar]
- 18. Zippel H. Etiologic problems in congenital hip dislocation with special reference to cytogenetic examination. 2. Beitr Orthop Traumatol 1971; 18:541–60. [PubMed] [Google Scholar]
- 19. Herzberg W, Meitz R, Halata Z.. Antetorsion of the femur neck. A variable of the trochanter minor?. Unfallchirurg 1991; 94:168–71. [PubMed] [Google Scholar]
- 20. Bedi A, Dolan M, Leunig M. et al. Static and dynamic mechanical causes of hip pain. Arthroscopy 2011; 27:235–51. [DOI] [PubMed] [Google Scholar]
- 21. Kim HY, Lee SK, Lee NK. et al. An anatomical measurement of medial femoral torsion. J Pediatr Orthop B 2012; 21:552–7. [DOI] [PubMed] [Google Scholar]
- 22. Noble PC, Kamaric E, Sugano N. et al. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res, 2003; 27–40. [PubMed] [Google Scholar]
- 23. Toogood PA, Skalak A, Cooperman DR.. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 2009; 467:876–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Prasad R, Vettivel S, Isaac B. et al. Angle of torsion of the femur and its correlates. Clin Anat 1996; 9:109–17. [DOI] [PubMed] [Google Scholar]
- 25. Reikeras O, Hoiseth A, Reigstad A. et al. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand 1982; 53:775–9. [DOI] [PubMed] [Google Scholar]
- 26. Murphy SB, Simon SR, Kijewski PK. et al. Femoral anteversion. J Bone Joint Surg Am 1987; 69:1169–76. [PubMed] [Google Scholar]
- 27. Sutter R, Dietrich TJ, Zingg PO. et al. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology 2012; 263:475–83. [DOI] [PubMed] [Google Scholar]
- 28. Decker S, Suero EM, Hawi N. et al. The physiological range of femoral antetorsion. Skeletal Radiol 2013; 42:1501–5. [DOI] [PubMed] [Google Scholar]
- 29. Akiyama M, Nakashima Y, Fujii M. et al. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol 2012; 41:1411–8. [DOI] [PubMed] [Google Scholar]
- 30. Atkinson HD, Johal KS, Willis-Owen C. et al. Differences in hip morphology between the sexes in patients undergoing hip resurfacing. J Orthop Surg Res 2010; 5:76.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nakahara I, Takao M, Sakai T. et al. Gender differences in 3D morphology and bony impingement of human hips. J Orthop Res 2011; 29:333–9. [DOI] [PubMed] [Google Scholar]
- 32. Tibor LM, Liebert G, Sutter R. et al. Two or more impingement and/or instability deformities are often present in patients with hip pain. Clin Orthop Relat Res 2013; 471:3762–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schneider B, Laubenberger J, Jemlich S. et al. Measurement of femoral antetorsion and tibial torsion by magnetic resonance imaging. Br J Radiol 1997; 70:575–9. [DOI] [PubMed] [Google Scholar]
- 34. Gordon JE, Pappademos PC, Schoenecker PL. et al. Diaphyseal derotational osteotomy with intramedullary fixation for correction of excessive femoral anteversion in children. J Pediatr Orthop 2005; 25:548–53. [DOI] [PubMed] [Google Scholar]
- 35. Hamdy RC, Ehrlich MG.. Subtrochanteric derotation osteotomy of the femur using three or four wires. A technical note. Clin Orthop Relat Res 1994; 302:111–4. [PubMed] [Google Scholar]
- 36. Hau R, Dickens DR, Nattrass GR. et al. Which implant for proximal femoral osteotomy in children? A comparison of the AO (ASIF) 90 degree fixed-angle blade plate and the Richards intermediate hip screw. J Pediatr Orthop 2000; 20:336–43. [PubMed] [Google Scholar]
- 37. Hoffer MM, Prietto C, Koffman M.. Supracondylar derotational osteotomy of the femur for internal rotation of the thigh in the cerebral palsied child. J Bone Joint Surg Am 1981; 63:389–93. [PubMed] [Google Scholar]
- 38. Staheli LT. Torsion–treatment indications. Clin Orthop Relat Res 1989; 847:61–6. [PubMed] [Google Scholar]
- 39. Kamath A. Subtrochanteric osteotomy for femoral mal-torsion through a surgical dislocation approach. J Hip Preserv Surg Adv Access 2015; 2(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ansari Moein CM, Ten Duis HJ, Oey PL. et al. Intramedullary femoral nailing through the trochanteric fossa versus greater trochanter tip: a randomized controlled study with in-depth functional outcome results. Eur J Trauma Emerg Surg 2011; 37: 615–22. [DOI] [PubMed] [Google Scholar]