Abstract
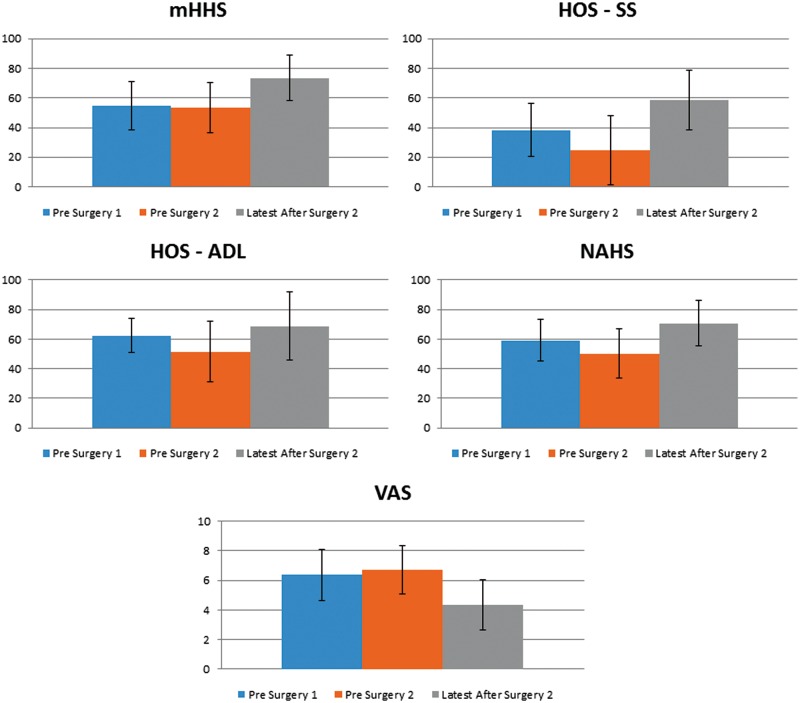
This study reviewed pain and outcome scores of patients undergoing revision surgery with heterotopic ossification (HO) excision following previous hip arthroscopy. The aim was to determine if performing the excision arthroscopically improved clinical outcomes. Data were prospectively collected and retrospectively reviewed in patients who had HO removed arthroscopically between February 2008 and 2014. Four patient-reported outcome (PRO) measures were collected: Modified Harris Hip Score (mHHS), Non-Arthritis Hip Score (NAHS), Hip Outcome Score-Activity of Daily Living (HOS-ADL) and Sport-Specific (HOS-SS) subscales. Minimum 1.5 year follow-up from index procedure was available for 23 patients (mean age = 38.6 years). Of the 23 patients who had revision surgery and HO removal, 19 (83%) were available for follow-up. Prior to revision, the average mHHS was 53.4, HOS-ADL 51.4, HOS-SS 24.5, NAHS 50.3 and VAS 6.7. Following revision with HO excision, each score had improved with an average mHHS of 73.62, HOS-ADL of 68.88, HOS SS of 58.51, NAHS of 70.83 and VAS of 4.33. Overall, mHHS increased by 20.26 points (P < 0.001), HOS-ADL increased by 17.48 points (P = 0.023), HOS-SS increased by 34.03 points (P < 0.001), NAHS increased by 20.55 points (P = 0.001) and VAS decreased by 2.38 points (P < 0.001). Patients undergoing revision hip surgery with HO excision demonstrated improved outcome scores and pain resolution; however, few patients achieved a good or excellent result. Revision hip surgery with HO excision should be approached cautiously because of the modest results in this patient group.
INTRODUCTION
Heterotopic ossification (HO) is a known complication after hip arthroscopy, and its incidence has been reported in up to 44% of individuals who were not prescribed prophylactic therapy [1]. This osteogenic response is not unique to hip arthroscopy; HO can be caused by soft tissue trauma, traumatic nervous system injury, or a genetic disorder, but it is a common complication following major hip surgery [2, 3]. Although it has not been demonstrated statistically, risk factors for HO development after hip arthroscopy include arthroscopic osteoplasty with capsular cut in male patients [4]. Although the underlying molecular mechanisms have not been fully elucidated, recent studies implicate an inflammatory cascade initiated by bone morphogenic proteins, and this cascade ultimately results in local tissue conditions that are optimal for formation, vascularization and innervation of heterotopic bone from locally derived stem cells [5, 6]. Methods to reduce HO following hip surgery have historically involved post-operative radiation or chemoprophylaxis with nonsteroidal anti-inflammatory drugs [4]. Beckmann et al. [7] found that giving patients chemoprophylaxis therapy in the form of naproxen twice daily for 3 weeks reduced the incidence of HO from 25 to 5.6%. This group also noted the highest rates of HO were seen in patients who had undergone combined acetabuloplasty and femoral osteochondroplasty arthroscopically. Bedi et al. [4] found rates of HO decrease from 8.3 to 1.8% when NSAID prophylaxis therapy was administered to their patients. Despite effective chemoprophylaxis therapy, HO still occurs in a small percentage of patients. Although HO is frequently recognized radiographically in the post-operative period, it is unclear whether HO is clinically relevant. Rath et al. [1] found no difference in functional outcomes when comparing those who developed HO and those who did not develop HO after hip arthroscopy. However, the study was underpowered to definitively make this conclusion. Our group has noted statistically significant improvement after revision hip arthroscopy [8]. When a patient has persistent hip pain following hip arthroscopy and HO, it can be difficult to counsel the patient. The clinical consequences of HO are debatable, and little is known about the prognosis of revision hip arthroscopy with HO excision. This study reviewed pain and outcome scores of patients undergoing revision surgery with HO excision and aimed to determine if surgical intervention improved clinical outcomes.
MATERIALS AND METHODS
This study was approved by our local institutional review board. Data were prospectively collected on all patients treated with hip arthroscopy between February 2008 and 2014. We retrospectively reviewed 2379 arthroscopic hip surgeries and identified patients who underwent revision hip arthroscopy with removal of HO or a loose body. We are unable to determine the primary reason for revision surgery from our database; we included only patients with HO that were excised at the time of arthroscopy. The index procedure was performed by the senior surgeon in all cases. Two reviewers evaluated all radiographs to include only patients who underwent removal of HO that was one centimeter (cm) or greater in one dimension on either the anteroposterior pelvis or false profile radiograph (Fig. 1). Sixty-eight patients were identified in our database and 23 of those patients had HO excision that was > 1 cm. A retrospective chart review was then performed to ensure the indication for revision surgery was consistent with second-look arthroscopy with HO excision or open HO excision surgery. Exclusion criteria were revisions with HO < 1 cm in size, and patients who had previous hip conditions such as Legg Calves-Perthes disease, avascular necrosis, and or dysplasia. All patients were assessed before and after their primary and revision surgeries using four patient-reported outcome (PRO) measures: the modified Harris Hip Score (mHHS), the Non-Arthritic Hip Score (NAHS), the Hip Outcome Score-Activity of Daily Living (HOS-ADL) and the Sport-Specific (HOS-SS) subscales. To estimate pain intensity, patients were asked to rate their pain on a visual analogue scale (VAS), where 0 was no pain, and 10 was intense pain. Patients were also asked to identify their satisfaction with their surgical results on a scale from 1 to 10, where 1 was not satisfied and 10 was extremely satisfied. Objective data such as sex, height, weight and body mass index were also collected. Follow-up data included conversion to total hip arthroplasty (THA) or revision hip arthroscopy. Dates of the index and revision surgeries were collected. All patients undergoing revision surgery had persistent hip pain following primary hip arthroscopy that did not respond to at least 3 months of non-operative treatment, including at least six weeks of physical therapy Non-operative treatment included activity modification, oral anti-inflammatory medication and other therapeutic modalities such as ultrasound and massage techniques.
Fig. 1.
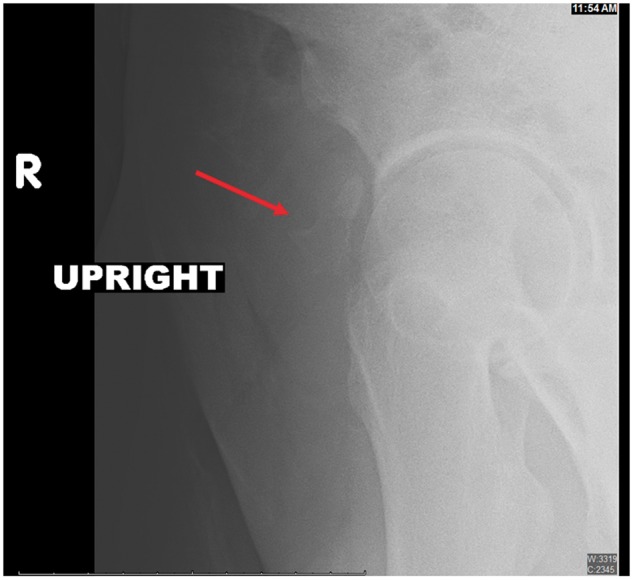
False-profile of a patient view documenting HO.
SURGICAL TECHNIQUE
All surgical procedures were performed by the senior surgeon while the patients were in the supine position. Diagnostic arthroscopy was first performed to check for loose bodies, chondral defects, labral tears, synovitis, ligamentum teres tears and additional intra-articular pathologies. Possible pain generators were identified and treated at the time of revision surgery, and all concomitant procedures were recorded. The labrum was evaluated and treated with repair or debridement if necessary. HO was identified arthroscopically and fluoroscopically. Electrocautery was used to remove fibrous tissue from the HO. In some cases the HO was osteotomized to allow removal through the arthroscopic portals. In two cases, the HO was too large to be removed arthroscopically, and the Smith Peterson approach was utilized for HO excision. All patients received 325 milligram aspirin twice daily for HO prophylaxis post-operatively for 6 weeks. Patients followed the same post-operative hip arthroscopy protocol that we utilize for primary hip arthroscopy. Patients are treated with toe-touch weight bearing for 2 weeks and wore a hip abduction orthosis for 2 weeks. All patients started an early range of motion program with a therapist. Patients undergoing labral reconstruction were treated toe-touch weight bearing for 6 weeks and wore a hip abduction orthosis for 6 weeks.
STATISTICS
The two-tailed, paired t-test was used to assess changes in preoperative and post-operative scores. An mHHS of 80 or better is often used to note good or excellent results [9, 10], and we calculated the number of patients who had an mHHS > 80 after revision surgery. A P values of < 0.05 was considered significant. Statistical analysis was completed using Microsoft Office Excel 2007 (Redmond, Washington, USA).
RESULTS
Of the 23 patients who had revision surgery and HO removal, 19 (83%) were available for follow-up. The average time from index procedure to revision with HO excision was 1.42 years (range, 0.3–4.14). All patients were evaluated radiographically, all patients were grade I in the Brooker classification and the HO was found on the anterolateral labral tissue. Three patients (16%) required conversion to THA, and one (5%) patient underwent a second revision at an outside facility. The remaining fifteen patients were available for follow-up. Patient demographics are displayed in Table I. Prior to their index surgery, the patients had an average mHHS of 54.7 [range, 12–86] HOS-ADL of 62.5 [range, 46–85], HOS-SS of 38.3 [range, 11–75], NAHS of 59.3 [range, 11–75] and VAS of 6.4 [range, 4–10]. Prior to the revision procedure, each of these scores had declined, with the exception of the VAS, which increased. Prior to revision surgery with HO excision, the patients had an average mHHS of 53.4, HOS-ADL of 51.4, HOS-SS of 24.5, NAHS of 50.3, and VAS of 6.7. This data are presented in Table II. Following revision surgery and HO excision each score had significantly improved, with an average mHHS of 73.62 [range, 49–100], HOS-ADL of 68.88 [range, 12–100], HOS-SS of 58.51 [range, 25–100], NAHS of 70.83 [41–96] and VAS of 4.33 [range, 1–8] (Table II and Fig. 2). Concomitant procedures performed at the time of the second-look arthroscopy are shown in Table III. When evaluating the scores from before and after revision, mHHS increased by 20.26 points (P = 0.001), HOS-ADL increased by 17.8 points (P = 0.023), HOS-SS increased by 34.03 points (P < 0.001), NAHS increased by 20.55 points (P = 0.001) and VAS decreased by 2.38 points (P = 0.001). Looking at individual patients, the majority had improvement in each category from before to after revision. Two of the fifteen patients (13%) had a decrease in their Harris Hip Scores, two (13%) had a decrease in their HOS-ADL, four (27%) had no change in their VAS and one (7%) had an increase in their VAS at their most recent follow-up. Satisfaction scores varied from 0 to 10 with an average of 7.6. Only, 3 of the 15 (20%) patients had a follow-up mHHS > 80 points.
Table I.
Cohort demographic information, including gender, laterality, age, follow-up time and revision information
| Demographics | |
|---|---|
| Count | 23 |
| Follow-up | 15 |
| THR | 3 |
| Outside revision | 1 |
| Opted out of study | 2 |
| Lost to follow-up | 2 |
| Follow-up % | 82.61% |
| HO to latest follow-up | 1.52 |
| Original surgery to latest follow-up | 2.73 |
| Initial surgery to HO | 1.42 |
| Gender | |
| Male | 10 |
| Female | 13 |
| Laterality | |
| Left | 12 |
| Right | 11 |
| Age | 38.6 |
Table II.
Pre- and post-operative 254 PRO scores for the mHHS, the HOS-ADL, the HOS-SS subscales, the NAHS, VAS and the satisfaction with t-tests between groups
| Score reporting | ||||||
|---|---|---|---|---|---|---|
| mHHS | HOS ADLS | HOS SSS | NAHS | VAS | Satisfaction | |
| Pre-primary | 54.71 | 62.51 | 38.27 | 59.28 | 6.37 | |
| Pre HO excision | 53.36 | 51.38 | 24.48 | 50.28 | 6.71 | |
| Lastest post-operative follow-up | 73.62 | 68.88 | 58.51 | 70.83 | 4.33 | 7.60 |
| T-Test | |||||
|---|---|---|---|---|---|
| mHHS | HOS ADLS | HOS SSS | NAHS | VAS | |
| Pre-primary to latest | 0.002 | 0.312 | 0.004 | 0.030 | 0.002 |
| Pre-primary to pre-HO excision | 0.800 | 0.048 | 0.051 | 0.078 | 0.518 |
| Pre-HO excision to latest | 0.001 | 0.023 | 0.000 | 0.001 | 0.000 |
Fig. 2.
Pre- and post-operative PRO scores for the mHHS, the HOS-ADL, the HOS-SS subscales and the NAHS and VAS with associated SDs.
Table III.
Concomitant procedures for the primary and revision surgeries
| Primary surgery procedures | |
|---|---|
| Femoral osteoplasty | 17 |
| Acetabuloplasty | 16 |
| Iliopsoas release | 4 |
| Removal of loose body | 3 |
| Trochanteric bursectomy | 2 |
| Labral treatment | |
| Base refixation | 4 |
| Debridement | 6 |
| Reconstruction | 1 |
| Simple Stitch | 8 |
| HO excision surgical procedures | |
|---|---|
| Femoroplasty | 6 |
| Chondroplasty | 5 |
| Acetabuloplasty | 4 |
| Iliopsoas release | 3 |
| Osteoplasty (peripheral) | 2 |
| Debridement of trochanteric bursitis | 1 |
| Iliotibial band release | 1 |
| Microfracture—acetabulum | 1 |
| Labral treatment | |
| Base refixation | 0 |
| Debridement | 13 |
| Reconstruction | 0 |
| Simple stitch | 0 |
DISCUSSION
In this cohort of patients undergoing second look arthroscopy and HO excision the clinical results were fair. There was a 21% rate of conversion to THA or subsequent revision. The remaining patients demonstrated significantly improved pain and functional outcome scores, but only three patients achieved a good or excellent result as measured by the mHHS. HO is recognized as a common complication following hip arthroscopy [7]. Rath et al. [1] found that 44% of their study cohort developed radiographically evident HO. None of those patients went on to reoperation for HO removal. Additionally, changes in mHHS, VAS, and HOS scores between those who developed HO and those that did not were not significantly different at follow-up, indicating that most cases of HO development after hip arthroscopy may not be clinically significant. However, previous studies from our institution looking at revision hip arthoscopy found that presence of HO was a predictor of decreased PROs, especially in the NAHS [8]. Features that predispose patients to the development of HO following a THA include male gender, bilateral hypertrophic osteoarthritis, a history of HO, ankylosing sponydlitis, diffuse idiopathic skeletal hyperostosis and Paget’s disease [1]. Characteristics that may predispose patients to the development of HO following hip arthroscopy include acetabuloplasties with osteochondropalsties for mixed-type FAI and a large amount of bone resection [7]. Arthroscopic procedures that require capsuolotomy or capsulectomy may also predispose patients to the formation of HO, but this has not been specifically studied [7, 11]. In our cohort, 43% of patients were men; 74% had femoral osteoplasty; 70% had acetabuloplaty and 83% had some type of labral debridement or repair. However, the prevalence of these characteristics compared to number of patients who did not develop clinically significant HO was not analysed in our data set, and conclusions cannot be drawn from this study.
Although a few studies have looked at the incidence of HO following hip arthroscopy and the effect of chemoprophylaxis therapy on this population, none have looked at excision following the formation of ectopic bone. Functional outcomes following the excision of HO following THA has previously been investigated in [12, 13]. They examined range of motion as well as pain and functional outcome scores and concluded that excision of HO reliably improves range of motion, but it does not improve functional outcomes as much as range of motion. Although satisfaction in this patient population was high, the authors concluded that pain should not be a primary indication for excision of HO [12, 13]. We argue that HO secondary to arthroscopic management of hip disorders is different than that found in the arthroplasty and trauma population. Range of motion is typically not a factor in these arthroscopic cases, but pain is typically an indication for workup and treatment. In cases of Brooker grades III and IV the decision to proceed with revision may be easy due to decreased range of motion and stiffness; however, in our experience, the vast majority of HO following hip arthroscopy is Brooker grade I or II.
The focus of this study was to look at functional outcome scores following excision of painful HO after hip arthroscopy, which has not previously been evaluated. Our data indicate that the majority of patients will receive some pain relief (35%) from revision surgery with HO excision. PROs improved in all categories, but the improvements were modest. For example, mHHS had a 20-point improvement, but the final average score remained in the ‘fair’ range. Average satisfaction scores following revision were high. Functional outcome scores improved for most patients, but for two patients, the functional outcome score decreased. The greatest improvement in functional outcomes scores was in HOS-ADL, although this was not statistically significant. VAS scores likewise improved in a majority of patients, but none of the patients were completely pain free, and the average VAS score at follow-up was 4 (range, 1–8). Given these modest improvements following excision of painful HO, careful patient selection and pre-operative counselling is recommended, and this operation should be performed with caution.
There are several limitations to this study. The sample size is small, and the scores included are not from uniform time intervals among patients. An improvement in this study would be to identify a matched, cohort of individuals with HO but that did not opt for revision surgery. This was not obtainable by our database, despite the large number of arthroscopic cases. Additionally, while each patient included in this study had an HO excision, many underwent additional surgical procedures to treat other possible pain generators. Last, more objective measures, such as the results of range of motion tests after HO excision, are not available for all patients and therefore were not included in this study. The inclusion of the results from range of motion tests before and after excision would provide valuable additional information.
CONCLUSIONS
Patients undergoing revision hip surgery with HO excision in addition to treatment of concomitant hip pathology demonstrated improvement in outcome and pain scores; however, few patients achieved a good or excellent result. Heterotopic ossificiation prophylaxis is highly recommended during primary intervention. Revision hip surgery with HO excision should be approached cautiously because of the modest results in this patient group.
FUNDING
This study was performed at the American Hip Institute. This study was approved by the Institutional Review Board (IRB ID: 5276)
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Rath E, Sherman H, Sampsom TG. et al. The Incidence of heterotopic ossification in hip arthroscopy. Arthroscopy 2013; 29: 427–33. [DOI] [PubMed] [Google Scholar]
- 2. Neal B, Harley G, MacMahon S. et al. Incidence of Heterotopic Bone Formation after Major Hip Surgery. ANZ J. Surg 2002; 72:808–21. [DOI] [PubMed] [Google Scholar]
- 3. Kaplan FS, Glaser DL, Hebela N. et al. Heterotopic Ossification. jaaos 2004; 12:116–25. [DOI] [PubMed] [Google Scholar]
- 4. Bedi A, Zbeda RM, Bueno VF. et al. The Incidence of Hetertopic Ossification After Hip Arthroscopy. Am J Sports Med 2012; 40:854–63. [DOI] [PubMed] [Google Scholar]
- 5. Reichel LM, Salisbury E, Moustoukas MJ. et al. Molecular mechanisms of heterotopic ossification. J Hand Surg Am 2014; 39: 563–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rodenberg E, Azhdarinaia A, Lazard Z. et al. Matrix metalloproteinase-9 is a Diagnostic marker of heterotopic ossification in a murine model. Tissue Eng 2011; 17: 2487–96. [DOI] [PubMed] [Google Scholar]
- 7. Beckmann JT, Wylie JD, Kapron AL. et al. The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med 2014; 42: 1359–64. [DOI] [PubMed] [Google Scholar]
- 8. Domb BG, Stake CE, Lindner D. et al. Revision Hip Preservation Surgery With Hip Arthroscopy: Clinical Outcomes. Arthroscopy 2014; 30:581–87. [DOI] [PubMed] [Google Scholar]
- 9. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone and Joint 1969; 51: 737–55. [PubMed] [Google Scholar]
- 10. Byrd JW, Jones KS.. Prospective analysis of hip arthroscopy with 2 year follow-up. Arthroscopy 2000; 16: 578–87. [DOI] [PubMed] [Google Scholar]
- 11. Randelli F, Pierannunzii L, Banci L. et al. Heterotopic ossifications after arthroscopic management of FAI: the role of NSAID prophylaxis. J Orthopaed Traumatol 2010; 11: 245–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cobb TK, Berry DJ, Wallrichs SL. et al. Functional outcome of excision of heterotopic ossification after THA. Clin Orthop Relat Res 1999; 361: 131–9. [DOI] [PubMed] [Google Scholar]
- 13. Vasileiadis GI, Amantaullah DF, Crenshaw JR.. Effect of Heterotopic Ossification on Hip Range of Motion and Clinical Outcome. J Arthroplasty 2015; 30: 461–4. [DOI] [PubMed] [Google Scholar]