Abstract
The purpose of this randomized prospective comparative controlled pilot study was to determine whether specific patient exercises done pre-hip arthroscopy surgery for femoro-acetabular impingement affected post-operative recovery. Between October 2013 and June 2014, 6 males and twelve females over the age of eighteen, who were listed for hip arthroscopy for femoro-acetabular impingement, were randomized into two groups. A hip-specific, 8-week home exercise programme was given to the experimental group before their surgery. The control group was given no instruction on exercise before surgery. All participants followed the same rehabilitation programme after surgery. Outcome measures were assessed at set time intervals. Hand held dynamometry was used to assess muscle strength, and the EQ-5D-5 L Score and the Non-Arthritic Hip Score were utilized. Sixteen participants completed the study (eight controls: mean age 41.75 years and eight intervention: mean age 37.5 years). A mixed ANCOVA analysis compared the treatment groups taking baseline values into account. A statistically significant difference was found between the treatment groups for knee extension strength on both operative (P = 0.05) and non-operative sides (P = 0.002), hip flexor strength operative side (P = 0.02) and for EQ-5D-5 L health (P = 0.03), in favour of the intervention group. There was no significant difference between the treatment groups for the other measures, although some tended towards significance. This small pilot study has been designed to aid the further research and the differences between the groups found in these results may inform future larger scale studies.
INTRODUCTION
Over the last decade there has been a rapid evolution in both diagnostic capabilities and surgical technology concerning the hip joint [1, 2]. Hip arthroscopy, used less commonly in the 1980s [2], is now being used progressively in the management of femoro-acetabular impingement, with rising numbers anticipated [3–5]. Physiotherapeutic management should therefore be reviewed in light of advances in the understanding of hip pathology, and its surrounding interventions [1].
To our knowledge, there have been no prospective studies looking at the effect of exercises in preparation for hip arthroscopy surgery. A search of the literature identified one study retrospectively analysing the benefit of pre-habilitation exercises in hip arthroscopy surgery patients [6]. Comparison studies looking at exercises before surgery with hip replacement subjects have recounted some positive conclusions but are analysing different, much older, less active patient groups [7–9]. Investigators looking at the conservative management of FAI with exercises and activity modification report there is suggestion that this may be beneficial in some, but have recommended that more extensive evaluation is required to ascertain these preliminary findings [10]. Experts in the field recommended that before elective surgery, patients should fail conservative treatment [11]. It is important that patients are engaged in an appropriate pre-habilitation routine to ensure they have exhausted all possible options to resolve their pain before deciding on surgical intervention. The pre-operative period is an opportunity to assess a patient’s pain, joint range of motion, muscle strength, other joint involvement, gait pattern, neuro-muscular movement control, expectations regarding surgery and to educate on their individual hip pathology, planned surgery and the rehabilitation journey.
A prospective randomized controlled trial was therefore designed, aiming to compare two groups of subjects having hip arthroscopy surgery where one group receives pre-habilitation exercises before surgery and the other group does not. Our hypothesis was that pre-habilitation exercises would improve patient reported outcome measure scores and muscle power post-operatively.
MATERIALS AND METHODS
Design
It was proposed that a prospective randomized controlled comparative pilot study was the most appropriate method of addressing the hypothesis within the time restraints of a Masters Degree programme. These time restraints also influenced the number of subjects that could be recruited for this pilot, thus it was not appropriate to perform a sample size calculation. The study was conducted in a private physiotherapy clinic setting during the period of October 2013 to June 2014. The Participant Identification Centre (PIC) was located at a National Health Service (NHS) Foundation Trust hospital, where a sole consultant orthopaedic surgeon specialist in the diagnosis and treatment of FAI and labral pathology, identified subjects meeting the study’s inclusion and exclusion criteria. The chartered physiotherapist involved in applying the intervention had over 20 years post-graduate experience in physiotherapy and post-graduate qualifications in musculoskeletal medicine. Outcomes were assessed in the intervention and control groups at baseline (8 weeks before surgery), and then at 1 week before surgery and at 2, 6 and 12 weeks post-surgery by an independent blinded chartered physiotherapist trained in the use of the study outcome measures.
Ethics
The involved University Health Ethics Committee, NHS Foundation Trust Hospital Research and Development Department, and the National Research Ethics Service (NRES) approved the study in September 2013 (IRAS ID 129236). The HAPI study was consequently recorded with the International Clinical Trials Registry database, International Standard Randomized Trial Number (ISRCTN) 13779749 (2013).
Participants
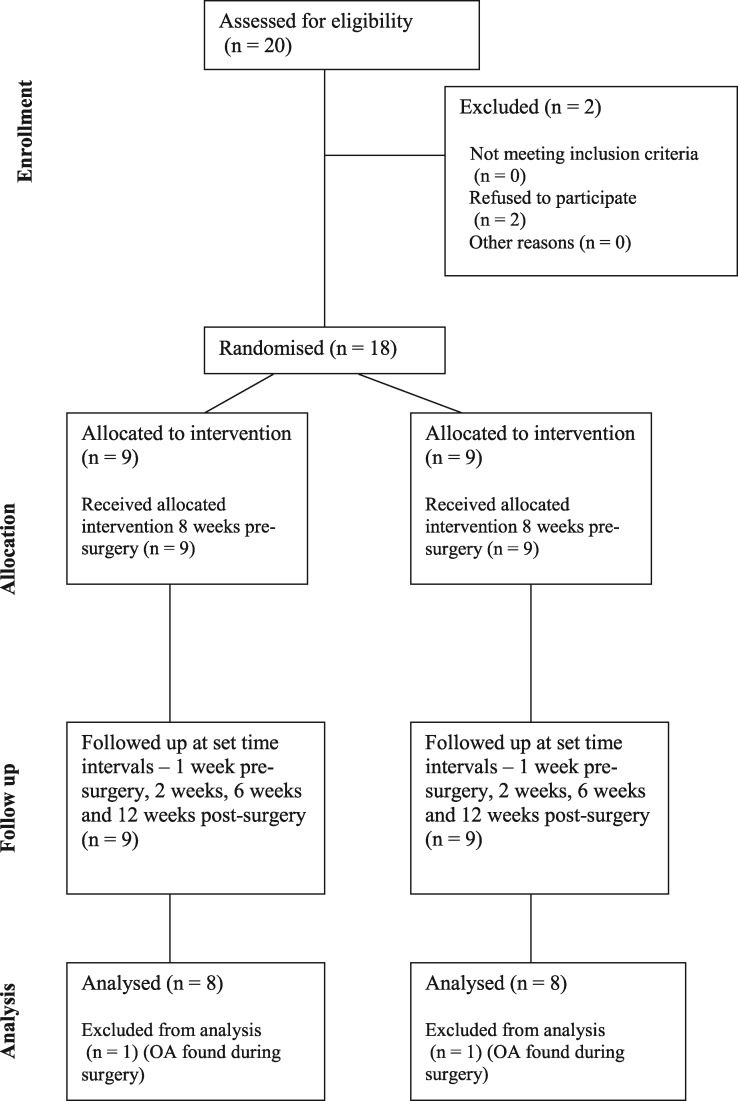
Patients awaiting hip arthroscopy surgery who had symptomatic FAI and a labral tear were recruited consecutively in clinic by the orthopaedic surgeon between the period of October 2013 and February 2014. Subjects were excluded if they had radiographic evidence of hip dysplasia or Grades 3–4 osteoarthritic changes (OA) [12], avascular necrosis or rheumatological disorders. Additional exclusions were subjects under the age of 18 years, an inability to give full written consent and previous ipsilateral hip surgery. Thirteen females and seven males who were identified as meeting the criteria were assessed for eligibility (Fig. 1) by the orthopaedic surgeon. Full written consent was obtained on initial attendance at the study centre.
Fig. 1.
CONSORT diagram showing the flow of participants through each stage of this randomized trial.
Randomization and blinding
The outcome measure assessor and the orthopaedic surgeon were blinded to the allocation of which group a participant belonged to. It was not possible to blind the physiotherapist carrying out the intervention or the participants. Randomization into either the control Group A or intervention Group B was conducted via random permutated blocks.
Study procedure
Each subject received 5 study visits, each visit lasting 60 min. At the start of each visit, the blinded assessor carried out the outcome measure tests with the subject in a private room with no other persons present. Once the assessor had left the room the intervention physiotherapist entered and carried out the procedures detailed below.
Visit 1
Eight weeks before surgery, Group A, the control group, received massage to the pre-operative lower limb by the intervention physiotherapist, to aid temporary comfort of the involved leg [13]. Subjects assigned to intervention Group B were instructed in the daily pre-operative pre-habilitation exercises defined in supplementary file SI. In addition to instruction on correct technique, the subjects were provided with a booklet containing each exercise, detailed with a description and photograph. Furthermore, an 8-week daily diary was given to record when they carried out each exercise and if any pain or discomfort was experienced. Hip flexor, extensor, hip adductor, hip abductor and external rotator exercises were selected as these muscle groups have previously been reported to be weak in FAI patients [14, 15]. Knee extensor exercises (single leg squat) were chosen as they have been identified as a muscle group that can influence post-operative outcome in total hip replacement surgery patients. It has been postulated that a higher pre-operative function in this muscle group may enhance post-operative outcomes [16]. Improvement of plantar flexor strength was included to promote ankle push-off function, as it is thought that increasing this function decreases the force through the anterior of the hip, which may consequently benefit hip labral pathology sufferers [17].
Visit 2
One week before surgery, a hard-copy post-operative rehabilitation guide (supplementary material files SII and SIII) that included a diary, was given to all participants, plus instruction on how to perform the exercises. Post-operative advice comprised no hip flexion past 90° for approximately 6 weeks, no driving for 2 weeks, no straight leg raising, no deep squats, no pivoting on a weight bearing leg, no exercising into pain, no prolonged sitting or sitting where the hips are lower than the knees.
Surgery
All participants underwent a unilateral hip arthroscopy, which involved labral repair and boney decompression for FAI. This was carried out under spinal and general anaesthesia in the supine position by the same surgeon at the same NHS hospital. They all received standard immediate post-operative care incorporating the application of a continuous passive motion machine to the operated leg for a period of 4 h overnight and standard pain relief. Patients were seen by the NHS in-patient chartered physiotherapist to ensure safe use of walking aids and flat foot partial weight-bearing, and were asked to use their walking aids until reassessment at their 2-week study visit.
Visit 3
Two weeks post-surgery, the intervention physiotherapist checked the participant’s gait, use of crutches and gave instructions on how to wean from them safely. Post-operative exercise diaries were reviewed and progressive exercises taught as per the rehabilitation guide. Massage for pain relief was carried out on the operated limb of all participants [18].
Visit 4
Six weeks post-surgery, all participants attended a hip specific hydrotherapy session (supplementary material file SIV), which is generally recommended in the recovery phase [19]. The intervention physiotherapist reviewed the exercise diaries, checked gait and progressed exercises from the rehabilitation guide.
Visit 5
All participants attended the study centre at twelve weeks post-surgery for a final study visit. The researcher assessed the feedback from the exercise diaries and instructed the subjects on appropriate exercises from the rehabilitation guide. Massage was carried out on each subject’s operative lower limb as per Visit 3. A final study visit summary letter was written to the GP and orthopaedic consultant to inform them of the participant’s progress, and arrangements made if further physiotherapy was required now the study visits had concluded.
Outcome measures
Patient reported outcome measures
All patients completed a Non-Arthritic Hip Score (NAHS) and EQ-5D-5 L questionnaires at each visit. The NAHS is recognized as a validated outcome measure for patients undergoing hip arthroscopy [20]. The EQ-5D-5 L is a health measurement scale aiming to reflect five elements of health [21]. Scores for each questionnaire were recorded by the blinded assessor, on a single sheet marked only with the unique reference number for that individual subject.
Dynamometry muscle function measurement
Hand held dynamometers (HHDs) have been found to be a reliable method of testing isometric strength [22, 23]. The MicroFet2 (Hoggan Health Industries, Inc., Draper, UT, United States) is an HHD device that has been used and validated in studies [16, 24]. The device was calibrated according to the manufacturer’s guidelines. A chartered physiotherapist, who is experienced in regular use of the HHD with hip patients, performed the assessment of muscle power. This clinician was blinded as to which group the subject was in. The test procedure was the same for every test and every individual. The muscle groups tested were hip abductors, hip adductors, hip flexors and hip external rotators, as these were reported to be weak in FAI sufferers [14, 15]. Additionally, knee extensors were tested as this muscle group was highlighted as a possible link to functional ability in patients undergoing hip arthroplasty surgery [16]. The same examination couch was used throughout, with the pelvis stabilized by a strap, for prone/supine positions. The leg to be tested when testing hip adduction and abduction was straight, the hip joint neutral, the subject in supine, and the opposite leg bent with foot flat on the table to aid stabilization of the body. Hip flexion was tested in supine, with the test leg in 45° hip flexion and foot flat on the bed; the opposite leg was in the same position. Hip external rotation isometric testing was performed in the prone position with the non-test leg straight and the test leg with knee at 90° flexion. The dynamometer placement was 5 cm proximal to the malleoli when testing hip abduction, adduction and external rotation, and 5 cm proximal to the superior patella border when testing hip flexion. Knee extensor muscle testing was carried out in sitting, hips and knees flexed to 90°, with both feet on the floor, the dynamometer was placed on the anterior tibia 5 cm proximal to the superior border of the medial malleoli [22].
The tester resisted the static (isometric), maximal voluntary contraction for 5 s and recorded the highest value read (in lbs) on the dynamometer, the ‘make’ method [24]. There was a practice test with each movement, and then the test was carried out four times with each movement [22]. The opposite leg was tested with the same movement as a comparison, giving the test leg a rest before the next isometric test.
Data and statistics
A mixed analysis of covariance (ANCOVA) was performed for each outcome variable in order to identify a difference between the treatment groups, and to establish if there were changes over time. Outcome variables were logged to stabilize the variances and make the technique appropriate.
RESULTS
Twelve females and six males gave written consent to enrol on this trial after being given a detailed patient information sheet. All eighteen participants completed the study and there were no drop-outs after enrolment. Data for two subjects had to be excluded from analysis as surgical findings revealed that grade 4 osteoarthritic changes were present in the joint that had not been detected on pre-surgery imaging. Baseline subject characteristics are shown in Table I.
Table II.
Comparison between intervention and non-intervention groups from baseline to 12 weeks post-operative
| Outcome (logged variables) | F(1,13) | P values |
|---|---|---|
| Hip abduction strength | ||
| Operated side | 0.28 | 0.60 |
| Non-operated side | 3.3 | 0.09 |
| Hip adduction strength | ||
| Operated side | 4.17 | 0.06 |
| Non-operated side | 2.98 | 0.11 |
| Hip flexion strength | ||
| Operated side | 6.73 | 0.022* |
| Non-operated side | 1.20 | 0.29 |
| Hip external rotation strength | ||
| Operated side | 0.43 | 0.52 |
| Non-operated side | 2.41 | 0.15 |
| Knee extension strength | ||
| Operated side | 4.84 | 0.046* |
| Non-operated side | 15.05 | 0.002* |
| Non-arthritic hip score | 0.43 | 0.53 |
| EQ-5D-5L | 6.05 | 0.029* |
Statistically significant P < 0.05.
Table II shows a comparison between the treatment groups from baseline to 12 weeks post-operative, taking into account that the groups differ on the baseline values. This is a small study, and generally the intervention group had higher values, see Table III, but not all values were statistically significant. Statistically significant differences (P < 0.05) were noted between the treatment groups for hip flexion strength on the operative side (P = 0.02) and for knee extension strength for both operative (P = 0.05) and non-operative sides (P = 0.002) and for EQ-5D-5 L health (P = 0.03).
Table I.
Baseline characteristics of randomized study subjects
| Characteristic | Non-intervention group | Intervention group |
|---|---|---|
| Mean age (years) | 41.75 ± 11.84 | 37.5 ± 6.05 |
| Women:men ratio | 7:1 | 4:4 |
| % in full time work | 100 | 100 |
| % taking daily analgesia | 62.5 | 50 |
| Mean time suffering pre-op | 36.5 months | 23.25 months |
| % of whom were an athlete | 0 | 0 |
Table III.
Descriptive statistics for muscle strength of the operative side, NAHS and ED-5Q-5 L at 8 and 2 weeks pre-operative, and 12 weeks post-operative
| Outcome | 8 wks pre-op Mdn (IRQ) | 2 wks pre-op Mdn (IRQ) | 12 wks post-op Mdn (IRQ) |
|---|---|---|---|
| Hip abductiona Non-Int | 15.5 (10.9–18.3) | 13.6 (8.5–14.7) | 18.8 (14.7–23.3) |
| Hip abductiona Int | 16.6 (12.7–28.6) | 20.9 (15.6–31.3) | 20.9 (18.3–31.3) |
| Hip adductiona Non-Int | 14.8 (8.9–16.9) | 12.4 (8.2–14.8) | 17.2 (13.7–20.3) |
| Hip adductiona Int | 13.4 (13.0–19.5) | 19.3 (15.9–29.3) | 18.8 (16.4–28.3) |
| Hip flexiona Non-Int | 23.4 (15.5–32.7) | 18.9 (10.5–27.4) | 25.5 (20.3–34.5) |
| Hip flexiona Int | 27.3 (16.4–47.6) | 32.9 (28.8–51.2) | 36.1 (22.0–51.6) |
| Hip ext Rota Non-Int | 13.7 (11.4–15.8) | 13.9 (9.3–15.0) | 15.6 (15.2–20.0) |
| Hip Ext Rota Int | 15.3 (12.0–19.1) | 19.0 (13.7–22.3) | 18.4 (14.3–31.5) |
| Knee Extensiona Non-Int | 33.6 (20.2–44.5) | 25.1 (18.4–36.4) | 38.7 (30.8–63.3) |
| Knee Extensiona Int | 37.1 (22.1–53.1) | 49.0 (34.2–88.5) | 56.4 (39.5–104.5) |
| NAHS Non-Int | 54.4 (46.6–79.7) | 48.8 (36.6–64.4) | 85.0 (79.7–88.8) |
| NAHS Int | 60.0 (48.4–80.3) | 56.3 (51.3–76.3) | 91.3 (78.8–94.7) |
| EQ-5D-5L (SOH) Non-Int | 57.5 (50.0–76.3) | 55.0 (42.5–67.5) | 82.5 (75.0–85.0) |
| EQ-5D-5L (SOH) Int | 55.0 (50.8–60.0) | 75.0 (71.3–80.0) | 85.0 (81.3–89.5) |
aMuscle strength measured in pounds (lbs), operative side leg.
Mdn, median; IQR, interquartile range; wks, weeks;
Pre-op, pre-operative; Post-op, post-operative; Non-int, non-intervention group; Int, intervention group; Ext Rot, external rotation; NAHS, Non-Arthritic Hip Score; SOH, scale of health.
DISCUSSION
Our hypothesis was that pre-habilitation exercises would improve patient reported outcome measure scores and muscle power post-operatively. On reflection of the study aims, there have been some encouraging results in favour of exercise before surgery. To the author’s knowledge, there was only one retrospective study of 69 subjects that has looked at the hypothesis of whether pre-operative exercises are beneficial in hip arthroscopy patients, reporting at 8 weeks post-surgery a significant improvement in the Modified Harris Hip Score, P = 0.0421 [6], and also one paper which demonstrated patients with greater pre-operative strength deficits may result in reduced ability in their post-operative recovery [25]. The lack of other studies makes it hard to draw comparisons.
The significant components of this study were randomization, an intervention and control group, blinding of the outcome measure assessor and surgeon and testing of outcome measures before the intervention, during the trial and at the end. The use of HDD provided objective measurements pre and post-surgery. The use of this method may have benefit in justifying treatment efficacy in clinical practice and providing feedback and education to patients [26, 27]. It is noteworthy to add that the subjects were recruited from the NHS to represent a sample from the general population. This was a pilot study to test treatment efficacy, aiming to analyse procedure and outcome measures in preparation for future research.
The pre-operative measurements between the two groups at Visit 1 (8 weeks before surgery) and Visit 2 (3 weeks before surgery) in the intervention group all improved (Table III). This could be of clinical importance as it suggests that it may be possible for patients with hip pathology to maintain or even improve their lower limb muscle power, and thus embark on surgery in a less weakened state [8]. A time span of 8–12 weeks of non-surgical intervention is advocated prior to surgical intervention [11], to ensure the patient has experienced conservative management including physiotherapy, medication and guided therapeutic injections. The patient diaries from the intervention group reported no pain aggravation from the pre-operative exercises. Muscle weakness, inflammation and pain may affect hip joint stability, gait and functional movement patterns, thus being able to improve strength without symptom provocation is encouraging [28, 29].
The HAPI study chose to implement specific rather than general exercises, to target those muscles reported in previous studies to be weak in FAI subjects, in order to improve hip muscle dysfunction [30]. Since completion of this study, further evidence has been published reporting specific muscle weakness in subjects with labral pathology [27], in FAI [31] and post-hip arthroscopy [32]. Recommendations as a result of these studies have been made to target single leg squats [32] and hip flexor strength in rehabilitation [2]. Our study demonstrated statistical significance regarding the positive benefits of pre-operative exercise in these two muscle groups, with the intervention group performing better in strength (hip flexion P = 0.02 and knee extension/quadriceps P = 0.05). The intervention group also improved greater in the quality of life questionnaire EQ-5D-5 L scale of health P = 0.03. The results from all these studies [27–32] highlight that patients do suffer specific muscle weakness and if this can be addressed in the pre-operative period it could optimize the patient’s recovery journey. A visit to a chartered physiotherapist before surgery to be taught specific exercises, how to care for your hip, education on avoiding pain-provoking situations, how to prepare for and what to expect from surgery, is potentially viable in clinical practice. Individuals who may not be compliant in the rehabilitation process may be acknowledged in this time period. The possibility of being able to reduce the amount of post-operative physiotherapy visits and improve outcome after surgery are important in patient care and healthcare economics. Furthermore, being able to provide evidence around practice is essential to demonstrate services and interventions are cost-effective.
LIMITATIONS
There are several limitations to this study, including a small sample size, an 8-week time span for pre-operative exercises and a 3-month follow-up post-surgery, due to the time restraints of the Masters programme; a longer period may have shown different results. This study had a broad inclusion criteria regarding age, over the age of 18. It would not have been feasible to have a stricter age-range as this would have affected the recruitment of individuals in the short time available for this project. Furthermore, variables present in the patient population such as age, gender, height, weight, length of time suffering with pain prior to surgery, daily commitments and to what degree they participate in sports, are all possible factors that could affect results. A stricter inclusion criteria with age limits, time period suffering before injury, and the type of FAI surgery carried out could be implemented in a future study, or sub-grouped for data analysis. In addition, although dynamometry gives us quantitative data regarding muscle force output, it does not tell us if there are any compensatory effects from other muscles or measure quality of functional movement patterns.
CONCLUSION
The findings of this study would suggest that, in patients undergoing hip arthroscopy for FAI, it may be possible for them to improve their pain, function and muscle power pre and post-operatively using specific exercises focusing on relevant muscle groups. As this is a pilot study, these findings can only be referred to as positive trends towards pre-operative exercises, statements made regarding recommendations for practice need to be based on strong evidence. This pilot study suggests that a main future study has the potential for informing practice around the benefit of pre-operative exercises to aid post-operative recovery from hip arthroscopy and highlighting the benefit of specific muscle strengthening to improve outcomes.
SUPPLEMENTARY DATA
Supplementary data are available at Journal of Hip Preservation Surgery online
Supplementary Material
ACKNOWLEDGEMENTS
Thank you to Mr Jon Conroy and his NHS research and development team for their collaboration. Thank you to Derek Cooper, Kay Caldwell and Elaine Atkins at Middlesex University in their guidance for my MSc research dissertation.
Thank you to Nicola Hinchliffe for her contribution as blinded assessor.
FUNDING
This research was funded solely by Louise Grant.
CONFLICT OF INTERESTS STATEMENT
None declared.
REFERENCES
- 1. Enseki KR, Martin R, Draovitch P.. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther 2006;36:516–25. [DOI] [PubMed] [Google Scholar]
- 2. Shetty VD, Villars RN.. Hip arthroscopy: current concepts and review of literature. Br J Sports Med 2007;41:64–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wahoff M, Ryan M.. Rehabilitation after hip femoroacetabular impingement arthroscopy. Clin Sports Med 2011;30:463–82. [DOI] [PubMed] [Google Scholar]
- 4. Larson CM, Giveans MR.. Arthroscopic management of femoroacetabular impingement: early outcome measures. Arthroscopy 2008;24:540–6. [DOI] [PubMed] [Google Scholar]
- 5. Clohisy JC, Lauren C, St John BS. et al. Surgical treatment of femoroacetabular impingement. A systematic review of the literature. Clin Orthop Relat Res 2010;468:555–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bortolli AD, Fujii EI, Ingham SM. et al. Paper♯31: The role of preoperative physiotherapy in patients undergoing arthroscopic surgery for FAI. International Society of Hip Arthroscopy Annual Scientific Meeting, Boston, USA2012. Available at: http://www.ishameetings.net/meetings/2012/asm/proceedings/contents/files/Paper_31.pdf. Accessed: 12 December 2012.
- 7. Coudeyre E, Jardin C, Givron P. et al. Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelines. Ann Readapt Med Phys 2007;50:189–97. [DOI] [PubMed] [Google Scholar]
- 8. Gill SD, McBurney H.. Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehab 2013;94:164–76. [DOI] [PubMed] [Google Scholar]
- 9. Vukomanovic A, Popovic Z, Durovic A, Krstic L.. The effect of short-term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanit Pregl 2008;65:291–7. [DOI] [PubMed] [Google Scholar]
- 10. Wall P, Fernandez M, Griffin D. et al. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R 2013;5:418–26. [DOI] [PubMed] [Google Scholar]
- 11. Enseki K, Harris-Hayes M, White DM. et al. Non-arthritic hip joint pain. Clinical practice guidelines. J Orthop Sports Phys Ther 2014;44:A1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tönnis D. Normal values of the hip joint for the evaluation of hip x-rays in children and adults. Clin Orthop 1976;119:39–47. [PubMed] [Google Scholar]
- 13. Adams R, White B, Beckett C.. The effects of massage on pain management in the acute care setting. Int J Ther Massage Bodywork 2010;3:4–11. [PMC free article] [PubMed] [Google Scholar]
- 14. Casartelli NC, Maffiuletti NA, Item-Glatthorn JF. et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage 2011;19:816–21. [DOI] [PubMed] [Google Scholar]
- 15. Tsai Y-S, McCrory JL, Sell TC. et al. Hip strength, flexibility and standing posture in athletes with an acetabular labral tear. J Orthop Sports Phys Ther 2004;34:A55–6. [Google Scholar]
- 16. Holstege MS, Lindeboom R, Lucas C.. Preoperative quadriceps strength as a predictor for short-term functional outcome after total hip replacement. Arch Phys Med Rehabil 2011;92:236–41. [DOI] [PubMed] [Google Scholar]
- 17. Lewis CL, Ferris DP.. Walking with increased ankle push off decreases hip muscle moments. J Biomech 2008;41:2082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mitchinson AR, Kim HM, Rosenberg JM. et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg 2007;142:1158–67. [DOI] [PubMed] [Google Scholar]
- 19. Enseki KR, Draovitch P.. Rehabilitation for hip arthroscopy. Oper Tech Orthop 2010;20:278–81. [Google Scholar]
- 20. Tijssen M, Cingel RV, Melick NV. et al. Patient reported outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskeletal Disord 2011;12:117.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jansson KA, Granath F.. Health-related quality of life (EQ-5D) before and after orthopaedic surgery. Acta Orthopaedicia 2011;82:82–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Thorburg K, Peterson J, Magnusson SP. et al. Clinical assessment using a hand-held dynamometer is reliable. Scand J Med Sci Sports 2010;20:493–501. [DOI] [PubMed] [Google Scholar]
- 23. Kelln BM, McKeon PO, Gontkof LM. et al. Hand held dynamometry: reliability of lower extremity muscle testing in healthy, physically active, young adults. J Sport Rehabil 2008;17:160–70. [DOI] [PubMed] [Google Scholar]
- 24. Stratford PW, Balsor BE.. A comparison of make and break tests using a hand-held dynamometer and the Kin-Com. J Orthop Sports Phys Ther 1994;19:28–32. [DOI] [PubMed] [Google Scholar]
- 25. Cooper J, Monahan S, Fox MB. et al. Paper♯ 54: Pre-op strength influences recovery following hip arthroscopy. Arthroscopy 2011;27:e103–4. [Google Scholar]
- 26. Kemp JL, Schache AG, Makdissi M. et al. Greater understanding of normal hip physical function may guide clinicians in providing targeted rehabilitation programmes. J Sci Med Sports 2013;16:292–6. [DOI] [PubMed] [Google Scholar]
- 27. Mendis MD, Wilson SJ, Hayes DA. et al. Hip flexor muscle size, strength and recruitment patterns in patients with acetabular labral tears compared to healthy controls. Man Ther 2014;19:405–10. [DOI] [PubMed] [Google Scholar]
- 28. Freeman S, Mascia A, McGill S.. Arthrogenic neuromusculature inhibition. Clin Biol 2013;28:171–7. [DOI] [PubMed] [Google Scholar]
- 29. Harris-Hayes M, Mueller MJ, Sahrmann SA. et al. Persons with chronic hip joint pain exhibit reduced hip muscle strength. J Ortho Sport Phys Ther 2014;44:890–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. French HP, Gilsenan C, Cusack T.. Gluteal muscle dysfunction and the role of specific strengthening in hip osteoarthritis: a review. Physical Ther Rev 200813:333–44. [Google Scholar]
- 31. Diamond LE, Wrigley TV, Hinman RS. et al. Isometric and isokinetic hip strength and agonist/antagonist ratios in symptomatic femoroacetabular impingement. J Sci Med Sport 2015; http://dx.doi.org/10.1016/j.jsams.2015.10.002 [DOI] [PubMed] [Google Scholar]
- 32. Charlton PC, Bryant AL, Kemp JL. et al. Single leg squat performance is impaired 1 to 2 years after hip arthroscopy. PM R 2015;8:321–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.