Abstract
Background and Objectives
Depressive symptoms have been identified as an important consequence of substance use. Both heavy drinking and marijuana use have acute and short-term effects on systems that regulate emotion, increasing the potential for substance use to induce problems with negative affect and irritability. We investigated the effects of alcohol and marijuana use on depressive symptoms among a sample of young Black men. We also tested the stress sensitization hypothesis that exposure to adverse childhood experiences would amplify the influence of substance use on men’s depressive symptoms.
Methods
Hypotheses were tested with 505 rural Black men who, at ages 19 to 22 years, provided data on their substance use, adverse childhood experiences, and depressive symptoms; they provided data again 18 months later.
Results
Substance use forecasted increases in depressive symptoms; cross-lagged analyses yielded no evidence for the inverse path, depressive symptoms increasing substance use. The impact of substance use on depressive symptoms was amplified among young Black men who were exposed to adverse childhood experiences. Substance use did not significantly predict depressive symptoms when adversity was low.
Discussion and Conclusions
Our findings suggest that, during young adulthood, substance use increases depressive symptoms among Black men who were exposed to childhood adversity. Because childhood adversity disproportionately affects Black men, these findings inform future cross-group research designed to investigate racial disparities in the consequences of substance use.
Scientific Significance
Depressive symptoms may be understood as an effect as well as a cause of substance use, particularly among vulnerable young Black men.
INTRODUCTION
Substance use rates peak among young adults in the years following high school.1 Alcohol and marijuana are the most commonly abused psychoactive substances.2 Among college-age youth, annual prevalence of illicit drug use exceeds 40%; use of drugs other than marijuana is 10%; and past-month binge drinking exceeds 25%.2 The acute and short-term consequences of substance use include medical complications of intoxication, injuries, accidents, and increased engagement in high risk health behavior such as risky sex.1 Substance use also negatively affects mental health and educational and vocational functioning.2
Accumulating data suggests that the negative consequences of substance use are elevated for young Black men, particularly those from low-socioeconomic status (SES) backgrounds. Black men experience more negative consequences per ounce of alcohol or other drugs consumed in terms of accidents, injuries, interpersonal problems, legal problems, and economic difficulties than do young men from other racial/SES groups.3,4 Negative consequences among Black men occur despite generally low levels of substance use among Black male youth during childhood and adolescence.5 However, during the transition to adulthood, rates of alcohol and marijuana use escalate rapidly.5 These data underscore the need to examine substance use and its consequences among Black men during the young adult years.
Depressive symptoms are a robust correlate of substance use.6,7 Epidemiological data suggests that men and Blacks experience lower rates of depressive symptoms and disorders than do women and members of other racial or ethnic groups.8 Recent research indicates that this may not be true for young Black men,9 particularly those from low resource environments.10 Recent research indicates11 that young Black men experience depressive symptoms at rates similar to or higher than those reported by Caucasian men and women. Other research suggests that typical assessments of depressive symptoms may lead to under-reporting of depression among men in epidemiological studies.12 In particular, when aspects of anger and irritable behavior are operationalized as forms of depressive symptomology for men, rates of depression generally increase12 and provide a conceptual expansion of depression that can inform effective treatment for men’s mental health.10
Depression has been identified both as a cause and as a consequence of substance use. The “self-medication hypothesis” posits that substances may be used as a means of coping with the negative emotions associated with depression.6 Conflicting evidence has emerged regarding this conjecture.7 Inclusive reviews have identified several reasons for initiating and escalating substance use, such as social and hedonistic motives and peer influences, that did not involve self-medication.13 Other research underscores the potential for substance use to contribue to depressive symptomology.7 For example, a recent longitudinal study indicated that, among Black men, substance use during the transition to adulthood forecasted psychological distress; the reverse, however, was not evident.14 Similar findings link substance use in early adolescence to later mood problems, a direction of effect that emerged for Black children but not for those from other racial/ethnic groups.15 Although drinking and marijuana use provide short-term stress-dampening effects, 16 the temporary appealing effects of substance use are followed by an increase in negative affect that includes irritability and emotional pain.17 The extent to which substance use during the transition to adulthood affects young Black men’s symptoms of depression, however, remains to be investigated.
The second aim of the present study is to investigate the potential for adverse childhood experiences to influence of the effect of substance use on depressive symptoms. Adverse childhood experiences include potentially traumatic events such as living in destructive home environments characterized by domestic violence, exposure to economic hardship, and experiencing neglectful or abusive treatment from caregivers.18 Studies indicate that that minority children are disproportionately exposed to childhood adversity compared to Caucasian youth.19,20 Considerable research documents links between assessments of adverse childhood experiences and substance use onset and escalation among young people18 as well as chronic substance use problems among adults.21 However, the potential for childhood adversity to amplify the association between depressive symptoms and substance use in young Black men, has not been investigated.
Our moderational hypothesis is informed by stress sensitization models regarding the development of substance use and mental health problems. Recent empirical and theoretical work emphasizes the role of early adversity in establishing vulnerabilities that can heighten reactivity to exposure to downstream risk factors.22 For example, a history of maltreatment may affect the likelihood that an adult abuses substances when exposed to negative life events.22 Childhood adversity has documented effects on the mesolimbic systems involved in processing substance use reinforcement, systems that also play critical roles in emotion processing and regulation.23 Existing vulnerabilities in these emotion regulation pathways may interact with substance use, compounding its effects.21 We thus hypothesize that substance use will have a particularly robust effect on depressive symptoms when young men have been exposed to adverse childhood experiences.
In summary, the purpose of this study was to test the hypotheses that among young Black men (a) substance use would predict increases in depressive symptoms and that (b) exposure to childhood adversity would amplify the effect of substance use on depressive symptoms. Hypotheses were tested with a sample of 505 men from resource poor rural environments, using a short-term prospective design (18 months). To increase the rigor of our analyses, we examined the alternative hypothesis that depression influenced changes in substance use and controlled for three confounding factors that have documented associations with both substance use and depressive symptoms: employment status, economic distress, and past year incarceration.
METHODS
Participants
Participants included 505 Black men who resided in one of 11 rural counties in South Georgia. These communities are representative of the southern Coastal Plain, a geographic concentration of rural poverty that coincides with the worst economic and health disparities by race in the United States.24 Men were 19 to 22 years of age (M = 20.29; SD = 1.10) at the baseline interview. Participants were recruited using respondent-driven sampling (RDS), which combines a prescribed chain referral recruitment method with a mathematical model that allows for post-stratification sample weighting. The method and weighting system are designed to attenuate the influence of biases common in chain referral samples and to better approximate a random sample of the target population.25
Recruitment and Data Collection Procedures
Community liaisons recruited 45 initial “seed” participants from targeted counties. These liaisons provided contact information to research staff, who conducted the baseline survey. Data collection staff visited participants at their homes or at convenient community locations, and participants completed an audio computer-assisted self-interview on a laptop computer. This allowed participants to navigate the survey privately with the help of voice and video enhancements, eliminating literacy concerns. Participants provided written informed consent at baseline; all study protocols were approved by the Human Subjects Review Board of the university at which the research was conducted. Participants received $100 for completing the survey.
Each seed participant was then asked to identify three other Black men in his community. Project staff contacted the referred participants, and the referring participant received $25 per person who completed the survey. After completing the survey, each referred participant, in turn, was asked to refer three men in his network. Referred participants also received $100 for completing the survey and $25 for each successful referral. Approximately 18.30 (SD = 4.19) months after the baseline survey, when men’s mean age was 21.86 years (SD = 1.24), a follow-up data collection visit was conducted. Of the 505 men who participated at baseline (T1), 83.8% completed the follow-up survey (T2). Retention status was not associated with any study variables. At each follow-up assessment, men received $100.00 for completing the survey.
Measures
Substance Use
At T1 and T2, men self-reported the number of days during the past month on which they engaged in binge drinking (four or more drinks in one sitting) and the number of days in the past month in which they used marijuana. Although alcohol and marijuana bind to different receptors, their influence on dopaminergic pathways implicated in addiction and emotion regulation are similar.26 We thus standardized and combined indicators of alcohol and marijuana use frequency to form a substance use index (Spearman’s ρ = .19, p < .01 at T1; ρ = .19, p < .01 at T2).
Depressive Symptoms
Assessment of depressive symptoms was informed by Martin and colleagues12 research that indicates men’s expression of depressive symptoms includes angry and irritable behaviors as well as more familiar internalizing symptoms. We thus operationalized depressive sympotoms as a latent construct comprised of two scales. Men self-reported their symptoms of depression in the past week using a 10-item brief version of the Center for Epidemiological Studies–Depression (CES-D) measure.27 The response scale ranged from 1 (rarely or none of the time) to 4 (all of the time); example items include, “I felt depressed,” and “I was bothered by things that usually don’t bother me.” Cronbach’s alphas were .74 at T1 and .78 at T2. On the second measure, men self-reported their feelings and expression of anger on an 8-item Anger subscale of the Client Evaluation of Self and Treatment.28 Men reported their agreement on a scale ranging from 1 (strongly disagree) to 4 (strongly agree). Example items include, “I feel a lot of anger inside me” and “I get mad at other people easily.” Alphas were .82 at T1 and .86 at T2.
Adverse Childhood Experiences
At baseline, men completed the 10-item Adverse Childhood Experiences measure.18 Participants reported the presence or absence of 10 types of adverse childhood experiences during their first 16 years of life. Adversities included one’s own experience of physical abuse, sexual abuse, or neglect; or of witnessing violence to one’s caregiver. Scores ranged from 0 to 10 adversities, with a mean of 2.23 (SD = 2.09).
Demographic Characteristics and Control Variables
Age at baseline was assessed as a continuous variable. Participants also reported their education levels (coded as 0 = < high school diploma, 1 = high school diploma/general educational development equivalent, and 2 = > high school diploma). Employment status was assessed with the item, “Are you currently employed at a job where you receive a paycheck?” The responses were coded as 0 (not employed) or 1 (employed).
Control variables included economic distress and criminal justice problems. Economic stress was assessed using a 5-item scale ranging from 1 (strongly disagree) to 4 (strongly agree). Young men reported whether, during the past 3 months, they had enough money for shelter, food, clothing, medical care, and personal items. Cronbach’s alpha was .79. Finally, criminal justice problems during the past year were assessed with the item, “In the past year, how many times, if any, were you arrested and charged or booked with a criminal offense?” Because of low base rates of arrests beyond seven, the range was truncated to a maximum of 7 to minimize undue influence of outliers.
Plan of Analysis
Hypotheses were tested with structural equation modeling as implemented in Mplus 7.13.29 Parameters were estimated and missing data were managed with Full Information Maximum Likelihood (FIML) procedures. We first examined the assessment of depressive symptoms using a 2nd order confirmatory factor analysis.29 We specified that the CES-D items and Anger items would tap distinct latent variables that, in turn, would each load on a latent depressive symptoms construct. This depressive construct was used in subsequent tests of study hypotheses. We then examined the directions of effect between substance use and depressive symptoms using cross-lagged analysis and controlling for demographic and current stress factors. We hypothesized that substance use at T1 would predict depressive symptoms at T2. We then tested the stress sensitization hypothesis that adverse childhood experiences would moderate the influence of substance use at T1 on depressive symptoms at T2. We specified T1 substance use, adverse childhood experiences, and an interaction term (substance use × adverse childhood experience) as predictors of T2 depressive symptoms, controlling for baseline depressive symptoms and other covariates.
RESULTS
Sample characteristics are presented in Table 1. The majority of men reported having a high school diploma or GED (56%); 29% reported having at least some college education. Of the men, 41.6% were employed. Approximately one in five men reported spending at least one night in jail in the past year. At T1 men reported binge drinking on average 1.6 days per month and using marijuana 8.4 days per month. At T2, binge drinking on average 2.6 days per month and using marijuana 8.2 days per month. Demographic characteristics of the sample were similar to those of samples of Black youth in Georgia obtained by a probability sampling method.30
TABLE 1.
Sample characteristics
| Variables | M (SD) or n (%) | Range |
|---|---|---|
| Demographic controls | ||
| Agea | 20.29 (1.10) | 19 – 22 |
| Education attainmentb | ||
| < High school | 77 (15.2) | – |
| High school/GED | 283 (56.0) | – |
| > High school | 145 (28.7) | – |
| Employment statusb | ||
| Unemployed | 295 (58.4) | – |
| Employed | 210 (41.6) | – |
| Current stress controls | ||
| Economic stressa | 2.10 (0.62) | 1.00 – 4.00 |
| Incarceration in the past yearb | ||
| No | 401 (79.4) | – |
| Yes | 104 (20.6) | – |
| Study variables | ||
| Adverse childhood experiencesa | 2.23 (2.09) | 0.00 – 10.00 |
| Substance use T1a | 9.99 (12.80) | 0.00 – 50.00 |
| Binge drinkinga | 1.63 (3.10) | 0.00 – 20.00 |
| Marijuana usea | 8.44 (12.13) | 0.00 – 30.00 |
| Substance use T2a | 10.04 (12.95) | 0.00 – 51.00 |
| Binge drinkinga | 2.16 (4.02) | 0.00 – 25.00 |
| Marijuana usea | 8.15 (11.71) | 0.00 – 30.00 |
| Male depressive symptoms T1 | ||
| CES-D Depressiona | 1.41 (.41) | 1.00 – 3.33 |
| Anger/hostilitya | 2.29 (.67) | 1.00 – 4.00 |
| Male depressive symptoms T2 | ||
| CES-D Depressiona | 1.45 (.45) | 1.00 – 2.89 |
| Anger/hostilitya | 2.20 (.71) | 1.00 – 4.00 |
Note. N = 505.
Mean, standard deviation, and value range are shown.
Number and percentage in each categorical value are shown.
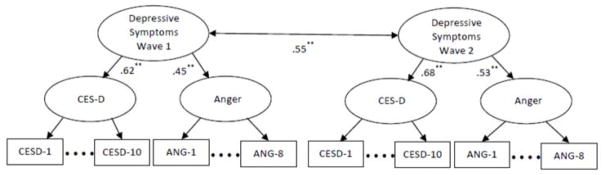
Figure 1 presents the results of the second-order factor analysis. At T1, model fit was as follows: χ2 = 279.58, df = 113, p < .01, CFI = .95, RMSEA = .04. The 10 CES-D items loaded significantly (p < .01) on the CES-D construct; lambdas ranged from .39 to .66. The eight anger items loaded on the anger construct significantly (p < .01); lambdas ranged from .63 to .84. The CES-D (λ = .62, p < .01) and Anger (λ = .45, p < .01) each loaded on the second order Depressive Symptoms construct. At T2, the model fit was χ2 = 287.08, df = 113, p < .01, CFI = .95, RMSEA = .04. The 10 CES-D items loaded significantly (p < .01) on the CES-D construct; lambdas ranged from .44 to .70. The eight anger items loaded on the anger construct significantly (p < .01); lambdas ranged from .66 to .85. The CES-D (λ = .68, p < .01) and Anger (λ = .53, p < .01) each loaded on the second order Depressive Symptoms construct.
FIGURE 1.
Second Order Confirmatory Factor Analysis of Depressive Symptoms
Note. T1 model fit: χ2 = 279.58, df= 113, P< .01, CFI= .95, RMSEA = .04; T2, model fit: χ2 287.08, df= 113, P< .01, CFI = .95, RMSEA = .04; **P <.01
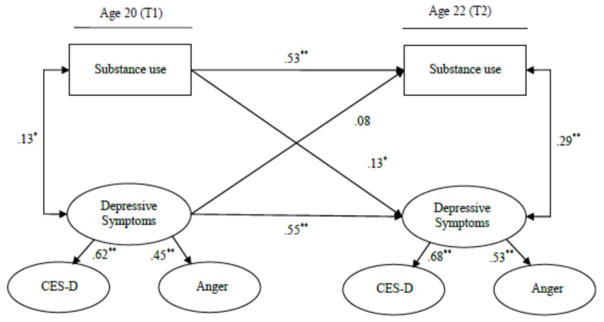
Figure 2 presents results of the cross-lagged analysis investigating the associations between substance use and depressive symptoms over time. This model fit the data as follows: χ2 = 11.57, df = 6, p = .07. RMSEA = .03. CFI = .98. Patterns of significant coefficients indicated that substance use at baseline forecasted changes in depressive symptoms from baseline to follow up (β = .15, p < .05). The reverse, however, was not evident (β = .01, ns). Table 2 presents the results of the test of the stress sensitization hypothesis. The model indicated that substance use at T1 interacted with childhood adversity to predict depressive symptoms at T2 (β = .09, p < .05) with T1 substance use, demographics, and other stress factors controlled. To interpret the interaction effect, we calculated the simple slopes under conditions of high and low adversity. Under conditions of low childhood adversity (< −1 SD), no significant association was evident between substance use and depressive symptoms (β = .07, p = .10). In contrast, under conditions of high childhood adversity (> +1 SD), a significant, positive association emerged (β = .25, p < .01).
FIGURE 2.
Cross-lagged model of the links between substance use and depressive symptoms
Note. χ2 = 1431.69, df= 713, p < .01. RMSEA = .04. CFI = .95. Standardized coefficients are shown. Target age, educational level, employment status, economic stress, and incarceration at T1 were controlled. *P< .05. **P<.01
TABLE 2.
Test of stress sensitization hypothesis. Substance use will interact with childhood adversity to predict depressive symptom at T2.
| Variable | β | SE |
|---|---|---|
| Demographic controls | ||
| Age | .08 | .05 |
| Education attainment | −.02 | .06 |
| Employment status | .02 | .05 |
| Current stress controls | ||
| Economic stress | .06 | .09 |
| Incarceration in the past year | .02 | .07 |
| Study variables | ||
| Male depressive symptom T1 | .45** | .08 |
| Substance use T1 | .08 | .05 |
| Adverse childhood experiences | .06 | .07 |
| Substance use T1 × Adverse childhood experiences | .11* | .05 |
Note. N = 505. χ2 = 1531.69, df = 725, P < .01. RMSEA = .04. CFI = .96.
P < .05.
P < .01.
DISCUSSION
The present study used an 18-month prospective design to examine the association between substance use and depressive symptoms during the transition to adulthood among low-SES Black men. Using a cross-lagged analysis, we found that substance use predicted increases in depressive symptoms; the path linking depressive symptoms to increases in substance use was not significant. This suggests that, during this developmental period, men were not necessarily using substances to cope with depressive symptoms. Rather, increases in depressive symptoms constituted a consequence of substance use. This effect was evident with a number of confounds and demographic characteristics controlled. We also hypothesized that the effects of substance use on depressive symptoms would be particularly pronounced among men exposed to adverse childhood experiences. Consistent with our hypothesis, childhood adversity was associated with a robust effect linking substance use to depressive symptoms. When childhood adversity was low, substance use had no significant effect on depressive symptoms.
Our results converge with other studies that suggest at this developmental time point and for this sample of young men, substance use is better understood as consequence rather than a cause of substance use. This finding is consistent with research on substance use motives among youth and young adults. Youth and young adults typically abuse substances in social contexts and commonly cite hedonistic and social reasons for their use. Our findings are also consistent with recent research examining paths between substance use and depressive symptoms among Black youth.14,15 These studies documented substance use effects on depression in both adolescents and adults. A final area of converging evidence involves laboratory and neurocognitive studies of the influence of alcohol and marijuana on systems associated with emotion regulation.17,21 Although marijuana and alcohol have disinhibitory effects during intoxication, use is followed by irritability and an increase in susceptibility to stress.17,26
Taken together, our results support a perspective that focuses on the potential mental health consequences of use, particularly for young adult users. During adolescence and young adulthood, substance use is common and typically arises from hedonistic and social motives and is often embedded in highly reinforcing peer cultures that celebrate use.13 In such cases, intervention strategies that teach coping skills for dealing with depression may not be indicated. Rather, efforts to influence peer norms and affiliations and to enhance efficacy for dealing with social situations may be more effective. For young people with a history of chronic use, however, the consequences for systems that regulate emotion can fundamentally alter the reasons for substance use. Over time, these reasons can change from social and lifestyle influences to efforts to cope with negative emotions.
The association of substance use with increases in depressive symptoms that emerged from our study was contingent on the experience of childhood adversity. Past studies have linked cumulative indices of adverse experiences to alcohol and drug use onset in adolescence and to drug abuse and addiction in adulthood.18,22 Our findings also are consistent with research conducted with animal models.31 When exposed as pups to social defeat, unresponsive parenting, and scarcity, adult rats exhibited a rapid progression from initial administration of a substance to addiction. Neuroscientists suggest that early adversity affects systems associated with the stress response, increasing reactivity to environmental risk factors.32 Early adversity alters systems associated with corticotropin releasing factor and the hypothalamic-pituitary-adrenal axis (CRF/HPA), extrahypothalamic CRF, autonomic arousal, and the central noradrenergic system. 21 These systems play roles in the development of both addiction and mood disorders.21,33,34
Although marijuana and alcohol use are quite common among young adults, the majority of users mature out of heavy substance use and experience few substance-related problems.1 Childhood adversity may be an important factor in understanding why some youth will continue to abuse substances. From a prevention and intervention perspective, a history of adverse childhood experiences suggests a focus on emotion regulation processes that may have been disrupted by a challenging childhood. Emotion regulation difficulties also may be complicated by normative pressures to fit in socially during a developmental phase in which many peers use substances. In general, for young people with challenging developmental histories, the same levels of substance use that characterize their peers may have significantly more pernicious effects on adjustment.
The focus of the present study on low-SES Black men has implications for understanding disparities in substance use consequences. Low-SES Black men experience heightened economic, social, and emotional consequences from using substances.4 Our findings suggest that childhood adversity may be a factor in these disparities. Low-SES Black men experience higher rates of adverse childhood experiences than do their peers from other racial and ethnic groups.20 To the extent that Black men experience greater adversity, normative increases in rates of substance use during the young adult years represents a unique threat to their wellbeing. Additional research with multiracial samples is needed to discover whether differential exposure to childhood adversity accounts for observed differences in the consequences of substance use. This would involve designs that specify childhood adversity as a mediator of the link between race/ethnicity and substance use consequences. In addition to childhood adversity, other factors warrant investigation in understanding racial disparities in the consequences of substance use for Black men. For example, extant studies document the influence of policing policies that target Black men on the high rates of drug and alcohol related arrests that they experience.35 Contextual risk factors, such as poverty and unemployment, also disproportionately affect Black men, potentially increasing the capacity for substance use to lead to negative consequences.4
A number of study limitations are noteworthy. The present study focused on rural Black men in the South; thus, the extent to which findings generalize to urban Black men is uncertain. Although cross-lagged analyses allowed examination of directions of effect, causal inferences using observational data require careful replication. Future research would benefit from the use of diagnostic and higher resolution assessments of the use of alcohol and other drugs. Finally, to inform findings regarding racial disparities in the consequences of substance use, future research is needed that can compare rates of early adversity across racial groups as a mediator of racial differences in substance use consequences.
Acknowledgments
Funding for this study was provided by Award Number R01 DA029488 to Steven M. Kogan and Award Number P30 DA027827 to Gene H. Brody, Center for Family Research, University of Georgia, from the National Institute on Drug Abuse, Rockville, MD.
We would like to thank Eileen Neubaum-Carlan, MS, for her editorial assistance.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 2.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future National Survey Results on Drug Use, 1975–2014: Volume 2, College Students and Adults Ages 19–55. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- 3.National Institute on Drug Abuse. Drug Use Among Racial/Ethnic Minorities, Revised. National Institutes of Health; 2003. [Google Scholar]
- 4.Zapolski TCB, Pedersen SL, McCarthy DM, Smith GT. Less drinking, yet more problems: understanding African American Drinking and related problems. Psychol Bull. 2014;140(1):188–223. doi: 10.1037/a0032113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watt TT. The race/ethnic age crossover effect in drug use and heavy drinking. J Ethn Subst Abuse. 2008;7(1):93–114. doi: 10.1080/15332640802083303. [DOI] [PubMed] [Google Scholar]
- 6.Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harvard Rev Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 7.Lembke A. Time to abandon the self-medication hypothesis in patients with psychiatric disorders. Am J Drug Alcohol Abuse. 2012;38(6):524–529. doi: 10.3109/00952990.2012.694532. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 9.Child Trends Data Bank. [Accessed July 15, 2009];Depressive symptoms among young adults. [WebPage] 2006 http://www.childtrendsdatabank.org/pdf/101_PDF.pdf.
- 10.Watkins DC. Depression over the adult life course for African American men: toward a framework for research and practice. Am J Men’s Health. 2012;6(3):194–210. doi: 10.1177/1557988311424072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsemann KM, Gee GC, Geronimus AT. Ethnic Differences in Trajectories of Depressive Symptoms: Disadvantage in Family Background, High School Experiences, and Adult Characteristics. J Health Soci Behav. 2009;50(1):82–98. doi: 10.1177/002214650905000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: analysis of the National Comorbidity Survey Replication. JAMA Psychiatry. 2013;70(10):1100–1106. doi: 10.1001/jamapsychiatry.2013.1985. [DOI] [PubMed] [Google Scholar]
- 13.Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clin Psychol Revi. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Green KM, Zebrak KA, Robertson JA, Fothergill KE, Ensminger ME. Interrelationship of substance use and psychological distress over the life course among a cohort of urban African Americans. Drug Alcohol Depende. 2012;123(1–3):239–248. doi: 10.1016/j.drugalcdep.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birkley EL, Zapolski TCB, Smith GT. Racial Differences in the Transactional Relationship Between Depression and Alcohol Use From Elementary School to Middle School. J Stud Alcohol Drugs. 2015;76(5):799–808. doi: 10.15288/jsad.2015.76.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sher KJ, Bartholow BD, Peuser K, Erickson DJ, Wood MD. Stress-Response-Dampening Effects of Alcohol: Attention as a Mediator and Moderator. J Abnorm Psychol. 2007;116(2):362–377. doi: 10.1037/0021-843X.116.2.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koob GF. Negative reinforcement in drug addiction: the darkness within. Curr Opin Neurobiol. 2013;23:559–563. doi: 10.1016/j.conb.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 18.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the Adverse Childhood Experiences Study. Pediatrics. 2003;111(3):564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 19.Child Trends. Adverse Experiences: Indicators on children and youth. [Accessed July 2013]. [Google Scholar]
- 20.Slopen N, Shonkoff JP, Albert MA, et al. Racial disparities in child adversity in the U.S.: interactions with family immigration history and income. Am J Prev Med. 2016;50(1):47–56. doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141(1):105–130. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers B, McLaughlin KA, Wang S, Blanco C, Stein DJ. Associations between childhood adversity, adult stressful life events, and past-year drug use disorders in the National Epidemiological Study of Alcohol and Related Conditions (NESARC) Psychol Addict Behav. 2014;28(4):1117–1126. doi: 10.1037/a0037459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salgado-Pineda P, Delaveau P, Blin O, Nieoullon A. Dopaminergic contribution to the regulation of emotional perception. Clin Neuropharmacol. 2005;28(5):228–237. doi: 10.1097/01.wnf.0000185824.57690.f0. [DOI] [PubMed] [Google Scholar]
- 24.Crockett LJ, Carlo G, Temmen C. Rural Ethnic Minority Youth and Families in the United States. New York, NY: Springer; 2016. Ethnic and racial minority youth in the rural United States: an overview; pp. 1–12. [Google Scholar]
- 25.Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Soc Probl. 2002;49(1):11–34. [Google Scholar]
- 26.Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35(1):217–238. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 28.Joe GW, Broome KM, Rowan-Szal GA, Simpson DD. Measuring patient attributes and engagement in treatment. J Subst Abuse Treat. 2002;22(4):183–196. doi: 10.1016/s0740-5472(02)00232-5. [DOI] [PubMed] [Google Scholar]
- 29.Mplus user’s guide [computer program]. Version 7.0. Los Angeles, CA: Stat Model; 2008–2012. [Google Scholar]
- 30.Kogan SM, Cho J, Simons LG, et al. Pubertal timing and sexual risk behaviors among rural African American male youth: testing a model based on life history theory. Arch Sex Behav. 2015;44(3):609–618. doi: 10.1007/s10508-014-0410-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bardo M, Neisewander J, Kelly T. Individual differences and social influences on the neurobehavioral pharmacology of abused drugs. Pharmacol Rev. 2013;65(1):255–290. doi: 10.1124/pr.111.005124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goeders NE. The impact of stress on addiction. Eur Neuropsychopharmacol. 2003;13(6):435–441. doi: 10.1016/j.euroneuro.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 33.Chen FR, Raine A, Soyfer L, Granger DA. Interaction of adrenocortical activity and autonomic arousal on children’s externalizing and internalizing behavior problems. J Abnorm Child Psychol. 2015;43(1):189–202. doi: 10.1007/s10802-014-9900-y. [DOI] [PubMed] [Google Scholar]
- 34.Heim C, Nemeroff CB. The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biol Psychiatry. 1999;46(11):1509–1522. doi: 10.1016/s0006-3223(99)00224-3. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell O, Caudy MS. Examining racial disparities in drug arrests. Justice Q. 2015;32(2):288–313. [Google Scholar]