Abstract
Introduction: PrEP awareness and uptake among men who have sex with men (MSM) and transgender women (TG) in Thailand remains low. Finding ways to increase HIV testing and PrEP uptake among high-risk groups is a critical priority. This study evaluates the effect of a novel Adam’s Love Online-to-Offline (O2O) model on PrEP and HIV testing uptake among Thai MSM and TG and identifies factors associated with PrEP uptake.
Methods: The O2O model was piloted by Adam’s Love (www.adamslove.org) HIV educational and counselling website. MSM and TG reached online by PrEP promotions and interested in free PrEP and/or HIV testing services contacted Adam’s Love online staff, received real-time PrEP eCounseling, and completed online bookings for receiving services at one of the four sites in Bangkok based on their preference. Auto-generated site- and service-specific e-tickets and Quick Response (QR) codes were sent to their mobile devices enabling monitoring and check-in by offline site staff. Service uptake and participant’s socio-demographic and risk behaviour characteristics were analyzed. Factors associated with PrEP uptake were assessed using multiple logistic regression.
Results: Between January 10th and April 11th, 2016, Adam’s Love reached 272,568 people online via the PrEP O2O promotions. 425 MSM and TG received eCounseling and e-tickets. There were 325 (76.5%) MSM and TG who checked-in at clinics and received HIV testing. Nine (2.8%) were diagnosed with HIV infection. Median (IQR) time between receiving the e-ticket and checking-in was 3 (0–7) days. Of 316 HIV-negative MSM and TG, 168 (53.2%) started PrEP. In a multivariate model, higher education (OR 2.30, 95%CI 1.14–4.66; p = 0.02), seeking sex partners online (OR 2.05, 95%CI 1.19–3.54; p = 0.009), being aware of sexual partners’ HIV status (OR 2.37, 95%CI 1.29–4.35; p = 0.008), ever previously using post-exposure prophylaxis (PEP) (OR 2.46, 95%CI 1.19–5.09; p = 0.01), and enrolment at Adam’s Love clinic compared to the other three sites (OR 3.79, 95%CI 2.06–6.95; p < 0.001) were independently associated with PrEP uptake.
Conclusions: Adam’s Love O2O model is highly effective in linking online at-risk MSM and TG to PrEP and HIV testing services, and has high potential to be replicated and scaled up in other settings with high Internet penetration among key populations.
Keywords: pre-exposure prophylaxis, PrEP scale up, PrEP uptake, Thailand, MSM, transgender women, technology, innovative model
Introduction
Thailand’s explosive HIV epidemic among men who have sex with men (MSM) and transgender women (TG) remains a major public health concern. In Bangkok, one in every three MSM are estimated to be HIV-positive [1] and HIV incidence rates, especially among young MSM (YMSM) aged 18–21 years, are alarmingly high (12.2 per 100 person years) [2]. Prevalence estimates from studies on Thai TG range from 10% to 17% [3–5]. Thailand aims to end the AIDS epidemic by 2030 and modelling showed the only way to achieve this goal is to increase HIV testing to cover 90% of key populations, to treat all HIV cases with antiretroviral therapy (ART) regardless of CD4 count [6], and to harness and maximize the use of innovative biomedical HIV prevention tools, such as pre-exposure prophylaxis (PrEP) for most-at risk populations.
PrEP, with daily use of a fixed-dose combination tablet of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC) is a safe, effective method of preventing HIV among MSM and TG [7–11]. The WHO Consolidated guidelines on HIV testing, treatment, and prevention call for expanded access to PrEP for all individuals who are at substantial ongoing risk of acquiring HIV, provisionally defined as an incidence of HIV greater than three per 100 person-years [12]. Given incidence rates and sexual and drug use risk behaviours among Thai MSM and TG [2,13], increasing uptake of PrEP is a critical priority.
Thailand was one of the first Asian countries to participate in PrEP clinical trials and implementation projects [14–17]. A number of demonstration projects are currently underway. To date, Thailand has relied heavily on traditional outreach models for PrEP scale up and delivery, despite inherent challenges with engaging hard to reach and closeted MSM [17,18]. A recent programme conducted under the Thailand Global Fund for AIDS, Tuberculosis and Malaria found that only 7% of MSM reached through offline outreach received HIV testing [19], a critical first step to confirm an HIV-negative status prior to initiation of PrEP and reduce the risk of drug resistance. The rate of annual HIV testing among the Thai MSM population, which is estimated to contribute to 40% of country’s new HIV cases during 2012–2016, is also very low at merely 29% [20,21]. HIV counselling and testing is a point of engagement into the HIV prevention continuum offering providers’ opportunities to foster bi-directional communication with clients, assess risks, introduce PrEP as one method in the combination HIV prevention package and encourage uptake. Lack of HIV testing and repeat testing of those at high risk of HIV infection remains the first and most critical barrier to PrEP awareness and subsequent PrEP uptake.
There is limited data on PrEP awareness among Thai MSM and TG communities and among those who are aware of PrEP multiple barriers to PrEP uptake still exist. In a study conducted in 2013 by Sineath et al., only few respondents (7%) reported having heard of PrEP [22]. However, Thai MSM have indicated a willingness to take PrEP, even if they had to experience inconvenience and expense [23]. Thus, finding ways to identify those individuals at highest risk through innovative and scalable testing methodologies, and seamlessly transitioning them into biomedical prevention services is needed. Particularly, extending outreach to include online venues is vital considering that Thai MSM and TG have some of the highest internet and technology utilization [24].
Adam’s Love website
Adam’s Love (www.adamslove.org), a technology-based HIV outreach, counselling and testing initiative in Asia for MSM and TG individuals, was launched in September 2011 by the Thai Red Cross AIDS Research Centre (TRCARC) and has demonstrated success in scaling-up HIV testing in Thailand and Indonesia [25–27]. Adam’s Love comprises of an HIV educational website, eCounseling platforms and integrated social media networks. Since its launch, Adam’s Love engaged more than 2.8 million website visitors. An estimated 17,357 MSM and TG individuals received real-time counselling at Adam’s Love eCounseling platforms and were successfully linked to relevant clinical services, for example, HIV and sexually transmitted infection (STI) testing, treatment, and care and post-exposure prophylaxis (PEP) [28]. Of MSM and TG clients who annually received HIV testing at TRCARC, an estimated 25% were recruited online via Adam’s Love and an HIV prevalence of 15.5% was reported in 2015 [25].
Gap that emerged in terms of connecting online visitors with critical offline clinical services
Previous efforts by Adam’s Love included online HIV testing and MSM/TG health promotions, eCounseling support and linkage to relevant clinical services, with limited focus on PrEP. Additionally, MSM and TG eCounseled and linked to offline sites had to start over the process of explaining their risk behaviours and service preference to the clinic reception staff. This often led to reluctance, confidentially concerns and fragmented experiences.
Our study evaluates the effect of a novel Online-to-Offline (O2O) model, piloted by Adam’s Love (www.adamslove.org) HIV educational and counselling website, on PrEP and HIV testing uptake among Thai MSM and TG.
Methods
Adam’s Love O2O model
Adam’s Love O2O model included three key features:
(a) tailored social media PrEP promotions including PrEP educational content, and photos/videos of Thai male celebrities and MSM and TG community promoting Adam’s Love non-financial incentives (i.e. bags, caps and T-shirts) for individuals receiving free PrEP and/or HIV testing services at clinic sites.
(b) refined eCounseling intervention to provide PrEP eCounseling support on Adam’s Love platforms (i.e. web message boards, popular social media and instant messaging applications with text and live video chat, and media sharing capabilities) and assess the risks of those eCounseled by asking a set of standardized questions (Appendix 1) including age; ever having an anal intercourse; number of sexual partners, condom use during anal sex and HIV testing in the past six months; and date of last possible HIV risk exposure.
(c) a free online booking system to facilitate effective linkage to relevant offline clinical services and a real-time monitoring feature to track individuals successfully linked to sites.
In January 2016, Adam’s Love set out to explore the potential of its O2O model (Figure 1) for PrEP scale up among Thai MSM and TG to test and ascertain the most appropriate approaches to the expansion of PrEP services in Thailand and other countries with widespread internet access and an educated population.
Figure 1.
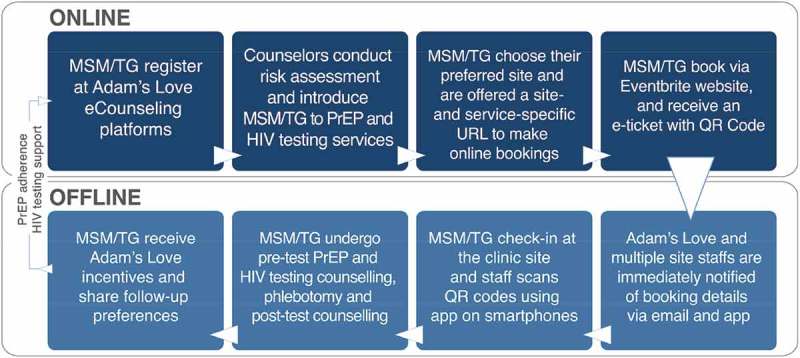
The Adam’s Love Online-to-Offline (O2O) model for PrEP and HIV testing scale up.
The O2O model includes eight steps: (1) MSM and TG people register at Adam’s Love eCounseling platforms and contact online counsellors, (2) Adam’s Love online counsellors conduct an individualized risk assessment by asking a set of standardized questions (consistent for all participants), introduce them to relevant PrEP and HIV testing services and enrol them in the study, (3) participants then prioritize their preferred site for receiving service and are offered a site- and service-specific booking URL to make online bookings, (4) participants register for free via Eventbrite (EVB) website, chose their preferred date and check-in time for their specified service and receive an email confirmation with an e-ticket with a QR code confirming the time and date of the booking, and a reminder email one day prior to the check-in date, (5) Adam’s Love site staff are immediately notified of the booking details via email and through the EVB app once a booking is made, (6) participants check-in at the clinic site and staff scans the QR codes (print or digital) on tickets using smartphone devices or manually via electronic lists, and a green bar appears next to the attendee’s order indicating that they’ve been successfully checked in, (7) participants undergo pre-test HIV testing counselling, phlebotomy and post-test counselling. If negative, PrEP is provided and (8) participants receive Adam’s Love merchandise (e.g. t-shirts, caps, tote bags), and share their preferred online platform, content and frequency for adherence or testing reminders.
Clinical partners
Adam’s Love launched a three-month pilot programme to enrol MSM and TG into free PrEP and HIV testing services at four sites in Bangkok including TRCARC Anonymous Clinic, Adam’s Love Clinic (an MSM and TG-focused and by-online-appointment only clinic operated by TRCARC) and two community-based drop-in centres including Rainbow Sky Association of Thailand (RSAT) which targeted MSM and TG and Service Workers In Group (SWING) Foundation which targeted male sex workers. The two drop-in centres provided PrEP as part of “community-led HIV services” run solely by non-medical community staff, who were trained and coached to perform counselling, rapid HIV and syphilis testing, sample collection for STI screening, PEP and PrEP prescription, case management, and adherence and retention support for both HIV-positive clients and HIV-negative clients. The non-medical community staff received ongoing quality assessment and quality improvement by the TRCARC. PrEP medication was free for participants in this programme through the Thai Red Cross Princess Soamsawali Prevention Fund.
Pilot test of O2O
MSM and TG reached online by O2O PrEP social media promotions (Supplementary Figure 1) and interested in free PrEP and/or HIV testing services contacted Adam’s Love online staff, received real-time PrEP eCounseling, were assessed for risks through a set of standardized questions (Appendix 1) and enrolled at one of the four sites in Bangkok based on their preference. Participants prioritized their preferred service and clinic site during the eCounseling session and were provided a site- and service-specific booking URL. Participants made free online bookings via the Eventbrite (EVB) application (app) – www.eventbrite.com, a self-service ticketing platform and received an auto-generated email confirming the booking summary, a downloadable and a Portable Document Format (PDF) attachment of an e-ticket with booking details, maps and directions to the clinic site, barcodes and a Quick Response (QR) code. The codes were later scanned using the EVB Organizer mobile app at check-in by offline site staff using smartphone devices. Adam’s Love and site staff would receive an e-ticket order number in an email each time a booking was made, and could track check-in data in real time and monitor live check-in statistics from the “Dashboard” within the app. A timestamp captured the time gap between placing the online order and check-in date at the offline site (Figure 1).
Data collected at the clinic site through participant-completed online questionnaires included socio-demographic and risk behaviour data such as age, education, income, sexual identity, social media usage and online sex seeking behaviour, HIV/STI test history, condom use, number of sexual partners and drug use (including alcohol, popper, ecstasy, cannabis, cocaine, methamphetamine, ketamine, LSD, and heroine) in the past 6 months. Online metrics included page views, reach (number of people who saw the promotions), number of orders, daily tickets ordered, attendee geolocation, order and attendance time, no-show rates and clinic site attended. Clinical and laboratory data included HIV testing and PrEP uptake and HIV test results.
All participants in the O2O programme were designated male at birth, reported having had anal intercourse with men, and were aged 18 years or above. Consent was provided online. Participants who tested positive for HIV were not eligible for PrEP. The study protocol was approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Chulalongkorn University in Bangkok, Thailand.
Statistical analysis
The total number of people reached through O2O PrEP promotions was measured using web and social media analytics tools including YouTube (www.youtube.com) analytics and Facebook (www.facebook.com) page insights.
Statistical analysis was conducted with Stata 14 (StataCorp LP, College Station, TX, USA). Descriptive statistics were used to summarize mean (SD), median (IQR) for continuous variables; frequency and percentage for categorical variables. Site characteristics were compared using a one-way ANOVA or Kruskal–Wallis test for continuous variables and categorical variables were tested a Chi-squared test or Fisher’s exact test, as appropriate. Multiple logistic regression was used to identify factors associated with the uptake of PrEP among all HIV-negative participants who made their visit. Covariates modelled included programme details such as time interval between ordering the e-ticket and actual check in, socio-demographics, patterns of social media use, self-reported risk behaviour and history of STIs. Factors significant at p ≤ 0.1 in univariate analysis were adjusted for in a multivariate model.
Results
Between January 10th and April 11th, 2016, Adam’s Love reached 272,568 people online via PrEP O2O social media promotions. 425 MSM and TG received eCounseling, made online bookings, and received QR codes and e-tickets. There were 325 (76.5%) MSM and TG who checked-in at one of the four study clinics and received HIV testing, Nine (2.8%) were diagnosed with HIV infection. Median age of participants was 27 years (IQR: 23–33), most (77.2%) had at least a high school education, majority (61.8%) had monthly income above 500 USD, most (77.9%) self-identified as gay and more than half (56.9%) hid their sexual identity. Almost a quarter of the participants (22.8%) had more than five sexual partners in the past six months, 26.8% reported ever having had an STI, almost half (48.1%) had sometimes or never used condoms in the past six months and less than one-third (30.2%) were aware of sexual partners HIV status. More than one-third of the participants (35.4%) had used drugs in the past six months of whom almost a quarter (21.7%) were amphetamine-type stimulants (ATS) users. Almost half (46.8%) of the participants were aware of PEP as an HIV prevention method of whom more than one-third (34.2%) had used PEP in the past. The majority (52.6%) spent more than seven hours per day using social media and almost one-third (32.6%) reported having sought sexual partners online.
Median (IQR) time between receiving e-ticket and check-in was 3 (0–7) days. Most participants (44%) checked in and received services at TRCARC Anonymous Clinic, one-third (34.1%) at Adam’s Love clinic, and the rest (21.9%) at the two community-based clinics. PrEP uptake was highest (70.4%) at Adam’s Love clinic compared with 46.8% at TRCARC Anonymous Clinic and 39.1% at community-based clinics (p < 0.001). Median age (IQR), having ever been tested for HIV, STI rates, social media usage and online sex seeking behaviour were similar among participants at all sites. Participants at TRCARC Anonymous Clinic and Adam’s Love clinic were higher educated (p < 0.001), had higher income (p < 0.001), were less likely to have lifetime sexual relationship with both male and female (p = 0.004) or currently be in relationship with both male and female (p = 0.006) and had fewer sexual partners in the past six months (p = 0.03) than those at the community-based clinics. Adam’s Love and community-based clinic participants were more likely to be based in Bangkok (p < 0.001), less likely to be aware of their sexual partner’s HIV status (p = 0.006) and less likely to have received an HIV test in the past six months (p = 0.001) than TRCARC Anonymous Clinic participants. Although not statistically significant, drug use behaviour was highest (45%) among participants at community-based clinics (Table 1).
Table 1.
Descriptive characteristics of all participants
| Characteristics N (%) |
All sites (N = 325) | Adam’s Love clinic (N = 111) | TRCARC clinic (N = 143) | Community-based sites (N = 71) | p-Value |
|---|---|---|---|---|---|
| Days between ticket and check-in | |||||
| Median (IQR) | 3 (0–7) | 4 (2–8) | 4 (1–8) | 0 (0–0) | <0.001b |
| Min, Max | 0, 45 | 0, 33 | 0, 45 | 0, 21 | |
| Monthly check-in (visits)e | <0.001c | ||||
| Month 1 | 77 (23.7) | 27 (24.3) | 40 (28.0) | 10 (14.1) | |
| Month 2 | 94 (28.9) | 16 (14.4) | 41 (28.7) | 37 (52.1) | |
| Month 3 | 154 (47.4) | 68 (61.3) | 62 (43.3) | 24 (33.8) | |
| HIV test result | >0.99d | ||||
| Negative | 316 (97.2) | 108 (97.3) | 139 (97.2) | 69 (97.2) | |
| Positive | 9 (2.8) | 3 (2.7) | 4 (2.8) | 2 (2.8) | |
| PrEP uptake among HIV-negative participants | <0.001c | ||||
| Non-PrEP users (HIV testers) | 148 (46.8) | 32 (29.6) | 74 (53.2) | 42 (60.9) | |
| PrEP users | 168 (53.2) | 76 (70.4) | 65 (46.8) | 27 (39.1) | |
| Age (years) | |||||
| Mean (SD) | 28.5 (7.4) | 28.6 (7.5) | 27.8 (7.2) | 29.8 (7.8) | 0.19a |
| Median (IQR) | 27 (23–33) | 27 (23–34) | 27 (23–32) | 28 (24–34) | |
| Age group | 0.84c | ||||
| ≤18 | 16 (4.9) | 6 (5.4) | 8 (5.6) | 2 (2.8) | |
| 19–24 | 93 (28.6) | 31 (27.9) | 45 (31.5) | 17 (23.9) | |
| 25–34 | 150 (46.2) | 52 (46.9) | 63 (44.1) | 35 (49.3) | |
| >34 | 66 (20.3) | 22 (19.8) | 27 (18.9) | 17 (23.9) | |
| Current residence | <0.001c | ||||
| Outside Bangkok | 37 (11.4) | 7 (6.3) | 29 (20.3) | 1 (1.4) | |
| Bangkok Metropolitan Region | 288 (88.6) | 104 (93.7) | 114 (79.7) | 70 (98.6) | |
| Education level | <0.001c | ||||
| High school or below | 74 (22.8) | 15 (13.5) | 18 (12.6) | 41 (57.8) | |
| Above High school | 251 (77.2) | 96 (86.5) | 125 (87.4) | 30 (42.3) | |
| Monthly income | <0.001c | ||||
| No salary as studying | 59 (18.2) | 16 (14.4) | 36 (25.2) | 7 (9.9) | |
| No salary as unemployed | 15 (4.6) | 0 (0) | 7 (4.9) | 8 (11.3) | |
| ≤500 USD | 50 (15.4) | 10 (9) | 14 (9.8) | 26 (36.6) | |
| 501–1,000 USD | 132 (40.6) | 48 (43.2) | 58 (40.6) | 26 (36.6) | |
| >1,000 USD | 69 (21.2) | 37 (33.3) | 28 (19.6) | 4 (5.6) | |
| Self-identified sexuality | <0.001c | ||||
| Gay | 253 (77.9) | 97 (87.4) | 115 (80.4) | 41 (57.8) | |
| Bisexual | 39 (12) | 10 (9) | 18 (12.6) | 11 (15.5) | |
| Transgender | 17 (5.2) | 2 (1.8) | 7 (4.9) | 8 (11.3) | |
| Male | 16 (4.9) | 2 (1.8) | 3 (2.1) | 11 (15.5) | |
| Disclosure status of gender identity | 0.58c | ||||
| Discreet (hidden) | 63 (19.4) | 21 (18.9) | 27 (18.9) | 15 (21.1) | |
| Open to some | 122 (37.5) | 42 (37.8) | 59 (41.3) | 21 (29.6) | |
| Open to all (out) | 140 (43.1) | 48 (43.2) | 57 (39.9) | 35 (49.3) | |
| Lifetime sexual relationships with which genders? | 0.004d | ||||
| Male only | 233 (71.7) | 89 (80.2) | 104 (72.7) | 40 (56.3) | |
| Male and female | 81 (24.9) | 20 (18) | 33 (23.1) | 28 (39.4) | |
| Female and TG | 5 (1.5) | 2 (1.8) | 3 (2.1) | 0 (0) | |
| Male and TG | 1 (0.3) | 0 (0) | 1 (0.7) | 0 (0) | |
| All (male, female, TG) | 5 (1.5) | 0 (0) | 2 (1.4) | 3 (4.2) | |
| Current sexual relationships with which genders? | 0.006d | ||||
| Male only | 277 (85.2) | 101 (91) | 125 (87.4) | 51 (71.8) | |
| Female only | 8 (2.5) | 1 (0.9) | 4 (2.8) | 3 (4.2) | |
| TG | 3 (0.9) | 0 (0) | 2 (1.4) | 1 (1.4) | |
| Male and female | 32 (9.9) | 7 (6.3) | 11 (7.7) | 14 (19.7) | |
| Female and TG | 3 (0.9) | 2 (1.8) | 1 (0.7) | 0 (0) | |
| All (male, female, TG) | 2 (0.6) | 0 (0) | 0 (0) | 2 (2.8) | |
| Ever tested for HIV | 0.80c | ||||
| No | 59 (18.2) | 21 (18.9) | 27 (18.9) | 11 (15.5) | |
| Yes | 266 (81.9) | 90 (81.1) | 116 (81.1) | 60 (84.5) | |
| Previous HIV test | 0.001c | ||||
| ≤1 month | 92 (28.3) | 18 (16.2) | 58 (40.6) | 16 (22.5) | |
| 1–6 months | 53 (16.3) | 24 (21.6) | 15 (10.5) | 14 (19.7) | |
| 6 months–1 year | 84 (25.9) | 38 (34.2) | 26 (18.2) | 20 (28.2) | |
| >1 year | 31 (9.5) | 10 (9) | 14 (9.8) | 7 (9.9) | |
| Never tested for HIV/can’t remember | 65 (20) | 21 (18.9) | 30 (21) | 14 (19.7) | |
| Ever had an STI | 0.57c | ||||
| No | 208 (64) | 67 (60.4) | 96 (67.1) | 45 (63.4) | |
| Yes | 87 (26.8) | 34 (30.6) | 32 (22.4) | 21 (29.6) | |
| Don’t know/never tested | 30 (9.2) | 10 (9) | 15 (10.5) | 5 (7) | |
| Time using social media per day | 0.19c | ||||
| 1–3 h a day | 44 (13.5) | 11 (9.9) | 19 (13.3) | 14 (19.7) | |
| 3–7 h a day | 110 (33.9) | 33 (29.7) | 53 (37.1) | 24 (33.8) | |
| >7 h a day | 171 (52.6) | 67 (60.4) | 71 (49.7) | 33 (46.5) | |
| Ever seek sexual partners online | 0.46c | ||||
| No | 219 (67.4) | 78 (70.3) | 98 (68.5) | 43 (60.6) | |
| Yes | 106 (32.6) | 33 (29.7) | 45 (31.5) | 28 (39.4) | |
| Number of sexual partners in the past 6 months | 0.03d | ||||
| Didn’t have sex in past 6 months | 10 (3.1) | 3 (2.7) | 5 (3.5) | 2 (2.8) | |
| One | 83 (25.5) | 26 (23.4) | 42 (29.4) | 15 (21.1) | |
| 2–5 | 158 (48.6) | 65 (58.6) | 66 (46.2) | 27 (38) | |
| 5–10 | 38 (11.7) | 11 (9.9) | 14 (9.8) | 13 (18.3) | |
| >10 | 36 (11.1) | 6 (5.4) | 16 (11.2) | 14 (19.7) | |
| Condom use in the past 6 months | 0.48d | ||||
| Didn’t have sex in past 6 months/refused to answer | 13 (4) | 3 (2.7) | 8 (5.6) | 2 (2.8) | |
| Always | 156 (48) | 49 (44.1) | 66 (46.2) | 41 (57.8) | |
| Sometimes | 137 (42.2) | 51 (46) | 60 (42) | 26 (36.6) | |
| Never | 19 (5.9) | 8 (7.2) | 9 (6.3) | 2 (2.8) | |
| Sexual partners’ HIV status awareness | 0.006c | ||||
| No | 167 (51.4) | 61 (55) | 62 (43.4) | 44 (62) | |
| Yes | 98 (30.2) | 25 (22.5) | 58 (40.6) | 15 (21.1) | |
| Never ask | 60 (18.5) | 25 (22.5) | 23 (16.1) | 12 (16.9) | |
| Substance use in past 6 months (including alcohol) | 0.11c | ||||
| No | 210 (64.6) | 78 (70.3) | 93 (65) | 39 (54.9) | |
| Yes | 115 (35.4) | 33 (29.7) | 50 (35) | 32 (45.1) | |
| Amphetamine-type stimulants | 0.06c | ||||
| No | 300 (92.3) | 106 (95.5) | 133 (93) | 61 (85.9) | |
| Yes | 25 (7.7) | 5 (4.5) | 10 (7) | 10 (14.1) | |
| Aware of PEP as an HIV prevention method | 0.07c | ||||
| No | 173 (53.2) | 50 (45.1) | 85 (59.4) | 38 (53.5) | |
| Yes | 152 (46.8) | 61 (55) | 58 (40.6) | 33 (46.5) | |
| Ever used PEP | 0.80c | ||||
| No | 273 (84) | 95 (85.6) | 118 (82.5) | 60 (84.5) | |
| Yes | 52 (16) | 16 (14.4) | 25 (17.5) | 11 (15.5) |
aOne-way ANOVA.
bKruskal–Wallis.
cChi-square test.
dFisher’s exact test.
eMonthly check-in refers to the number of participants checked in and accessing HIV testing and PrEP services in each month.
Of 316 HIV-negative MSM and TG, 168 (53.2%) decided to start PrEP. In a multivariate model adjusting for income and ever having tested for HIV, higher education (OR 2.30, 95%CI 1.14–4.66; p = 0.02), seeking sex partners online (OR 2.05, 95%CI 1.19–3.54; p = 0.009), being aware of sexual partners’ HIV status (OR 2.37, 95%CI 1.29–4.35; p = 0.008), ever previously using PEP (OR 2.46, 95%CI 1.19–5.09; p = 0.01), and enrolment at Adam’s Love clinic (OR 3.79, 95%CI 2.06–6.95; p < 0.001) were independently associated with PrEP uptake. Past STI history, anal sex role, condom use, number of sexual partners and drug use in the past 6 months were not associated with PrEP uptake (Table 2).
Table 2.
Logistic regression model of factors associated with using PrEP among all HIV-negative participants who made their visit. (Factors significant at p ≤ 0.1 in univariate analysis were adjusted for in a multivariate model)
| Non-PrEP users (n = 148) |
PrEP users (n = 168) |
Univariate |
Multivariate |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | freq | % | freq | % | OR | 95%C.I. | p-Value | OR | 95%C.I. | p-Value |
| Days between ticket and check-in | 0.56 | |||||||||
| <4 | 85 | 57% | 91 | 54% | 1 | ref | ||||
| ≥4 | 63 | 43% | 77 | 46% | 1.14 | 0.73–1.78 | ||||
| Service delivery site | <0.001 | <0.001 | ||||||||
| TRCARC clinic | 74 | 50% | 65 | 39% | 1 | ref | 1 | ref | ||
| Adam’s Love clinic | 32 | 22% | 76 | 45% | 2.70 | 1.59–4.60 | 3.79 | 2.06–6.95 | ||
| Community-based sites | 42 | 28% | 27 | 16% | 0.73 | 0.41–1.32 | 1.13 | 0.54–2.33 | ||
| Education level | <0.001 | 0.02 | ||||||||
| High school or below | 49 | 33% | 23 | 14% | 1 | ref | 1 | ref | ||
| Above High school | 99 | 67% | 145 | 86% | 3.12 | 1.79–5.45 | 2.30 | 1.14–4.66 | ||
| Monthly income | 0.003 | 0.45 | ||||||||
| No salary as studying/unemployed | 43 | 29% | 30 | 18% | 1 | ref | 1 | ref | ||
| ≤500 USD | 29 | 20% | 18 | 11% | 0.89 | 0.42–1.88 | 1.10 | 0.47–2.61 | ||
| 501–1000 USD | 50 | 34% | 79 | 47% | 2.26 | 1.26–4.07 | 1.43 | 0.74–2.76 | ||
| >1000 USD | 26 | 18% | 41 | 24% | 2.26 | 1.15–4.45 | 0.85 | 0.39–1.87 | ||
| Ever tested for HIV | 0.01 | >0.99 | ||||||||
| No | 35 | 24% | 22 | 13% | 1 | ref | 1 | ref | ||
| Yes | 113 | 76% | 146 | 87% | 2.05 | 1.14–3.70 | 1.002 | 0.42–2.39 | ||
| Ever had any STI | 0.40 | |||||||||
| No | 99 | 67% | 106 | 63% | 1 | ref | ||||
| Yes | 34 | 23% | 49 | 29% | 1.35 | 0.80–2.26 | ||||
| Don’t know/never tested | 15 | 10% | 13 | 8% | 0.81 | 0.37–1.79 | ||||
| Ever seek sexual partners online | 0.02 | 0.009 | ||||||||
| No | 109 | 74% | 103 | 61% | 1 | ref | 1 | ref | ||
| Yes | 39 | 26% | 65 | 39% | 1.76 | 1.09–2.85 | 2.05 | 1.19–3.54 | ||
| Number of sexual partners in the past 6 months | 0.60 | |||||||||
| 0–1 | 44 | 30% | 46 | 27% | 1 | ref | ||||
| 2–5 | 72 | 49% | 80 | 48% | 1.06 | 0.63–1.79 | ||||
| 5–10 | 19 | 13% | 19 | 11% | 0.96 | 0.45–2.04 | ||||
| >10 | 13 | 9% | 23 | 14% | 1.69 | 0.76–3.75 | ||||
| Anal sex role | 0.78 | |||||||||
| Insertive | 52 | 35% | 67 | 40% | 1 | ref | ||||
| Receptive | 39 | 26% | 45 | 27% | 0.89 | 0.51–1.57 | ||||
| Both | 48 | 32% | 47 | 28% | 0.76 | 0.44–1.30 | ||||
| Didn’t have sex | 9 | 6% | 9 | 5% | 0.78 | 0.29–2.09 | ||||
| Condom use in the past 6 months | 0.50 | |||||||||
| Always/didn’t have sex | 73 | 49% | 91 | 54% | 1 | ref | ||||
| Sometimes | 64 | 43% | 69 | 41% | 0.86 | 0.55–1.37 | ||||
| No | 11 | 7% | 8 | 5% | 0.58 | 0.22–1.52 | ||||
| Sexual partners’ HIV status awareness | 0.004 | 0.008 | ||||||||
| No | 81 | 55% | 81 | 48% | 1 | ref | 1 | ref | ||
| Yes | 33 | 22% | 64 | 38% | 1.94 | 1.15–3.26 | 2.37 | 1.29–4.35 | ||
| Never ask | 34 | 23% | 23 | 14% | 0.68 | 0.37–1.25 | 0.77 | 0.38–1.52 | ||
| Substance use in past 6 months (including alcohol) | 0.28 | |||||||||
| No | 101 | 68% | 105 | 63% | 1 | ref | ||||
| Yes | 47 | 32% | 63 | 38% | 1.29 | 0.81–2.06 | ||||
| Ever used PEP | <0.001 | 0.01 | ||||||||
| No | 135 | 91% | 129 | 77% | 1 | ref | 1 | ref | ||
| Yes | 13 | 9% | 39 | 23% | 3.14 | 1.6–6.15 | 2.46 | 1.19–5.09 | ||
Discussions
Previously conducted studies have mostly focused on PrEP awareness, PrEP acceptability, and willingness among MSM and TG groups and the barriers and facilitators [29]. We demonstrated for the first time that a novel O2O model could reach high-risk, closeted MSM and TG individuals and successfully bridge online outreach to offline uptake of HIV testing and PrEP services.
Greater attention should be placed on increasing PrEP awareness through public health campaigns targeting MSM with high-risk behaviours [30]. In our study, tailored social media promotions successfully reached a large number of Thai MSM and TG groups, a critical challenge faced by traditional and one-on-one outreach models. Of the large number of people who saw the promotions, 0.16% actively contacted counsellors and engaged in eCounseling. Participation in social media implies an excess effort to act on the promotional post compared with seeing the post and could have been low due to multiple factors such as content type, day/timing of promotion or divided attention [31,32]. It is also possible that only motivated individuals contemplating behaviour change [33] or seeking new HIV prevention methods participated in eCounseling. Access to and capacity of eCounseling were not determining factors in limited uptake as all possible efforts were made to ensure prompt responses and establish dialogue same day an inquiry was made.
The community-based sites staff with Internet-enabled and EVB app-installed smartphones promoted free PrEP and encouraged online bookings as part of their daily face-to-face outreach activities in various hotspot areas, leading to mostly same day check-ins at community-based sites. Internet access or literacy was not reported as a challenge by either staff or client. More efforts and trainings to strengthen community-based site staffs’ online outreach and scheduling capabilities are needed.
Some MSM self-identify as straight male, especially if they also have sex with women, are married, take insertive role in anal sex [34], and/or have sex with men for money [35]. This identity was commonly selected at community-based sites with the highest number of discreet participants. It is also possible that these included low income straight-identified MSM who engaged in transactional sex.
Several studies have found that one of the biggest barriers to the provision of PrEP are the reticence of healthcare providers [36–39] and suggested that PrEP programmes need to be coupled with HIV risk management counselling in stigma-free settings [40]. Real-time eCounseling and support by Adam’s Love experienced and trained counsellors helped foster relationships with MSM and TG individuals reached online, assess individuals at risk for HIV infection, provide basic education about PrEP and how to access it in virtual non-judgmental settings. This may have helped reduce social, structural and individual-level barriers before enrolling them into actual clinical services. Online booking process involved entering a preferred pseudonym and a valid email address. No additional personal identifying information was needed to enter the programme and helped overcome participant confidentiality and privacy concerns, a critical barrier to accessing sexual health services among Thai MSM and TG [41]. Use of technology with real-time monitoring features helped track, validate participants and identify participants’ choice of service. Such innovative monitoring approaches could help fill significant programmatic gaps in tracking individuals through Thailand’s Reach-Recruit-Test-Treat-Retain cascade [42].
A majority of those who made online bookings and received e-tickets (76.4%), actually checked in to receive free PrEP and HIV testing services. High PrEP uptake has been reported when made available free of charge by experienced providers [10], possibly contributing to high interest and uptake among MSM and TG participants in our study.
The clinic site itself played a significant role in participant’s preference for PrEP uptake. A private and friendly by-appointment clinic was preferred over public clinic and community-based sites for enrolling in PrEP service, this pattern may be due to multiple stigmas associated with PrEP among MSM and TG communities including stigma of being related to HIV and other stigmas, such as homosexuality, sex work, and/or drug use [43], suggesting higher confidentiality and anonymity needs for those interested in enrolling in PrEP services. Although staffing and other resources differed across the four clinic sites, we believe that counselling at the site did not impact PrEP uptake as all participants had prioritized their preferred service during eCounseling session and approach was consistent. Extending online promotions and outreach through existing social media networks of community-based sites staff and popular online platforms used for seeking sex are critical to reach, engage and scale up PrEP among high-risk groups in the future.
Similar to the results of the PrEP Brasil demonstration project [44], most MSM and TG individuals enrolled in PrEP in our study were young adults (age 26–35 years). A higher level of education is related to an increased likelihood of taking PrEP [45], our PrEP participants had higher education and higher income, which may indicate a greater understanding of the medication or greater overall health literacy and greater awareness of partner’s HIV status. It may also be possible that some participants were in serodiscordant relationships and were planning to use PrEP with their HIV-positive partners.
Those who had sought sex partners on the Internet and those with past PEP use were more likely to choose and receive PrEP services. Prior PEP use was found to be a predictor of interest and willingness in taking PrEP among MSM who engage in online networking [46]. Self-identifying as bisexual has been previously associated with increased PrEP awareness [46]. However, PrEP users in our study were less likely to be bisexual, this might be because of the stigma associated with bisexuality and less willingness among Thai bisexual MSM to seek clinical services [47].
Our results demonstrate that PrEP uptake was unrelated with risk behaviours including drug use, condom-use behaviour, number of sexual partners and STI history, in contrast to previously published studies that have found PrEP acceptability to be correlated with higher-risk behaviours [46,48–50]. More efforts are therefore needed to build self-risk assessment abilities and encourage PrEP uptake among these vulnerable MSM and TG groups, a significant consideration for the next generation of Adam’s Love O2O platform. Further, the O2O model was less successful at engaging MSM and TG with lower education to PrEP services, indicating future tailoring of the model for wider PrEP scale up.
Limitations
To participate in our O2O programme, participants had to have access to a computer- or a web-enabled mobile device such as a tablet or smartphone. Given high internet and technology utilization among Thai MSM and TG [24], we assume that this limitation would not have been a major barrier to participation. Another limitation is that we did not focus on tailoring our intervention to support and measure PrEP adherence, a critical priority to ensure PrEP efficacy and offset the development of resistance. This remains the key focus for the next phase of O2O programme.
Conclusions
Our study demonstrates that Adam’s Love O2O model is highly effective in linking online at-risk MSM and TG to PrEP and HIV testing services, using eCounseling and booking as ‘bridging steps’ likely by overcoming the barriers and challenges to PrEP uptake. The study reveals significantly high interest in PrEP uptake among Thai MSM and TG and helps identify predictors of PrEP uptake. The O2O model has high potential to be replicated and scaled up in other settings with high internet penetration among key populations, where MSM and TG friendly, qualified and low or no cost PrEP service delivery sites exist.
Acknowledgements
Generic TDF/FTC drug for this research study was provided from the Thai Government Pharmaceutical Organization to the programme at a lower than market price. Funding: Laboratory and other implementation costs were supported by USAID/PEPFAR through LINKAGES programme. Funding support was provided in part by amfAR through a grant from the US National Institutes of Health’s National Institute of Allergy and Infectious Diseases, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Cancer Institute, National Institute of Mental Health, and National Institute on Drug Abuse as part of the International Epidemiology Databases to Evaluate AIDS (IeDEA; U01AI069907).
The authors would kindly like to thank Ngai Sze WONG for her contribution with the preliminary analysis of the data. The content is solely the responsibility of the authors and does not necessarily represent the official views of the institutions above. The authors are extremely grateful to all our sponsors, and thank all research participants and study staff for their significant contributions.
Biography
Tarandeep Anand and Chattiya Nitpolprasert designed and implemented the Adam’s Love Online-to-Offline (O2O) model. All authors contributed to the outline of the paper. Tarandeep Anand assumed primary responsibility for writing and revising the manuscript. Nittaya Phanuphak, Chattiya Nitpolprasert, Deondara Trachunthong and Stephen J Kerr substantially contributed to the preparation of this paper. All authors edited and reviewed the manuscript and gave their final approval for submission to the journal.
Appendix 1. Set of standardized questions used by Adam’s Love online counsellors to assess participants’ risks during the eCounseling session
• age
• ever having an anal intercourse
• number of sexual partners, condom use during anal sex, and HIV testing in the past six months
• date of last possible HIV risk exposure
Competing interests
None.
Disclaimer
The content and views in this manuscript are solely the responsibility of the authors and do not necessarily represent the views or policies of the US Army and the US Department of Defense.
Supplementary material
To access the supplementary material to this article please see Supplementary Files under Article Tools online.
References
- 1. van Griensven F, Varangrat A, Wimonsate W, Tanpradech S, Kladsawad K, Chemnasiri T, et al. Trends in HIV prevalence, estimated HIV incidence, and risk behavior among men who have sex with men in Bangkok, Thailand, 2003–2007. J Acquir Immune Defic Syndr. 2010;53(2):234–11. [DOI] [PubMed] [Google Scholar]
- 2. Ananworanich J, Chitwarakorn A, Wimonsate W, Varangrat A, Chaikummao S, Sriporn A, et al. HIV and syphilis infection among men who have sex with men – Bangkok, 2005–2011. MMWR Morb Mortal Wkly Rep. 2013;62(25):518–20. [PMC free article] [PubMed] [Google Scholar]
- 3. Nemoto T, Iwamoto M, Perngparn U, Areesantichai C, Kamitani E, Sakata M.. HIV-related risk behaviors among kathoey (male-to-female transgender) sex workers in Bangkok, Thailand. AIDS Care. 2012;24(2):210–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guadamuz TE, Wimonsate W, Varangrat A, Phanuphak P, Jommaroeng R, McNicholl JM, et al. HIV prevalence, risk behavior, hormone use and surgical history among transgender persons in Thailand. AIDS Behav. 2011;15(3):650–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National AIDS Committee 2012 Thailand AIDS response progress: status at a glance. Thailand: National AIDS Committee; 2012. [cited 2016 July21] Available from: http://namc.ddc.moph.go.th/namc/document/documentry/4-Other/หนังสือ-คชปอ/2012Thailand%20AIDS%20Response%20Progress%20Report%202010-2011%20Status%20at%20a%20glance/Final%20Status%20Eng.pdf [Google Scholar]
- 6. UNAIDS Smart investments. Geneva: Joint United Nations Programme on HIV/AIDS; 2013. [cited 2016 July21] Available from: http://www.unaids.org/sites/default/files/media_asset/20131130_smart-investments_en_1.pdf [Google Scholar]
- 7. Hosek S, Rudy B, Landovitz R, Kapogiannis B, Siberry G, Liu N, et al. An HIV pre-exposure prophylaxis (PrEP) demonstration project and safety study for young men who have sex with men in the United States (ATN 110). Presented at: 8th IAS Conference on HIV Pathogenesis Treatment and Prevention; 2015 July18–22; Vancouver, Canada; 2015. [Google Scholar]
- 8. Molina JM, Capitant C, Spire B, Pialoux G, Chidiac C, Charreau I, et al. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay trial. Oral session presented at: Conference on Retroviruses and Opportunistic Infections, abstract 23LB; 2015 February23–26; Seattle, WA; 2015. [Google Scholar]
- 9. Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Results of the iPrEx open-label extension (iPrEx OLE) in men and transgender women who have sex with men: PrEP uptake, sexual practices, and HIV incidence. Oral session presented at: 20th International AIDS Conference, abstract TUAC0105LB; 2014 July20–25; Melbourne, Australia; 2014. [Google Scholar]
- 10. Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The World Health Organization (WHO) Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV [Internet] Geneva: World Health Organization, 2015. [cited 2016 July21] Available from: http://www.ncbi.nlm.nih.gov/books/NBK327118/ [PubMed] [Google Scholar]
- 13. Piyaraj P. The impact of internet use to recruit sex partners and methamphetamine use on incident HIV infection among men who have sex with men in Bangkok, Thailand [dissertation] Baltimore (MD): The Johns Hopkins University; 2013. [Google Scholar]
- 14. van Griensven F, Na Ayutthaya PP, Wilson E. HIV surveillance and prevention in transgender women. Lancet Infect Dis. 2013;13(3):185–6. [DOI] [PubMed] [Google Scholar]
- 15. MTN-017 Microbiside Trials Network (MTN). Pittsburgh (PA): MTN; 2013. [cited 2016 July21] Available from: http://www.mtnstopshiv.org/studies/4495 [Google Scholar]
- 16. Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90. [DOI] [PubMed] [Google Scholar]
- 17. Thai Red Cross AIDS Research Centre (TRCARC) Study to evaluate the feasibility of community-based test and treat strategies among men who have sex with men and transgender women to increase the uptake of HIV testing and treatment services in Thailand. Thailand: Thai Red Cross AIDS Research Centre; 2014. [cited 2016 July21] Available from: https://clinicaltrials.gov/ct2/show/NCT02383602 [Google Scholar]
- 18. Thai Red Cross AIDS Research Centre (TRCARC) Evaluation of a facility-based test, treat, and prevent HIV program among men who have sex with men and transgender women in thailand (PrEP). Thailand: Thai Red Cross AIDS Research Centre; 2014. [cited 2016 July21] Available from: http://www.clinicaltrials.gov/ct2/show/NCT02369887 [Google Scholar]
- 19. Wolf RC. Thailand global fund round 8 external evaluation: men who have sex with men (MSM). 2012. [cited 2016 July21] Available from: http://www.researchgate.net/publication/260293958_Thailand_Global_Fund_Round_8_External_Evaluation_MSM_Thailand_Global_Fund_Round_8_External_Evaluation_Men_Who_Have_Sex_with_Men_%28MSM%29_Thailand_Global_Fund_Round_8_External_Evaluation_MSM_ACKNOWLEDGEMENTS
- 20. Thai Working Group on HIV/AIDS Projections (2005) A2 project in Thailand. The Asian Epidemic Model (AEM) Projections for HIV/AIDS in Thailand: 2005–2025. Thailand; 2008. [cited 2016 July21] Available from: http://www.aidsdatahub.org/sites/default/files/documents/The_Asian_Epidemic_Model_Projections_for_HIVAIDS_in_Thailand_2005_2025.pdf [Google Scholar]
- 21. National AIDS Committee Thailand AIDS response progress report 2012 reporting period: 2010-2011. Thailand; 2012. [cited 2016 July21] Available from: http://www.aidsdatahub.org/sites/default/files/documents/UNGASS_2012_Thailand_Narrative_Report.pdf [Google Scholar]
- 22. Sineath RC, Finneran C, Sullivan P, Sanchez T, Smith DK, van Griensven F, et al. Knowledge of and interest in using preexposure prophylaxis for HIV prevention among men who have sex with men in Thailand. J Int Assoc Provid AIDS Care. 2013;12(4):227–31. [DOI] [PubMed] [Google Scholar]
- 23. Wheelock A, Eisingerich AB, Ananworanich J, Gomez GB, Hallett TB, Dybul MR, et al. Are Thai MSM willing to take PrEP for HIV prevention? An analysis of attitudes, preferences and acceptance. PLoS One. 2013;8(1):e54288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thai PBS Survey shows the third gender spent the most time surfing the internet. Thailand: Thai PBS; 2015. [cited 2016 July21] Available from: http://englishnews.thaipbs.or.th/survey-shows-the-third-gender-spent-the-most-time-surfing-the-internet/ [Google Scholar]
- 25. Anand T, Nitpolprasert C, Ananworanich J, Pakam C, Nonenoy S, Jantarapakde J, et al. Innovative strategies using communications technologies to engage gay men and other men who have sex with men into early HIV testing and treatment in Thailand. J Virus Erad. 2015;1(2):111–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Anand T, Nitpolprasert C, Sohn AH, Parwati Merati T, Djauzi S, Yunihastuti E, et al. Temanteman.org, an integrated public-private sector communication strategy to scale up early and routine HIV testing among most-at-risk populations (MARPs) in Indonesia. Poster session presented at: 20th International AIDS Conference, abstract TUPE174; 2014 July20–25; Melbourne, Australia; 2014. [Google Scholar]
- 27. Anand T, Ananworanich J, Sohn AH, Parwati Merati T, Yunihastuti E, Imran D, et al. A culturally sensitive online communication campaign to reach hidden men who have sex with men (MSM) for HIV/STI prevention and testing in Indonesia. Poster session presented at: 7th IAS conference on HIV Pathogenesis, Treatment and Prevention, abstract WEPE590; 2013 Jun 30-Jul 3; Kuala Lumpur, Malaysia; 2013. [Google Scholar]
- 28. Anand T, Nitpolprasert C, Ananworanich J, Jantarapakde J, Kerr SJ, Sohn AH, et al. Characteristics of HIV risks among Thai young men who have sex with men and transgender youth using an eCounseling platform. Poster session presented at: 21st International AIDS Conference, abstract PEC229; 2016 July18–22; Durban, South Africa; 2016. [Google Scholar]
- 29. Kennedy C, Fonner V. Pre-exposure prophylaxis for men who have sex with men: a systematic review. 2014. [cited 2016 July21] Available from: http://www.ncbi.nlm.nih.gov/books/NBK294007/
- 30. Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men in the United States. Curr HIV Res. 2013;11(7):520–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Golshani I. Consumer engagement factors on online social media platforms [Master’s thesis] Arrhus C (Denmark): Aarhus University; 2015. [Google Scholar]
- 32. Hodas NO, Lerman K. How visibility and divided attention constrain social contagion. In: IEEE, editor Privacy, Security, Risk and Trust (PASSAT), 2012 International Conference on Social Computing (SocialCom); 2012 September3–5; Amsterdam, Netherlands; 2012. [Google Scholar]
- 33. Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res. 2014;16(2):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reisen CA, Zea MC, Bianchi FT, Poppen PJ, Shedlin MG, Penha MM. Latino gay and bisexual men’s relationships with non-gay-identified men who have sex with men. J Homosex. 2010;57(8):1004–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Masvawure TB, Sandfort TG, Reddy V, Collier KL, Lane T. ‘They think that gays have money’: gender identity and transactional sex among black men who have sex with men in four South African townships. Cult Health Sex. 2015;17(7):891–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Krakower D, Oldenburg CE, Mitty JA, Wilson I, Kurth A, Maloney K, et al. New England healthcare providers’ perceptions, knowledge and practices regarding the use of antiretrovirals for prevention. Presented at: 9th International Conference on HIV Treatment and Prevention Adherence, abstract 270; 2014 June8–10; Miami, FL; 2014. [Google Scholar]
- 37. Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58(5):704–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tellalian D, Maznavi K, Bredeek UF, Hardy WD. Pre-exposure prophylaxis (PrEP) for HIV infection: results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDS. 2013;27(10):553–9. [DOI] [PubMed] [Google Scholar]
- 39. Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18(9):1712–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Veloso VG, Mesquita F, Grinsztejn B. Pre-exposure prophylaxis for men and transgender women who have sex with men in Brazil: opportunities and challenges. J Int AIDS Soc. 2015;18 (4 Suppl 3):20010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. UNESCO Promoting health-seeking behaviours and quality of care among men who have sex with men and transgender women: evidence from 5 provinces in Thailand. Thailand: UNESCO Bangkok: 2012. [cited 2016 December21] Available from: http://unesdoc.unesco.org/images/0021/002171/217197e.pdf [Google Scholar]
- 42. National AIDS Committee Thailand national operational plan accelerating ending AIDS, 2015-2019. Thailand; 2014. [cited 2016 December21] Available from: http://www.aidsdatahub.org/sites/default/files/publication/Thailand_National_Operational_Plan_Accelerating_Ending_AIDS_2015-2019.pdf [Google Scholar]
- 43. Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. [DOI] [PubMed] [Google Scholar]
- 44. Hoagland B, Veloso VG, De Boni RB, Madruga JV, Kallas EG, Fernandes NM, et al. Pre-exposure prophylaxis (PrEP) uptake and associated factors among MSM and TGW in the PrEP Brasil demonstration project. Presented at: 8th IAS Conference on HIV Pathogenesis, Treatment and Prevention; 2015 July 18–22; Vancouver, Canada; 2015. [Google Scholar]
- 45. Mustanski B, Johnson AK, Garofalo R, Ryan D, Birkett M. Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS Behav. 2013;17(6):2173–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Krakower DS, Mimiaga MJ, Rosenberger JG, Novak DS, Mitty JA, White JM, et al. Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an internet social networking site. PLoS One. 2012;7(3):e33119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Guadamuz TE, Cheung DH, Wei C, Koe S, Lim SH. Young, online and in the dark: scaling up HIV testing among MSM in ASEAN. PLoS One. 2015;10(5):e0126658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schneider J, Kumar R, Dandona R, Kumar P, Kumar A, Lakshmi V, et al. Social network and risk-taking behavior most associated with rapid HIV testing, circumcision, and preexposure prophylaxis acceptability among high-risk Indian men. AIDS Patient Care STDS. 2012;26(10):631–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zhou F, Gao L, Li S, Li D, Zhang L, Fan W, et al. Willingness to accept HIV pre-exposure prophylaxis among Chinese men who have sex with men. PLoS One. 2012;7(3):e32329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Liu AY, Kittredge PV, Vittinghoff E, Raymond HF, Ahrens K, Matheson T, et al. Limited knowledge and use of HIV post- and pre-exposure prophylaxis among gay and bisexual men. J Acquir Immune Defic Syndr. 2008;47(2):241–7. [PubMed] [Google Scholar]


