Abstract
Alignment and stability are two key factors for success in total knee arthroplasty (TKA). Several techniques have been advocated, the two best known being measured resection and tensioned gaps.
Dogma and fuzzy wording have cast an obscure shadow on the dualistic discussion between proponents of both techniques.
This review is an attempt to clarify definitions, analyse the flaws and pitfalls in the different techniques and make some suggestions for improvement.
Cite this article: EFORT Open Rev 2017;2. DOI: 10.1302/2058-5241.2.170001. Originally published online at www.efortopenreviews.org
Keywords: stability, total knee arthroplasty, alignment
Introduction
Total knee arthroplasty (TKA) is, in essence, a resurfacing procedure, and should thus respect ligament tension in order to function properly. Failure mechanisms and indications for revision of TKA have shifted over time. In the 1980s and 1990s, catastrophic polyethylene wear and osteolysis challenged the longevity of the procedure. Improvement of polyethylene quality and sterilisation processes, in combination with better technical solutions for reducing backside wear and micromotion in modular implants, have greatly reduced this problem. Today infection, instability, malalignment, stiffness and dissatisfaction with the outcome of the procedure are the main drivers for early revision.1 In particular, this is a more serious problem for young patients, for whom an early revision is not only a major setback in the short term, but a serious threat to the long-term function of the limb.2 Instability and stiffness are directly related to the position, size and geometry of the components, and with tension in the ligaments throughout the motion arc.
Traditionally, two apparently conflicting surgical techniques have been proposed.
Proponents of the so called measured resection technique use bony references as the basis for component positioning and, if needed, try to adapt ligament tension by releasing tight ligaments. This concept is, in a semantically confusing way, often referred to as balancing.
Proponents of the so called dependent technique use ligament tensioners to define the optimum position of the implants in order to achieve stability. They will adapt the bone cuts and take ligament tension as the basis for positioning.
Both techniques have significant flaws in concept and surgical execution, as will be explained in the following sections.
Definitions
Orthopaedic literature on this subject is polluted with confusing terminology, so for the sake of clarity we will use the following terms:
- Gaps. The space between tibia and femur, after bone cuts have been made. The extension gap refers to the available space with the knee near full extension. It is often forgotten that the tibial cut is made slightly oblique in the sagittal plane (slope), so that the tibia and femur are artificially separated with a block or an instrument, with the knee in slight flexion. The flexion gap refers to the available space with the knee in a position around 90° flexion.
- Gap equality. This term refers to the equality between the extension and the flexion gap.
- Gap symmetry. This term refers to the equality between the medial and the lateral side of either flexion or extension gap.
- Tensioned gaps. After the tibial cut has been made, based upon geometrical references, the ligaments are tensioned with an instrument that separates tibia and femur, a so-called tensioner. The obtained position is used to define the bone cuts of the femur and eventual position of the femoral component in one or more planes. This technique can be used in extension or in flexion.
- Ligament release. A ligament that is considered too tight can be cut (as in ligament sacrificing, e.g. the posterior cruciate ligament (PCL)), detached from its insertion, partially cut (pie crusting) or perforated sequentially with a needle (needle puncturing). It is important to realise that all of these techniques will damage the integrity of the ligament and induce at least scar formation. Also, ligament release is extremely difficult to titrate and correct assessment of the surgical action is difficult.
- Balancing. I will avoid using this word as it suggests that something is balanced, which includes a two-sided action. This is rarely the case as a tight ligament virtually always will be released whereas a slack ligament is rarely tightened. Also, the term does not define when the balance is achieved, although generally authors mean that tension on the medial and lateral side will be equal, given a set position of separation between femur and tibia. Finally, this two-sided approach is too limited for the three-dimensional reality of the human joint.
Kinematics
The study of kinematics describes the relative motion of rigid bodies, in casu, the motion of the femur relative to the tibia. In other words, when one understands the kinematics of the normal knee, one understands ‘how the normal knee moves’. It is intuitively attractive to assume that a TKA that functions as the normal knee will be perceived as satisfactory by the patient. Still, as of today, there is no literature available that correlates patient satisfaction with more normal kinematics. On the other hand, there is abundant literature that describes abnormal kinematics and instability after TKA, sometimes with good results.3,4 Whereas the relationship between normal kinematics and increased patient satisfaction has not yet been proven, instability has been identified as a major cause for early failure.1
During the surgical process of insertion of a TKA, many stabilising structures are removed (such as menisci and/or cruciate ligaments), altered (such as the tibial plateau geometry) or damaged (such as capsular or ligament insertions). Whatever technique or type of TKA is used, a certain level of intrinsic constraint needs to be added in order to compensate for the lost stability. This can be achieved by means of surface geometry as in a deep dish or a medial pivoting device, a cam-post mechanism as in a posterior stabilised knee, or a mechanical link as in a hinged implant. It is perfectly clear that less intrinsic implant constraint implies post-operative stability to be more dependent on capsular and ligament tension.
Numerous studies have made clear that the medial and lateral side of the knee are geometrically and functionally fundamentally different.5,6 The medial side of the knee is more congruent and more stable and the medial collateral ligament is isometric in its central fibres.7 The lateral side of the knee is more mobile, slides further posteriorly with increasing flexion and the lateral collateral slackens with increasing flexion and is thus anisometric. These differences have significant consequences on the main surgical techniques that are in use today.
Measured resection versus tensioned gaps
The conceptual disagreement between proponents of either technique has been fierce, maybe because both concepts share a common goal. They strive to obtain the desired alignment in a reliable and consistent way. They both aim at restoring the natural flexion axis and functional stability throughout range of motion (ROM). An objective analysis of the surgical steps reveals significant flaws and pitfalls with either technique.
Tensioned gaps
Ligaments have a non-linear stress-strain curve (Fig. 1)
Fig. 1.
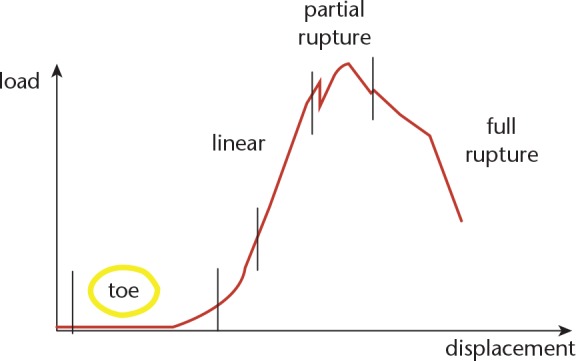
Example of a typical stress-strain curve of a ligament with the initial toe phase, followed by the linear phase.
In the initial phase of the stress-strain curve, a small increase in force will lead to a great displacement. This so-called ‘toe phase’ is followed by a linear curve that ends near the yield point. This argument might seem academic but it is real: most tensioners do not measure force of distraction, and those which do measure distraction force are not precise about the optimum value. In addition, the weight of the limb can significantly influence the force of distraction between femur and tibia, especially in flexion. Finally, the medial collateral ligament is stronger and stiffer than the lateral collateral ligament. Consequently, with increasing distraction force the lateral side will open more than the medial side
The normal knee is not symmetrical
As pointed out earlier, the medial and lateral side of the knee behave fundamentally differently.7,8 In particular, the non-isometric behaviour of the lateral collateral ligament is in contradiction with the ‘holy grail’ of gap symmetry (see definition above).
Tensioners check position at two discrete points in the motion arc: near full extension and around 90° of flexion
It is assumed that ligament tension will be excellent in all positions if it is in these two discrete positions, but mid- and deep-flexion stability and laxity are not assessed.
The relative positions of the femur and tibia in the sagittal plane are not taken into account
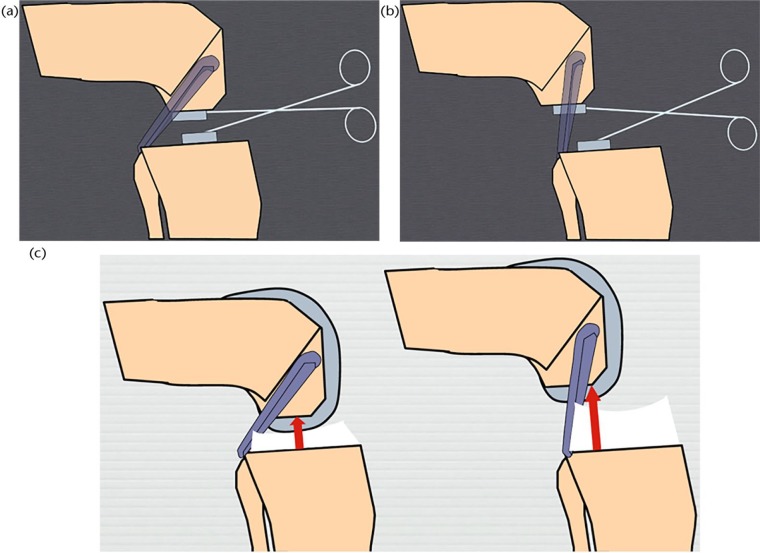
Wymenga and Christen described this phenomenon in the cruciate-retaining knee.9 With increasing distraction, the tibia is pushed forwards and the PCL is verticalised. The eventual position at which tibia and femur are assessed is not necessarily the relative final position of the bones after insertion of the implants (Fig. 2).
Fig. 2.
a) Position of femur, tibia and posterior cruciate ligament (PCL) with moderate distraction; b) position of femur, tibia and PCL with maximum distraction; c) relative position of femur and tibia relating to setting (a) and (b). Note the more anterior position of the tibia and more vertical PCL at the right of the image.
Uncontrolled variables
Many arthritic knees have suffered acute traumatic ligament injury or chronic ligament injury as a consequence of coronal or sagittal malalignment. It is, for instance, well-known that varus deformity above 10° creates distraction of the lateral compartment of the knee in the coronal plane. These patients often display a varus trust during walking, as a signature of a stretched lateral capsule and collateral ligament. One can argue whether it is wise to use a damaged structure as a reference for implant positioning.
In most systems, the patella is dislocated at the time of using the technique of tensioned gaps. This dislocated patella certainly affects the resistance to distraction on the lateral side, potentially adding a serious bias.
Measured resection
Distal cartilage and bone wear
In the measured resection technique, the surface of proximal tibia and distal femur are important references. At the distal femur, the cut is usually made close to perpendicular to the mechanical axis. As the joint line orientation (not to be confused with the overall limb alignment in the coronal plane) in the normal knee is in slight varus, the distal cutting instrument will first hit the medial distal joint line (Fig. 3) reference for the resection level. Distal medial cartilage or bone wear will induce a more proximal resection of the femoral bone cut and will raise the joint line level.
Fig. 3.
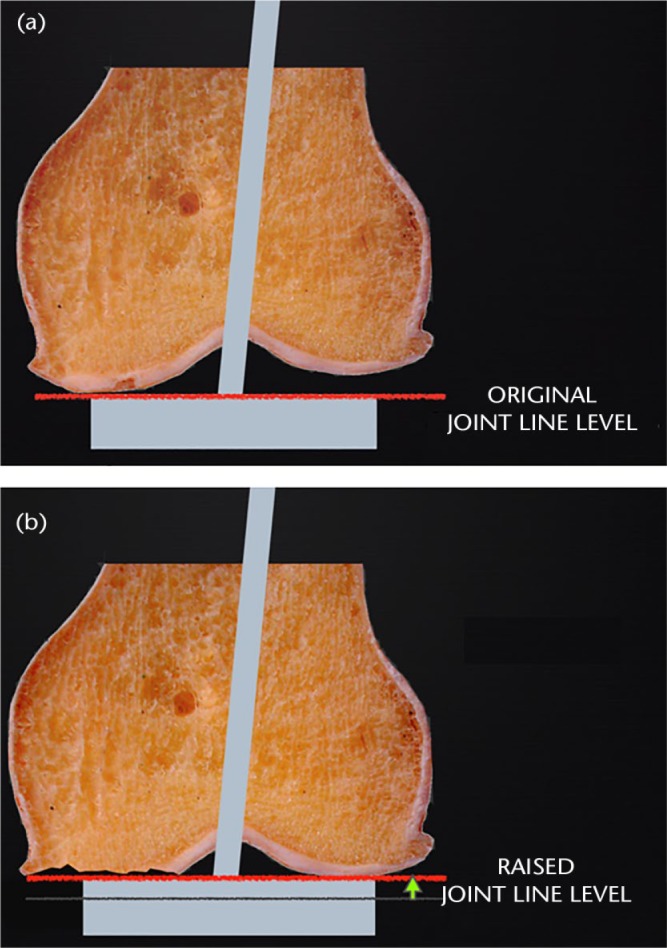
Animation of the introduction of the intramedullary rod in the femur set at predefined valgus angle with distal reference block. In (a) the block is touching the distal femoral condyle at the correct level and the preset cut will be correct. In (b) there is medial cartilage and bone wear. The bone will slide up to the distal lateral condyle and too much bone will be removed from the distal femur.
Posterior cartilage and bone wear
The instrument that sets femoral rotation and defines the anteroposterior position of the femoral component has paddles that engage under the condyles. When arthritis has worn out the condyle posteriorly, the position of the femoral component in the sagittal and horizontal plane will be erroneously influenced.
Dysplasia
Condylar dysplasia is often present in the valgus knee. Referencing off a smaller lateral condyle will induce internal rotation of the femoral component.
Inability to find the reference axis
The surgical epicondylar axis has been shown to be a good reference for rotational alignment of the femoral component.10 Still, it is a very difficult axis to reliably and reproducibly identify during surgery.
Variability of the reference axis
Some authors propose the use of the trochlear axis as a reference for rotational alignment of the femoral component. However, the large variability of this axis questions the validity of its routine and exclusive use for setting rotational alignment of the femoral component.10
Rotation of the femoral cutting block
In most systems, the femoral cutting block rotates in the horizontal plane around a central pivot point. In applying external rotation, the amount of bone that is cut posteromedially increases, leading to flexion instability11 or joint line elevation (Fig. 4).
Fig. 4.
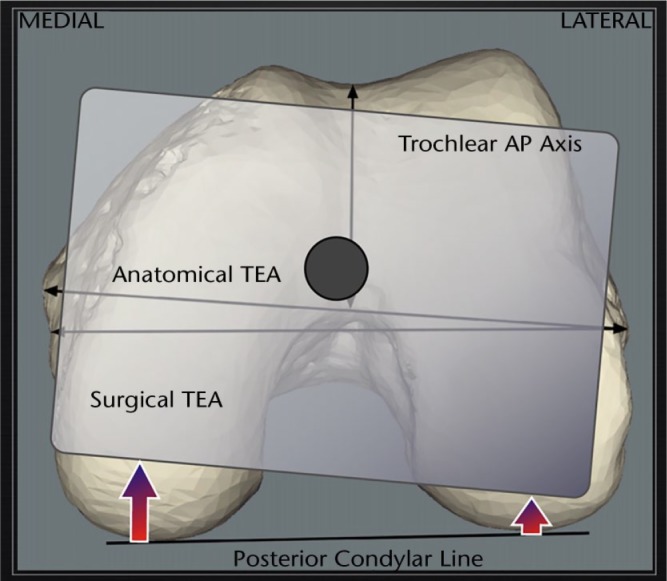
Central pivoting of the femoral block when giving external rotation will induce excessive (more than replaced with metal) resection on the posterior medial condyle.
The above description is not exhaustive but describes the difficulties faced during surgery. The pitfalls with their potential consequences are summarised in Table 1.
Table 1.
Schematic overview of techniques with potential pitfalls
| Technique | Pitfall | Result |
|---|---|---|
| Tensioned gaps | Natural lateral laxity | External rotation |
| Tight patellar tendon | Internal rotation | |
| Ligament imbalance | Inconsistent | |
| Wrong tibial cut | Inconsistent | |
| MR- PCL | Lateral dysplasia | Internal rotation |
| MR -Trochl AP axis | Large variability | Inconsistent |
| MR- TEA | Inconsistent location | Inconsistent |
MR, measured resection; PCL, posterior condylar line; TEA, surgical transepicondylar axis
The role of coronal alignment
In the case of healthy ligaments, the insertion of a knee prosthesis with an identical geometry in the native position (meaning maintaining joint line and coronal alignment of the native knee) would deliver normal ligament tension, provided the capsule or ligaments are not affected by surgical damage. This is obviously a hypothetical situation as correction of deformity is part of the surgical procedure of TKA. There is, however, evidence that slight undercorrection of the deformity is beneficiary, both for longevity12 and function.13
We described the prevalence of constitutional varus14 and its influence on joint line orientation in the coronal plane.15 With this insight, the potential better outcomes of slight undercorrection of the initial deformity can be understood. As a knee, deformed by arthritis, is surgically reduced to its ‘native pre-arthritic’ condition, it is unlikely that ligament releases would be necessary.14 Further reduction to neutral, or worse, slight overcorrection will increase the need for ligament release. Given the potential problems with ligament release (instability or scarring) one can understand the sub-optimal results in these cohorts of patients. Two important words of caution, however. There is evidence in the literature that a varus tibial cut increases the risk of failure,16 and this should thus be avoided. Second, undercorrection should be limited to 5° in the coronal plane. It is currently not proven that greater undercorrection of the initial deformity is beneficial and the risk for subsequent failure of fixation should be taken into account.
Suggestions for improvement and author preference
With the above described analysis in mind and taken the current knowledge into account we use the following algorithm.
Maintain the medial joint line level
As the medial side of the knee is the stable and isometric side, it is very logical to maintain the joint line level on this side. This will avoid the occurrence of mid-flexion instability17 and gives the best guarantee to restore the original flexion axis.
Technically, this can be achieved by paying close attention to the distal and posterior resection level, compensating for cartilage or bone loss and using a femoral block that rotates around the posteromedial condyle instead of around the centre of the femur in the horizontal plane
Avoid dogmatic thinking and use measured resection in combination with tensioned gaps
As both techniques are subject to dangerous shortcomings and have inherent flaws and drawbacks, the available information for positioning the components should be maximised. In cases with conflicting information or outlier positions, a compromise should be found. For instance, a varus knee with chronic lateral laxity can be steered towards an excessive external rotation of the femoral component by only using the tensioned gaps technique, and this should not be accepted. Still, it is wise to add a few degrees of external rotation in addition to what one would give based upon measured resection only, in order to partially compensate for the lateral instability. The greater the initial deformity, the more forgiving the compromise will have to be in either direction (ligaments or alignment). The old dogma of equal and symmetric gaps is often not possible to achieve in the real world.
Avoid overcorrection of the original deformity in the coronal plane
With every degree of correction beyond the original pre-arthritic coronal alignment of the limb, the need for ligament release will increase. A few degrees already dramatically change intra-articular loads.18 In experienced hands, a small undercorrection is probably beneficial. It should be carried out at the level of the femur as the tibial cut is best perpendicular to the mechanical axis.
Avoid oversizing of the components
It has been shown that oversizing causes conflicts between the implant and the soft tissues.19 The old mantra was to avoid notching of the anterior femoral cortex by all means. As a consequence, many surgeons aimed at oversizing the femoral component.
It is obviously still contra-indicated to undercut the anterior cortex of the femur but careful sizing of the components is of utmost importance. With current systems providing the surgeons with a big number (often ten or more) of sizes and divergent anterior femoral cuts, a better sizing of the femoral and tibial component is both possible and desirable.
We need to measure better what we do
Intra-operative assessment of alignment and laxity is subjective and inaccurate. Surgical navigation can be cumbersome to use but a comeback of this technology in a more user -friendly form is vitally needed. Current technological developments also allow the measurement of intra-articular loads. This feedback will help to steer the fine tuning of the bone cuts and/or subtle ligament releases.
Footnotes
ICMJE Conflict of Interest Statement: JV reports that his institution receives grants from ZimmerBiomet, Corin, Smith & Nephew, Vigo, Stryker and DePuy Synthes. He also receives royalties from a patent for High Performance Knee.
Funding
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Thiele K, Perka C, Matziolis G, et al. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg [Am] 2015;97:715-720. [DOI] [PubMed] [Google Scholar]
- 2. Scott CE, Oliver WM, MacDonald D, et al. Predicting dissatisfaction following total knee arthroplasty in patients under 55 years of age. Bone Joint J 2016;98-B:1625-1634. [DOI] [PubMed] [Google Scholar]
- 3. Dennis DA, Komistek RD, Colwell CE, Jr, et al. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 1998;356:47-57. [DOI] [PubMed] [Google Scholar]
- 4. Victor J, Mueller JK, Komistek RD, et al. In vivo kinematics after a cruciate-substituting TKA. Clin Orthop Relat Res 2010;468:807-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hill PF, Vedi V, Williams A, et al. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg [Br] 2000;82-B:1196-1198. [DOI] [PubMed] [Google Scholar]
- 6. Victor J, Van Glabbeek F, Vander Sloten J, et al. An experimental model for kinematic analysis of the knee. J Bone Joint Surg [Am] 2009;91-A:150-163. [DOI] [PubMed] [Google Scholar]
- 7. Victor J, Wong P, Witvrouw E, Sloten JV, Bellemans J. How isometric are the medial patellofemoral, superficial medial collateral, and lateral collateral ligaments of the knee? Am J Sports Med 2009;37:2028-2036. [DOI] [PubMed] [Google Scholar]
- 8. Van Damme G, Defoort K, Ducoulombier Y, et al. What should the surgeon aim for when performing computer-assisted total knee arthroplasty? J Bone Joint Surg [Am] 2005;87-A:52-58. [DOI] [PubMed] [Google Scholar]
- 9. Wymenga AB, Christen B, Wehrli U. Posterior cruciate ligament balancing in total knee arthroplasty with a dynamic PCL spacer. In: Bellemans J, Ries MD, Victor JMK, ed. Total Knee Arthroplasty. Berlin: Springer Verlag, 2005. [Google Scholar]
- 10. Victor J, Van Doninck D, Labey L, et al. A common reference frame for describing rotation of the distal femur: a ct-based kinematic study using cadavers. J Bone Joint Surg [Br] 2009;91-B:683-690. [DOI] [PubMed] [Google Scholar]
- 11. Olcott CW, Scott RD. The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res 1999;367:39-42. [PubMed] [Google Scholar]
- 12. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg [Am] 2010;92-A:2143-2149. [DOI] [PubMed] [Google Scholar]
- 13. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 2013;21:2325-2330. [DOI] [PubMed] [Google Scholar]
- 14. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 2012;470:45-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Victor JM, Bassens D, Bellemans J, et al. Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 2014;472:98-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ritter MA, Davis KE, Meding JB, et al. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg [Am] 2011;93-A:1588-1596. [DOI] [PubMed] [Google Scholar]
- 17. Victor J, Luyckx T. Mid-flexion instability after TKA. In Insall Scott Kelly Knee Surgery In press [Google Scholar]
- 18. Walker PS, Meere PA, Bell CP. Effects of surgical variables in balancing of total knee replacements using an instrumented tibial trial. Knee. 2014; 21:156-61 [DOI] [PubMed] [Google Scholar]
- 19. Bonnin MP, Van Hoof T, De Kok A, et al. Imaging the implant-soft tissue interactions in total knee arthroplasty. J Exp Orthop 2016;3:24. [DOI] [PMC free article] [PubMed] [Google Scholar]