Abstract
A nerve injury has a profound impact on the patient’s daily life due to the impaired sensory and motor function, impaired dexterity, sensitivity to cold as well as eventual pain problems.
To perform an appropriate treatment of nerve injuries, a correct diagnosis must be made, where the injury is properly classified, leading to an optimal surgical approach and technique, where timing of surgery is also important for the outcome.
Knowledge about the nerve regeneration process, where delicate processes occur in neurons, non-neuronal cells (i.e. Schwann cells) and other cells in the peripheral as well as the central nervous systems, is crucial for the treating surgeon.
The surgical decision to perform nerve repair and/or reconstruction depends on the type of injury, the condition of the wound as well as the vascularity of the wound.
To reconnect injured nerve ends, various techniques can be used, which include both epineurial and fascicular nerve repair, and if a nerve defect is caused by the injury, a nerve reconstruction procedure has to be performed, including bridging the defect using nerve-grafts or nerve transfer techniques.
The patients must be evaluated properly and regularly after the surgical procedure and appropriate rehabilitation programmes are useful to improve the final outcome.
Cite this article: EFORT Open Rev 2017;2. DOI: 10.1302/2058-5241.2.160071. Originally published online at www.efortopenreviews.org
Keywords: nerve injury, nerve repair, nerve reconstruction, nerve transfer, nerve regeneration, neuroma
Background
Injuries to the extremities and hand are common; the incidence of hand injuries is 7 to 37/1000 inhabitants/year in Europe1 and around 50% of the injuries are fractures. Among the affected structures that are much less affected (i.e. around 3%) are peripheral nerves; the incidence of nerve injury is 0.14/1000 inhabitants/year.2 Nerve injuries most commonly affect the upper extremities, but the sciatic, peroneal and tibial nerve trunks may also be affected in the lower extremities, where the regenerative capacity varies; for example, the peroneal nerve is worse than the tibial nerve.3 Treatment of peripheral nerve injuries is a real challenge for surgeons and physicians, since the outcome after different procedures still may be insufficient, although continuous efforts have been made to improve the outcome. To make a correct diagnosis and to treat patients properly with various nerve injuries and disorders, it is important to have a basic knowledge of the neurobiological mechanisms that are active after injuries, since strategies to improve the outcome following nerve injuries are often based on such mechanisms. If the patients are treated with a delay, or if the care is inappropriate, it will often reduce the functional outcome and create further costs for society due to potentially more extensive surgical procedures, longer rehabilitation and longer sick leave.4,5 Furthermore, the outcome of treatment of nerve injuries depends on a large number of different factors, but two important ones are the competence and experience of the treating surgeon as well as the quality of the staff performing the rehabilitation – a vital teamwork. In the present review, the principles for treating nerve injuries located at the finger level up to the brachial plexus level, as well as principles valid for nerve injuries in the lower extremities, are presented and related to the neurobiological alterations that occur in peripheral nerves and in the surrounding cells as well as the secondary changes occurring up in the central nervous system.
The peripheral nerve
Peripheral nerves are susceptible to different types of trauma that may extend from simple compression and stretching injuries up to severe lacerations creating extensive nerve defects between the proximal and distal nerve ends. The peripheral nerve consists of the extended process from the neuronal cell body—the axon—and the surrounding Schwann cells that are wrapped segmentally around the axon along its length or are associated with several axons thus forming myelinated and unmyelinated axons. The myelinated nerve fibres consist of a single axon which are wrapped around by a chain of Schwann cells that create the myelin sheath consisting of the flat processes of the cytoplasm of such cells. The node of Ranvier is the interval between two consecutive myelin sheaths from two adjacent Schwann cells. The thickness of the myelin sheath and the length between the different nodes of Ranvier (i.e. internodal length) are directly proportional to the size of the axons and to the conduction velocity in the peripheral nerve. In contrast to the myelinated nerve fibres, the unmyelinated nerve fibres have a different construction, where a single Schwann cell enwraps several unmyelinated axons. Bundles of myelinated and unmyelinated nerve fibres are clustered together and are surrounded by a dense and strong connective tissue sheath—the perineurium—forming a fascicle. Inside a fascicle, i.e. the endoneurial space, a loose connective tissue with various cells, like fibroblasts, macrophages and mast cells, further supports and protects the nerve fibres. Fibrils of collagen are grouped around the nerve fibres and thereby specific endoneurial tubes are formed around each nerve fibre along its course in the nerve trunk. Within such tubes there is a basal lamina that is produced by the Schwann cells forming the continuous tube around the unit axon-Schwann cell. The pressure in the endoneurium—endoneurial fluid pressure—is higher than in the surrounding tissue, which is a further protection of the content of the endoneurial space. The effects of the increased endoneurial fluid pressure can be seen as mushrooming of the endoneurial content after transection of a nerve trunk, thus the bulging of the content (i.e. compare the toothpaste with the toothpaste tube). In the endoneurial space, there is a rich network of capillaries that provides the axons with oxygen.6
A number of fascicles are clustered together, which are further protected by a loose connective tissue—epineurium—that consists of collagen fibrils. The amount of epineurium varies along the nerve trunk. In the epineurium, there are numerous blood vessels extending along the axis of the nerves, which are provided by blood from segmentally approaching blood vessels in the mesoneurium (i.e. compare with mesentery).6 The segmentally approaching blood vessels are coiled in their structure, thus allowing reserve capacity during the excursion of the nerve trunk in connection with movement of the limb. Furthermore, a nerve trunk can be surgically mobilised over a certain distance without restriction of the blood flow. The fundamental difference between the epineurial blood vessels and the endoneurial capillaries are the resistance against trauma. The epineurial blood vessels are much more susceptible to trauma, thereby forming an epineurial oedema, while the endoneurial capillaries are more resistant. However, if a severe injury occurs to the endoneurial capillary wall with subsequent increased vascular permeability, the consequences for the nerve fibres are extreme, since any oedema in the closed endoneurial compartment will substantially increase the endoneurial fluid pressure. This will markedly reduce the blood flow in the endoneurial capillaries. Thus, a closed compartment syndrome in miniature is formed after such trauma, which may consist of extensive compression or stretching of the nerve trunk.7
Classification of nerve injuries
Nerve injuries can be classified according to the old, but still relevant, classifications by Sir Herbert Seddon and Sir Sydney Sunderland (Table 1).8,9 Seddon divided the injury into three grades, while Sunderland further subdivided them according to discontinuity of the different layers of the connective tissue in the peripheral nerve.9 Neuropraxia (i.e. Sunderland grade 1) is compression or mild crush of the nerves that damage the Schwann cell sheath, but the axons and the connective tissue are still in continuity. Clinically, this produces a nerve conduction block with disturbed motor and sensory function, which is transient, extending from hours up to a few weeks. The term axonotmesis, introduced by Seddon, is used when the axon and its sheaths are disconnected. Sunderland further divides this stage into three different grades. The Sunderland grade 2 injury denotes an injury that disconnects only the axon and its surrounding Schwann cell sheath, but the continuity of all the connective tissue layers is preserved. Thereby, there will be a denervation of the targets and with a disturbed motor and sensory function. The functional recovery may take up to weeks or months since regeneration of the axons is necessary, but this grade does usually not require any surgical intervention. In the Sunderland grade 3 injury, the axon and its sheaths as well as the endoneurial layer, but not the other connective tissue layers, are disconnected and the functional recovery, if it occurs, may be more difficult to achieve. If the trauma is more severe, there may be a Sunderland grade 4 injury, where only the epineurium is in continuity, while the axon, its sheaths, the endoneurium as well as the perineurium are disconnected. Finally, the term neurotmesis (i.e. Sunderland grade 5; principally, grade 4 can also sometimes be classified as a neurotmesis) denotes also the epineurium is disconnected.9 Such a complete nerve transection (or laceration) injury needs prompt and obligatory surgical intervention to achieve functional recovery. In some circumstances, the expression ‘grade 6’ injury may be used and designates an injury with mixed injuries, (e.g. after closed traction, gunshot or stab wounds) causing partial nerve injuries; i.e. a neuroma-in-continuity (i.e. all degrees of nerve injury may co-exist). Surgical exploration is necessary, using electrodiagnostic methods intra-operatively, and tentative nerve reconstruction with nerve grafts due to a loss of substance creating a nerve defect (Table 1).
Table 1.
| Seddon classification | Sunderland classification | Causes | Pathophysiology | Surgical intervention | Recovery |
|---|---|---|---|---|---|
| Neuropraxia | Grade 1 | Compression, mild crush, traction, local ischemia | Axons and connective tissue in continuity – nerve conduction block | None, unless remaining external compression | Complete - hours up to a few weeks |
| Axonotmesis | Grade 2 | Nerve crush | Axons divided, but all connective layers intact | Usually not | Complete - weeks to months |
| Grade 3 | Nerve crush | Axons with its sheaths and endoneurial layer disconnected (subsequent scarring) | Usually not | Incomplete and variable - months | |
| Grade 4 | Nerve crush | Axons with its sheaths, endoneurium and perineurium disconnected | Usually necessary; procedure depending findings | Incomplete and variable - depending on injury and treatment – months to years | |
| Neurotmesis | Grade 5 | Nerve transection or laceration | Axons with its sheaths, endoneurium, perineurium and epineurium disconnected (i.e. whole nerve divided) | Necessary; early nerve repair or reconstruction | Incomplete - months to years |
| Grade 6 (according to MacKinnon) | Closed traction damage, gunshot or stab wounds with partial injuries – neuroma-in continuity | Mixed injury – all grades present | Surgical exploration and intraoperative electrodiagnostic methods - nerve reconstruction or nerve transfer | Incomplete - months to years |
Cellular reactions after nerve injury
Intracellular signals after a nerve injury
After severe nerve injuries, such as nerve transection and nerve laceration injuries, there is a cascade of different intra-neuronal signals elicited from the site of lesion, including the ones released from invading macrophages and reacting Schwann cells, that are transported up to the nerve cell body.10,11 These injury-induced signals, occurring in different phases, make the neurons able to switch from transmission state to a regenerative state causing changed expressions of many genes involved in survival or death of the neuron as well as in regrowth of the axons.12-14
Wallerian degeneration and cellular reactions after nerve injury
The segment of the nerve distal to the site of a lesion undergoes the process that is known as Wallerian degeneration, which starts immediately after an injury.15 This process involves degeneration of the axons and breakdown of the myelin, with subsequent proliferation of the Schwann cells, recruitment of immune cells, such as macrophages (eliminating myelin and cell debris), as well as remodelling of the tissues. These events have the purpose to create an optimal milieu for the axonal outgrowth after the injury.
The proliferation of Schwann cells, forming an optimal pathway for the outgrowing axons, is accompanied by upregulation of a large number of different trophic factors in the Schwann cells supporting the axons during the regrowth—processes that decline over time, leading to impaired nerve regeneration.16,17 Thus, a nerve repair or reconstruction procedure should be done promptly due to the fact that Schwann cells have ‘a best before date’ after a nerve injury.10,18,19
Axonal outgrowth and re-myelination
Soon after the nerve injury, the distal tip of the proximal axon emits numerous collateral sprouts that cross the injury zone and then the formed axons regenerate into the distal nerve end at a rate of around 1 mm to 2 mm/day in humans if the milieu is optimal.7,20 In successful cases, there is a re-myelination of the axons in which the size of the axon as well as the thickness of the myelin increase.19 The diameter of the regenerated axons does not reach pre-injury levels; thereby the conduction velocity will be below normal. After completion of the nerve regeneration process, the intracellular activities in the nerve cell body go back to a transmitter mode.
Nerve injury and cerebral alterations
A peripheral nerve injury results in profound changes in the central nervous system, particularly in functional alterations in the brain that can be observed by functional MRI.21 Such changes are important factors that determine the clinical outcome, in particular regarding recovery of sensory function, which is particularly good in children (i.e. below the age of 12 years).22 This age effect in nerve regeneration after injury is based on the tremendous capacity of the central nervous system to change and adapt to an injury, a phenomenon called ‘cerebral plasticity’.21
Clinical examination of the patient
All patients with a potential nerve injury should be judged individually and the general condition of the patient is extremely important in the decision-making of if and when a procedure on the peripheral nerve should be done,1 since extremity injuries have a lower priority than other concomitant injuries, e.g. chest, abdomen, skull, etc. However, it is crucial that any nerve injury is detected early so that the decision to perform a surgical procedure should not be delayed. Basically, every patient with a dysfunctional nerve and a wound that are overlying the course of the peripheral nerve trunk should be regarded as having a transected nerve until proved otherwise. Decisive factors for an optimal outcome after repair or reconstruction of a nerve injury are the timing of surgery, the type of nerve injury and the nature as well as vascularity of the wound. In the future, surgeons have to create optimal trauma organisations to be able to treat nerve injuries urgently in order to use the inherent capacity of axons to regenerate.
Each nerve injury is unique in its character and the symptoms may be highly variable, but it is important to make a correct diagnosis initially.1 The history of the patient and evaluation of the mechanism of the injury must be evaluated by the surgeon. Sensory and motor functions should be carefully examined, where the motor evaluation includes pinch and grip strength as well as evaluation of the function and the strength of individual muscles that are innervated by the specific involved nerves. Sensory function can be evaluated by examination of light touch, but in patients with an acute injury it may be easier to assess the patient’s ability to feel pain (e.g. that applied by a forceps) in the innervation area of the specific nerve. Two-point discrimination and the patient’s ability to separate sharp and blunt objects can be used, but the former may be less specific in the acutely injured patient. Sudomotor function can be checked even in children with a suspected nerve injury. A positive Tinel’s sign may also be present over the proximal nerve end of the injured nerve.
Electrophysiology
Neurography and electromyography (EMG) can help to establish the diagnosis and identify the injured nerve branches, but results may be difficult to interpret during the first weeks due to the unclear detectable signs of nerve degeneration (one to two weeks by neurography) and muscular denervation (two to four weeks by needle EMG).23 One should not delay any exploration of an injured nerve, if there is a strong indication for exploration, by waiting for an electrophysiological examination. Intra-operative nerve conduction and electrical stimulation of individual nerve branches or fascicles can be of great help in deciding how a nerve reconstruction of a nerve injury in continuity should be done since some intact fascicles can be spared if functional axons are located.
Combined nerve injuries
Peripheral nerve injuries are usually not isolated, but are combined with single or multiple tendon injuries, injuries to blood vessels and in combination with fractures. Extensive tissue damage, with a contaminated wound that affects the management of the nerve injury making it necessary to perform an extensive debridement and cleaning of the wound, are also seen. Such procedures have to carefully and meticulously be done before any nerve repair or reconstruction is prepared. Ideally, the repair or reconstruction should be performed in a tissue bed which is well nourished, consisting of muscle or fat. Therefore, it may be suitable to apply a pedicled or free flap to reconstruct the defect of skin in connection with a nerve repair and reconstruction procedure or in single cases less recommendable with the nerve procedure at a later stage.1 Thus, in the future, trauma surgeons with different competencies need to cooperate closely to promptly and optimally treat the nerve injuries.
To explore or to wait?
In those patients, where there are clinical signs of a nerve injury, but without any fresh wound or any scar, a conservative attitude may be the best for the first four to six weeks.1 However, clinical signs of functional recovery should be carefully and regularly be investigated and documented—‘active surveillance’—preferably daily or weekly by the same surgeon. If no signs of spontaneous recovery are spotted, an electrophysiological examination can be done at this time. If no functional recovery is observed at all after three months, supported by clinical and electrophysiological findings, the injured nerves should be explored. This is supported by experimental and clinical studies that both the proximal and distal nerve segments, including the target organ, will have suffered devastating changes following that time-point,18,24 thus resulting in inappropriate functional recovery.25 If functional recovery of the specifically innervated muscles along the course of the nerve is perceived, one may continue the conservative approach and follow the regeneration process. During this time-point, it is important to provide the patients with instructions, with training exercises and suitable day and or night splints, in collaboration with a physiotherapist and an occupational therapist. A specific problem is nerve injuries in combination with closed, but comminuted and dislocated, fractures.26 In most of the cases with a mid-shaft humerus fracture and a concomitant radial nerve injury, complete functional recovery of the nerve is seen, making it not necessary to explore or treat the nerve. However, if the fractured bone is treated with suitable osteosynthesis material, requiring exposure of the bone close to the suspected nerve injury, one may consider exploration of the nerve.26 In the future, the surgeon’s decision to operate or wait may be supported by the use of new techniques, such as trachtography of the injured peripheral nerve trunk.
By contrast, nerve injuries with an open wound should always be explored due to the high risk of a complete nerve injury. If there is a clear-cut injury, the nerve should be repaired immediately (for technique see below),27 whereas a crush injury with the nerve in continuity can be left for clinical follow-up (see above for classification of nerve injuries). It may be a real challenge for the surgeon and a difficult decision, regarding nerve repair or reconstruction in some specific complex cases, such as open crush injuries and gunshot wounds, since it may be difficult to judge and classify the injury. Most importantly, a careful debridement and coverage of the area with viable tissue should be accomplished. A nerve reconstruction (for technique see below) should always be performed when the bed for the nerve grafts is optimal and the risk for wound infections is low.1 In some specific cases, when there is a need for multiple debridement, and a later flap coverage, one should consider waiting with the nerve reconstruction at a later stage. However, this should be performed preferably within three weeks. In such cases, it may be simpler to define the zone of nerve injury and extent of the scar tissue, leading to an easier excision of the non-viable or scarred tissue (see below under nerve reconstruction). In the future, new imaging techniques, like trachtography, may help the surgeon’s decision-making of if and how to reconstruct the nerve trunk.
Treatment of nerve injuries
Immediate and delayed nerve repair
Surgery should always be performed in a well-anaesthetised patient and by the use of a tourniquet to ensure optimal vision. Primary immediate repair should always be the choice of method for neurobiological reasons (see previous section) and it is technically easier to perform than a delayed nerve repair (Fig. 1). The wound should also be exposed widely to ensure that no other tissue injuries are present that need simultaneous repair. A safe dissection should be done of the nerve, which is approached from the healthy tissue area down to the zone of injury. The use of microsurgical instruments, under either loop magnification or microscope, is essential in order to treat the nerve with respect and to identify non-viable tissue that should be resected using a surgical blade, or sometimes using microsurgical scissors.
Fig. 1.

Schematic drawings showing a nerve transection injury (A), after cutting necrotic parts away from the nerve ends, which is repaired after co-aptation and secured using 9-0 nylon sutures (B). Illustrations performed by Peregrin Frost.
The proximal and distal nerve ends can carefully be mobilised, which makes it possible to overcome the elastic recoil of the nerve ends occurring after the injury. In the acute stage, it may be possible to properly approximate the proximal and distal nerve ends after examining the micro-anatomy of the epineurial vessels at the surface of the nerve, thus avoiding rotation and subsequent mis-match of fibres, of the distal or proximal nerve ends during co-aptation (Fig. 1). The fascicular pattern can also be identified, together with the epineurial blood vessels, to distinguish the topographical arrangement that will facilitate a better nerve repair. It is of outmost importance to accomplish a tension-free repair of the injured nerve trunk. Tension to a peripheral nerve end is deleterious, since it may compromise the vascular supply to the nerve end with subsequent effects on the viability of the Schwann cells, which will lead to impaired axonal outgrowth.28,29 If the primary nerve repair cannot be performed without any tension a primary nerve reconstruction should be considered (for technique see below). Trimming of the injured nerve trunk, where non-viable tissue is resected, usually results in ‘mushrooming’ of the fascicles together with a slight retraction of the epineurium in the proximal and distal nerve ends. The proximal and distal nerve ends are co-apted and secured with interrupted 9-0 or 10-0 nylon sutures. The number of sutures should be no greater than the minimum number required to ensure co-aptation of the nerve ends. The nerve ends should not be closed too tightly to each other. In some circumstances, one may even advocate ‘a minimal gap’. Such a ‘minimal mm-long’ gap will be bridged by the biological healing mechanisms with formation of a fibrin matrix between the proximal and distal nerve ends across which Schwann cells and outgrowing axons can migrate.30,31 Commercial fibrin glue can be used as an alternative to sutures, or more often as an adjunct to epineurial sutures. Basically, the sutures should be applied as an epineurial nerve repair, since fascicular nerve repair usually obliges more extensive dissection of the proximal and distal nerve ends. However, for some specific nerves, such as a transection injury of the ulnar nerve at wrist level, a fascicular adaptation can be performed, since the sensory and motor nerve branches of that specific nerve are very well defined.
After the primary nerve repair, the wound should be closed with interrupted skin sutures. It is recommended that a local anaesthetic is provided in the wound before the dressing to avoid further systemic use of analgesics. Immobilisation with a plaster that primarily restricts the excessive movement and avoids tension for the nerve repair is recommended. Immobilisation is usually recommended for up to three weeks for a digital nerve repair and in repairs of larger nerve trunks, for example at wrist level or lower extremity, a six-week immobilisation is strongly recommended to avoid extensive movements. Further research is warranted in the future to evaluate if, and how, repaired nerves can be mobilised earlier.
Nerve reconstruction with nerve grafts
In the clinical situation, when the nerve injury is severe with a primary loss of nervous tissue and a co-aptation cannot be done without tension, or if it is obvious that the defect is extensive after the lacerated proximal and distal nerve ends are cleaned, a nerve reconstruction has to be performed (Fig. 2). The gold standard is still to use autologous nerve grafts,32 although other strategies, such as nerve allografts and different synthetic nerve conduits have been introduced (see below).
Fig. 2.

Schematic drawings showing a nerve injury with a defect (A), after resection of the lacerated parts of the bundles of fascicles (sometimes done in steps as indicated). The nerve defect is reconstructed using nerve grafts (here four cables attached), which are secured with single 9-0 nylon sutures (B). After application of the sutures fibrin glue is usually applied (shown in Fig. 3). Illustrations performed by Peregrin Frost.
Before the nerve ends are prepared, a proper skin incision, preserving any flaps, is done making it easy to close the wound with good tissue coverage of the reconstructed area. The initial steps in nerve grafting are to prepare the nerve tissue, which is the same as the procedures done when a primary nerve repair is performed. It is of outmost importance that the nerve ends are properly resected to create a clean-cut surface, where there are no remaining scar tissues or non-viable tissue (Fig. 2). A simple rule is to observe that mushrooming is present, indicating that there is a fresh nerve end suitable for attachment of the graft. After resection of the non-viable proximal and distal nerve ends and presence of adequate mushrooming, the maximum length of the defect is measured. Due to the fact that the autologous nerve grafts may shrink at about 10% to 15%, the graft should exceed the maximum length of the nerve defect by that percentage.
Donor nerves can be harvested from different common locations and should be selected with having the size and length of the defect of the specific reconstructed nerve in mind. The most common nerve grafts are the sural nerve, the medial antebrachial cutaneous nerve, the lateral antebrachial cutaneous nerve and the terminal branch of the posterior interosseous nerve. The last three nerves can be used to graft smaller nerves, like the common digital nerves and the proper digital nerves in the hand, while the sural nerve, with application of several cables, is suitable to bridge nerve defects in major nerve trunks, like the radial, ulnar and median nerves as well as the nerves in the lower extremity, for example the sciatic and tibial nerves (Fig. 3). The donor nerve should be harvested with caution and care taken to keep it moist to avoid drying. If the nerve is dried, the viability of the Schwann cells is compromised with subsequent impairment of the regeneration in the graft; thus, jeopardising the whole graft procedure.33 The autologous nerve graft should preferably be reversed when it is placed in the nerve defect.
Fig. 3.
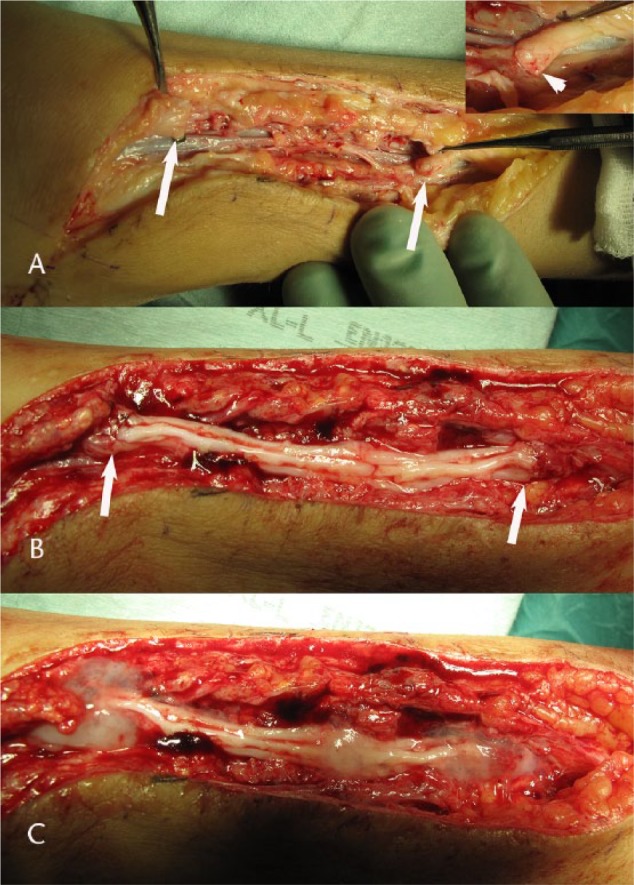
Intra-operative photographs showing the steps in reconstruction of a tibial nerve trunk in the lower leg using the sural nerve as cables in the nerve graft procedure. The proximal and distal nerve ends (arrows) are carefully resected (A) visualising healthy nerve fascicles (shown in the insert in the upper corner in A; arrowhead). Sural nerve cables are individually attached between the nerve ends (arrows indicating the proximal (right) and distal (left) nerve ends) and secured with single 9-0 nylon sutures (hardly seen; B). Finally, fibrin glue is applied around the proximal and distal site of attachment, respectively (grey substance around the sites; C).
After a sufficient number of cables of the donor nerve have been applied to cover most of the area of the injured nerve ends, and secured with single 9-0 nylon sutures, the co-aptation is sometimes accomplished with fibrin glue, which is applied around the two sites of co-aptation, preferably formed as a conduit only around the close interface between the graft and the nerve end (Fig. 3). The individual nerve graft cables should be positioned precisely in the tissue bed and not adhere too closely to each other, since the survival of the nerve grafts requires diffusion of oxygen and other nutrients as well as re-vascularisation from the surrounding tissue bed. Re-vascularisation probably occurs through ingrowth of capillaries, from both the surroundings and the proximal and distal nerve ends. Angiogenesis occurs in close connection with the migration of Schwann cells and axonal outgrowth.31 When bridging a defect in a proper digital nerve, it may be enough with a single nerve graft, like the terminal branch of the posterior interosseous nerve. The latter nerve graft is suitable since it does not create any residual problems for the patient.1 Furthermore, the risk for residual problems after harvesting the sural nerve for autologous nerve reconstruction procedures in the other major nerve trunks is very low.34
Alternative nerve reconstruction procedures
Even if the gold standard to bridge nerve defects is an autologous nerve grafting procedure, there might be some disadvantages related with the use of such grafts, such as the lack of graft material, time for the procedure to harvest donor nerves, scarring and mismatch between the injured nerve and the grafts.1,35 Therefore, alternatives have been developed to bridge nerve defects, which include particularly processed acellular nerve allografts (i.e. extracted nerve grafts),36-38 and various biodegradable nerve conduits composed of different polymer-based materials (e.g. polyglycolic acid polymer, polylactide caprolactone polymer, polyhydroxy butyrate)39 and other available materials (such as chitosan conduits40 and collagen conduits).41 However, these alternatives seem to be best used to reconstruct short nerve defects. The technique of using the processed acellular nerve allografts is similar to that for autologous nerve grafts.36 Application of a nerve conduit is simple by using one or two 9-0 sutures at each end by going through the wall of the conduit, hooking up the epineurium of the injured nerve end and then going with the needle back through the wall of the conduit or by using a sheath that is wrapped around the injured nerve ends and then secured with sutures as above. By these techniques, the nerve ends can easily be positioned into the conduit a few mm as described earlier.39,42 In the future, it should be possible that new three-dimensional (3D) printed biologically suitable materials formed as a nerve graft can be designed and produced for the individual patient with a nerve injury. Such materials can be populated with various specific and suitable cells, e.g. with the function of Schwann cells, obtained from the patient’s own cells, such as fibroblasts, and produced by cell reprogramming technologies.43
Nerve transfers: new alternatives to re-innervate muscles
The practice of nerve transfers has been highlighted during recent years to reconstruct nerve injuries, particularly when the injury is located in the brachial plexus, but is also applicable after other nerve injuries. A number of different nerve transfer procedures have been developed for re-innervation of muscles in the proximal extremity as well as in the distal extremity and hand.44-48 The main advantage of nerve transfers is to ‘move the nerve co-aptation more close to the target organ’, which reduces the time until re-innervation. There are some specific indications for the use of nerve transfers, such as a brachial plexus injury with root avulsions (i.e. unsuitable proximal nerve ends), a proximal nerve lesion with a long distance to the target organs, nerve injuries where very long nerve graft may be needed (i.e. > 10 cm), a long time interval from injury to nerve reconstruction (i.e. also depending on the level of injury due to the condition of the distal nerve end), heavily scarred tissue areas where there is a risk of damaging other vital structures at exploration and a previously failed proximal nerve reconstruction. Contra-indications are when there are better surgical solutions (i.e. a more direct nerve reconstruction), a severe degeneration of the target muscle due to long time from injury as well as the strength of the donor nerve below M4 (MRC-scale M0 to M5). The donor site morbidity should also be considered, since there may be a risk of reducing function of the muscle/s innervated by the donor nerve.49
The general surgical rules for peripheral nerve repair and reconstruction are applicable also for nerve transfers, where an accurate and meticulous dissection, using loupes, should be done, particularly avoiding unnecessary donor site morbidity. Both the donor and recipient nerve should be tested with direct electrical stimulation. In the first surgical step, the recipient nerve is isolated and tested. If there are no signs of recovery, the transfer is indicated and the donor nerve is explored. The nerves are then divided using the rules for dividing the nerves: ‘donor distal’ and ‘recipient proximal’ and again with the intention to completely avoid tension or any need for nerve grafts.49 The co-aptation is used as for a nerve reconstruction, where a single suture is applied and a possible further secure of the co-aptation with fibrin glue (Fig. 4).
Fig. 4.
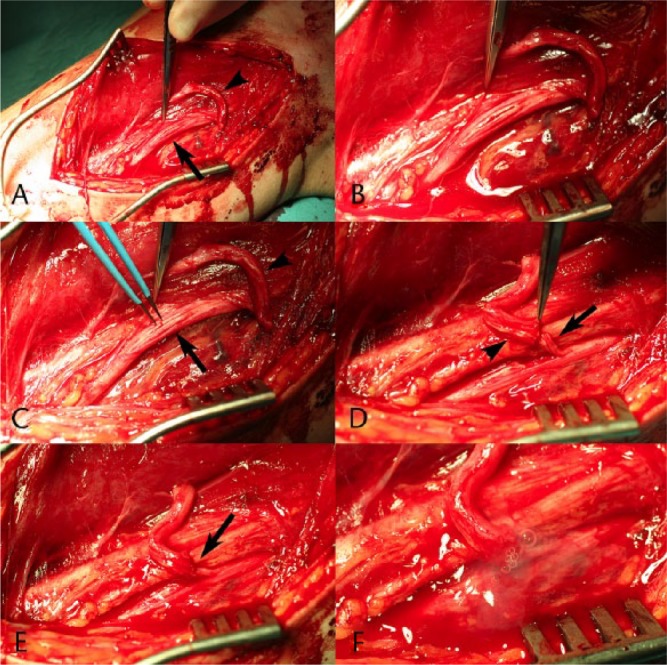
Intra-operative photographs showing a nerve transfer procedure, where the ulnar nerve (A; arrow) is used to reconstruct an injured musculocutaneous nerve (distal nerve end indicated by arrowhead). A few nerve fascicles, innervating the flexor carpi ulnaris muscle, from an intact ulnar nerve (B) are identified with electrical stimulation (C; arrow), transected and transferred (D; arrow) to the distal end of the initially injured musculocutaneous nerve (D; arrowhead). The axons from the ulnar nerve are in this way allowed to regenerate through the site of repair (E; arrow) through the musculocutaneous nerve down to the target, i.e. biceps and brachialis muscles. The nerve repair is finally secured with fibrin glue (F; grey substance). During the rehabilitation period, the patient learns how to use the ulnar nerve fibres in elbow flexion by using cerebral plasticity.
A common nerve transfer is transfer of one radial nerve branch (i.e. one that innervates the lateral head of the triceps) to the distal axillary nerve to restore axillary nerve function.50 The branches of the radial nerve going to the lateral head of the triceps muscle should preferably be used instead of the branches to the long or the medial heads of the triceps. After transection of the appropriate radial nerve branch, it is transferred up to the axillary nerve, which is divided and the sensory branch of the axillary nerve is removed in order to concentrate all the available proximal axons from the radial nerve branch down into the motor component of the axillary nerve. Again, the nerves are co-aptated with a single suture without any tension and possibly with fibrin glue as an adjunct. Different authors advocate the use of the medial or long heads of the triceps muscle, but it may be recommended not to use the branch to the medial head since it is important for powerful elbow extension.50,51
Another common and successful nerve transfer is transfer of a few ulnar nerve fascicles to the biceps motor branches (i.e. the classical Oberlin procedure)52 to restore elbow flexion. Approximately two fascicles with predominant innervation of the flexor carpi ulnaris muscle of the ulnar nerve are identified by electrical stimulation after fascicular dissection. These few fascicles are transferred at the upper arm to the distal musculocutaneous nerve as close as possible to the muscle belly of the biceps muscle with the same technique as described above (Fig. 4).
Another example of nerve transfer is partial median nerve fascicle transfer (i.e. innervating predominantly the flexor carpi radialis or the palmaris longus muscles) to the musculocutaneous nerve branch innervating the biceps muscle. Sometimes this transfer is combined with the mentioned Oberlin procedure, where the fascicles from the ulnar nerve are connected to the biceps motor nerve branch and the fascicles from the median nerve are connected to the brachialis motor nerve branch (i.e. double fascicular transfer), which will lead to better elbow flexion. Furthermore, the flexor carpi ulnaris or extensor carpi radialis brevis motor nerve branches can be connected to the pronator teres branch to improve pronation of the forearm. The distal anterior interosseous nerve can be transferred to the ulnar nerve motor branch to restore the function of the intrinsic muscles of the hand. Branches in the median nerve that innervate the superficial finger flexor muscles, flexor carpi radialis or palmaris longus muscles can be identified and connected to the branches of the radial nerve supplying the extensor carpi radialis brevis muscles and to the posterior interosseous nerve to restore wrist and finger extension. Finally, there are also sensory transfers available, which are less often used.49
Rehabilitation after a nerve transfer is a challenging task, where the patient, together with physiotherapists, has to activate the new function by co-contraction of the donor and recipient muscles at the same time, e.g. train ulnar wrist flexion at the same time as the patient thinks about elbow flexion. In this context, cerebral plasticity mechanisms are decisive for the success of the nerve transfer21 and in the future new rehabilitation methods may further improve outcome.
Post-operative care
There is still a debate about the rule of early active mobilisation after microsurgical nerve repair and reconstruction. Early mobilisation may increase the risk for tension at the site of the nerve repair and reconstruction resulting in impaired functional outcome. On the other hand, immobilisation may create scar tissue with adhesions around the nerve causing secondary problems. Most importantly, nerve grafts should be applied at a minimal tension in order to allow full range of motion without causing tension over the site of reconstruction. The surgeon, with close collaboration of physiotherapists and occupational therapists, should execute supervision of the rehabilitation procedure, including detection of the progression of Tinel’s sign distally from the site of injury and judgement of return of muscle function: ‘active surveillance’.1 Immobilisation is generally recommended three weeks after a nerve reconstruction, although some authors advocate mobilisation after a week when active and passive mobilisation is initiated. After some nerve reconstructions, such as at the wrist and in the thigh, it is recommended to use prolonged protection up to six weeks post-operatively.
Cortical re-organisation and sensory re-education
The cortical organisation of the neurons executing motor and sensory functions in the extremities are very well structured, where, for example, the projection area in the brain reflects the delicate functions of the extremities. The hand is well represented in the brain (e.g. see the homunculus figure) and the individual fingers are projected like bands in the somatosensory area. After a nerve injury, there is a ‘silent area’ created by the injured nerve’s representational area in the brain, and the brain compensates for loss of sensory input with adjacent cortical neurones expanding their function into the ‘silent area’ by specific mechanisms involving both hemispheres.21 After the injury and repair or reconstruction, the original well-organised hand representation will not be achieved in adults (i.e. after puberty), but a distorted and mosaic-like pattern with disappearance of, as well as overlapping of, fingers in the brain appears. Due to these events, one usually expresses it as ‘the hand speaks a new language to the brain’. These phenomena are used in the training of the patients after nerve repairs, reconstructions or nerve transfers and are divided into two phases, where phases one and two denote training before and after, respectively, the re-innervation of the targets.53 Thus, relearning programmes are initiated that helps the patient to interpret the new language spoken by the hand. The effectiveness of the relearning and sensory re-education processes is influenced by the motivation of each individual patient, where we consider that each individual patient is provided with coping strategies.54-56 Coping is the process where the patient’s resources are used to adapt to the condition (i.e. injury) and overcome the problems in daily activities,54,55 an area of research that will probably expand in the future.
Outcomes
The outcome after a nerve repair or reconstruction procedure should be carefully assessed, where the final evaluation may be necessary at least two to three years after the procedures since re-innervation and sensory re-education processes are progressing during this time-period.1 However, electrophysiological improvement can be seen at least five years after median or ulnar nerve repair at wrist level.57 Generally, there is no real consensus about how to evaluate outcome in a standardised manner covering all types of nerve injuries, although a specific scoring system has been described and validated for median and ulnar nerve repairs at wrist level (i.e. the Rosen score).58,59 There are different protocols to assess outcome, such as the British Medical Research Council Scale.60,61 However, some criticism may be raised against these scales since they are based on subjective findings, although the patient’s subjective experience is the most important as outcome. The lack of validated scoring systems may complicate our ability to introduce new treatment strategies and compare different sets of patients as well as the outcome from different observers that is important for stringency in randomised clinical studies. In the future, research projects will probably optimally define how outcome should be evaluated with the purpose to collect results of various nerve procedures in national registries (e.g. www.hakir.se; see English version).
Factors relevant for outcome
There are a number of factors, while some of them are not possible to influence, that affect outcome. For recovery of motor function, age, delay before repair or reconstruction, the level of injury as well as type of the injured nerve are important.62 Similarly, age and delay before repair or reconstruction are the most important factors that influence recovery of sensory function.62 Age deserves a specific comment, since there is a clear association between the age of the patient and recovery of specifically sensory function. One may consider that superior nerve regeneration processes as well as shorter regeneration distances explain the better outcome in children after nerve injury or reconstruction. However, the main factor is that children have a greater adaptability in the brain to compensate for the sub-optimal nerve regeneration mechanisms with mis-direction of fibres.22 Children, who have sustained a median nerve injury that was repaired or reconstructed before the age of 12 years, have an almost similar activation pattern in the brain as healthy participants. Recent data indicate that changes in both brain hemispheres are relevant, indicating the significance of inter-hemispheric communication.63
Post-traumatic neuroma: symptoms, diagnosis and treatment
When a peripheral nerve sustains either a partial or a total injury, which interrupts the axonal continuity (Seddon axonotmesis and neurotmesis; Sunderland 2 to 5, even grade 6)64 (Table 1), there is a cascade of events aimed at regeneration as described in the first part of the review.18,65 However, regeneration is not always possible, and even if the injured nerve is optimally repaired or only partially damaged, there is a rapid retrograde neuronal loss of mainly sensory neurones in the dorsal root ganglia66 with a secondary cascade of events in the central nervous system with subsequent re-organisation both at the spinal and supraspinal levels.64 Even at the injury site, there will be a regeneration of only about 50% of the remaining surviving sensory neurones for unclear reasons, but possibly due to sub-optimal re-alignment of fascicles.13 All these events could probably take part in the formation of the syndrome of post-traumatic neuroma. This means that pain after a traumatic nerve injury could be a result of peripheral and/or central events, while a neuroma is normally defined as the formation of a swelling at the proximal nerve end, consisting of a disorganised regeneration of axons together with a mixture of cells, such as Schwann cells, endothelial cells, macrophages and fibroblasts. A neuroma may be formed when a transected nerve is not repaired or when the repair itself does not allow the re-growing axons to find their distal nerve end. However, why some patients develop a neuroma and others not, even when one thinks they are treated in a similar way, is more difficult to understand. Luckily, taking into account the high number of traumatic nerve injuries, mainly in the upper limb, the incidence of neuroma is low.67
The diagnosis of a neuroma is mainly by examination with clinical findings, such as localised pain, sensory disturbances, allodynia, hyper-/dysaesthesia and a positive Tinel’s sign. In some cases, ultrasound examination and/or MRI will add further information about the location and structure of the neuroma.
Several treatment strategies, either operative or non-operative, have been used, indicating that none of them is optimal. The non-operative techniques consist mainly of pharmacological substances (i.e. antidepressants, opioids, anticonvulsants), local nerve-destruction/inhibiting methods (e.g. injection of phenol or botulinum toxin, bipolar cautery, cryotreatment) or rehabilitation (e.g. desensitisation, TNS, acupuncture, work modification, psychotherapy). The operative treatment mainly aims to relocate the injured nerve and its neuroma from mechanical irritation, which normally means relocating it to a deeper site. In those cases where there is an end-neuroma, i.e. a totally injured nerve with a neuroma formation, the neuroma bulb is normally resected before the relocation is performed.67 Several sites for relocation have been used, such as bone, muscle, tendons and veins, depending on the location; none is perfect and give varying results.68 Another surgical technique to reduce the irritation of a neuroma is by different ways of ‘wrapping’, either using different flaps to enhance local circulation in addition to protect the neuroma or different ways of entubulation (e.g. veins, synthetic conduits).68 A specific problem is seen when having a ‘neuroma-in-continuity’, where the nerve is only partially damaged, but the damaged part has created a neuroma. Thus, there is a fear of further damage to the nerve by an additional surgical intervention. In those cases, where surgery is strongly considered, neurolysis and a possible resection of the neuroma with additional grafting or entubulation with conduits can be used. For small nerves, even a surgical transection, in addition with the neuroma resection and relocation, can be an alternative, even if this would result in further sensory loss.67
Nerve injury: the risk for severe disability and complex regional pain syndrome
A patient with an injured peripheral nerve has a high probability of disability and subsequent social consequences, leading to dramatic impact of the specific person’s capacity to function adequately as well as having effects on their professional life with psychological mechanisms,56 thus with high risks for further affecting their daily life. The dysfunctions, such as motor and sensory dysfunction, pain problems, allodynia and cold intolerance, can be partly compensated depending on an individual patient’s ability to use coping strategies to handle the injury. However, the most serious dysfunction after a nerve injury is development of the complex regional pain syndrome (CRPS), consisting of types 1 and 2, reflected in that the latter requires a known nerve injury. CRPS is a disabling condition and set by a clinical diagnosis, involving symptoms of regional pain, burning and aching in nature, together with autonomic dysfunction, functional impairment and atrophy. Surgeons should be alert to find patients that develop the initial signs of CRPS early.69 Cigarette smokers and women have a higher risk for CRPS, although the condition strikes at any age, but most commonly around middle age. Different types of treatment strategies should be promptly initiated. Rehabilitation methods are probably the most effective since there are no single or simple successful pharmacological treatments available, and poly-pharmacy should be avoided.69
In order to improve outcome after various procedures for a nerve injury, the key point is that surgeons and physicians are aware of the risk of nerve injuries in connection with any trauma to the upper or lower extremities. An initial and careful clinical examination, sometimes repeated, leading to the correct diagnosis and early exploration with subsequent appropriate surgical treatment is advocated in injuries with wounds. A conservative attitude may be relevant in closed nerve injuries, but a meticulous and regular re-evaluation of the patient—‘active surveillance’—to follow any recovery is advocated. In the future, any improved imaging techniques, such as 3D high-resolution MRI with diffusion tensor imaging and tractography, may be tools that can improve the diagnostic accuracy, but cannot replace the initial and appropriate basic clinical examination. Neuroma formation and CRPS type 2, involving complex peripheral and central mechanisms, are unpredictable and difficult to treat. The best recommendation to minimise neuroma formation is prompt and optimal treatment of nerve injuries. Thorough knowledge about the neurobiological mechanisms in nerve injury and during repairs, reconstructions and transfers are crucial for any surgeon that treats peripheral nerve injuries
Footnotes
ICMJE Conflict of Interest Statement: LD reports that he is a consultant for Pergamum AB.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Farnebo S, Thorfinn J, Dahlin LB. Peripheral nerve injuries of the upper extremity. In: Neligan PC, Chang J, van Beek AL, eds. Hand Surgery (A volume in the Plastic Surgery 6-Volume Set: Expert Consult Premium). Third ed. China: Elsevier Saunders, 2012. [Google Scholar]
- 2. Asplund M, Nilsson M, Jacobsson A, von Holst H. Incidence of traumatic peripheral nerve injuries and amputations in Sweden between 1998 and 2006. Neuroepidemiology 2009;32:217-228. [DOI] [PubMed] [Google Scholar]
- 3. Maripuu A, Björkman A, Björkman-Burtscher IM, et al. Reconstruction of sciatic nerve after traumatic injury in humans - factors influencing outcome as related to neurobiological knowledge from animal research. J Brachial Plex Peripher Nerve Inj 2012;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rosberg HE, Carlsson KS, Höjgård S, et al. Injury to the human median and ulnar nerves in the forearm–analysis of costs for treatment and rehabilitation of 69 patients in southern Sweden. J Hand Surg Br 2005;30:35-39. [DOI] [PubMed] [Google Scholar]
- 5. Thorsén F, Rosberg HE, Steen Carlsson K, Dahlin LB. Digital nerve injuries: epidemiology, results, costs, and impact on daily life. J Plast Surg Hand Surg 2012;46:184-190. [DOI] [PubMed] [Google Scholar]
- 6. Lundborg G. Intraneural microcirculation. Orthop Clin North Am 1988;19:1-12. [PubMed] [Google Scholar]
- 7. Geuna S, Haastert-Talini K, Navarro X. The nerve trunk in injury and during regeneration. In: Dahlin LB, Leblebicioglu G, eds. Current treatment of nerve injuries and disorders. Zurich: Palmer Publications; 2013:51-61. [Google Scholar]
- 8. Seddon HJ. Surgical disorders of the peripheral nerves. Second ed. Edinburgh: Churchill Livingstone, 1975. [Google Scholar]
- 9. Sunderland S. Nerves and nerve injuries. Second ed. Edinburgh: Churchill Livingstone, 1978. [Google Scholar]
- 10. Dahlin LB. The role of timing in nerve reconstruction. Int Rev Neurobiol 2013;109:151-164. [DOI] [PubMed] [Google Scholar]
- 11. Sulaiman W, Gordon T. Neurobiology of peripheral nerve injury, regeneration, and functional recovery: from bench top research to bedside application. Ochsner J 2013;13:100-108. [PMC free article] [PubMed] [Google Scholar]
- 12. Raivich G, Makwana M. The making of successful axonal regeneration: genes, molecules and signal transduction pathways. Brain Res Rev 2007;53:287-311. [DOI] [PubMed] [Google Scholar]
- 13. Welin D, Novikova LN, Wiberg M, Kellerth JO, Novikov LN. Survival and regeneration of cutaneous and muscular afferent neurons after peripheral nerve injury in adult rats. Exp Brain Res 2008;186:315-323. [DOI] [PubMed] [Google Scholar]
- 14. McKay Hart A. Sensory neuronal protection & improving regeneration after peripheral nerve injury. [Doctoral thesis]: Umeå University; (2003). [Google Scholar]
- 15. Geuna S, Fornaro M, Raimondo S, Giacobini-Robecchi MG. Plasticity and regeneration in the peripheral nervous system. Ital J Anat Embryol 2010;115:91-94. [PubMed] [Google Scholar]
- 16. Saito H, Dahlin LB. Expression of ATF3 and axonal outgrowth are impaired after delayed nerve repair. BMC Neurosci 2008;9:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gordon T, Tyreman N, Raji MA. The basis for diminished functional recovery after delayed peripheral nerve repair. J Neurosci 2011;31:5325-5334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jonsson S, Wiberg R, McGrath AM, et al. Effect of delayed peripheral nerve repair on nerve regeneration, Schwann cell function and target muscle recovery. PLoS One 2013;8:e56484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fex Svennigsen A, Dahlin LB. Repair of the peripheral nerve-remyelination that works. Brain Sci 2013;3:1182-1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Andersson- Sjöland A, Nihlberg K, Eriksson L, Bjermer L, Westergren-Thorsson G. Fibrocytes and the tissue niche in lung repair. Respir Res 2011;12:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Björkman A. Cerebral reorganization after nerve injury. In: Dahlin LB, Leblebicioglu G, eds. Current treatment of nerve injuries and disorders. Davut Öztürk. Zurich: Palmer Publications; 2013:81-92. [Google Scholar]
- 22. Chemnitz A, Björkman A, Dahlin LB, Rosén B. Functional outcome thirty years after median and ulnar nerve repair in childhood and adolescence. J Bone Joint Surg [Am] 2013;95:329-337. [DOI] [PubMed] [Google Scholar]
- 23. Robinson LR. How electrodiagnosis predicts clinical outcome of focal peripheral nerve lesions. Muscle Nerve 2015;52:321-333. [DOI] [PubMed] [Google Scholar]
- 24. Terenghi G, Hart A, Wiberg M. The nerve injury and the dying neurons: diagnosis and prevention. J Hand Surg Eur Vol 2011;36:730-734. [DOI] [PubMed] [Google Scholar]
- 25. Jivan S, Kumar N, Wiberg M, Kay S. The influence of pre-surgical delay on functional outcome after reconstruction of brachial plexus injuries. J Plast Reconstr Aesthet Surg 2009;62:472-479. [DOI] [PubMed] [Google Scholar]
- 26. Thomsen NO, Dahlin LB. Injury to the radial nerve caused by fracture of the humeral shaft: timing and neurobiological aspects related to treatment and diagnosis. Scand J Plast Reconstr Surg Hand Surg 2007;41:153-157. [DOI] [PubMed] [Google Scholar]
- 27. Dahlin LB. Techniques of peripheral nerve repair. Scand J Surg 2008;97:310-316. [DOI] [PubMed] [Google Scholar]
- 28. Yi C, Dahlin LB. Impaired nerve regeneration and Schwann cell activation after repair with tension. Neuroreport 2010;21:958-962. [DOI] [PubMed] [Google Scholar]
- 29. Scherman P, Kanje M, Dahlin LB. Bridging short nerve defects by direct repair under tension, nerve grafts or longitudinal sutures. Restor Neurol Neurosci 2004;22:65-72. [PubMed] [Google Scholar]
- 30. Dahlin L, Brandt J, Nilsson A, Lundborg G, Kanje M. Schwann cells, acutely dissociated from a predegenerated nerve trunk, can be applied into a matrix used to bridge nerve defects in rats. Acta Neurochir Suppl 2007;100:57-59. [DOI] [PubMed] [Google Scholar]
- 31. Brandt J, Dahlin LB, Kanje M, Lundborg G. Spatiotemporal progress of nerve regeneration in a tendon autograft used for bridging a peripheral nerve defect. Exp Neurol 1999;160:386-393. [DOI] [PubMed] [Google Scholar]
- 32. Millesi H. Nerve grafting. Clin Plast Surg 1984;11:105-113. [PubMed] [Google Scholar]
- 33. Widerberg A, Dahlin LB. Reduction of proliferating non-neuronal cells in dried nerve segments partly impairs nerve regeneration. Neuroreport 2000;11:2707-2709. [DOI] [PubMed] [Google Scholar]
- 34. Hallgren A, Björkman A, Chemnitz A, Dahlin LB. Subjective outcome related to donor site morbidity after sural nerve graft harvesting: a survey in 41 patients. BMC Surg 2013;13:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wiberg M, Terenghi G. Will it be possible to produce peripheral nerves? Surg Technol Int 2003;11:303-310. [PubMed] [Google Scholar]
- 36. Vögelin E, Juon B. Nerve allografts and vein grafts in nerve reconstruction. In: Dahlin LB, Leblebicioglu G, eds. Current treatment of nerve injuries and disorders. Zurich: Palmer Publications, 2013:272-278. [Google Scholar]
- 37. Kvist M, Sondell M, Kanje M, Dahlin LB. Regeneration in, and properties of, extracted peripheral nerve allografts and xenografts. J Plast Surg Hand Surg 2011;45:122-128. [DOI] [PubMed] [Google Scholar]
- 38. Rinker BD, Ingari JV, Greenberg JA, et al. Outcomes of short-gap sensory nerve injuries reconstructed with processed nerve allografts from a multicenter registry study. J Reconstr Microsurg 2015;31:384-390. [DOI] [PubMed] [Google Scholar]
- 39. Aberg M, Ljungberg C, Edin E, et al. Clinical evaluation of a resorbable wrap-around implant as an alternative to nerve repair: a prospective, assessor-blinded, randomised clinical study of sensory, motor and functional recovery after peripheral nerve repair. J Plast Reconstr Aesthet Surg 2009;62:1503-1509. [DOI] [PubMed] [Google Scholar]
- 40. Haastert-Talini K, Geuna S, Dahlin LB, et al. Chitosan tubes of varying degrees of acetylation for bridging peripheral nerve defects. Biomaterials 2013;34:9886-9904. [DOI] [PubMed] [Google Scholar]
- 41. Boeckstyns ME, Sørensen AI, Viñeta JF, et al. Collagen conduit versus microsurgical neurorrhaphy: 2-year follow-up of a prospective, blinded clinical and electrophysiological multicenter randomized, controlled trial. J Hand Surg Am 2013;38:2405-2411. [DOI] [PubMed] [Google Scholar]
- 42. Dahlin LB, Lundborg G. Use of tubes in peripheral nerve repair. Neurosurg Clin N Am 2001;12:341-352. [PubMed] [Google Scholar]
- 43. Chen G, Wernig M, Berninger B, et al. In vivo reprogramming for brain and spinal cord repair. eNeuro 2015;2;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mackinnon SE. Donor distal, recipient proximal and other personal perspectives on nerve transfers. Hand Clin 2016;32:141-151. [DOI] [PubMed] [Google Scholar]
- 45. Bulstra LF, Shin AY. Nerve transfers to restore elbow function. Hand Clin 2016;32:165-174. [DOI] [PubMed] [Google Scholar]
- 46. Pet MA, Lipira AB, Ko JH. Nerve transfers for the restoration of wrist, finger, and thumb extension after high radial nerve injury. Hand Clin 2016;32:191-207. [DOI] [PubMed] [Google Scholar]
- 47. Soldado F, Bertelli JA, Ghizoni MF. High median nerve injury: motor and sensory nerve transfers to restore function. Hand Clin 2016;32:209-217. [DOI] [PubMed] [Google Scholar]
- 48. Patterson JM. High ulnar nerve injuries: nerve transfers to restore function. Hand Clin 2016;32:219-226. [DOI] [PubMed] [Google Scholar]
- 49. Calcagni M, Giovanoli P. Peripheral nerve transfers. In: Dahlin LB, Leblebicioglu G, eds. Current treatment of nerve injuries and disorders. Davut Öztürk. Zurich: Palmer Publications, 2013:286-295. [Google Scholar]
- 50. Dahlin LB, Cöster M, Björkman A, Backman C. Axillary nerve injury in young adults–an overlooked diagnosis? Early results of nerve reconstruction and nerve transfers. J Plast Surg Hand Surg 2012;46:257-261. [DOI] [PubMed] [Google Scholar]
- 51. Desai MJ, Daly CA, Seiler JG, III, et al. Radial to axillary nerve transfers: a combined case series. J Hand Surg Am 2016;41:1128-1134. [DOI] [PubMed] [Google Scholar]
- 52. Oberlin C, Béal D, Leechavengvongs S, et al. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: anatomical study and report of four cases. J Hand Surg Am 1994;19:232-237. [DOI] [PubMed] [Google Scholar]
- 53. Lundborg G, Rosén B. Hand function after nerve repair. Acta Physiol (Oxf) 2007;189:207-217. [DOI] [PubMed] [Google Scholar]
- 54. Cederlund RI, Ramel E, Rosberg HE, Dahlin LB. Outcome and clinical changes in patients 3, 6, 12 months after a severe or major hand injury–can sense of coherence be an indicator for rehabilitation focus? BMC Musculoskelet Disord 2010;11:286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cederlund R, Thorén-Jönsson AL, Dahlin LB. Coping strategies in daily occupations 3 months after a severe or major hand injury. Occup Ther Int 2010;17:1-9. [DOI] [PubMed] [Google Scholar]
- 56. Chemnitz A, Dahlin LB, Carlsson IK. Consequences and adaptation in daily life – patients’ experiences three decades after a nerve injury sustained in adolescence. BMC Musculoskelet Disord 2013;14:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lundborg G, Rosén B, Dahlin L, Holmberg J, Rosén I. Tubular repair of the median or ulnar nerve in the human forearm: a 5-year follow-up. J Hand Surg Br 2004;29:100-107. [DOI] [PubMed] [Google Scholar]
- 58. Rosén B, Lundborg G. A model instrument for the documentation of outcome after nerve repair. J Hand Surg Am 2000;25:535-543. [DOI] [PubMed] [Google Scholar]
- 59. Rosén B. Recovery of sensory and motor function after nerve repair. A rationale for evaluation. J Hand Ther 1996;9:315-327. [DOI] [PubMed] [Google Scholar]
- 60. Novak CB, Kelly L, Mackinnon SE. Sensory recovery after median nerve grafting. J Hand Surg Am 1992;17:59-68. [DOI] [PubMed] [Google Scholar]
- 61. Dellon AL, Curtis RM, Edgerton MT. Reeducation of sensation in the hand after nerve injury and repair. Plast Reconstr Surg 1974;53:297-305. [DOI] [PubMed] [Google Scholar]
- 62. Ruijs AC, Jaquet JB, Kalmijn S, Giele H, Hovius SE. Median and ulnar nerve injuries: a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plast Reconstr Surg 2005;116:484-494. discussion 495-496. [DOI] [PubMed] [Google Scholar]
- 63. Chemnitz A, Weibull A, Rosén B, et al. Normalized activation in the somatosensory cortex 30 years following nerve repair in children: an fMRI study. Eur J Neurosci 2015;42:2022-2027. [DOI] [PubMed] [Google Scholar]
- 64. Birch R, Bonney G, Wynn Parry CB. Surgical disorders of the peripheral nerves. London: Churchill Livingstone, 1998. [Google Scholar]
- 65. Reid AJ, Welin D, Wiberg M, Terenghi G, Novikov LN. Peripherin and ATF3 genes are differentially regulated in regenerating and non-regenerating primary sensory neurons. Brain Res 2010;1310:1-7. [DOI] [PubMed] [Google Scholar]
- 66. Hart AM, Terenghi G, Kellerth JO, Wiberg M. Sensory neuroprotection, mitochondrial preservation, and therapeutic potential of N-acetyl-cysteine after nerve injury. Neuroscience 2004;125:91-101. [DOI] [PubMed] [Google Scholar]
- 67. Elliot D, Sierakowski A. The surgical management of painful nerves of the upper limb: a unit perspective. J Hand Surg Eur Vol 2011;36:760-770. [DOI] [PubMed] [Google Scholar]
- 68. Brogan DM, Kakar S. Management of neuromas of the upper extremity. Hand Clin 2013;29:409-420. [DOI] [PubMed] [Google Scholar]
- 69. Dahlin LB, Søe N. Complex regional pain syndrome. In: Murray PM, Hammert WC. editors. Hand Surgery Update VI. Chicago: The American Society for Surgery of the Hand (ASSH), 2016. [Google Scholar]


