Abstract
Chronic infections are one of the major challenges in orthopaedic surgery, both for surgeons and patients. They are characterised by obstinate persistency of the causing microorganisms and resulting long-term disablement of the patients, associated with remarkable costs for the health care system.
Difficulties derive from the biofilm-mode of living of pathogens with resistances against immunological defence and antimicrobial substances, and osseous defects resulting from the disease itself and surgical interventions.
Established techniques usually require multiple costly operations with extended periods of disablement and impairment of the patients, sometimes making the therapy worse than the disease.
Better understanding of the backgrounds of the conditions has led to new surgical techniques and differentiated application of antibiotics, aiming in improved quality of life for our patients.
Cite this article: EFORT Open Rev 2017;2. DOI: 10.1302/2058-5241.2.160063. Originally published online at www.efortopenreviews.org
Keywords: chronic orthopaedic infection, biofilm, chronic osteomyelitis, prosthetic joint infection, antibiotic delivery, bone defect, effective therapy
Introduction1
Most orthopaedic infections arise as sequela to traumatic episodes and during surgery, especially when foreign material is implanted, as in osteosynthesis or total joint replacement (TJR). Bacteria, mostly staphylococci, are able to bind to damaged tissue and implanted material with immediate formation of biofilms that may be considered mature after several days. Clinical signs persisting for longer than ten days are associated with the development of necrotic bone and chronic osteomyelitis (COM). COM and prosthetic joint infection (PJI) are characterised by the persistence of micro-organisms on dead bone and implants, causing low-grade inflammation with occasional acute episodes, eventually associated with fistulous tracts. Removal of dead material is a prerequisite for cure. However, there is no consensus on the time interval between debridement and definitive reconstruction. The second procedure is mostly performed when clinical findings and laboratory parameters have returned to normal. In the meantime, external fixators and/or spacers will provide some temporary stabilisation while systemic and/or local antibiosis will sterilise the infected site. However, the prolonged hospitalisation and its associated costs, the delayed mobilisation and rehabilitation, and the risk of multiple surgery are marked drawbacks, especially in elderly patients. Is it worthwhile to wait?
Difficulties of treatment derive from two distinct issues: 1) resistance of the causing pathogens against antimicrobials and immunological defences; and 2) osseous defects caused by osteolysis, sequestration and surgical interventions.
Biofilm
Most failures derive from the traditional conceptions of antimicrobial treatment dealing with freely floating planktonic bacteria. In orthopaedic infections, our most obstinate opponents are not the familiar planktonic pathogens but their phenotypically different sessile forms embedded in an extracellular matrix, the glycocalix.2-4 The surface of unvascularised bone and eventually implants acts as a substratum for the attachment of bacteria and the formation of biofilms. Biofilm-embedded bacteria require much higher concentrations of antibiotics for elimination than their planktonic forms. Several reasons for that specific behaviour have been proposed. Antimicrobial molecules must diffuse through the biofilm matrix in order to inactivate the encased cells. The extracellular polymeric substances constituting this matrix present a diffusional barrier for these molecules by influencing either the rate of transport of the molecule to the biofilm interior or the reaction of the antimicrobial material inside the matrix material. Conditions that elicit decreased growth, such as nutrient limitation or presence of toxic substances (antibiotics), favour the formation of biofilms.
Debridement may remove the majority of bacteria, but even after a perfect debridement some colonies detached from the biofilm during manipulation may remain, able to colonise niches with poorly vascularised surfaces and cause recurrence after an indefinite period of time. This has been the reason for avoiding simultaneous insertion of osteosynthetic material or endoprostheses at a freshly debrided site and for using external fixators for stabilisation.
Bone defects5
After removal of infected implants and radical sequestrectomy, bony defects will always be present. There are several suggestions as to how to address this issue; what all have in common is the use of multiple procedures requiring multiple stages, leading to prolonged treatment and impairment of the condition of the patients. One of the predisposing factors for continuation of infection is inflammation. There are several reasons for inflammation, such as mechanical factors (instability, foreign bodies), as well as chemical or immunological features. When filling a previously infected site, it therefore seems favourable to avoid any reason for inflammation as much as possible. PMMA (polymethylmethacrylate cement) or bone substitutes are clearly foreign bodies that tend to create an inflammatory response. The Masquelet technique of induced membranes6 uses this inflammatory reaction for inducing a pseudosynovial membrane around PMMA spacers that consequently secrete growth factors apparently enhancing the incorporation of autologous bone grafts, placed at a second stage some weeks later. However, its ability to assist in the healing of critical-sized segmental defects when compared with empty controls remained inconclusive.7 The authors of this study reported a 90% union rate but this requires a mean of 6.11 surgical interventions within a mean of 14.4 months to obtain union.8 Other authors prefer resection of the altered osseous section and the creation of new bone via bone transportation9,10 or a vascularised fibular graft.11 All of these procedures show a high rate of complications, require multiple interventions over several months or even years, and represent a severe pressure on the patient, both physically and psychologically, as is illustrated by the voluntary amputation rate of 1.6%.12
Bone grafting has been used in COM for decades.13 Autologous bone (i.e. bone from the patient) is considered preferable for reconstruction but mostly is not available in sufficient amounts, requires additional surgery and is unprotected against bacterial re-colonisation. Allograft bone is available in unlimited amounts but since it is not vascularised it may be a substrate for bacterial growth. Highly purified bone matrix of the same species seems to show the highest biocompatibility of all available materials; it additionally grants the advantages of some load-bearing capability and the possibility of accelerated incorporation into the host organism through uncompromised osteoconduction.14
Chronic osteomyelitis: classification
There are several systems available for the classification of COM. For clinical practice, the Cierny-Mader classification15 seems to be the most valuable one since it is a clinical classification based on anatomical, clinical and radiological features. It divides osteomyelitis into four anatomical stages.
In stage 1, or the medullary stage, osteomyelitis is confined to the medullary cavity of the bone.
In stage 2, or the superficial stage, osteomyelitis involves only the outside of cortical bone and most often originates from a direct inoculation or a contiguous focus infection.
In stage 3, or the localised stage, osteomyelitis usually involves both cortical and medullary bone. In this stage, the bone remains stable and the infectious process does not involve the entire bone diameter.
In stage 4, or the diffuse stage, osteomyelitis involves the entire thickness of the bone, with loss of stability.
The system adds a second dimension, characterising the host as either A, B or C. While A hosts are patients without any additional risk factors, B hosts are affected by either local or systemic compromise. It is remarkable that Cierny and Mader have introduced the completely subjective term of C hosts, who are patients so severely compromised that the radical treatment necessary would have an unacceptable risk-benefit ratio. It opens an option, or rather obligation, for the surgeon to choose between alternatives in order to provide the best possible quality of life.
Peri-prosthetic joint infection
There are several suggestions for the classification and staging of PJI.16 For practical use, the most important is the time of onset of infection whereas the definition by Zimmerli et al17 is most widely accepted. Early infections develop less than three months after surgery, delayed infections after three to 24 months and late infections after more than 24 months. Both early and delayed infections originate from the previous surgery, late infections are usually of haematogenous origin. While early and late infections may be considered ‘acute’ and may be treated successfully with more conservative approaches,18,19 a delayed infection definitely is chronic and always requires surgical removal of all non-viable material for cure. There is ongoing debate on the timing of re-implantation of a new prosthesis, either in one single stage or in multiple stages.20 Two-stage revision is widely considered the ‘gold standard’ of treatment, although there is no evidence-based reason for that assumption. Meta-analysis of the existing literature could not indicate that one- or two-stage methods have different re-infection outcomes, either for hips21 or for knees.22
Quality of life
COM and delayed PJI are characterised by persistence and difficulty to treat, but they rarely lead to life-threatening situations. As doctors and surgeons, it is our primary task to provide cure of the disease. However, we should not forget that we do not only deal with a disease but also with patients who have a family, work, social contacts and a right of leisure activities. Cierny and Mader were right in saying that ‘some treatments may be worse than the disease’. These observations should guide our strategy when suggesting a treatment. It sometimes may be more advantageous to accept remission instead of cure while providing fast rehabilitation. Multiple-stage procedures, such as wide resections as in oncological surgery, inevitably predict long-standing disability. In PJI, one-stage procedures are favoured regarding the preservation of quality of life23 and post-operative function.24 Finding the balance between advantages and disadvantages is often a difficult task but remains the responsibility of the surgeon, including evaluation of the needs of the patient with fully informed consent.
Antibiotic delivery
The idea of delivering antibiotics by a local drug-delivery system was first followed by Buchholz et al, who mixed antibiotics and PMMA to create a local carrier.25 From these findings, Klemm et al have developed techniques using antibiotic-loaded bone cement in the form of beads to be placed into debrided bone defects.26 However, meanwhile it has become clear that antibiotic concentrations produced by antibiotic-loaded cement may kill planktonic bacteria but are not effective in eliminating remaining biofilm clusters. Between 90% and 95% of the antibiotic remains trapped in the cement and the amounts released from the surface create only moderate concentrations for the first hours after implantation, leaving antibiotic-loaded cement ineffective as anti-biofilm tool. Ninety percent of implanted bead chains and 50% of spacers are covered with biofilms at removal,27,28 often associated with induction of resistance to even the planktonic forms.29,30 Small colony variants (SCVs) require up to 100-fold of the minimal-inhibiting concentrations (MIC), biofilm embedded pathogens up to 1000-fold MIC for elimination31 and these are usually not possible for systemic antibiotic therapy as well as for antibiotics released from PMMA.32
In developing novel systems, the antibiotics must pass several tests qualifying them for that purpose. Few antibiotics have been identified to meet those criteria. Among them, glycopeptides and aminoglycosides are the most widely evaluated ones. The majority of the pathogens involved in bone infection are Gram-positive and susceptible to vancomycin. Most Gram-negatives are susceptible to tobramycin. Vancomycin and tobramycin show the least cytotoxic effect of all commonly used antibiotics33 and are not likely to cause systemic side effects after local application.34 It is therefore suggested that local application of antibiotics with similar properties as vancomycin together with an appropriate carrier may be a valuable tool against orthopaedic infections.
For eliminating residual biofilm fragments, local carriers are necessary to provide sufficiently high local antibiotic concentrations for prolonged periods of time.35,36 For mature biofilms of Staph. aureus, Post et al showed that after 28 days under static conditions, the Staph. aureus biofilm was completely eradicated at 200 mg/L vancomycin and higher concentrations, but not under 100 mg/L.37 Fragments of biofilms are more vulnerable to antibiotics compared with intact biofilm systems,38,39 but their elimination still requires concentrations exceeding the levels provided by systemic or conventional local antibiotic therapy. An ideal carrier should provide for high initial levels to penetrate remaining biofilms rapidly and consequently keep the concentrations above the critical level (which in the case of vancomycin is estimated at between 200 and 500 mg/L) for a minimum of 72 hours.
Bone grafts as antibiotic carriers
When mixing bone grafts with antibiotics, it turned out that their storage capability for antibiotics vastly exceeds those of PMMA40-42 and other carriers. Especially when loading highly purified cancellous bone local concentrations of up to 20 000 mg/L can be released with vancomycin (Table 1) and up to 13 000 mg/L with tobramycin.5 With this kind of impregnation an antibiotic-bone-compound is created with the whole amount of loaded antibiotic being available for antimicrobial activity and the activity remains beyond the susceptibility of relevant pathogens for several weeks (Fig. 1). These capacities make them attractive for reconstruction of contaminated sites and act as a powerful local carrier at the same time.
Table 1. Kinetics of purified bone versus polymethylmethacrylate (PMMA).
| Antibiotic carrier | Purified bone | PMMA |
|---|---|---|
| Storage capacity / 10 cc | 1 g | 0.1 g |
| Availability | > 90% | < 10% |
| Release 1 day | 10.000 - 20.000 mg/l | 40 – 400 mg/l |
| Release 6 day | 60 – 130 mg/l | Trace |
| Release 100 day | 0 | Trace |
Fig. 1.
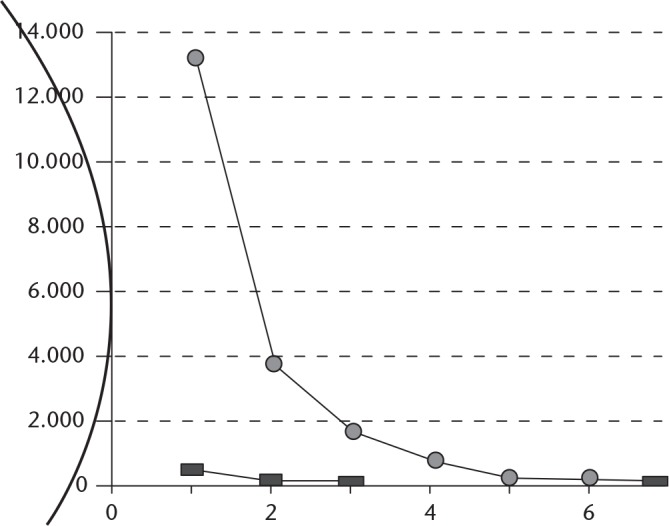
Loading of carriers with antibiotics. Purified bone may store 10x the amount of vancomycin compared with cement. Almost the whole amount is available, leading to markedly elevated local concentrations and a prolonged biofilm-active release.
Effective therapy of biofilm-mediated infection
A chronically infected operative site must be surgically debrided but cannot be sterilised by debridement alone. Debridement will remove the predominant amount of bioburden but even the most careful cleaning cannot provide sterility. It is commonly accepted that whatever filler is used for dead space management (DSM), it needs some kind of protection against re-colonisation with remaining bacteria. DSM after debridement may be performed with antibiotic-loaded cement or ceramics. It should be kept in mind that those devices beside their mechanical function cannot be considered as an anti-biofilm tool; their antibiotic content provides short-lived prophylactic aid against colonisation with planktonic bacteria but is not capable of sterilising sites contaminated with sessile bacteria and provides no protection against biofilm colonisation.43-46 Micro-clusters disrupted from biofilms may be the cause of recurrence after an indefinite period of time. Fragments of biofilms seem to be more vulnerable to antibiotics compared with intact biofilm systems38,39 but their elimination still requires concentrations exceeding the ones provided by systemic or conventional local antibiotic therapy. For eliminating residual biofilm fragments local carriers are advisable, providing sufficiently high local antibiotic concentrations for a prolonged period of time.35,36
Treatment of bone infection is a highly specialised discipline and should be reserved to experienced surgeons in a dedicated centre. In order to eradicate biofilm-mediated infections, five basic requirements should be followed (5D):
Detection: localise their habitats as exactly as possible;
Debridement: drastically reduce their number of bacteria and their means of livelihood by removing all identified dead material as radically as possible;
Disruption: disturb the living community of residual biofilm colonies by mechanically disrupting their established structures as thoroughly as possible;
Dead space management: obliterate possible colonisation foci by filling dead space with inaccessible material as completely as possible;
Decontamination: eliminate sessile bacteria inside remaining fragments using antimicrobial substances in concentrations as high and as consistent as possible.
In addition, reconstruction of bony defects is often necessary to restore the function of the affected limb.
The access to the infected site must follow pre-determined pathways with excision of sinus tracts and/or scars of former surgical procedures. The soft tissues should be carefully examined and debrided immediately as soon as infectious tissue is identified. Implants, cement and sequestra must be removed completely. Tissue specimens from at least four different locations should be sent for culturing. Implants and bone fragments may be examined by sonication. Sclerotic bone need not necessarily be sacrificed as long as it is vascularised. Even poorly vascularised parts may serve an important role for stability. Since biofilms are attached only at the surface cautious abrasion is sufficient for elimination of biofilms. Every debridement must be accompanied by extensive lavage, e.g. by using pulsed saline.
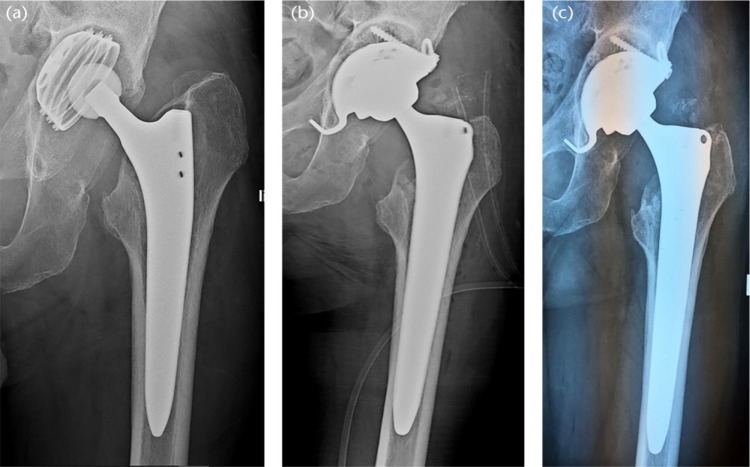
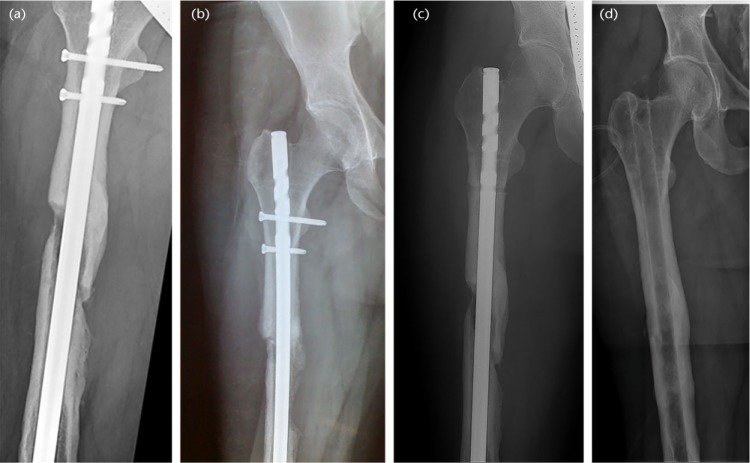
Reconstruction even of small defects seems to be favourable with regard to further revisions. Allograft bone is widely used for reconstruction of bony defects and performs favourably in two-stage revisions of TJR.47 However, only when using antibiotic-impregnated graft may it be performed in a single-stage procedure. In that context, impaction grafting of ABC infections has shown favourable results so far, both in PJI (Fig. 2) and in COM (Fig. 3).1,48 However, multiple-stage revision is considered the ‘gold standard’, but the number of surgeons mainly performing one-stage procedures is increasing constantly.
Fig. 2.
A 66-year-old male who sustained a femoral neck fracture treated with uncemented total hip arthroplasty. Post-operatively he complained of unspecific pain with only slightly elevated infection markers. a) Three years later loosening of the acetabular component was diagnosed with marked osseous defect periacetabular and signs of osteolysis around the proximal part of the stem. b) One stage exchange with uncemented components. The defects were filled with antibiotic impregnated bone Osteomycin V. Sonification of explanted material revealed growth of two strains of Staph. epidermidis (MSSE) and Propionibact. sp. Hospital stay was one week, with Cefuroxim intravenously, followed by six weeks of Amoxicillin/Clavulanic acid and Rifampicin orally. c) six months post-operatively the patient is painfree with no sign of infection and unlimited mobility. There is partial remodelling of the allograft.
Fig. 3.
Radiographs from a 24-year-old male. He was involved in a car accident and had a fractured femur treated with intramedullary nailing. There was post-operative infection. He had three revisions, exchange of nail. fever, ongoing fistulation, cultures revealed Staph. aureus (methicillin sensitive) and Staph. epidermidis (methicillin resistant). a) Post-operative radiograph. An exchange of the intramedullary nail was performed with rigid fixation by locking screws proximally and distally, with defects filled with antibiotic-bone-compound ABC. b) Radiograph at six weeks after surgery. The patient was fully weight-bearing with no sign of infection. c) Radiograph at one year after surgery. Dynamisation was performed by removing the proximal interlocking screws; the patient is fully weight bearing with no signs of infection. d) Radiograph at seven years after surgery. Hardware has been removed. There is complete union and the defects are restored. The patient returned to sports with no signs of infection.
To address the problem of potentially undetected polymicrobial colonisation, it appears best to reserve application of a single local antibiotic to cases with strong evidence of monomicrobial Gram-positive infection, i.e. acute onset of symptoms with typical clinical appearance (fever, pus) and unambiguous culture. Cases with prior infection-related surgery or non-specific cultures should be considered polymicrobial. They should be treated with a combination of two or more antibiotics, such as local combinations of vancomycin with tobramycin which seem to be favourable by taking advantage of the synergistic activity of the two antibiotics.49,50 This combined approach should cover most of the relevant pathogens. Complete soft tissue coverage is essential for success, using muscular or fasciocutanous flaps if necessary.
Systemic antibiotic treatment must always follow the results of pre-operative cultures. In case of culture-negative infection, a second generation cephalosporin appears advisable until the results of intra-operative cultures become available. Suggestions on duration of concomitant systemic antibiosis vary widely, from days to several months. All recommendations are empirical and it is questionable whether long-term therapy after surgical intervention provides any additional benefit. Planktonic bacteria may be eliminated rather quickly; however, biofilm remnants are vulnerable only a short period of time after disruption. Either they are eliminated during and shortly after surgical intervention or they are not. If they cannot be eradicated during the ‘window of opportunity’ they are fully re-organised after three weeks at the latest and are again inaccessible for systemically administered antibiotics. Futhermore, it is a concern that prolonged antibiotic therapy may carry the risk of undesired side effects and induction of resistance, even of planktonic bacteria. Hence, long-term antimicrobial treatment may be considered in a new light, where possible advantages and disadvantages need to be weighed against each other.
Osteomyelitic lesions and infected implants may be successfully treated using thorough debridement in conjunction with local antimicrobial therapy using antibiotic carriers. As long as the local antibiotic levels are higher than the dosage required for eliminating biofilm-embedded bacteria, the risk of contamination of alloplastic material is low. Internal fixation and re-implantation of endoprostheses may be performed simultaneously as under non-septic condition. Using antibiotic carriers such as impregnated bone grafts treatment of infection, reconstruction and internal stabilisation may be performed within a single operation. Re-infection may occur in complex cases where secluded infected foci are not detected during debridement. An exact pre-operative mapping of infected areas is therefore mandatory as well as consequent post-operative follow-up. Re-revisions are markedly less demanding when missed foci are detected early, as in oncological surgery. Care should be taken to achieve good soft tissue coverage, using muscle flaps in doubtful situations. For single-stage procedures, the choice of simultaneously implanted material should be considered carefully.
We can never have certainty of having cured bone infection. Assuming that recurrence may occur within an unknown period of time, it should be the responsibility of the surgeon to provide for a treatment reducing the complications for the patient to an absolute minimum. In this sense, it should be agreed that treatments should be kept as short and as pain-free as possible. Adequate single-stage protocols with simultaneous reconstruction of defects may serve as a favourable tool in reaching that goal in future.
Footnotes
ICMJE Conflict of Interest Statement: HW reports financial support outside the current work in the form of consultancy fees from LIMA sppa and Gerson Lehman.
Funding
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Winkler H, Haiden P. Treatment of chronic bone infection. Oper Tech Orthop 2016;26:2-11. [Google Scholar]
- 2. Gristina AG, Oga M, Webb LX, Hobgood CD. Adherent bacterial colonization in the pathogenesis of osteomyelitis. Science 1985;228:990-993. [DOI] [PubMed] [Google Scholar]
- 3. Gristina AG, Costerton JW. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J Bone Joint Surg [Am] 1985;67-A:264-273. [PubMed] [Google Scholar]
- 4. Costerton JW. Biofilm theory can guide the treatment of device-related orthopaedic infections. Clin Orthop Relat Res 2005;437:7-11. [DOI] [PubMed] [Google Scholar]
- 5. Winkler H, Janata O, Berger C, Wein W, Georgopoulos A. In vitro release of vancomycin and tobramycin from impregnated human and bovine bone grafts. J Antimicrob Chemother 2000;46:423-428. [DOI] [PubMed] [Google Scholar]
- 6. Masquelet AC, Fitoussi F, Begue T, Muller GP. [Reconstruction of the long bones by the induced membrane and spongy autograft]. Ann Chir Plast Esthet 2000;45:346-353. (In French) [PubMed] [Google Scholar]
- 7. Christou C, Oliver RA, Yu Y, Walsh WR. The Masquelet technique for membrane induction and the healing of ovine critical sized segmental defects. PLoS One 2014;9:e114122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Karger C, Kishi T, Schneider L, Fitoussi F, Masquelet AC; French Society of Orthopaedic Surgery and Traumatology (SoFCOT). Treatment of posttraumatic bone defects by the induced membrane technique. Orthop Traumatol Surg Res 2012;98:97-102. [DOI] [PubMed] [Google Scholar]
- 9. Ilizarov GA, Lediaev VI. [Replacement of defects of long tubular bones by means of one of their fragments]. Vestn Khir Im I I Grek 1969;102:77-84. (In Russian) [PubMed] [Google Scholar]
- 10. Arora S, Batra S, Gupta V, Goyal A. Distraction osteogenesis using a monolateral external fixator for infected non-union of the femur with bone loss. J Orthop Surg (Hong Kong) 2012;20:185-190. [DOI] [PubMed] [Google Scholar]
- 11. Low CK, Pho RW, Kour AK, Satku K, Kumar VP. Infection of vascularized fibular grafts. Clin Orthop Relat Res 1996;323:163-172. [DOI] [PubMed] [Google Scholar]
- 12. Papakostidis C, Bhandari M, Giannoudis PV. Distraction osteogenesis in the treatment of long bone defects of the lower limbs: effectiveness, complications and clinical results; a systematic review and meta-analysis. Bone Joint J 2013;95-B:1673-1680. [DOI] [PubMed] [Google Scholar]
- 13. Hazlett JW. The use of cancellous bone grafts in the treatment of subacute and chronic osteomyelitis. J Bone Joint Surg [Br] 1954;36-B:584-590. [DOI] [PubMed] [Google Scholar]
- 14. Thorén K, Aspenberg P. Increased bone ingrowth distance into lipid-extracted bank bone at 6 weeks. A titanium chamber study in allogeneic and syngeneic rats. Arch Orthop Trauma Surg 1995;114:167-171. [DOI] [PubMed] [Google Scholar]
- 15. Cierny G, III, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res 2003;414:7-24. [DOI] [PubMed] [Google Scholar]
- 16. McPherson EJ, Tontz W, Jr, Patzakis M, et al. Outcome of infected total knee utilizing a staging system for prosthetic joint infection. Am J Orthop (Belle Mead NJ) 1999;28:161-165. [PubMed] [Google Scholar]
- 17. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med 2004;351:1645-1654. [DOI] [PubMed] [Google Scholar]
- 18. Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE. Role of rifampin for treatment of orthopedic implant-related staphylococcal infections: a randomized controlled trial. Foreign-Body Infection (FBI) Study Group. JAMA 1998;279:1537-1541. [DOI] [PubMed] [Google Scholar]
- 19. Koyonos L, Zmistowski B, Della Valle CJ, Parvizi J. Infection control rate of irrigation and débridement for periprosthetic joint infection. Clin Orthop Relat Res 2011;469:3043-3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lichstein P, Gehrke T, Lombardi A, et al. One-stage vs two-stage exchange. J Arthroplasty 2014;29:108-111. [DOI] [PubMed] [Google Scholar]
- 21. Beswick AD, Elvers KT, Smith AJ, et al. What is the evidence base to guide surgical treatment of infected hip prostheses? Systematic review of longitudinal studies in unselected patients. BMC Med 2012;10:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kunutsor SK, Whitehouse MR, Lenguerrand E, Blom AW, Beswick AD; INFORM Team. Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS One 2016;11:e0151537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wolf CF, Gu NY, Doctor JN, Manner PA, Leopold SS. Comparison of one and two-stage revision of total hip arthroplasty complicated by infection: a Markov expected-utility decision analysis. J Bone Joint Surg [Am] 2011;93-A:631-639. [DOI] [PubMed] [Google Scholar]
- 24. De Man FH, Sendi P, Zimmerli W, et al. Infectiological, functional, and radiographic outcome after revision for prosthetic hip infection according to a strict algorithm. Acta Orthop 2011;82:27-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Buchholz HW, Engelbrecht H. [Depot effects of various antibiotics mixed with Palacos resins]. Chirurg 1970;41:511-515. (In German) [PubMed] [Google Scholar]
- 26. Klemm K. [Gentamicin-PMMA-beads in treating bone and soft tissue infections (author’s transl)]. Zentralbl Chir 1979;104:934-942. (In German) [PubMed] [Google Scholar]
- 27. Neut D, van de Belt H, Stokroos I, et al. Biomaterial-associated infection of gentamicin-loaded PMMA beads in orthopaedic revision surgery. J Antimicrob Chemother 2001;47:885-891. [DOI] [PubMed] [Google Scholar]
- 28. Nelson CL, Jones RB, Wingert NC, Foltzer M, Bowen TR. Sonication of antibiotic spacers predicts failure during two-stage revision for prosthetic knee and hip infections. Clin Orthop Relat Res 2014;472:2208-2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tunney MM, Ramage G, Patrick S, et al. Antimicrobial susceptibility of bacteria isolated from orthopedic implants following revision hip surgery. Antimicrob Agents Chemother 1998;42:3002-3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chang CC, Merritt K. Microbial adherence on poly(methyl methacrylate) (PMMA) surfaces. J Biomed Mater Res 1992;26:197-207. [DOI] [PubMed] [Google Scholar]
- 31. Saginur R, Stdenis M, Ferris W, et al. Multiple combination bactericidal testing of staphylococcal biofilms from implant-associated infections. Antimicrob Agents Chemother 2006;50:55-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van de Belt H, Neut D, Schenk W, et al. Infection of orthopedic implants and the use of antibiotic-loaded bone cements. A review. Acta Orthop Scand 2001;72:557-571. [DOI] [PubMed] [Google Scholar]
- 33. Edin ML, Miclau T, Lester GE, Lindsey RW, Dahners LE. Effect of cefazolin and vancomycin on osteoblasts in vitro. Clin Orthop Relat Res 1996;333:245-251. [PubMed] [Google Scholar]
- 34. Buttaro MA, Gimenez MI, Greco G, Barcan L, Piccaluga F. High active local levels of vancomycin without nephrotoxicity released from impacted bone allografts in 20 revision hip arthroplasties. Acta Orthop 2005;76:336-340. [PubMed] [Google Scholar]
- 35. Ehrlich GD, DeMeo PJ, Costerton JW, Winkler H, eds. Culture negative orthopedic biofilm infections. Heidelberg, New York: Springer, 2012. [Google Scholar]
- 36. Smith AW. Biofilms and antibiotic therapy: is there a role for combating bacterial resistance by the use of novel drug delivery systems? Adv Drug Deliv Rev 2005;57:1539-1550. [DOI] [PubMed] [Google Scholar]
- 37. Post V, Wahl P, Richards RG, Moriarty TF. Vancomycin displays time dependent eradication of mature Staphylococcus aureus biofilms. J Orthop Res 2017;35:381-388 [DOI] [PubMed] [Google Scholar]
- 38. El-Azizi M, Rao S, Kanchanapoom T, Khardori N. In vitro activity of vancomycin, quinupristin/dalfopristin, and linezolid against intact and disrupted biofilms of staphylococci. Ann Clin Microbiol Antimicrob 2005;4:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fux CA, Wilson S, Stoodley P. Detachment characteristics and oxacillin resistance of Staphyloccocus aureus biofilm emboli in an in vitro catheter infection model. J Bacteriol 2004;186:4486-4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Witsø E, Persen L, Løseth K, Benum P, Bergh K. Cancellous bone as an antibiotic carrier. Acta Orthop Scand 2000;71:80-84. [DOI] [PubMed] [Google Scholar]
- 41. Witsø E, Persen L, Løseth K, Bergh K. Adsorption and release of antibiotics from morselized cancellous bone. In vitro studies of 8 antibiotics. Acta Orthop Scand 1999;70:298-304. [DOI] [PubMed] [Google Scholar]
- 42. Buttaro MA, Pusso R, Piccaluga F. Vancomycin-supplemented impacted bone allografts in infected hip arthroplasty. Two-stage revision results. J Bone Joint Surg [Br] 2005;87:314-319. [DOI] [PubMed] [Google Scholar]
- 43. Greene N, Holtom PD, Warren CA, et al. In vitro elution of tobramycin and vancomycin polymethylmethacrylate beads and spacers from Simplex and Palacos. Am J Orthop (Belle Mead NJ) 1998;27:201-205. [PubMed] [Google Scholar]
- 44. Masri BA, Duncan CP, Beauchamp CP. Long-term elution of antibiotics from bone-cement: an in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J Arthroplasty 1998;13:331-338. [DOI] [PubMed] [Google Scholar]
- 45. Bertazzoni Minelli E, Benini A, Magnan B, Bartolozzi P. Release of gentamicin and vancomycin from temporary human hip spacers in two-stage revision of infected arthroplasty. J Antimicrob Chemother 2004;53:329-334. [DOI] [PubMed] [Google Scholar]
- 46. Walenkamp GH. Gentamicin PMMA beads and other local antibiotic carriers in two-stage revision of total knee infection: a review. J Chemother 2001;13:66-72. [DOI] [PubMed] [Google Scholar]
- 47. Ammon P, Stockley I. Allograft bone in two-stage revision of the hip for infection. Is it safe? J Bone Joint Surg [Br] 2004;86-B:962-965. [DOI] [PubMed] [Google Scholar]
- 48. Winkler H. Rationale for one stage exchange of infected hip replacement using uncemented implants and antibiotic impregnated bone graft. Int J Med Sci 2009;6:247-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Watanakunakorn C, Tisone JC. Synergism between vancomycin and gentamicin or tobramycin for methicillin-susceptible and methicillin-resistant Staphylococcus aureus strains. Antimicrob Agents Chemother 1982;22:903-905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. González Della Valle A, Bostrom M, Brause B, Harney C, Salvati EA. Effective bactericidal activity of tobramycin and vancomycin eluted from acrylic bone cement. Acta Orthop Scand 2001;72:237-240. [DOI] [PubMed] [Google Scholar]