Abstract
Most of tumours of the foot are tumour-like (synovial cyst, foreign body reactions and epidermal inclusion cyst) or benign conditions (tenosynovial giant cells tumours, planta fibromatosis). Malignant tumours of the soft-tissue and skeleton are very rare in the foot and their diagnosis is often delayed with referral to specialised teams after initial inappropriate procedures or unplanned excisions. The adverse effect of these misdiagnosed tumours is the increasing rate of amputation or local recurrences in the involved patients. In every lump, imaging should be discussed before any local treatment. Every lesion which is not an obvious synovial cyst or plantar fibromatosis should have a biopsy performed.
After the age of 40 years, chondrosarcoma is the most usual malignant tumour of the foot. In young patients bone tumours such as osteosarcoma or Ewing’s sarcoma, are very unusually located in the foot. Synovial sarcoma is the most frequent histological diagnosis in soft tissues. Epithelioid sarcoma or clear cell sarcoma, involve more frequently the foot and ankle than other sites. The classic local treatment of malignant conditions of the foot and ankle was below-knee amputation at different levels. Nowadays, with the development of adjuvant therapies, some patients may benefit from conservative surgery or partial amputation after multidisciplinary team discussions.
The prognosis of foot malignancy is not different from that at other locations, except perhaps in chondrosarcoma, which seems to be less aggressive in the foot. The anatomy of the foot is very complex with many bony and soft tissue structures in a relatively small space making large resections and conservative treatments difficult to achieve.
Cite this article: EFORT Open Rev 2017;2. DOI: 10.1302/2058-5241.2.160078. Originally published online at www.efortopenreviews.org
Keywords: foot and ankle, malignant tumours, diagnosis, biopsy, imaging, treatment modalities
Introduction
Benign tumours and tumour-like lesion of the foot and ankle are not uncommon but malignant tumours and especially malignant bone tumours of the foot are rare.
Most of the foot tumours are benign: usually synovial cysts (30% of all foot tumours)1,2 and lipomata arise onthe dorsum of the foot.3 Villonodular synovitis (or tenosynovial giant cell tumours) are more frequent and deep-seated lesions and plantar fibromatosis or epidermal inclusion cysts and foreign body reaction are encountered in the sole. Rheumatoid nodules and gouty tophi should not be mistaken for a tumour.
We have excluded Darier-Ferrand’s dermatofibrosarcoma and melanoma which have different presentations and are usually treated and followed up in dermatology departments.
Diagnosis of bone and soft-tissue foot tumours is often delayed and many malignant conditions are referred to specialised sarcoma teams after an initial inappropriate procedure.4-6 The adverse effect of these misdiagnosed tumours is the increasing rate of amputation or local recurrences in the involved patients. After the age of 40 years, chondrosarcoma is the most usual malignant tumour of the foot. In bone tumours such as osteosarcoma or Ewing’s sarcoma, the foot and ankle are very unusual sites. In soft-tissue tumours, such as epithelioid sarcoma (ES) or clear cell (CC) sarcoma, the foot and ankle are relatively more frequently involved than other sites. Synovial sarcoma (SS) is the most frequent histological diagnosis. The classic local treatment of malignant conditions of the foot and ankle was below-knee amputation at different levels. Nowadays, with the development of adjuvant therapies, some patients may benefit from conservative surgery or partial amputation after multidisciplinary team discussions.7-9 The prognosis of foot malignancy is not different from that at other location, except perhaps in chondrosarcoma, which seems to be less aggressive in the foot.10
The anatomy of the foot is very complex with many bony and soft tissue structures in a relatively small space. The foot can be divided into the plantar and the dorsal compartments. The plantar compartment is divided into three parts, separated by thin aponeuroses, crossed by tendons and vascular bundles making the extensive spread of tumours easier and therefore large resections difficult to achieve.11
Epidemiology
It is difficult to draw definitive statistics about prevalence of malignant tumours and different histological sub-types of foot tumours because the reported series give very different results. The foot and ankle have less than 5% of all soft-tissue sarcomas which represent less than 25% of all foot tumours.1,2,12-14
Malignant bone tumours represent less than 25% of all bone tumours, and all types of bone tumours of the foot together are less than 6% of all bone tumours.10,12-14
Malignant conditions are relatively more frequent in children or adolescents, and in the heel.
Sarcomata are very rare in middle age and occur more in children or adolescents and after the age of 60 years. There is no significant gender predominance.
Clinical symptoms are often confusing in foot tumours.
The patients often present with a so-called ‘footwear problem’. Children are sometimes referred for limping without evidence of a hip or knee problem. Some malignant bone tumours can also mimic an infection, such as Ewing’s sarcoma, with fever, and inflammatory reaction on blood samples. A pre-existing history of trauma can be found in 20% of the cases.
Pain seems more frequent in malignant conditions but is not constant. Swelling usually appears at a late stage.1,2,15
In our experience and in the literature, tumours of the foot and ankle are often diagnosed with a delay of several weeks up to two years. In bone tumours, the reported delay in diagnosis showed no influence on the incidence of metastasis at diagnosis or on overall survival at five years. Many soft-tissue and malignant bone tumours, approximately 40% to 60%, are referred after an inadequate excision. In these lesions, an inadequate previous procedure is reported to have an adverse effect on prognosis.4-6,10,16,17
Imaging
Often patients have had no imaging (excepted echography) before the first surgery. It is then often difficult to plan an adequate secondary excision.
Echography may show typical patterns in ganglion cyst or benign lipoma.11,15 It can show the size, situation and vascularity of soft-tissue tumours, but in all suspected tumours (benign or not) it is mandatory to perform at least an MRI before any surgery.18 In soft-tissue tumours, echography of the whole limb will assess lymphatic node extension of the disease.
In case of a bone lesion, a plain radiograph can eliminate a stress fracture (but some stress fractures are not visible on conventional radiograph). It can also show soft-tissue calcification in soft-tissue tumours. In bone tumours, bone formation or osteolysis are seen but not quantitated.11,15
Technecium bone scans and positron-emitting tomography (PET) are useful tools to localise the site of a lesion causing unexplained limping. This will not define whether the lesion is malignant or not. It is also mandatory in assessing extent of the disease. PET can also help in determining the primary tumour in metastatic disease.
MRI is mandatory in all tumours before any surgery or biopsy. It should comprise at least T1, T2 and T1 fat-sat injection sequences. Images in the three planes, coronal, sagittal and axial, are necessary. In bone tumours of the distal tibia (and perhaps of the foot) an MRI of the whole tibia will assess the presence of potential skip metastases. In soft-tissue lesions, such as ganglion cyst, lipoma, haemangioma, bursitis and muscle tears, MRI can determine whether the lesion is typical enough to allow surgical treatment without biopsy.15,17,18
CT is a useful tool in differential diagnosis for diagnosing fatigue fractures, osteoarthritis or benign lesions such as osteoid osteoma. In soft-tissue tumours, it can help to assess secondary bone involvement in aggressive lesions.15
Diagnosis: the biopsy
When?
A biopsy is always necessary in the diagnosis of malignant foot and ankle bone tumours. The biopsy is performed after completing imaging (to avoid artifacts due to post-operative haematoma or swelling). The biopsy should be performed in a referral centre, either by the surgeon who will be in charge of the further local treatment or by a radiologist of the team. Small (less than 1.5 cm is considered as small in foot and hand, 5 cm in tumours from other locations) and superficial tumours can be resected without biopsy provided a complete resection can be performed. Deep-seated tumours and tumours in which a complete resection is not feasible at the first attempt should always have a biopsy.7,8 It is not necessary to biopsy obvious ganglion cysts, lipomata or reactive lesions when they can be resected.18
How?
Core biopsy is now universally recommended in soft-tissue lesions.7,11
Core or surgical biopsy is preferred in bone tumours, depending on the expertise of the pathologist and the suspected diagnosis. In France, many bone pathologists prefer open biopsies. In cases of suspected Ewing’s tumour, a needle biopsy can allow a very quick and safe diagnosis.
The biopsy should be oriented according to the imaging, in a viable part of the tumour avoiding necrotic areas and non-homogenous lesions. Some infections may mimic a bone tumour and bacteriology is needed to make the differential diagnosis.
The surgical or core biopsy approach should allow further complete resection of a potentially malignant tumour and avoid local tumour spread, and should be discussed with the surgeon and the radiologist in a multidisciplinary team meeting.
Malignant bone tumours
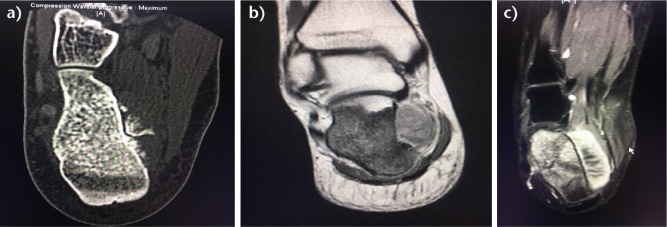
Chondrosarcoma is (with Ewing tumour) one of the most common malignant bone tumours of the ankle and foot, but less than 5% of chondrosarcomas occur in this site. The calcaneus is the most common location. Plain radiographs and CT scans show an osteolytic lesion with a calcified matrix (Fig 1). Low-grade tumours are usually more calcified than high-grade ones. Endosteal scalloping of the cortex and cortical destruction with a soft tissue mass are characteristic of a malignant lesion. There is rarely a sclerotic rim and periosteal reaction is rare. On MRI scanning, the soft-tissue extension, hyper-intense in T2, appears more lobulated and thicker than in benign enchondromata. Scalloping is usually not visible in small bones of the foot.15,19,20 Osteochondroma of the small bones of the foot and hand have distinct pathological features that should not lead to over-diagnosing a chondrosarcoma. Chondrosarcoma is characterised by permeation through the cortex and soft tissue (Fig. 2) 21 and seems to have a better prognosis according to grade than at other locations.14
Fig. 1.

Chondrosarcoma of the calcaneus in a 52-year-old male. Plain radiograph showing osteolysis and calcification with soft tissue extension of the tumour.
Fig. 2.
This 55-year-old male had resection of a large tumour of the dorsum of the foot without biopsy. The histological diagnosis was grade 2 chondrosarcoma. a) CT scan of the left foot before first surgery. b) MRI at time of local recurrence. c) Decision is made to perform a Pirogoff/Boyd amputation: drawing of the incision. d) Final appearance of the Pirogoff/boyd stump. e) CT scan showing arthrodesis of the calcaneus to the tibia after the amputation and resection of the talus.
Osteosarcoma is a malignant tumour forming neoplastic bone matrix which rarely occurs in the foot (1% of all osteosarcoma) and is only slightly less uncommon at the distal tibia or fibula (2.5%). It arises usually in adolescents and in the elderly (then on pre-existing lesions or pathology). Osteosarcoma appears as an aggressive bone lesion with area of increased bone density and osteolysis, cortical destruction and periosteal reaction. In MRI, there is replacement of the normal bone marrow signal, peri-tumoural oedema and soft-tissue involvement. On MRI, the ossified matrix will be seen as a low signal on all pulse sequences while the soft-tissue tumour can be heterogeneous with varying signal intensity and enhancement depending on the degree of haemorrhage and necrosis (Fig.3).11,15
Fig. 3.
Osteosarcoma of the calcaneus in a 17-year-old female. a) CT scan showed increased bone density of the calcaneus and a soft tissue extension with periostal reaction. b) MRI showing a low signal in bone and soft tissue extension on T1 coronal view. c) intense tumour enhancement on T2 fat sat injected sequences.
Ewing’s sarcoma is a small round-cell tumour of bone and soft tissue with neuro-ectodermal differentiation that can involve any part of the skeleton. It is the second most common malignant bone tumour in children and 80% of patients are aged less than 20 years. It is characterised by a recurrent chromosomal translocation t11,22 detectable in approximately 85% of cases.22 It occurs rarely in the foot, but is the most common malignancy of feet bones in children.12 However, it is very unusual in the small bones of the feet. The talus, calcaneus and the metatarsals are most commonly involved.
On plain radiograph, Ewing’s sarcoma is often characteristised by a ‘permeated’ or ‘moth-eaten’ pattern of bone destruction (Fig. 4). The classical periosteal reaction ‘onion skin-shaped’ is more often seen in diaphyseal tumours. A very large tissue mass is quite characteristic in Ewing’s sarcoma but is rarely seen in the foot. In the foot, the bone destruction is often more marked than the periosteal reaction, and can be appreciated on CT. MRI helps more than CT in biopsy to determine the intra-osseous and extra-osseous extent of the tumour.15
Fig. 4.
This ten-year-old female had a Ewing’s sarcoma of the second metatarsal. She received six VIDE courses of induction chemotherapy. a) MRI of the left foot before local treatment. b) Post-operative appearance of the foot after second and third metatarsal resection. c) Post-operative radiograph after iliac crest bone grafting to fill the gap between the remaining metatarsals. d) Appearance of the foot 11 years after surgery and post-operative radiotherapy. e, f) Radiographs of the foot at last follow-up.
Soft-tissue malignant tumours
SS is a mesenchymal spindle-cell tumour which displays variable epithelial differentiation, including glandular formation and has a specific chromosomal translocation t(X;18) (p11;q11). It may occur at any site. It does not arise from the synovium, but occurs within deep tissues adjacent to joints or tendon sheaths (not intra-articular). SS most commonly occurs in the lower extremities of young adults (aged 15 to 40 years). It represents 5% to 10% of all soft-tissue tumours in the foot and ankle and is the most common sarcoma in the foot (approximately 45% to 55%).12,13 Growth is relatively slow and indolent, and patients may present with a painless swelling which is often misdiagnosed as a cyst or plantar fibromatosis. Contrary to rapidly growing tumours, lesions noticed for a long period before presentation are locally invasive and may involve bone but tend to have a better outcome, presumably because of they are less aggressive. A radiograph may show dystrophic calcification, typically in adolescent and young adults in biphasic SS type. Ultrasound imaging is of limited value but will reveal the solid nature of the tumour. On MRI the classical appearance of small SS is homogenously hypo-intense in T1, and a round circumscribed mass in T2. Larger tumours may demonstrate the classic ‘triple sign’ (low, intermediate and high signal intensity on long TR pulse sequences due to the presence of fibrous tissues, calcium, haemorrhage and necrosis).11,15
ES occurs in adolescents and young adults (aged 10 to 40 years), with a male gender predominance. It is less infrequent in the distal extremities of upper and lower limbs. When superficially located, ES usually presents as firm, slowly growing painless nodules or plaque-like lesions. Ulceration of the skin may occur. Deep-seated lesions tend to spread along the fascia and nerve or tendon sheaths. There is a high rate (37% to 70%) of local recurrence depending on the adequacy of initial excision. Metastases occur in 40% of patients, and the five- to ten-year survival rate is 50% to 80%.23
On MRI the mass shows poorly-defined margins, often subcutaneous and infiltrating longitudinally along tissue planes. It is moderately bright on PD and T2 and enhances with contrast.15
CC sarcoma of soft tissues is a tumour of young adults (aged 10 to 50 years) with a peak incidence in the third and fourth decades. More than 90% occur in the extremities and 40% in the foot and ankle. Presentation is of a slowly growing mass, usually small, with pain and tenderness in up to 50% of the cases. CC sarcoma is usually deep-seated and often attached to aponeuroses and tendons. The tumour may extend into the subcutaneous or lower dermis, but the epidermis is typically intact. On an MRI, they may be well-defined when small with a benign-looking appearance with a slightly increased intensity on T1-weighted images compared with muscle in about half the cases. CC sarcomata become less distinct as they enlarge along other soft tissue structures. On T1, they have low signal but are slightly brighter than muscle. On T2, they are bright and enhance with contrast. Prognosis is poor, local recurrence and metastases are common, sometimes ten years after diagnosis, and the mortality rate is 37% to 59%.15
Other types of sarcoma can occur in the foot or ankle including pleiomorphic sarcoma (formerly malignant fibrous histiocytoma), fibrosarcoma (low grade fibromyxoid sarcoma, sclerosing epithelioid FS, myxo FS) and leiomyosarcoma, Liposarcoma are rare. In children, congenital fibrosarcoma can be seen in the new-born and has a very good prognosis, even in cases of incomplete surgery. Rhabdomyosarcoma occurs in paediatric patients aged 0 to 20 years. The ten-year overall survival is 62%. The alveolar sub-group seems to have a worse prognosis. Hand and foot lesions have a less favourable outcome.24
Differential diagnosis
Metastases
Metastatic lesions are uncommon in the foot and ankle. When they occur, it is usually in association with generalised metastatic disease, but they can reveal an unknown primary cancer. The most commonly reported primary sites are the colon, kidney, lung, bladder and breast.11,25
Non-neoplastic lesions
Plantar fibromatosis is a benign fibroblastic proliferation arising in the plantar fascia of children or adolescents, usually in the mid to distal aponeurosis. It presents as a firm subcutaneous nodule or thickening, adherent to skin and often mildly painful. Echography shows a hypo-echogenic fusiform mass along the aponeurosis. It can be quite hypervascular in colour Doppler. MRI usually shows low signal on T1and T2, but some cases show T2 signal brightness and strong contrast enhancement but with no involvement of the deeper tissue planes.
Pigmentar villonodular synovitis or giant cell tumour of the tendon sheath can occur in adolescents to middle-aged adults and can mimic a SS. The lesion has a characteristic MRI aspect in spin echo due to haemosiderin deposition.11,15
Fibroma of tendon sheath is a small fibrous nodule arising near tendinous structures, more commonly in the hands than in the feet and rarely in the toes.15
Reactive pseudotumors, such as florid reactive periostitis (parosteal fasciitis), bizarre parosteal osteochondromatous proliferation, subungual exostosis and turret exostosis, leave the bone cortex intact (this is different from osteochondroma).
Morton’s neuroma (interdigital neuroma) is a reactive process due to repetitive trauma and compression of the interdigital nerve and surrounding soft tissues between the metatarsal heads. It is most common in the third web space (and, to a lesser extent, the second).
Bursitis can develop after repeated trauma, rheumatoid arthritis or overuse. In the foot, common locations are the intermetatarsal, over the medial surface of a hallux valgus or in the plantar fat pad below the first or fifth metatarsal head.
Ganglions are cystic lesions usually located adjacent to and sometimes communicating with a joint or tendon sheath. The images are usually characteristic on ultrasound and MRI (which should be done before surgery to eliminate an aggressive lesion).
Prognosis
It had for a long time been supposed that the malignant bone tumours of the foot have a different behaviour from those at other sites. There is an increased delay in diagnosis and tumours tend to be smaller but there is no proven influence on death rate and metastases. Rhabdomyosarcoma seems to have a worse prognosis in the foot and hand. Chondrosarcoma of the foot, and especially the forefoot, tends to be less aggressive than elsewhere.10,14,24 Local recurrence has an adverse effect on survival, mainly in high-grade bone tumours26 but also in soft-tissue sarcomata.10,27 Usually, local recurrence in bone and soft-tissue sarcomata occurs within the first two years after treatment.27 Local recurrence is more frequent after an initially inadequate local treatment.10,16,17
Treatment
The modalities of treatment of foot malignant conditions are not different from those in other locations. According to the histological diagnosis and local and distant extension of the disease, the different treatment options should be discussed in an multidisciplinary team meeting, in a specialised sarcoma centre.7,8,28
In bone sarcoma, like osteosarcoma and Ewing’s sarcoma, chemotherapy has dramatically improved the prognosis and seems absolutely mandatory, according different protocols. New therapies, including immunotherapy, Zolendronate and targeted therapies, are being evaluated.8,28,29 In conventional chondrosarcoma, adjuvant treatments have not proven their efficiency yet and the treatment is mainly surgical. New protocols are in progress to try to improve the prognosis of de-differentiated, mesenchymal and high-grade chondrosarcomata.29
In localised soft-tissue sarcomata, the role of conventional chemotherapy remains debatable. Some specific histological sub-types of soft tissue sarcoma could benefit from new therapies. Patients with metastatic disease should generally receive adjuvant systemic treatments.7
The purpose of this paper is not to analyse the different chemotherapies in bone and soft-tissue sarcomata.
Radiotherapy
Radiotherapy is proven to be effective in local treatment of Ewing’s sarcoma26,28 and improves local control in soft-tissue tumours.7,30 In foot tumours, the late sequelae of radiotherapy (problems with soft-tissue sclerosis and footwear) has decreased. Modern modalities of radiotherapy with improved techniques and the results of the ‘Euro-Ewing’ protocol tend to increase the indications for external radiation therapy in Ewing’s sarcoma.26 The indication for brachytherapy in soft-tissue sarcoma of the foot seems anecdotal because of the distance between the skin and the skeleton.
Surgery
Surgery, whatever the modality, remains the ‘gold standard’ in local treatment of sarcomata. The recommended surgery for soft-tissue and bone sarcomata is wide resection, intending to provide margins free of tumour, with at least a layer of normal cells between the surgical cut and the tumour itself. The recommended thickness of that layer is widely debated . Surgery should be discussed in a multidisciplinary team meeting with at least two surgeons and a specialised radiologist in order to plan a complete resection and a reconstruction aiming to achieve a sufficient functional result.7,8 When a complete resection with a risk of local recurrence or when the intended sequelae of surgery would be unacceptable, amputation should be advised. The foot is a complex anatomical entity with many different tissues, joints, vascular, neurological and tendinous structures. The skin is thin and poorly vascularised in some places (especially the medial aspect of the ankle). Challenging problems of bone and soft-tissue reconstruction should not interfere with planning of a wide resection.31-33 The surgeon should remember that the primary goal of the surgery is the oncological result.31 After surgery the resected tumour should be carefully assessed by histopathologic examination. The initial diagnosis should be confirmed. Margins of resection should be measured in millimetres and their relationship to fascia, if present, indicated. In cases of neo-adjuvant chemotherapy, assessment of the response to treatment should also be assessed.7,8,33
Below-knee amputation has been the recommended local treatment for foot malignancy for many years. It is known to allow excellent functional outcome and even participation in high-level sports activities. Recent publications have shown at least equivalent or better functional results with conservative treatments. Gribb et al advocated the benefit of a ‘time-consuming surgical reconstruction and adjuvant therapy’ in soft-tissue sarcomata of the foot thanks to the development of plastic surgical procedures. For them (and us), good functional and oncological results have been achieved with conservative treatment in malignant tumours of the foot.9,31,34,35
The optimistic belief that the patient would always be happy with an amputation because of their very good functional results should be balanced with the possible residual pain that will impair their quality of live. Older patients tend to have less acceptable function after an amputation than youngsters.34-36
When a previous incomplete surgery has been performed with contaminated margins, revision surgery should be advised. If possible, a second conservative procedure should be considered, but always tends to be more extensive than the primary resection because of the need to resect potential areas of contamination (Fig. 2). It can result in the need for more reconstructive procedures (flaps and skin grafts) and wider adjuvant radiation fields. Histological examination of the re-excision of an unplanned excision field found approximately 50% of cases with a residual tumour cells. These unplanned surgeries tend to generate more local recurrences and secondary amputations than adequate procedures performed in sarcoma centres.4,16,37
Proposals for treatment according to the site of the tumour
Bone tumours
Forefoot
In the toes, the local treatment should be an amputation (or metatarso-phalangeal disarticulation) with a level depending on the proximal extension of the tumour. In the metatarsals, if the tumour is small with little soft tissue extension, an intercalary resection and reconstruction by bone grafting (vascularised or not) is feasible. In large tumours, a mid-foot amputation should be preferred. In cases of multiple metatarsal involvement, a partial amputation keeping the first and the fifth is possible with good results (Fig. 4). A free flap may be necessary for bone and/or soft-tissue reconstruction, such as a parascapular or a fibular free flap.38-40
Mid-foot
Some papers report cases of conservative treatment in malignant bone tumours of the mid-foot. It is often difficult to achieve the wide margins accepted in intra-osseous tumours or tumours with limited local spread. Reconstruction can sometimes be achieved by limited arthrodesis with bone grafting and flap for soft-tissue coverage.41,42
Hind-foot
Resection of a bone tumour of the calcaneus is technically demanding and possible in malignant conditions only in cases with an intra-osseous tumour. The surgeon should be aware of the risk for achieving only narrow margins of resection. Two surgical approaches may be necessary. It is also possible to perform a posterior approach with Achilles tendon section.
In calcaneus resection, there is a risk of heel anaesthesia if sacrificing the calcaneal branch of the posterior tibial nerve. Different options for bone reconstruction should be discussed. Diabetic foot surgery has shown that calcanectomy without reconstruction is possible with acceptable results. Acceptance, in our experience is better than with amputation but functional results are poorer.
Because the skin is very close to bone, there is a high risk of infection after reconstruction. Reconstructions with autografts of iliac crest graft with arthrodesis to adjacent bone or induced membrane technique have been reported.43 Some prefer to use allograft.44 Mobility of the heel skin over the reconstructed calcaneus is always a concern.
After talus resection is it possible in small children to articulate the distal tibia with the calcaneus and the joint will remodel with time. In the adolescent and adult, it is preferable to perform and arthrodesis between distal tibia, calcaneus and navicular, with very good functional results. There is a concern about very long-term degenerative changes in the adjacent joints of the foot. We have no experience in using allografts or prostheses, but good results have been reported.44,45
Distal tibial resection can be performed by a medial approach allowing control of the tibialis posterior bundle. The surgery can be performed in two stages, one for resection of the tumour (and the margin assessment) with reconstruction with cement and osteosynthesis. Then, after completion of adjuvant treatments, bone grafting, using the so-called ‘Masquelet procedure’.46 In cases of incomplete resection, an amputation should be performed. Some have published reconstruction by custom-made prosthesis.47,48 We prefer tibio-talar arthrodesis with different options: either induced membrane, tibial strut graft or vascularised fibular transfer (with fascio-cutaneous flap if necessary).9,49
In the distal fibula, reconstruction is not mandatory provided the ankle remains stabilised by an external brace for three months. Different options for reconstructions have been published, that can avoid long-term bracing for ankle stabilisation.50,51
Soft-tissue tumours
As in bone tumours, wide margins are mandatory and difficult to achieve in deep-seated lesions, close to the tendon sheaths and neurovascular structures.33 In cases of soft-tissue tumours with close contact or even bone invasion, the procedure should be to remove a layer of bone en bloc with the tumour.
Wound closure can be a concern. In the sole, the skin is very thick and there is a necessity for a sentient reconstruction. On the dorsal aspect of the foot, the skin is very thin and vascular and tendinous structures are very superficial. In small lesions, a primary suture is sometimes possible or a rotation flap to cover tendon and neurovascular structures. The donor site can be covered with a skin graft (in a non-weight-bearing area).
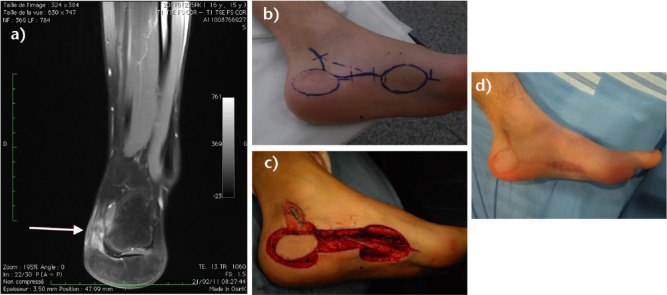
One should remember that a local recurrence can occur and lead to a secondary amputation.33,36 The flap should not modify a further amputation. In small resections of the hind-foot, the island medial plantar flap is sentient distal to the level of the primary tumour (Fig. 5). We prefer to avoid the distal sural flap (at least 5 cm above lateral malleolus, to keep the anastomoses with the fibular artery) for the heel and ankle defects, because it can change the level of a further amputation in cases of relapse.52
Fig. 5.
This 16- year-old male had a lump resection of the heel, without pre-operative imaging or biopsy. The diagnosis was a clear cell sarcoma. a) MRI of the left foot before ‘second-look’ surgery (T1 fat sat sequence coronal view). b) Drawing of the planned resection and flap. c) Intra-operative view after resection of the heel tumour and rotation of the medial plantar flap. Clear margins were achieved. d) Appearance of the foot two years after surgery.
In bigger resections, a free flap should be performed by a plastic surgeon.32,42 The antebrachial flap is easily harvested but cosmetically debatable. The parascapular flap (composite with bone) can allow bone and soft-tissue reconstruction. The dorsalis major flap is usually too large for the foot. The anterolateral region tight flap (ALT flap) is usually bulky and would have to be thinned secondarily. In all cases, these free flaps do not resolve the problem of plantar sensitivity.32
Recent development of the VAC therapy has allowed resection of superficial tumours with no reconstruction and secondary skin grafting.53
In all cases, healing of the wound should not delay the adjuvant treatment (chemotherapy and radiotherapy).33
Amputation
After amputation of lesser toes, an orthosis can help in keeping the other toes aligned. Some patients will have secondary deformities of adjacent toes, such as hallux valgus after second toe amputation. In cases of hallux amputation, a tenotomy of the flexor digitorum longus of the second toe at the proximal phalanx lever can limit the development of a secondary claw toe. It is generally recommended to resect the sesamoid bones and, if possible, to keep more plantar skin.
Partial longitudinal amputation usually gives good functional results thanks to an adapted shoe fitted with custom-made toe filler and moulded insole. In cases of fifth metatarsal amputation, the peroneus brevis should be fixed to the cuboid.
Lisfranc amputation gives good functional results provided it is possible to retain plantar soft tissue and skin to cover the stump. Some patients will use custom-made shoes but others can use normal shoes or boots with a combination of sole stiffeners and rocker bottoms in association with moulded insoles and toe fillers.54 Tibialis anterior and peroneus brevis tendons should be fixed to the remaining skeleton. It will often be necessary to perform a gastrocnemius lengthening to avoid equinus deformity.
Chopart’s amputation is at risk of secondary equinus or varus/valgus deformity (imbalance between triceps and extensors even after tendon transfer), with the development of painful callosities. Quality of skin coverage is a concern when one cannot keep plantar soft tissues.
In children, the hind-foot should be stabilised by fixation of the talus to the calcaneus by a screw, not intended to perform an arthrodesis before the end of skeletal growth. In the adult, the hind-foot is better stabilised by tibio-talo-calcaneal arthrodesis before doing the amputation itself. It is the only way to fix the hind-foot in a proper position and to avoid secondary deformities and impairment of propulsion. The stump should be covered by thick and sentient skin. The footwear can be normal in some rare cases with a forefoot filler but with poor function. The best functional results necessitate the use of a long prosthesis (up to the proximal tibia) to improve load transfer.
Symes amputation is no longer recommended because it is difficult to fit the prosthesis and there is much concern with instability of the skin over the bone.
The modified Pirogoff/Boyd amputation, with sacrifice of the talus and arthrodesis of the tibia to the calcaneus, is an alternative to Chopart’s amputation. The malleoli should be resected to decrease the width of the stump and allow easier fitting of the prosthesis. As in Chopart’s amputation, the patient will be able to walk without the prosthesis.
The distal tibia is the classic level of amputation in foot tumours and in cases of local recurrence of malignancy. Sometimes the tibia should be shortened in order to achieve adequate soft-tissue coverage of the skeleton to allow proper fitting of the prosthesis. It can give very good functional results provided there are no unexpected pain and skin complications.55
Keypoints
Malignant conditions are very rare in the foot.
They are often misdiagnosed and 50% are initially inadequately treated.
Always do imaging before removing a lump and send all resected fragments to the pathologist.
If a swelling is not an obvious synovial cyst or a plantar fibromatosis, do a biopsy.
Ewing’s and osteosarcoma have the same prognosis as in other locations (amputation should be considered).
Chondrosarcoma and soft-tissue sarcomata are often less aggressive than elsewhere.
Some histology of soft-tissue sarcoma (CC and epithelioid) is very confusing and more frequent in the foot.
All cases must be discussed in multidisciplinary team meetings and treated in specialised sarcoma centres.
Conservative treatments are difficult and lead to an increased risk of local recurrence.
Many local recurrences occur in soft-tissue tumours because of the particular anatomy of the foot.
Always consider if an amputation should be preferred to conservative management.
Footnotes
Conflict of Interest: None
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Kirby EJ, Shereff MJ, Lewis MM. Soft-tissue tumors and tumor-like lesions of the foot. An analysis of eighty-three cases. J Bone Joint Surg [Am] 1989;71-A:621-626. [PubMed] [Google Scholar]
- 2. Bakotic BW, Borkowski P. Primary soft-tissue neoplasms of the foot: the clinicopathologic features of 401 cases. J Foot Ankle Surg 2001;40:28-35. [DOI] [PubMed] [Google Scholar]
- 3. Macdonald DJ, Holt G, Vass K, Marsh A, Kumar CS. The differential diagnosis of foot lumps: 101 cases treated surgically in North Glasgow over 4 years. Ann R Coll Surg Engl 2007;89:272-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pretell-Mazzini J, Barton MD, Jr, Conway SA, Temple HT. Unplanned excision of soft-tissue sarcomas: current concepts for management and prognosis. J Bone Joint Surg [Am] 2015;97:597-603. [DOI] [PubMed] [Google Scholar]
- 5. Temple HT, Worman DS, Mnaymneh WA. Unplanned surgical excision of tumors of the foot and ankle. Cancer Control 2001;8:262-268. [DOI] [PubMed] [Google Scholar]
- 6. Young PS, Bell SW, MacDuff EM, Mahendra A. Primary osseous tumors of the hindfoot: why the delay in diagnosis and should we be concerned? Clin Orthop Relat Res 2013;471:871-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Group EESNW; ESMO/European Sarcoma Network Working Group. Soft tissue and visceral sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014;25:iii102-iii112. [DOI] [PubMed] [Google Scholar]
- 8. Group EESNW; ESMO/European Sarcoma Network Working Group. Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014;25:iii113-iii123. [DOI] [PubMed] [Google Scholar]
- 9. Cribb GL, Loo SC, Dickinson I. Limb salvage for soft-tissue sarcomas of the foot and ankle. J Bone Joint Surg [Br] 2010;92-B:424-429. [DOI] [PubMed] [Google Scholar]
- 10. Brotzmann M, Hefti F, Baumhoer D, Krieg AH. Do malignant bone tumors of the foot have a different biological behavior than sarcomas at other skeletal sites? Sarcoma 2013;2013:767960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Singer AD, Datir A, Tresley J, et al. Benign and malignant tumors of the foot and ankle. Skeletal Radiol 2016;45:287-305. [DOI] [PubMed] [Google Scholar]
- 12. Ruggieri P, Angelini A, Jorge FD, Maraldi M, Giannini S. Review of foot tumors seen in a university tumor institute. J Foot Ankle Surg 2014;53:282-285. [DOI] [PubMed] [Google Scholar]
- 13. Azevedo CP, Casanova JM, Guerra MG, et al. Tumors of the foot and ankle: a single-institution experience. J Foot Ankle Surg 2013;52:147-152. [DOI] [PubMed] [Google Scholar]
- 14. Zeytoonjian T, Mankin HJ, Gebhardt MC, Hornicek FJ. Distal lower extremity sarcomas: frequency of occurrence and patient survival rate. Foot Ankle In 2004;25:325-330. [DOI] [PubMed] [Google Scholar]
- 15. Schatz J, Soper J, McCormack S, et al. Imaging of tumors in the ankle and foot. Top Magn Reson Imaging 2010;21:37-50. [DOI] [PubMed] [Google Scholar]
- 16. Charoenlap C, Imanishi J, Tanaka T, et al. Outcomes of unplanned sarcoma excision: impact of residual disease. Cancer Med 2016;5:980-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gaston CL, Nakamura T, Reddy K, et al. Is limb salvage surgery safe for bone sarcomas identified after a previous surgical procedure? Bone Joint J 2014;96-B:665-672. [DOI] [PubMed] [Google Scholar]
- 18. Papp DF, Khanna AJ, McCarthy EF, et al. Magnetic resonance imaging of soft-tissue tumors: determinate and indeterminate lesions. J Bone Joint Surg [Am] 2007;89-A:103-115. [DOI] [PubMed] [Google Scholar]
- 19. Fayad LM, Ahlawat S, Khan MS, McCarthy E. Chondrosarcomas of the hands and feet: A case series and systematic review of the literature. Eur J Radiol 2015;84:2004-2012. [DOI] [PubMed] [Google Scholar]
- 20. Ogose A, Unni KK, Swee RG, et al. Chondrosarcoma of small bones of the hands and feet. Cancer 1997;80:50-59. [PubMed] [Google Scholar]
- 21. Bertoni F, Bacchini P, Hogendorn PCW. Chondrosarcoma. In: Fletcher CDM, Unni KK, Mertens F, ed. WHO classification of tumours of soft tissue and bone. Fourth ed. Lyon: IARC Press, 2013:247-251. [Google Scholar]
- 22. Ushigome S, Machinami R, Sorensen PH. Ewing sarcoma. In: Fletcher CDM, Unni KK, Mertens F, ed. WHO Classification of tumours of soft tissue and bone. Fourth ed. Lyon: IARC Press, 2013:297-300. [Google Scholar]
- 23. Guillou L, Kaneko Y. Epithelioid sarcoma. In: Fletcher CDM, Unni KK, Mertens F, ed. WHO classification of Tumours of soft tissue and bone. Lyon: IARC Press, 2013:205-207. [Google Scholar]
- 24. Oberlin O, Rey A, Brown KL, et al. Prognostic factors for outcome in localized extremity rhabdomyosarcoma. Pooled analysis from four international cooperative groups. Pediatr Blood Cancer 2015;62(12):2125-2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stomeo D, Tulli A, Ziranu A, Perisano C, Maccauro Vde S. Acrometastasis: a literature review. Eur Rev Med Pharmacol Sci 2015;19:2906-2915. [PubMed] [Google Scholar]
- 26. Foulon S, Brennan B, Gaspar N, et al. Can postoperative radiotherapy be omitted in localised standard-risk Ewing sarcoma? An observational study of the Euro-E.W.I.N.G group. Eur J Cancer 2016;61:128-136. [DOI] [PubMed] [Google Scholar]
- 27. Nakamura T, Grimer RJ, Carter SR, et al. Outcome of soft-tissue sarcoma patients who were alive and event-free more than five years after initial treatment. Bone Joint J 2013;95-B:1139-1143. [DOI] [PubMed] [Google Scholar]
- 28. Saeter G; ESMO Guidelines Working Group. Ewing’s sarcoma of bone: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol 2007;18:ii79-ii80. [DOI] [PubMed] [Google Scholar]
- 29. Kager L, Whelan J, Dirksen U, et al. The ENCCA-WP7/EuroSarc/EEC/PROVABES/EURAMOS 3rd European Bone Sarcoma Networking Meeting/Joint Workshop of EU Bone Sarcoma Translational Research Networks; Vienna, Austria, September 24-25, 2015. Workshop Report. Clin Sarcoma Res 2016;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jyothirmayi R, Sittampalam Y, Harmer C. Soft tissue sarcoma of the hand or foot: conservative surgery and radiotherapy. Sarcoma 1999;3:17-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Davidge KM, Wunder J, Tomlinson G, et al. Function and health status outcomes following soft tissue reconstruction for limb preservation in extremity soft tissue sarcoma. Ann Surg Oncol 2010;17:1052-1062. [DOI] [PubMed] [Google Scholar]
- 32. Ring A, Kirchhoff P, Goertz O, et al. Reconstruction of soft-tissue defects at the foot and ankle after oncological resection. Front Surg 2016;3:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kandel R, Coakley N, Werier J, et al. ; Sarcoma Disease Site Group of Cancer Care Ontario’s Program in Evidence-Based Care. Surgical margins and handling of soft-tissue sarcoma in extremities: a clinical practice guideline. Curr Oncol 2013;20:e247-e254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Furtado S, Grimer RJ, Cool P, et al. Physical functioning, pain and quality of life after amputation for musculoskeletal tumours: a national survey. Bone Joint J 2015;97-B:1284-1290. [DOI] [PubMed] [Google Scholar]
- 35. Aksnes LH, Bauer HC, Jebsen NL, et al. Limb-sparing surgery preserves more function than amputation: a Scandinavian sarcoma group study of 118 patients. J Bone Joint Surg [Br] 2008;90-B:786-794. [DOI] [PubMed] [Google Scholar]
- 36. Stojadinovic A, Jaques DP, Leung DH, Healey JH, Brennan MF. Amputation for recurrent soft tissue sarcoma of the extremity: indications and outcome. Ann Surg Oncol 2001;8:509-518. [DOI] [PubMed] [Google Scholar]
- 37. Thacker MM, Potter BK, Pitcher JD, Temple HT. Soft tissue sarcomas of the foot and ankle: impact of unplanned excision, limb salvage, and multimodality therapy. Foot Ankle Int 2008;29:690-698. [DOI] [PubMed] [Google Scholar]
- 38. Toma CD, Dominkus M, Pfeiffer M, et al. Metatarsal reconstruction with use of free vascularized osteomyocutaneous fibular grafts following resection of malignant tumors of the midfoot. A series of six cases. J Bone Joint Surg [Am] 2007;89-A:1553-1564. [DOI] [PubMed] [Google Scholar]
- 39. Fujioka M, Hayashida K, Senju C. Reconstruction of lateral forefoot using reversed medial plantar flap with free anterolateral thigh flap. J Foot Ankle Surg 2014;53:324-327. [DOI] [PubMed] [Google Scholar]
- 40. Mathieu G, Mascard E, Wicart P, Dubousset JF. Forefoot reconstruction after lesser intermediate metatarsal bone resection for aggressive or malignant tumors in children: report of three cases. Foot Ankle Int 2007;28:1011-1016. [DOI] [PubMed] [Google Scholar]
- 41. Battiston B, Artiaco S, Piana R, Boux E, Tos P. Midfoot reconstruction with serratus anterior-rib osteomuscular free flap following oncological resection of synovial sarcoma. J Orthop Traumatol 2015;16:347-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hara H, Kawamoto T, Onishi Y, et al. Reconstruction of the midfoot using a free vascularized fibular graft after en bloc excision for giant cell tumor of the tarsal bones: a case report. J Foot Ankle Surg 2016;55:838-841. [DOI] [PubMed] [Google Scholar]
- 43. Kurvin LA, Volkering C, Kessler SB. Calcaneus replacement after total calcanectomy via vascularized pelvis bone. Foot Ankle Surg 2008;14:221-224. [DOI] [PubMed] [Google Scholar]
- 44. Ayerza MA, Piuzzi NS, Aponte-Tinao LA, Farfalli GL, Muscolo DL. Structural allograft reconstruction of the foot and ankle after tumor resections. Musculoskelet Surg 2016;100:149-156. [DOI] [PubMed] [Google Scholar]
- 45. Harnroongroj T, Harnroongroj T. The talar body prosthesis: results at ten to thirty-six years of follow-up. J Bone Joint Surg [Am] 2014;96:1211-1218. [DOI] [PubMed] [Google Scholar]
- 46. Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R. Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury 2011;42:591-598. [DOI] [PubMed] [Google Scholar]
- 47. Shekkeris AS, Hanna SA, Sewell MD, et al. Endoprosthetic reconstruction of the distal tibia and ankle joint after resection of primary bone tumours. J Bone Joint Surg [Br] 2009;91-B:1378-1382. [DOI] [PubMed] [Google Scholar]
- 48. Stéphane S, Eric M, Philippe W, Félix DJ, Raphael S. Resection arthrodesis of the ankle for aggressive tumors of the distal tibia in children. J Pediatr Orthop 2009;29:811-816. [DOI] [PubMed] [Google Scholar]
- 49. Bishop AT, Wood MB, Sheetz KK. Arthrodesis of the ankle with a free vascularized autogenous bone graft. Reconstruction of segmental loss of bone secondary to osteomyelitis, tumor, or trauma. J Bone Joint Surg [Am] 1995;77-A:1867-1875. [DOI] [PubMed] [Google Scholar]
- 50. Jung ST, Park HW, Chung JY. Treatment of a severe neglected valgus deformity after excision of the distal fibula for Ewing’s sarcoma. J Bone Joint Surg [Br] 2012;94-B:138-140. [DOI] [PubMed] [Google Scholar]
- 51. Leibner ED, Ad-El D, Liebergall M, et al. Lateral malleolar reconstruction after distal fibular resection. A case report. J Bone Joint Surg [Am] 2005;87-A:878-882. [DOI] [PubMed] [Google Scholar]
- 52. Grandjean A, Romana C, Fitoussi F. Distally based sural flap for ankle and foot coverage in children. Orthop Traumatol Surg Res 2016;102:111-116. [DOI] [PubMed] [Google Scholar]
- 53. Maker AV, Iteld L. Closure of melanoma defects on the sole of the foot using glaborous skin: the end of the flap? Ann Surg Oncol 2015;22:4081-4082. [DOI] [PubMed] [Google Scholar]
- 54. Millstein SG, McCowan SA, Hunter GA. Traumatic partial foot amputations in adults. A long-term review. J Bone Joint Surg [Br] 1988;70-B:251-254. [DOI] [PubMed] [Google Scholar]
- 55. Pinzur MS, Gottschalk FA, Pinto MA, Smith DG; American Academy of Orthopaedic Surgeons. Controversies in lower-extremity amputation. J Bone Joint Surg [Am] 2007;89:1118-1127. [DOI] [PubMed] [Google Scholar]