Abstract
Pheochromocytoma is an uncommon tumor of the adrenal glands that can present with headaches, sweating, palpitations, and paroxysmal hypertension. Pheochromocytoma crisis can lead to cardiomyopathy, pulmonary edema, and even total circulatory collapse. We describe a patient with hypoxic respiratory failure requiring extracorporeal membrane oxygenation to stabilize until the pheochromocytoma was discovered and treated.
Pheochromocytoma is an uncommon tumor of the adrenal glands that can present with headaches, sweating, palpitations, and paroxysmal hypertension (1). Surgical excision is the only curative option. Preoperative management includes alpha blockade and volume expansion followed by beta blockade to treat tachycardia after sufficient alpha blockade has been established in order to prevent pheochromocytoma crisis. This crisis can usually be prevented if the pheochromocytoma is known, but sometimes this hypertensive crisis is the initial manifestation of the disorder. A crisis can lead to cardiomyopathy, pulmonary edema, and even total circulatory collapse (2). We describe a patient with hypoxic respiratory failure requiring extracorporeal membrane oxygenation (ECMO) to stabilize until the pheochromocytoma was discovered and treated.
CASE REPORT
A 37-year-old woman initially presented to an outside hospital with a chief complaint of nausea, vomiting, and abdominal pain. In the emergency department waiting room, she had a syncopal episode and was found to have a pulse oximeter oxygen saturation of 80% and hypertension with a blood pressure of 200/100 mm Hg. She was intubated because her hypoxia could not be improved with noninvasive methods and was then transferred to our tertiary medical center. Upon admission, an arterial blood gas showed a pH of 6.8, partial pressure of carbon dioxide of 51, partial pressure of oxygen of 71, and lactate of 10 mmoL/L. She had progressively worsening oxygenation and ventilation despite increasing ventilatory support. Neuromuscular-blocking agents and multiple ventilator modes and maneuvers including airway pressure release ventilation were unsuccessful in improving her respiratory status. Her initial chest radiograph is shown in Figure 1. During this time she also had extreme blood pressure lability with systolic pressures ranging from 80 to 200 mm Hg. Because she could not be adequately ventilated and oxygenated, the cardiothoracic surgical service was consulted. The patient was placed on veno-venous ECMO with a 23Fr femoral venous cannula and a 21Fr right internal jugular venous cannula. While stabilized on veno-venous ECMO, ventilation, oxygenation, and metabolic acidosis improved over the next few days.
Figure 1.

Chest radiograph on the day of admission.
Her family disclosed that the patient had a long history of refractory hypertension with failed medical management, intermittent headaches, and palpitations. The family also reported that the patient had not taken any of her blood pressure medications during the 2 weeks prior to her presentation because she could no longer afford them. Computed tomography angiography of the chest, abdomen, and pelvis showed bilateral, diffuse areas of ground glass opacity in the lung parenchyma and a large left adrenal mass (Figure 2). A 24-hour urinary vanillylmandelic acid (VMA) was 311 mg/dL (normal range < 7 mg/dL) and metanephrines were 91,867 mcg/24 h (normal range 147–523 mcg/24 h).
Figure 2.
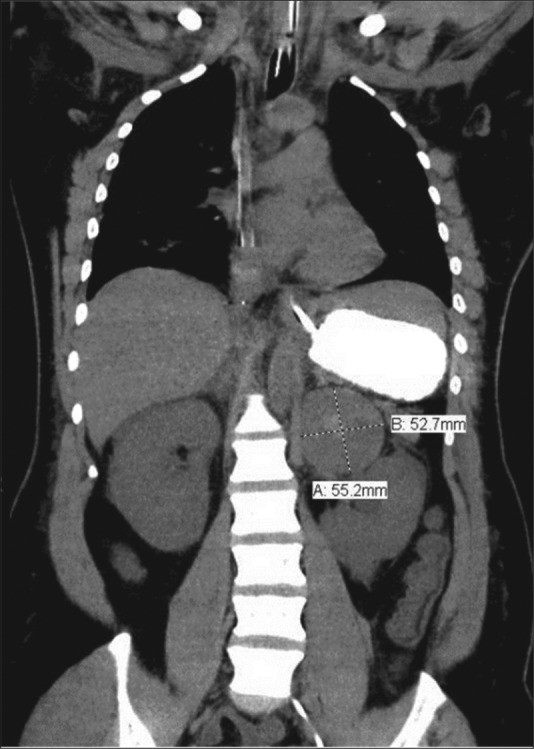
Computed tomography showing the adrenal mass.
The patient remained on veno-venous ECMO for 3 days. During the hospitalization, blood pressures were labile and temporary hemodialysis was required, but she then improved without permanent end-organ damage. After 2 weeks of alpha blockade, the patient underwent an open adrenalectomy (Figure 3). Blood pressure then became much easier to control. Pheochromocytoma without local invasion was confirmed histologically. The patient was discharged on carvedilol 25 mg twice daily and at 6 months postoperatively was doing well with a blood pressure of 108/71 mm Hg, normal renal function, and normal 24-hour urinary metanephrines.
Figure 3.

Surgical specimen of left adrenalectomy.
DISCUSSION
Pheochromocytoma is a catecholamine-secreting tumor arising from the chromaffin cells of the adrenal medulla. Present in only 0.2% of all patients with hypertension in the United States (1), these tumors typically occur sporadically, although they have been associated with genetic disorders including multiple endocrine neoplasia syndrome type 2 (3). Due to the low prevalence of pheochromocytoma and its often nonspecific signs and symptoms, diagnosis is often delayed. The classic triad of paroxysmal hypertension, palpitations, and headaches is an unusual presentation of pheochromocytoma. Twenty-four-hour urinary VMA and metanephrine testing remain the gold standard for diagnostic testing. The sensitivity and specificity of 24-h urinary VMA and metanephrines are 87.5% and 99.7%, respectively (4). About 10% of pheochromocytomas are malignant, and surgical extirpation is the only chance for a cure. However, the diagnosis of a malignant pheochromocytoma may prove difficult because they are histologically identical to benign pheochromocytomas, and the only definitive proof of malignancy is local or distant invasion or metastasis.
Preoperative optimization is essential to the safe performance of adrenalectomy (5). Alpha blockade with phenoxybenzamine and prazosin and correction of intravascular volume contraction are the essential tenets of preoperative management. Beta blockade for residual tachycardia may be added only after adequate alpha blockade has been achieved to prevent unopposed alpha adrenergic activity. Such unopposed alpha adrenergic activity can lead to circulatory collapse.
The preoperative requirement of ECMO due to crisis, as in our patient, is rare, but has been previously described (2, 6, 7). The patient's clinical history and large adrenal mass pointed the team toward the correct cause for her hypertensive emergency. Early recognition led to early appropriate treatment and a successful outcome. This case highlights the difficulty in the management of cardiogenic shock and respiratory failure secondary to pheochromocytoma and the important role that ECMO can play in the successful resuscitation and management of these patients and demonstrates a successful multidisciplinary approach in the management of a critically ill, complex patient.
References
- 1.Stein PP, Black HR. A simplified diagnostic approach to pheochromocytoma. A review of the literature and report of one institution's experience. Medicine. 1991;70(1):46–66. doi: 10.1097/00005792-199101000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Chao A, Yeh YC, Yen TS, Chen YS. Phaeochromocytoma crisis—a rare indication for extracorporeal membrane oxygenation. Anaesthesia. 2008;63(1):86–88. doi: 10.1111/j.1365-2044.2007.05251.x. [DOI] [PubMed] [Google Scholar]
- 3.Pacak K, Eisenhofer G, Ilias I. Diagnosis of pheochromocytoma with special emphasis on MEN2 syndrome. Hormones (Athens) 2009;8(2):111–116. doi: 10.14310/horm.2002.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheps SG, Jiang NS, Klee GG, van Heerden JA. Recent developments in the diagnosis and treatment of pheochromocytoma. Mayo Clin Proc. 1990;65(1):88–95. doi: 10.1016/s0025-6196(12)62113-2. [DOI] [PubMed] [Google Scholar]
- 5.Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, Naruse M, Pacak K, Young WF., Jr Endocrine Society. Pheochromocytoma and paraganglioma: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915–1942. doi: 10.1210/jc.2014-1498. [DOI] [PubMed] [Google Scholar]
- 6.Suh IW, Lee CW, Kim YH, Hong MK, Lee JW, Kim JJ, Park SW, Park SJ. Catastrophic catecholamine-induced cardiomyopathy mimicking acute myocardial infarction, rescued by extracorporeal membrane oxygenation (ECMO) in pheochromocytoma. J Korean Med Sci. 2008;23(2):350–354. doi: 10.3346/jkms.2008.23.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sojod G, Diana M, Wall J, D'Agostino J, Mutter D, Marescaux J. Successful extracorporeal membrane oxygenation treatment for pheochromocytoma-induced acute cardiac failure. Am J Emerg Med. 2012;30(6):1017.e1–1017.e3. doi: 10.1016/j.ajem.2011.05.006. [DOI] [PubMed] [Google Scholar]


