Abstract
Vitamin B12 deficiency may present as pseudothrombotic microangiopathy. Pseudothrombotic microangiopathy is anemia, thrombocytopenia, and schistocytosis caused by vitamin B12 deficiency. Pseudothrombotic microangiopathy may be mistaken for microangiopathic hemolytic anemia, confounding appropriate treatment. Evaluation of lactate dehydrogenase, reticulocyte count, bilirubin, and platelet count are most helpful in differentiating pseudothrombotic microangiopathy from a true microangiopathic hemolytic anemia. A case of pseudothrombotic microangiopathy due to severe vitamin B12 deficiency is presented.
Vitamin B12 deficiency may present with hemolytic anemia, thrombocytopenia, and schistocytosis, mimicking a microangiopathic hemolytic anemia. This is known as pseudothrombotic microangiopathy. Differentiating between pseudothrombotic microangiopathy and a true microangiopathic hemolytic anemia is of paramount importance, as the treatments are markedly different. A true microangiopathic hemolytic anemia such as thrombotic thrombocytopenic purpura (TTP) may be treated with intensive care unit admission and plasmapheresis, while pseudothrombotic microangiopathy may be treated with outpatient vitamin B12 supplementation.
CASE REPORT
A 36-year-old black man presented to an urban emergency department with a chief complaint of fatigue and poor exercise tolerance. His symptoms had been present for the past 2 years and were progressively worsening. His hemoglobin was 7.9 g/dL. There were no signs of active hemorrhage, fecal occult blood testing was negative, and he was hemodynamically stable.
Laboratory studies (Table 1) revealed a concurrent leukopenia and a platelet count in the low normal range. Erythrocyte indices showed macrocytosis, and corrected reticulocyte count reflected an inadequate reticulocyte response for the degree of anemia present. Iron studies were consistent with anemia of chronic inflammation. Vitamin B12 was determined to be markedly low, with an associated elevation in methylmalonic acid. Lactate dehydrogenase was profoundly elevated and haptoglobin was diminished, suggesting hemolysis. Renal function was normal and electrolytes were unremarkable. A peripheral smear (Figure 1) revealed moderate to severe macrocytic anemia with red cell fragmentation and schistocytes, as well as rare hypersegmented neutrophils. Prominent anisopoikilocytosis with teardrop cells, elliptocytes, macroovalocytes, and target cells was also identified.
Table 1.
Laboratory findings in the patient described
| Test | Result |
|---|---|
| Leukocytes (/mL) | 3300 |
| Hemoglobin (g/dL) | 7.9 |
| Platelets (/μL) | 157,000 |
| Mean corpuscular volume (fL) | 104.4 |
| Corrected reticulocyte count | 1.6% |
| Ferritin (ng/mL) | 380 |
| Iron (μg/dL) | 86 |
| Total iron binding capacity (μg/dL) | 222 |
| Iron saturation | 39% |
| Vitamin B12 (pg/mL) | 111 |
| Folate (ng/mL) | >24 |
| Homocysteine (μM/L) | 181.3 |
| Methylmalonic acid (mM/L) | 19.69 |
| Lactate dehydrogenase (U/L) | 3988 |
| Haptoglobin (mg/dL) | <30 |
| Aspartate aminotransferase (U/L) | 130 |
| Alanine aminotransferase (U/L) | 64 |
| Bilirubin (mg/dL) | 1.2 |
| Direct antiglobulin test | Negative |
Figure 1.
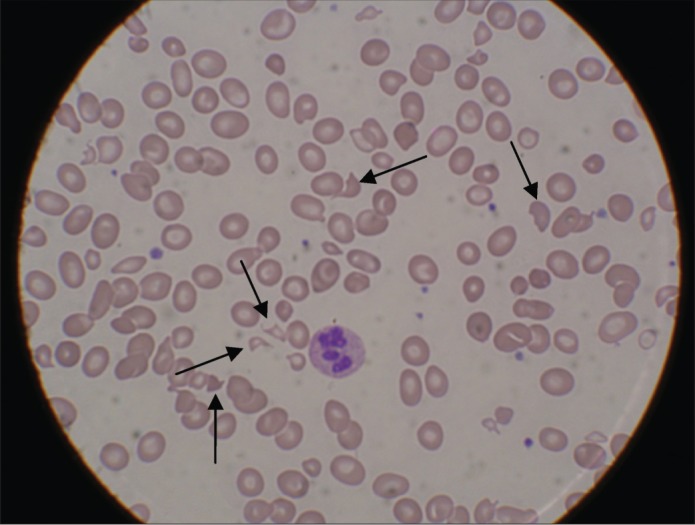
Peripheral smear showing a hypersegmented neutrophil and multiple schistocytes (arrows).
Neurologic examination, including mental status, cognition, reflexes, vibration, and proprioception, was normal. A bone marrow biopsy was performed, revealing macrocytic anemia, neutropenia, and mild marrow hypercellularity with trilineage dysplasia and a shift towards immaturity. Erythroid precursors were hyperplastic. No increase in the blast population and no evidence of an immunophenotypically aberrant cell population was noted. Serum anti-intrinsic factor antibodies were present. Esophagogastroduodenoscopy was performed and gastric biopsies were taken. Gastric biopsy showed evidence of reactive gastropathy, though features of atrophic gastritis were not confirmed. A diagnosis of severe vitamin B12 deficiency due to pernicious anemia with resultant pseudothrombotic microangiopathy was made. Hemoglobin levels remained stable, and the patient was discharged to home with subcutaneous cyanocobalamin injections.
DISCUSSION
The patient in this case report exhibited an uncommon manifestation of vitamin B12 deficiency: pseudothrombotic microangiopathy. The cause of this pseudothrombotic microangiopathy appeared to be intramedullary destruction of erythrocytes (ineffective erythropoiesis) (1). In one case series of 201 patients with vitamin B12 deficiency, 2.5% of patients exhibited pseudothrombotic microangiopathy (2). The infrequent occurrence of pseudothrombotic microangiopathy makes its accurate identification and diagnosis more difficult. Differentiating between pseudothrombotic microangiopathy and a true microangiopathic hemolytic anemia, such as TTP, is important, since an inappropriate diagnosis of TTP may lead to numerous unnecessary and expensive treatments, such as intensive care unit admission and plasmapheresis (3).
When treating a patient with suspected pseudothrombotic microangiopathy, laboratory studies are indispensable. The lactate dehydrogenase (LDH) and bilirubin levels should be evaluated. A more elevated LDH as well as a relatively normal unconjugated bilirubin is suggestive of pseudothrombotic microangiopathy. The purported mechanism is that the nucleated erythrocytes in the bone marrow elevate the LDH much more when they are lysed than unnucleated erythrocytes in the peripheral blood. In addition, the immature erythrocytes in the bone marrow contain very little hemoglobin, leading to only minor elevations in the unconjugated bilirubin when lysed. Another important laboratory study found to suggest pseudothrombotic microangiopathy in one case series was a low reticulocyte count (3). This is expected, as a deficiency of vitamin B12 leads to defective DNA synthesis and production of megaloblastic cells. Eighty to ninety percent of these cells are destroyed in the bone marrow through the action of marrow macrophages. This intramedullary hemolysis is the cause of the low reticulocyte count (ineffective erythropoiesis) (1). The platelet count should also be examined. The thrombocytopenia associated with TTP is generally severe, an average of 12,500 platelets/μL (3). The average platelet count of patients with pseudothrombotic microangiopathy is higher, approximately 70,000 platelets/μL (2, 3). The platelet count in this case report was atypical for pseudothrombotic microangiopathy in that it was low normal, 157,000 platelets/μL.
References
- 1.Antony AC. Megaloblastic anemias. In: Hoffman R, Benz EJ Jr, Shattil SJ, Furie B, Cohen HJ, Silberstein LE, McGlave P, editors. Hematology, Basic Principles and Practice. 4th ed. Philadelphia, PA: Elsevier; 2005. pp. 519–556. [Google Scholar]
- 2.Andrès E, Affenberger S, Zimmer J, Vinzio S, Grosu D, Pistol G, Maloisel F, Weitten T, Kaltenbach G, Blickle JF. Current hematological findings in cobalamin deficiency: a study of 201 consecutive patients with documented cobalamin deficiency. Clin Lab Haematol. 2006;28(1):50–56. doi: 10.1111/j.1365-2257.2006.00755.x. [DOI] [PubMed] [Google Scholar]
- 3.Noël N, Maigné G, Tertian G, Anguel N, Monnet X, Michot JM, Goujard C, Lambotte O. Hemolysis and schistocytosis in the emergency department: consider pseudothrombotic microangiopathy related to vitamin B12 deficiency. QJM. 2013;106(11):1017–1022. doi: 10.1093/qjmed/hct142. [DOI] [PubMed] [Google Scholar]


