Abstract
Background
The 2010 Dependent Coverage Provision (DCP) of the Affordable Care Act allowed young adults to remain on their parents’ health insurance plans until age 26y. While the provision improved coverage and survey-reported access to care, little is known regarding its impact on timely access for acute conditions. This study aims to assess changes in insurance coverage and perforation rates among young adults with acute appendicitis—an established metric for population-level healthcare access—after the DCP.
Methods
The National Inpatient Sample and difference-in-differences linear regression were used to assess pre-/post-policy changes for policy-eligible young adults (19–25 year-olds) compared to a slightly older, policy-ineligible comparator group (26–34 year-olds).
Results
After adjustment for covariates, 19–25 year-olds experienced a 3.6-percentage-point decline in the uninsured rate after the DCP (baseline 22.5%), compared to 26–34 year-olds (p<0.001). This coincided with a 1.4-percentage-point relative decline in perforated appendix rate for 19–25 year-olds (baseline 17.5%), compared to 26–34 year-olds (p=0.023). All subgroups showed significant reductions in uninsured rates; however, statistically significant reductions in perforation rates were limited to racial/ethnic minorities, patients from lower-income communities, and patients presenting to urban teaching hospitals.
Conclusions
Reductions in uninsured rates among young adults after the DCP were associated with significant reductions in perforated appendix rates relative to a comparator group, suggesting that insurance expansion could lead to fewer delays in seeking and accessing care for acute conditions. Greater relative declines in perforation rates among the most at-risk subpopulations hold important implications for the use of coverage expansion to mitigate existing disparities in access to care.
INTRODUCTION
Significant disparities in healthcare access and outcomes have been associated with a lack of insurance coverage in the United States.1–5 A major goal of the Affordable Care Act (ACA) is to reduce the number of uninsured in order to improve access to care. One of the earliest provisions of the ACA to take effect was the 2010 Dependent Coverage Provision (DCP), which enabled young adults to stay on their parents’ insurance plans until their 26th birthday. The DCP has led to an estimated 3–7% of uninsured young adults gaining insurance coverage6–12 and has also been linked to gains in access to care,13–15 decreases in self-reported delays in seeking care,9,16 and improvements in self-reported mental and physical health status.9,16,17 However, analyses of the DCP’s impact have been limited primarily to self-reported data. The impact of the policy on objective clinical measures of improved access to care remains unknown. Additionally, there remain no demonstrations of differential responses to gains in coverage among sociodemographic subgroups.
Perforated appendix rate among adults is a common and well-validated measure of access and quality in healthcare systems.18–22 It has been proposed as an ideal proxy for ambulatory-sensitive care because of it’s consistent and time-sensitive natural history progressing toward perforation (in the absence of treatment), with no known biological basis for variation among sociodemographic groups.18,20,21,23 While some have questioned its time-sensitive nature,24,25 perforated appendix rates are used throughout the literature as a marker for measuring access to care.16,17,20–23,26 Additionally, in 2001 perforated appendix rate was established as one of the Agency for Healthcare Research and Quality’s (AHRQ) Prevention Quality Indicators (PQIs).20 The PQIs are a set of 16 population-level metrics developed by the Department of Health and Human Services to utilize hospital inpatient discharge data to assess trends in ambulatory care sensitive conditions (ACSCs)—conditions that are thought to benefit from early intervention and access to care.20,21 Existing literature has demonstrated that perforated appendix rates are related to a number of population-level risk factors21 including insurance status,2,18,27,29,30 income,18,27 race,2,18,27 rurality,31 strength of surrounding healthcare delivery system,32,33 and healthcare utilization behavior.27
Especially for the mostly-healthy young adult population, evaluating a change in the perforated appendix rate presents an objective, sensitive, and well-established indicator that can relate changes in health insurance coverage to timely access to care. The purpose of this study is to assess changes in insurance coverage and perforation rates among young adults with acute appendicitis after the DCP. Specifically, this study exploits the quasi-experimental nature of the DCP by using a difference-in-differences (DID) analysis to: (1) assess changes in insurance coverage rates among young adults with acute appendicitis after the DCP, (2) measure any changes in perforated appendix rates associated with the DCP, and (3) examine whether changes in coverage and perforation rates varied across sociodemographic subgroups.
METHODS
Dataset
This was a retrospective analysis of 2006–2012 data from the Healthcare Cost and Utilization Project’s (HCUP) National Inpatient Sample (NIS)–the largest publicly-available dataset of all-payer inpatient discharges in the United States.34 The NIS is a stratified probability sample of inpatient hospital discharges that are weighted by region, hospital size, and teaching status to provide scaled national estimates. Notably, the sampling framework of the NIS changed in 2012.35 Prior to 2012, the NIS represented all discharge data from a 20% stratified sample of US hospitals. Starting in 2012, the NIS changed its sampling method to contain a 20% sample of discharges from all participating hospitals. To enable trend analysis across this sampling change, HCUP created updated discharge weights for the pre-2012 samples to make them comparable to the new design.35 Importantly, the NIS is particularly appropriate for analysis of perforated appendix rates as each admission is assigned 1–15 diagnosis codes based on ICD-9-CM classification system and because the NIS is the basis of the AHRQ PQIs, including PQI #2: perforated appendix admission rate.20,22
Variables
The primary outcome measure was the PQI-defined perforated appendix rate, calculated as the proportion of all patients with acute appendicitis who had any listed ICD-9-CM diagnosis codes for perforations or abscesses of the appendix (540.0, 540.1).22 The study’s secondary outcome was insurance status, coded as private, public, self-pay (uninsured), or other (which includes a heterogeneous mix of workers compensation, TRICARE, Indian Health Service, other government insurance, and other miscellaneous insurance).34
Covariates included patient- and neighborhood-level factors (age, sex, race/ethnicity, zip-code level income, comorbidities as defined below, and residential county rurality) and facility-level factors (teaching status and geographic region) thought to potentially impact perforated appendix rates. Race/ethnicity was defined as non-Hispanic White, Black, Hispanic, and other. Due to differential state-level reporting in the NIS, race/ethnicity information was missing for 17.9% of the included sample. To account for this, patient encounters were weighted using reweighted estimating equations – a method considered the least biased approach for handling missing race in the NIS.36 Corresponding inverse probability weights were incorporated into HCUP-NIS discharge weights using STATA-based svy commands. Patients missing race/ethnicity information were then excluded from adjusted analyses. The NIS provides an ordinal measure of community income by ranking the patient’s home zip code 1–4 according national quartile of per-zip code median household income. Patients living in zip-codes with a median household income in the highest two national quartiles for each year were defined as living in “higher-income communities” and those in the lowest two quartiles were defined as living in “lower-income communities.” Of note, this does not provide an actual measure of individual income, but rather it describes the income of the community in which the patients live. Elixhauser scores, categorized as 0 or ≥1, were calculated as a measure of comorbidity. Urban/rural status was based on patients’ residential counties and defined as large urban (counties with >= 1 million population), metro suburban (counties in metro areas with populations of 50,000–999,999), micropolitian (counties in metro areas with populations of 10,000–50,000), or rural (counties that are neither metropolitan or micropolitan) based on definitions provided by NIS and derived from the National Center for Health Statistics.34 Facilities were categorized according to the four geographic census regions and based on teaching status, using a NIS-defined variable that categorized hospitals as teaching (urban) or non-teaching (both urban and rural) facilities.
Analytic Sample
All patients 19–34 years old with any listed ICD-9-CM diagnosis code for acute appendicitis (540.0, 540.1, 540.9, 541) were included in the analytic sample. As per PQI specifications, obstetric admissions and transfers from other institutions were excluded.22 The DCP was enacted in September 2010 and enabled young adults to remain on their parents’ private insurance plans until their 26th birthday, effective with the date of a person’s plan renewal over the ensuing 12 months.9 As such, the analytic sample was restricted to policy-eligible patients (aged 19–25 years) and a slightly-older comparator group (aged 26–34 years). This comparator group was chosen because it is expected to have been similarly affected by any unmeasured secular trends during the study period and because of its similarities in demographics, insurance coverage rates prior to the DCP, labor market trends, and commonality of medical problems.8–11,13,37
Admissions from 2006 through the second quarter of 2010 (January–May) were included in the pre-policy period; admissions in 2011–2012 were included in the post-policy period. Since the DCP began in September 2010 but did not take effect for many enrollees until plans renewed at the end of the year (January 2011), admissions in the third/fourth quarters (June–December) of 2010 were excluded.
Analysis
This study leveraged the quasi-experimental nature of the DCP and used a difference-in-differences (DID) approach comparing changes in outcomes in the policy-eligible group to those in the comparator group, both before and after the DCP. This approach has already been used extensively to describe the effects of the DCP on young adults.8–11,13,37
This study relies on three DID analyses. First, a DID model was used to examined how the insurance coverage rate changed among 19–25 year-old patients with appendicitis before and after the DCP, as compared to 26–34 year olds. Second, a similar model was used to determine the effect of the DCP on perforated appendix rates between the two age groups. Lastly, the sample was stratified into sub-groups based on gender, race/ethnicity, baseline comorbidities, community income, rurality, and facility teaching status to test for variability in changes in coverage and perforated appendix rates after the policy. Post-hoc analyses of uninsured rates and perforated appendix rates during the pre- and post-policy periods were also performed. These post-hoc analyses included all adults with appendicitis aged 19–64 years in order to compare policy-eligible young adults to all non-elderly adults and to identify national secular trends during the study period.
All models were weighted to account for variations in sampling methodology and clustering of patients within hospitals. Analyses were conducted using STATA 14.0; two-sided p-values<0.05 were considered significant. The study was approved by the Partners Human Research Committee, the Institutional Review Board of Partners HealthCare.
Sensitivity Analyses
In order to determine the appropriateness of using a DID model, tests for parallel trends in study outcomes during the pre-policy period were performed. Three additional sensitivity analyses were then performed. Because the oldest members of the policy-eligible group and the youngest members of the comparator group would be expected to be most similar regarding the impact of secular trends, a sensitivity analysis was also performed to test the impact of focusing on a narrowed age band in the sample, comparing 22–25 year olds as the treatment group versus 26–29 year olds as the comparator group. To ensure that the effects were not driven by a longer pre-policy period, a second sensitivity analysis was performed to test the impact of focusing on a narrowed time period, in which only data from 2009–2012 were considered. Finally, to ensure that the results were not driven solely by the 2012 NIS redesign a specification test was performed by running the model unweighted but adding the NIS-provided weighting variables (discharge weight, hospital, and NIS stratum) as covariates to the model.
RESULTS
A total of 110,552 young adults (weighted to represent 527,210 patient encounters) met inclusion criteria for this study. Pre-policy tests for parallel trend in unadjusted uninsured rates and perforated appendix rates between the two groups revealed that the trends over time during the pre-policy period were not significantly different (Adjusted Wald test: p=0.133 and p=0.661). Pre- and post-policy demographics of the policy-eligible and comparator groups are shown in Table 1. In both groups, males were more likely to present with appendicitis than females—consistent with previously published national data.21 For both groups, approximately 4 in 10 patients were racial/ethnic minorities and approximately half of patients lived in lower-income communities. Most patients had no comorbidities (80.8% and 77.1% in the policy-eligible and comparator populations, respectively). Additionally, pre-policy uninsured rates were 22.5% for the policy-eligible group and 20.1% for the comparator group.
Table 1.
Comparison of Study Population Demographics Before and After the Dependent Coverage Provision
| Before the DCP1
|
After the DCP2
|
|||
|---|---|---|---|---|
| Policy-eligible Ages 19–25 | Policy-ineligible Ages 26–34 | Policy-eligible Ages 19–25 | Policy-ineligible Ages 26–34 | |
| Population3 | 37,479 | 42,477 | 14,637 | 15,959 |
| Mean Age (sd) | 21.8 (1.9) | 29.7 (2.6) | 21.8 (1.9) | 29.8 (2.6) |
|
| ||||
| Gender | ||||
|
| ||||
| Male | 57.2% | 57.3% | 55.5% | 54.9% |
| Female | 42.8% | 42.7% | 44.5% | 45.1% |
|
| ||||
| Race/Ethnicity4 | ||||
|
| ||||
| White, non-Hispanic | 62.5% | 59.3% | 58.0% | 55.9% |
| Non-white | 37.5% | 40.7% | 42.0% | 44.1% |
|
| ||||
| Patient comorbidities (Elixhauser score) | ||||
|
| ||||
| None | 80.8% | 75.4% | 77.1% | 71.4% |
| >= 1 | 19.2% | 24.6% | 22.9% | 28.6% |
|
| ||||
| Insurance Coverage | ||||
|
| ||||
| Private | 53.2% | 59.2% | 53.6% | 53.9% |
| Public | 16.2% | 14.8% | 18.6% | 18.6% |
| Uninsured | 22.5% | 18.7% | 20.1% | 20.0% |
| Other | 8.8% | 7.5% | 7.7% | 7.5% |
|
| ||||
| Income level of patient’s community5 | ||||
|
| ||||
| Lower income community | 50.7% | 49.5% | 51.0% | 49.9% |
| Higher income community | 49.3% | 50.5% | 49.0% | 50.1% |
|
| ||||
| Urban/rural designation of patient’s county | ||||
|
| ||||
| Urban | 66.0% | 68.9% | 60.4% | 63.9% |
| Metro Suburban | 19.3% | 17.7% | 25.8% | 24.1% |
| Micropolitan | 9.3% | 8.5% | 8.9% | 7.5% |
| Rural | 5.3% | 4.9% | 4.9% | 4.5% |
|
| ||||
| Facility teaching category | ||||
|
| ||||
| Teaching hospital | 12.0% | 11.1% | 11.6% | 10.1% |
| Non-teaching hospital | 88.0% | 88.9% | 88.4% | 89.9% |
|
| ||||
| Facility census region | ||||
|
| ||||
| Northeast | 22.4% | 19.9% | 23.4% | 21.3% |
| Midwest | 19.2% | 17.8% | 16.6% | 16.1% |
| South | 34.6% | 35.0% | 32.1% | 33.1% |
| West | 23.8% | 27.3% | 27.9% | 29.5% |
SOURCE: National Inpatient Sample (NIS), 2006 through 2012.
NOTE:
Before the DCP includes Q1 2006 through Q2 2010.
After the DCP includes Q1 2011 through Q4 2012.
According to NIS-provided discharge weights, the discharge-weighted population represents 178,321 policy-eligible patients before the policy and 70,517 post, as well as 201,575 policy-ineligible patients pre-policy and 76,797 post;
Non-white includes Black, Hispanic, and Other;
Based on whether median household income of patient’s zip code is in the lowest 2 vs highest 2 quartiles
Table 2 shows the DID estimates for changes in coverage and perforated appendix rates. During the pre-policy period, 19–25 year olds had lower private insurance rates (53.2% vs 59.2%), higher uninsured rates (22.5% vs 18.7%), and lower perforated appendix rates (17.5% vs 18.5%), as compared to 26–34 year olds (p<0.01 for all). After adjustment for covariates, 19–25 year old policy-eligible group experienced an increase in private coverage while the 26–34 year olds reported a decrease in private coverage; the difference between the two levels of change was +5.8 percentage points (p<0.001). Likewise, after adjustment for covariates, 19–25 year olds experienced a decrease in the rate of being uninsured, while the 26–34 year olds reported an increase in the uninsured rate; the difference between the two levels of change was −3.6 percentage points (p<0.001). The policy-ineligible 26–34 year olds experienced a significant increase in perforated appendix rate from 18.5% to 19.9% (p=0.007) from the pre-policy to post-policy period. Over the same period, policy-eligible 19–25 year olds experienced no significant change in perforation rate from 17.5% to 17.8% (p=0.649). After adjustment for covariates, the difference between the two levels of change in perforation rate was −1.4 percentage points (p=0.023). Three sensitivity analyses revealed very similar results (Appendix 1). Taken together at the population level, these findings suggest that for every 1,000 young adults presenting with acute appendicitis, 36 additional patients were now insured, when they would not have been previously. Coincident with these relatively small coverage changes, 14 fewer patients presented with perforation among the same hypothetical population of 1,000 young adults with appendicitis.
Table 2.
Changes in Insurance Status and Perforated Appendix Rates among Young Adults Ages 19–25 vs 26–34, Before and After The Dependent Coverage Provision
| Ages 19–25 | Ages 26–34 | Unadjusted difference in change between groups2 | Adjusted difference in change between groups3 | p value for between group difference | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Before Policy1 | After Policy | Before Policy | After Policy | ||||
| Sample | |||||||
|
| |||||||
| Patient encounters4 | 37,479 | 42,477 | 14,637 | 15,959 | -- | -- | -- |
|
| |||||||
| Insurance Status | |||||||
|
| |||||||
| Private | 53.2% | 53.7% | 59.2% | 53.9% | 5.8% | 5.8% | <0.001*** |
| Public | 16.2% | 18.6% | 14.8% | 18.6% | −1.5% | −1.6% | 0.018* |
| Other | 8.8% | 7.7% | 7.5% | 7.5% | −1.2% | −0.9% | 0.073 |
| Uninsured | 22.5% | 20.1% | 18.7% | 20.0% | −3.8% | −3.6% | <0.001** |
|
| |||||||
| Clinical endpoint | |||||||
|
| |||||||
| Perforated Appendix Rate | 17.5% | 17.8% | 18.5% | 19.9% | −1.1% | −1.4% | 0.023* |
SOURCE: National Inpatient Sample, 2006–2012.
NOTE:
Before Policy is years 2006 to Q2 of 2010, After policy is years 2011–2012, quarters 3 and 4 of 2010 are used as a washout year as the policy began in September 2010;
Calculated by subtracting the pre/post difference of the 19–25 year old age group from the pre/post difference of the 26–34 year old age group;
Adjusted for sample variation in year, patent-factors (age, sex, race, comorbidities, community income, urban/rural status), and facility-factors (census region and teaching status);
According to NIS-provided discharge weights, the discharge-weighted population represents 178,321 policy-eligible patients before the policy and 70,517 post, as well as 201,575 policy-ineligible patients pre-policy and 76,797 post;
p<0.05,
p<0.01,
p<0.001
Subgroup analyses revealed significant, although often unequal, reductions in uninsured rates regardless of sex, race/ethnicity, comorbid status, income, rurality, or teaching status of the managing facility (Table 3). However, statistically significant reductions in perforated appendix rates were concentrated among patients belonging to racial/ethnic minorities, from lower-income communities, or among patients presenting to urban teaching hospitals (Table 3).
Table 3.
Subpopulation Changes in Uninsured Rates and Perforated Appendix Rates
| Pre-policy1 baseline, 19–25 yo | Pre-policy1 baseline, 26–34 yo | Post-policy1 mean 19–25 yo | Post-policy1 mean, 26–34 yo | Adjusted difference in change between age groups2,3 | p-value for between age group difference | |
|---|---|---|---|---|---|---|
| Total Population4 | ||||||
|
| ||||||
| Uninsured Rate | 22.5% | 18.7% | 20.1% | 20.0% | −3.6% | <0.001*** |
| Perforation Rate | 17.5% | 18.5% | 17.8% | 19.9% | −1.4% | 0.023* |
|
| ||||||
| Males | ||||||
|
| ||||||
| Uninsured Rate | 26.7% | 22.6% | 23.7% | 24.9% | −4.8% | <0.001*** |
| Perforation Rate | 20.2% | 20.4% | 20.5% | 22.2% | −1.6% | 0.060 |
|
| ||||||
| Females | ||||||
|
| ||||||
| Uninsured Rate | 16.8% | 13.7% | 15.6% | 14.3% | −1.8% | 0.032* |
| Perforation Rate | 14.0% | 15.9% | 14.6% | 17.3% | −1.1% | 0.206 |
|
| ||||||
| White, non-Hispanic | ||||||
|
| ||||||
| Uninsured Rate | 16.6% | 13.8% | 15.1% | 16.1% | −4.3% | <0.001*** |
| Perforation Rate | 16.4% | 17.5% | 17.8% | 19.8% | −1.1% | 0.151 |
|
| ||||||
| Non-white5 | ||||||
|
| ||||||
| Uninsured Rate | 31.6% | 26.5% | 27.9% | 26.1% | −2.7% | 0.008** |
| Perforation Rate | 20.6% | 20.7% | 17.9% | 20.1% | −1.9% | 0.037* |
|
| ||||||
| No comorbidities | ||||||
|
| ||||||
| Uninsured Rate | 23.2% | 19.6% | 20.6% | 20.4% | −3.2% | <0.001*** |
| Perforation Rate | 16.5% | 17.3% | 16.6% | 18.4% | −1.2% | 0.074 |
|
| ||||||
| Elixhauser score >=1 | ||||||
|
| ||||||
| Uninsured Rate | 19.8% | 15.9% | 18.2% | 18.9% | −4.2% | 0.001** |
| Perforation Rate | 22.0% | 22.2% | 21.9% | 23.8% | −2.3% | 0.084 |
|
| ||||||
| Higher-income patient community6 | ||||||
|
| ||||||
| Uninsured Rate | 17.0% | 13.8% | 14.6% | 15.4% | −4.0% | <0.001*** |
| Perforation Rate | 16.7% | 17.6% | 17.0% | 18.8% | −0.8% | 0.327 |
|
| ||||||
| Lower-income patient community6 | ||||||
|
| ||||||
| Uninsured Rate | 27.9% | 23.6% | 25.5% | 24.6% | −3.2% | 0.001** |
| Perforation Rate | 18.3% | 19.2% | 18.5% | 20.9% | −2.0% | 0.026* |
|
| ||||||
| Urban or metro suburban patient county | ||||||
|
| ||||||
| Uninsured Rate | 22.2% | 18.5% | 19.8% | 19.8% | −3.4% | <0.001*** |
| Perforation Rate | 17.5% | 18.5% | 17.4% | 19.4% | −1.1% | 0.080 |
|
| ||||||
| Micropolitan or rural patient county | ||||||
|
| ||||||
| Uninsured Rate | 27.0% | 21.3% | 22.9% | 22.2% | −4.4% | 0.018* |
| Perforation Rate | 18.8% | 18.8% | 21.1% | 23.7% | −3.2% | 0.079 |
|
| ||||||
| Teaching Hospitals | ||||||
|
| ||||||
| Uninsured Rate | 27.4% | 22.1% | 23.6% | 22.2% | −4.0% | 0.049* |
| Perforation Rate | 18.6% | 18.1% | 19.9% | 22.5% | −4.5% | 0.031* |
|
| ||||||
| Nonteaching Hospitals | ||||||
|
| ||||||
| Uninsured Rate | 21.8% | 18.2% | 19.5% | 19.6% | −3.4% | <0.001*** |
| Perforation Rate | 17.4% | 18.5% | 17.6% | 19.5% | −1.0% | 0.114 |
SOURCE: National Inpatient Sample, 2006–2012.
NOTE:
Pre-policy is years 2006 to Q2 of 2010, Post-policy is years 2011–2012, Q3 and Q4 of 2010 are used as a washout year as the policy began in September 2010;
Calculated by subtracting the pre/post difference of the 19–25 year old age group from the pre/post difference of the 26–34 year old age group;
Adjusted for sample variation in year, patent-factors (age, sex, race, comorbidities, community income), and facility-factors (census region, urban-rural status, teaching status);
According to NIS-provided discharge weights, the discharge-weighted population represents 178,321 policy-eligible patients before the policy and 70,517 post, as well as 201,575 policy-ineligible patients pre-policy and 76,797 post. Please see Table 1 for proportions of each sample belonging to each subpopulation;
Non-white includes Black, Hispanic, and Other;
Based on median household income of patient’s Zip-code;
p<0.05,
p<0.01,
p<0.001
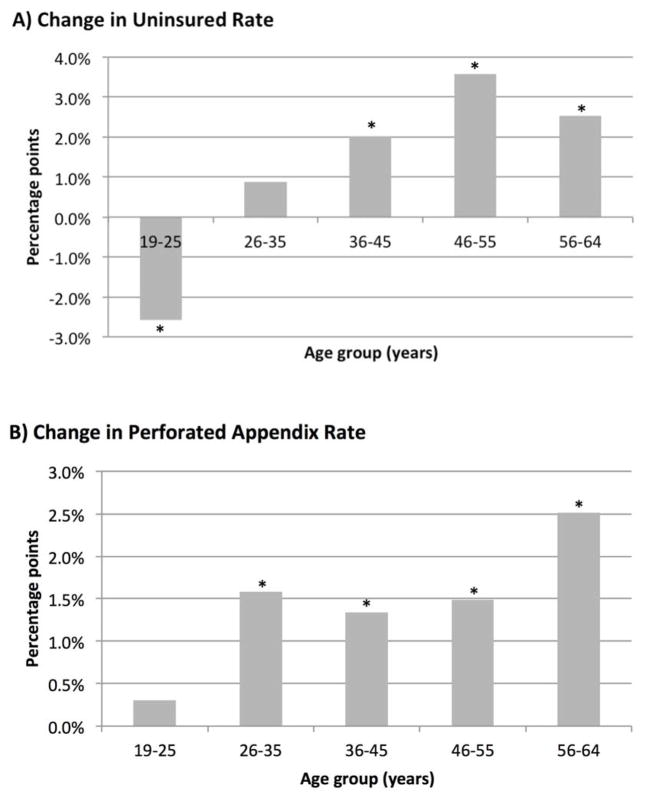
Nationally-weighted, post-hoc analyses of all adults aged 19–64 years with acute appendicitis showed that absolute uninsured rates increased across all age groups except for policy-eligible 19–25 year olds between the pre- and post-policy periods (Figure 1). Additionally, absolute perforation rates increased significantly by 1.3–2.5 percentage-points across all patients aged 26–64 years (p<0.05 for all). Notably, the policy-eligible 19–25 year olds did not experience a significant change in perforation rate (+0.3 percentage-points, p=0.510) (Figure 1).
Figure 1. Unadjusted, Absolute Change in Uninsured rates and Perforated Appendix Rates Among Non-elderly Adults During the Pre- and Post-policy Periods, by Age Group.
SOURCE: National Inpatient Sample (NIS), 2006–2012. NOTE: Based on post-hoc analysis of 19–64 year olds weighted to represent a total of 1,308,454 patients. Unadjusted, absolute percentage-point changes in (a) uninsured rate sand (b) perforated appendix rates are shown by age group (in years). The pre-policy period includes 2006 through the 2nd quart of 2010. Post-policy period includes 2011–2012. Quarters 3 and 4 of 2010 were used as a washout period because the dependent coverage provision policy began in September 2010 and did not come into effect for some until policies were renewed in January. * p < 0.05
DISCUSSION
Analysis of the largest nationally representative all-payer database in the United States demonstrated that the ACA’s DCP was associated with significant reductions both in the uninsured rate and in the rate of perforation among young adults with acute appendicitis, compared to a similar population-based policy-ineligible comparator group. Reductions in uninsured rates occurred in all analyzed subpopulations of young adults. However, significant reductions in perforated appendix rates were concentrated among minority and lower-income patients, as well as those presenting to teaching hospitals.
The DCP directly led to expanded insurance coverage for a substantial proportion of young adults, but had no other obvious mechanism to affect a patient’s health status, income, social community, or availability of ambulatory care providers. Although existing literature suggests that appendicitis perforation rates are related to a number of patient- and community-level factors2,18,27–33 the quasi-experimental approach used in this study attempted to isolate the effect secondary to changes in insurance status alone—as the DID model provided reasonable adjustment for other secular trends. Prior studies of the DCP have demonstrated fewer self-reported delays in seeking care, an increased likelihood of having a usual source of care, improved self-reported health status, decreased proportion of expenses paid out of pocket, and reductions in the inability to seek care due to costs.9,16,17 Similarly, others have shown that following implementation of the DCP, fewer young adult patients in the emergency room were uninsured37 and there was a modest decrease in emergency department for discretionary visits.14 The findings of the current study further existing literature by demonstrating that the DCP was associated with improvements in an objective, clinically-based measure of access to care.
As an AHRQ PQI for delayed access to care, higher perforation rates among the uninsured are thought to result from a combination of patient, provider, and systems-based causes for delay.2,19,38 Prior literature suggests that delays in seeking care and delays in accessing care once the decision to seek care has been made,39 and not in-hospital treatment delays, are the most important causes of delay among patients with acute appendicitis.2,27,29,40 Uninsured patients have been previously shown to have a longer duration of symptoms prior to presentation for acute appendicitis.29 Additionally, patients with an established primary care physician and those with a history of well-patient visits have lower perforated appendix rates, possibly because of fewer delays in choosing to seek care and fewer barriers to accessing care.27 Conversely, perforated appendix rates were not found to be associated with longer in-hospital delays to definitive therapy after arriving at a treating facility40 or a facility’s negative appendectomy rate.2
It is notable that the post-hoc analysis revealed increased or unchanged uninsured rates among all non-elderly adults who were not in the policy-eligible age group. All of these policy-ineligible nonelderly adults also experienced significantly higher perforated appendix rates in the post-policy period (Figure 1). The follow-up period of the study ended in 2012, prior to the initiation of most insurance coverage-related policies related to the ACA (2013–2015). The observed population-wide trends among 26–64 year olds may be, at least partly, reflective of residual effects of the economic recession, which could have led to more uninsured patients and, thus, more delays in seeking care. The consistent increases in both uninsured rates and perforation rates across all age groups except those eligible for the dependent coverage expansion suggest that the DCP may have spared the policy-eligible young adults from some of the negative effects of the economic downturn experienced by older nonelderly adults.
It is therefore possible that the protection against rising perforated appendix rates seen among policy-eligible young adults after the DCP is due to changes in patients’ care-seeking behavior in response to receiving insurance coverage. Young adults have been shown to be at high risk of delaying care due to costs,8 and thus it is possible their relative reduction in perforation rate was due to a perceived reduction in financial barriers to seeking care after the acquisition of insurance coverage. Additionally, it is possible that the coverage gains from the DCP, which have been associated with an increased likelihood of having a primary care provider,16 could lead to both earlier care seeking behavior as well as more timely means to access care via ambulatory referral.
It is notable that all subgroups experienced significant coverage gains, and yet statistically significant reductions in perforated appendix rates were concentrated among racial/ethnic minorities. This calls into question the potential influence of socioeconomic and community factors2,5,39 on patients’ responses to gaining insurance coverage. Further studies will be required to better understand the mechanisms behind these associations. It is possible that patients from higher-income communities seeking care at non-teaching hospitals have the means to pay for care out of pocket and thus may have been less likely to delay seeking care, despite being uninsured, prior to the DCP. Conversely, lower income and minority patients who may be more reliant on teaching hospitals41 may be at greater risk for delays in seeking care when uninsured,5 which could partially explain a more robust response to gains in coverage. These findings suggest that patients who are socially or economically disadvantaged may benefit the most from insurance expansion policies. The DCP was not intended to address existing racial/ethnic disparities in access to care. It extended coverage to people of all races and income levels, however minority patients and lower income patients experienced substantially smaller increases in coverage. Further research is needed to provide a more detailed understanding of this differential response to coverage gains in order to better inform policy makers seeking to mitigate disparities in access to care.
Finally, it should be noted that reducing the number of uninsured is only one component of improving access. Since October 2013, many uninsured adults ineligible for Medicaid are gaining coverage through Health Insurance Marketplace plans, many of which require significant cost sharing in the form of high deductibles and copayments.42 In effect, some patients may move from being uninsured to being underinsured. As such, future studies regarding changes in access to care after gaining insurance will need to be mindful of these issues.
The findings of this study must be interpreted in light of the following limitations. First, the NIS does not permit following individual patients longitudinally through multiple encounters over time. As such, only population-level changes can be determined from these analyses. However, the AHRQ PQI of perforated appendix rates is itself a population-level metric. Further, the type of DID models utilized in this study are commonly used to analyze population-level effects of policy changes. Second, the NIS changed their sampling methodology in 2012, which makes the data more difficult to compare over time. To account for this, all of the DID models in this study were run using NIS-provided weights to enable analysis across this sampling change35 and a sensitivity analysis adjusting for this change also resulted in the similar findings (Appendix 1) Also, the DID models used in this study are not expected to be biased by these sampling changes, since they should have similarly affected both policy-eligible 19–25 year olds and policy-ineligible 26–34 year olds. Third, while this study used patients ages 26–34 as a comparison group in keeping with prior studies involving the DCP,9–12,16,17 there is no way to guarantee that this comparator group was affected by secular trends in exactly the same ways as the policy-eligible 19–25 year olds. However, a sensitivity analysis that used tighter age groups that are expected to be more similar regarding unmeasured secular trends found very similar results (Appendix 1).
In summary, this nationally representative analysis of young adults with acute appendicitis suggests that reductions in the uninsured rate after implementation of the ACA’s dependent coverage provision were associated with relative reductions in perforated appendix rates—an established metric for population-level healthcare access. This suggests that insurance expansion may have led to fewer delays in seeking care as well as fewer delays in accessing care when sought. Specific subpopulations, notably racial/ethic minorities, those from lower income communities, and those reliant on teaching hospitals appear to have been more responsive to coverage gains as evidenced by more robust reductions in perforation rates. These findings have important implications for the potential use of insurance expansion polices to reduce existing disparities in access to care.
Supplementary Material
Footnotes
Declaration of Conflicts of Interest
Dr. Scott, Dr. Rose, Dr. Salim, and Ms. Zogg have no conflicts of interest or financial disclosures. Dr. Shrime received speaking fees from Ethicon in 2014 for work unrelated to this project. Dr. Sommers and Dr. Tsai serve part-time as advisors to the Office of the Assistant Secretary for Planning and Evaluation at the Department of Health & Human Services. This work does not represent the official views of the US Department of Health and Human Services. Dr. Haider is the PI of a contract (AD-1306-03980) with the Patient-Centered Outcomes Research Institute entitled “Patient-Centered Approaches to Collect Sexual Orientation/Gender Identity in the ED” and a Harvard Surgery Affinity Research Collaborative (ARC) Program Grant entitled “Mitigating Disparities Through Enhancing Surgeons’ Ability To Provide Culturally Relevant Care.” AHH is also the co-founder and an equity holder in Patient Doctor Technologies Inc., which owns and operates the website www.doctella.com.
References
- 1.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet Health Needs of Uninsured Adults in the United States. JAMA. 2000;284(16):2061–9. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 2.Ponsky TA, Huang ZJ, Kittle K, et al. Hospital- and Patient-Level Characteristics and the Risk of Appendiceal Rupture and Negative Appendectomy in Children. JAMA. 2004;292(16):1977–82. doi: 10.1001/jama.292.16.1977. [DOI] [PubMed] [Google Scholar]
- 3.Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R. Uninsured Adults Presenting to US Emergency Departments: Assumptions vs Data. JAMA. 2008;300(16):1914–24. doi: 10.1001/jama.300.16.1914. [DOI] [PubMed] [Google Scholar]
- 4.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE. Race and Insurance Status as Risk Factors for Trauma Mortality. Archives of Surgery. 2008;143(10):945–9. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 5.Hargraves JL, Hadley J. The Contribution of Insurance Coverage and Community Resources to Reducing Racial/Ethnic Disparities in Access to Care. Health Serv Res. 2003;38(3):809–29. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sommers BD. Number of young adults gaining insurance due to the Affordable Care Act now tops 3 million [Internet] Washington (DC): Department of Health and Human Services; 2012. Jun, [cited 2015 Sept 24]. Available from: http://aspe.hhs.gov/aspe/gaininginsurance/rb.cfm. [Google Scholar]
- 7.Antwi YA, Moriya A, Simon K. Effects of Federal Policy to Insure Young Adults: Evidence from the 2010 Affordable Care Act Dependent Coverage Mandate. Am Econ J. 2013;5(4):1–28. [Google Scholar]
- 8.Cantor JC, Monheit AC, delia D, Lloyd K. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47(5):1773–90. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sommers BD, Buchmueller T, Decker SL, Carey C, Kronick R. The Affordable Care Act Has Led To Significant Gains In Health Insurance And Access To Care For Young Adults. Health Affairs. 2013;32(1):165–74. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 10.Sommers BD, Kronick R. The Affordable Care Act and insurance coverage for young adults. JAMA. 2012;307(9):913–4. doi: 10.1001/jama.307.9.913. [DOI] [PubMed] [Google Scholar]
- 11.Scott JW, Sommers BD, Tsai TC, Scott KW, Schwartz AL, Song Z. Dependent Coverage Provision Led To Uneven Insurance Gains And Unchanged Mortality Rates In Young Adult Trauma Patients. Health Affairs. 2015;34(1):125–33. doi: 10.1377/hlthaff.2014.0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott JW, Salim A, Sommers BD, Tsai TC, Scott KW, Song Z. Racial and Regional Disparities in the Effect of the Affordable Care Act’s Dependent Coverage Provision on Young Adult Trauma Patients. J Am Coll Surg. 2015;221(2):495–501. doi: 10.1016/j.jamcollsurg.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antwi YA, Moriya AS, Simon K. Access to health insurance and the use of inpatient medical care: Evidence from the Affordable Care Act young adult mandate [Internet] Bloomington, IN: Indiana University; 2013. [cited 2015 Sept 24]. Available from: http://business.illinois.edu/nmiller/mhec/Antwi.pdf. [DOI] [PubMed] [Google Scholar]
- 14.Antwi YA, Moriya AS, Simon K, Sommers BD. Changes in Emergency Department Use Among Young Adults After the Patient Protection and Affordable Care Act’s Dependent Coverage Provision. Ann Emerg Med. 2015;65(6):664–672. doi: 10.1016/j.annemergmed.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Barbaresco S, Courtemanche CJ, Qi Y. Impacts of the Affordable Care Act dependent coverage provision on health-related outcomes of young adults. Cambridge (MA): National Bureau of Economic Research; 2014. May, (NBER Working Paper No. 20148) [DOI] [PubMed] [Google Scholar]
- 16.Wallace J, Sommers BD. Effect of dependent coverage expansion of the Affordable Care Act on health and access to care for young adults. JAMA Pediatr. 2015;169(5):495–7. doi: 10.1001/jamapediatrics.2014.3574. [DOI] [PubMed] [Google Scholar]
- 17.Chua K-P, Sommers BD. Changes in Health and Medical Spending Among Young Adults Under Health Reform. JAMA. 2014;311(23):2437–9. doi: 10.1001/jama.2014.2202. [DOI] [PubMed] [Google Scholar]
- 18.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-Related Differences in the Risk of Ruptured Appendix. N Engl J Med. 1994;331(7):444–9. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 19.Bickell NA, Siu AL. Why do delays in treatment occur? Lessons learned from ruptured appendicitis. Health Serv Res. 2001;36(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 20.AHRQ Quality Indicators—Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2001. [cited 2016 Mar 1]. Available from: http://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf. [Google Scholar]
- 21.Barrett ML, Hines AL, Andrews RM. HCUP Statistical Brief #159. [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2013. Trends in Rates of Perforated Appendix, 2001–2010. [cited 2015 Sept 24] Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb159.pdf. [PubMed] [Google Scholar]
- 22.Perforated Appendix Admission Rate Technical Specifications [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2013. [cited 2015 Sept 24] Available from: http://www.qualityindicators.ahrq.gov/Downloads/Modules/PQI/V45/TechSpecs/PQI%2002%20Perforated%20Appendix%20Admission%20Rate.pdf. [Google Scholar]
- 23.Nwomeh BC, Chisolm DJ, Caniano DA, Kelleher KJ. Racial and socioeconomic disparity in perforated appendicitis among children: Where is the problem? Pediatrics. 2006;117(3):870–5. doi: 10.1542/peds.2005-1123. [DOI] [PubMed] [Google Scholar]
- 24.Livingston EH, Fomby TB, Woodward WA, Haley RW. Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Archives of Surgery. 2011;146(3):308–14. doi: 10.1001/archsurg.2011.2. [DOI] [PubMed] [Google Scholar]
- 25.Livingston EH, Fairlie RW. Little Effect of Insurance Status or Socioeconomic Condition on Disparities in Minority Appendicitis Perforation Rates. JAMA Surgery. 2012;147(1):11–7. doi: 10.1001/archsurg.2011.746. [DOI] [PubMed] [Google Scholar]
- 26.Gadomski A, Jenkins P. Ruptured appendicitis among children as an indicator of access to care. Health Serv Res. 2001;36(1):129–42. [PMC free article] [PubMed] [Google Scholar]
- 27.Guagliardo MF, Teach SJ, Huang ZJ, Chamberlain JM, Joseph JG. Racial and ethnic disparities in pediatric appendicitis rupture rate. Academic Emergency Medicine. 2003;10(11):1218–27. doi: 10.1111/j.1553-2712.2003.tb00606.x. [DOI] [PubMed] [Google Scholar]
- 28.Jablonski KA, Guagliardo MF. Pediatric appendicitis rupture rate: a national indicator of disparities in healthcare access. Popul Health Metr. 2005;3(1):1–9. doi: 10.1186/1478-7954-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Toole SJ, Karamanoukian HL, Allen JE. Insurance-related differences in the presentation of pediatric appendicitis. J Ped Surgery. 1996;31(8):1032–4. doi: 10.1016/s0022-3468(96)90079-2. [DOI] [PubMed] [Google Scholar]
- 30.Pieracci FM, Eachempati SR, Barie PS, Callahan MA. Insurance status, but not race, predicts perforation in adult patients with acute appendicitis. ACS. 2007;205(3):445–52. doi: 10.1016/j.jamcollsurg.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Paquette IM, Zuckerman R, Finlayson SRG. Perforated appendicitis among rural and urban patients: implications of access to care. Ann Surg. 2011;253(3):534–8. doi: 10.1097/SLA.0b013e3182096d68. [DOI] [PubMed] [Google Scholar]
- 32.Mack D, Rust GS, Baltrus P, et al. Using appendiceal perforation rates to measure impact of a disaster on healthcare system effectiveness. South Med J. 2012;106(1):82–8. doi: 10.1097/SMJ.0b013e31827c5a0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neuwahl S, Ricketts T, Holmes M. The impact of general surgeon supply on the risk of appendiceal rupture in North Carolina. Ann Surg. 2014;259(5):910–5. doi: 10.1097/SLA.0b013e3182988804. [DOI] [PubMed] [Google Scholar]
- 34.Overview of the National (Nationwide) Inpatient Sample (NIS) [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2013. [cited 2016 Mar 1]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2013.jsp. [Google Scholar]
- 35.Houchens RL, Ross DN, Elixhauser A, Jiang J. Nationwide Inpatient Sample Redesign Final Report 2014 [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2014. [cited 2015 Sept 24]. Available from: http://www.hcup-us.ahrq.gov/db/nation/nis/nisrelatedreports.jsp. [Google Scholar]
- 36.Henry AJ, Hevelone ND, Lipsitz S, Nguyen LL. Comparative methods for handling missing data in large databases. J Vasc Surg. 2013;58(5):1353–6. doi: 10.1016/j.jvs.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 37.Mulcahy A, Harris K, Finegold K, Kellermann A, Edelman L, Sommers BD. Insurance coverage of emergency care for young adults under health reform. N Engl J Med. 2013;368(22):2105–12. doi: 10.1056/NEJMsa1212779. [DOI] [PubMed] [Google Scholar]
- 38.Bickell NA, Hwang U, Anderson RM, Rojas M, Barsky CL. What Affects Time to Care in Emergency Room Appendicitis Patients? Medical Care. 2008;46(4):417–22. doi: 10.1097/MLR.0b013e31815c1e66. [DOI] [PubMed] [Google Scholar]
- 39.Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Social Science & Medicine. 1994;38(8):1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 40.Drake FT, Mottey NE, Farrokhi ET, et al. Time to Appendectomy and Risk of Perforation in Acute Appendicitis. JAMA Surgery. 2014;149(8):837–44. doi: 10.1001/jamasurg.2014.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Silber JH, Rosenbaum PR, Romano PS, Rosen AK, Wang Y, Teng Y, et al. Hospital teaching intensity, patient race, and surgical outcomes. Archives of Surgery. 2009;144(2):113–20. doi: 10.1001/archsurg.2008.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gabel J, Whitmore H, Green M, Stromberg S, Oran R. Consumer Cost-Sharing in Marketplace vs. Employer Health Insurance Plans, 2015 [Internet] The Commonwealth Fund; 2015. [cited 2016 Mar 1]. Available from: http://www.commonwealthfund.org/publications/issue-briefs/2015/dec/cost-sharing-marketplace-employer-plans. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.