Abstract
Purpose
Preclinical evidence suggests that both docetaxel and enzalutamide target androgen receptor translocation and signaling. This phase Ib study assessed the safety, tolerability, and pharmacokinetics of docetaxel when administered with enzalutamide as first-line systemic chemotherapy in men with metastatic castration-resistant prostate cancer (mCRPC).
Experimental Methods
Docetaxel-naïve patients received 21-day cycles of docetaxel (75 mg/m2). Enzalutamide (160 mg/day) was administered daily starting on day 2 of cycle 1. Patients were allowed to stop and restart docetaxel at any time following cycle 2. Treatment continued indefinitely until unacceptable toxicity or discontinuation due to investigator or patient preference.
Results
A total of 22 patients received docetaxel, of whom 21 also received enzalutamide. Docetaxel was administered for a median of 5.0 cycles and enzalutamide for a median of 12.0 months. With concomitant treatment, geometric mean docetaxel exposure decreased by 11.8%, whereas peak concentrations decreased by 3.7% relative to docetaxel alone. The most common toxicities observed during the period of concomitant therapy were neutropenia (86.4%) and fatigue (77.3%). Common toxicities observed with post-docetaxel enzalutamide were constipation (23.8%), decreased appetite (19.0%), fatigue (19.0%), and musculoskeletal pain (19.0%). Treatment with enzalutamide and docetaxel resulted in prostate-specific antigen decreases in almost all patients based on exploratory analysis of available baseline and on-study prostate-specific antigen data.
Conclusions
The combination of docetaxel and enzalutamide is feasible, although higher rates of neutropenia and neutropenic fever than anticipated were observed. Reductions in docetaxel exposure with enzalutamide coadministration were not considered clinically meaningful. This combination warrants further study in a larger mCRPC population.
Introduction
Docetaxel combined with prednisone was approved by the U.S. Food and Drug Administration (FDA) in 2004 for the treatment of men with androgen-independent (hormone refractory) metastatic prostate cancer based on results of the TAX 327 study, which demonstrated that docetaxel and prednisone improved overall survival (OS), reduced pain and prostate-specific antigen (PSA) levels, and improved quality of life relative to mitoxantrone and prednisone (1, 2).
Enzalutamide is an oral, potent, androgen receptor (AR) inhibitor. Mechanistically, enzalutamide inhibits binding of androgens to the AR, blocks nuclear translocation of the AR complex, and interferes with the association of the AR complex and DNA (3). An initial phase I/II trial in patients with advanced castration-resistant prostate cancer (CRPC) revealed that enzalutamide had clinical efficacy in both chemotherapy-naïve patients and those previously treated with docetaxel (4). Subsequently, two large placebo-controlled phase III trials have demonstrated that enzalutamide significantly improves OS and radiographic progression-free survival in patients with metastatic CRPC (mCRPC) in both the pre- and post-docetaxel settings (PREVAIL [5] and AFFIRM [6] trials, respectively).
Preclinical studies have shown that docetaxel, for which microtubule stabilization is the principal mechanism of action, can also directly affect AR signaling in prostate cancer by inhibiting nuclear translocation of the AR (7–9). These studies suggest that the therapeutic effect of docetaxel may, in part, be due to its ability to impair AR signaling. A recent study based on in vitro assays showed that docetaxel at low (nanomolar) concentrations had no impact on AR localization (10); however, the clinical significance of this finding is uncertain as plasma concentrations of docetaxel are typically maintained above 10 nmol/L for at least 24 hours in patients receiving 75 mg/m2 docetaxel.
Given that both enzalutamide and docetaxel are approved by the FDA for treatment of patients with mCRPC, the combination of these agents may have the potential to further increase response rates and survival compared with monotherapy. The present trial evaluated the safety, tolerability, and pharmacokinetics (PK) of docetaxel when combined with enzalutamide in men with mCRPC. Posttreatment PSA levels were also assessed as an exploratory efficacy endpoint.
Patients and Methods
The study enrolled men with mCRPC who were eligible to receive docetaxel as their first systemic chemotherapy. The study was conducted at two sites, Memorial Sloan Kettering Cancer Center (MSKCC), New York, New York, and Virginia Oncology Associates, Norfolk, Virginia. The study protocol was approved by the respective institutional review boards, and all patients provided written informed consent prior to participating in the study. The study was conducted under the principles of the World Medical Association, Declaration of Helsinki, and Good Clinical Practice in accordance with International Conference on Harmonisation guidelines.
Study population
Eligible patients were men (ages ≥18 years) with histologically or cytologically confirmed adenocarcinoma of the prostate without neuroendocrine differentiation or small cell features. Patients had castration-resistant disease and either continued their androgen deprivation therapy with gonadotropin-releasing hormone analog or had undergone bilateral orchiectomy and were required to have a serum testosterone level of <50 ng/dL. An Eastern Cooperative Oncology (ECOG) performance status of 0 to 1 and estimated life expectancy of at least 6 months were required. Patients were required to have an absolute neutrophil count ≥1,500/μL, platelet count ≥100,000/μL, and hemoglobin ≥5.6 mmol/L (9 g/dL) at their screening visit. Patients were ineligible for enrollment if there was evidence of brain metastasis or active leptomeningeal disease; they had a history of or predisposition to seizure; they had any other malignancy within the last 5 years except nonmelanomatous skin cancer; they were previously treated with docetaxel-based chemotherapy; they had received palliative radiotherapy for bone metastases less than 2 weeks prior to initiation of study therapy; or they had received treatment with potent cytochrome P450 (CYP)–3A4 or CYP3A5 inhibitors or inducers within 4 weeks of starting the study. Furthermore, patients were ineligible if they had clinically significant cardiovascular disease, including myocardial infarction or uncontrolled angina within 6 months of enrollment; the presence or history of New York Heart Association class III or IV congestive heart failure (unless a screening echocardiogram or multigated acquisition scan performed within 3 months demonstrated a left ventricular ejection fraction ≥45%); a history of clinically significant ventricular arrhythmias (e.g., ventricular tachycardia, ventricular fibrillation, torsades de pointes); a history of Mobitz type II second- or third-degree heart block without a permanent pacemaker; hypotension (systolic blood pressure [BP] <86 mm Hg on two consecutive measurements); bradycardia (heart rate <50 beats per minute on electrocardiogram [ECG]); or uncontrolled hypertension (systolic BP >170 mm Hg or diastolic BP >105 mm Hg).
Study treatments
Docetaxel (75 mg/m2) was administered by constant rate, 1-hour intravenous infusion once on day 1 of each 21-day cycle. Study visits were on days 1, 2, 8, and 15 of cycles 1 and 2 and on days 1 and 15 of subsequent cycles. Patients received premedication with dexamethasone (8 mg by mouth) at 12, 3, and 1 hours before the start of each docetaxel infusion and 5 mg prednisone twice daily for as long as docetaxel treatment continued. Oral enzalutamide (160 mg/day) was administered daily starting on day 2 of the docetaxel cycle 1 (treatment cycles defined as 21-day cycles of docetaxel therapy). Treatment with docetaxel and enzalutamide or enzalutamide alone was continued indefinitely until unacceptable toxicity, initiation of another cytotoxic or investigational agent, or discontinuation at the investigator’s discretion.
Per protocol, the docetaxel dose could be reduced from 75 to 60 mg/m2 for cases of febrile neutropenia, neutrophils <500 cells/mm3 for at least 1 week, severe or cumulative cutaneous reactions, or moderate neurosensory signs or symptoms (or both); if these continued, docetaxel therapy was discontinued. Docetaxel was not given to patients with total bilirubin levels greater than the upper limit of normal (ULN) or with aspartate aminotransferase or alanine aminotransferase >1.5 × ULN concurrently with alkaline phosphatase >2.5 × ULN. Patients were allowed to stop and then restart docetaxel at any time following cycle 2. Growth factor support was allowed per standard of care and institutional guidelines. Patients who discontinued docetaxel for any reason, including patient preference, could continue with enzalutamide monotherapy.
Dose reductions of enzalutamide to 80 mg/day were allowed at the investigator’s discretion with the approval of the medical monitor.
Safety assessments
Safety and tolerability were determined by assessment of adverse events, concomitant medications, physical examinations, ECOG performance status, 12-lead ECGs, vital signs, and safety laboratory assessments on days 1, 2, 8, and 15 during cycles 1 and 2 and on days 1 and 15 for all subsequent cycles (Supplementary Fig. S1). The safety population included all patients who received at least one dose of enzalutamide, docetaxel, or both. Patients receiving enzalutamide monotherapy after discontinuing the combination regimen were evaluated for safety every 3 months. A final follow-up safety visit was performed 30 days after the last dose of enzalutamide. Severity grade of abnormal laboratory values was classified using the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. Safety was assessed during the combination therapy (docetaxel + enzalutamide) window (defined as the period of time starting on the date of docetaxel dose + 30 days) and the post-docetaxel enzalutamide time window.
PSA assessments
Serum PSA concentration was determined at baseline. Although not specified in the protocol, if postbaseline PSA values were assayed as part of the standard of care, the data were collected from the medical records for exploratory analyses. Exploratory analyses included individual percentage PSA change from baseline to nadir, proportion of patients with 50% PSA responses, proportion of patients with 90% PSA responses, duration of PSA response, and mean and median PSA changes from baseline.
PK assessments
Plasma samples for docetaxel and enzalutamide PK assessments were obtained in cycle 1 (before initiation of enzalutamide dosing) and cycle 2 (after approximately 21 consecutive days of enzalutamide dosing; Supplementary Fig. S1). Docetaxel PK samples were collected preinfusion and at 0.5, 1, 1.5, 2, 4, 8, and 24 hours after the start of the docetaxel infusions. Enzalutamide predose (minimum plasma concentration [Cmin]) PK samples were collected on day 1 of cycle 1 and cycle 2 (Supplementary Fig. S1). Validated, sensitive, liquid chromatography with tandem mass spectrometry methods were used to measure plasma concentrations of docetaxel, enzalutamide, and the major human metabolites of enzalutamide, N-desmethyl enzalutamide (an active metabolite) and a carboxylic acid metabolite (an inactive metabolite). The lower limit of quantification was 5.0 ng/mL for docetaxel and 0.020 μg/mL for enzalutamide and its metabolites. Docetaxel PK parameters (with and without concomitant enzalutamide therapy) included maximum plasma concentration (Cmax), area under the plasma concentration time curve (AUC) from time zero to last measurable plasma concentration (AUClast), and AUC from time zero extrapolated to infinite time (AUCinf); these measurements were used to assess the potential effect of enzalutamide treatment on docetaxel PK. Docetaxel PK parameters were calculated from plasma time–concentration data using standard noncompartmental methods in Phoenix WinNonlin version 5.2 (Pharsight Corporation) and SAS version 9.1.3 (SAS Institute). Plasma concentration data for enzalutamide were summarized by descriptive statistics and compared with historical data for enzalutamide as a single agent.
The PK full analysis population (N = 22) included all patients who received docetaxel with at least one plasma concentration determination. The PK evaluable population (n = 18) was defined as all enrolled patients who received an uninterrupted infusion of docetaxel (75 mg/m2) in cycles 1 and 2, received enzalutamide (160 mg/day) without interruption from day 2 of cycle 1 to day 1 of cycle 2, and had sufficient PK samples for calculation of at least one PK parameter (Cmax, AUClast, or AUCinf) for at least one cycle. Assessment of potential effects of enzalutamide on docetaxel PK involved patients in the PK evaluable population who had reportable values for Cmax, AUClast, and AUCinf for both cycles 1 and 2 (i.e., reference and test treatments, respectively).
Statistical analysis
A planned sample size of approximately 18 patients who could receive at least two full doses of docetaxel was considered sufficient to evaluate safety, tolerability, and PK. As a small phase 1b study with endpoints of safety and PK and without cross-cohort comparisons or efficacy endpoints, the sample size was based on clinical and regulatory considerations and had no formal statistical testing. Dosing, adverse events, and baseline patient characteristics were summarized using descriptive statistics.
The intention-to-treat (ITT) population included all enrolled patients, whereas the modified ITT (mITT) population consisted of all enrolled patients who received at least one dose of enzalutamide and had a baseline and at least one postbaseline PSA value. Analyses of patient baseline demographics, disease factors, disease characteristics, prior therapies for prostate cancer, concomitant medications, and measurements of treatment compliance throughout the study were performed using the safety population (N = 22). PSA evaluations were performed using the mITT population (n = 20), which excluded two patients (one who did not receive enzalutamide and another lacking a postbaseline PSA value).
To assess any potential effect of enzalutamide on docetaxel PK, a linear mixed-effects model, with fixed effects for treatment period and measurements within patient as repeated measures, was performed on natural logarithmic-transformed Cmax, AUClast, and AUCinf values of docetaxel. Point estimates and 90% confidence intervals (CIs) for the treatment differences (test minus reference) on the natural logarithmic scale were exponentiated to obtain estimates for ratios of geometric means (test/reference) on the original scale.
Results
Patients
The first patient enrolled on January 22, 2012. A total of 22 patients were enrolled (10 at MSKCC and 12 at Virginia Oncology Associates). All 22 patients received study treatment with docetaxel, 21 of whom also received enzalutamide (one patient suffered a serious adverse event of acute coronary syndrome during the first docetaxel infusion and discontinued the study before receiving enzalutamide). As of the data cutoff date (July 1, 2013), 10 patients (45.5%) remained on study, and 12 patients (54.5%) had discontinued owing to disease progression (eight patients), adverse events (two patients), death on study (one patient), and withdrawn consent (one patient).
Demographics and baseline disease characteristics
Patient baseline demographic and disease characteristics are shown in Table 1. At study enrollment, all patients had received at least one type of hormonal therapy for prostate cancer, most commonly leuprolide (86.4%) and/or bicalutamide (68.2%). Most patients (72.7%) had prior therapy for localized disease (typically prostatectomy and/or external beam radiation therapy) and had received a median of two prior systemic therapies. Five (22.7%) patients had received prior abiraterone. In addition, seven patients (31.8%) were treated with a bone-targeting agent (denosumab) and seven patients (31.8%) were treated with an experimental therapy (investigational drug). One patient (4.5%) was treated with the antineoplastic agents carboplatin, estramustine, and paclitaxel approximately 11 years before enrollment; one patient (4.5%) was treated with temsirolimus approximately 2.5 years before enrollment. Of note, patients treated at MSKCC were older (median age 76 years vs. 68.5 years) and had received more prior radiation (90.0% vs. 41.7%) and prior systemic therapies (median 3.5 vs. 2) than patients treated at Virginia Oncology Associates.
Table 1.
Demographics and baseline disease characteristics
| Characteristics | Site 1a (n = 10) | Site 2b (n = 12) | All patients (N = 22) |
|---|---|---|---|
| Median age (range), years | 76.0 (46.0–85.0) | 68.5 (47.0–75.0) | 70.5 (46.0–85.0) |
| ≥75 years, n (%) | 6 (60.0) | 1 (8.3) | 7 (31.8) |
| Race, n (%) | |||
| Black or African American | 0 | 3 (25.0) | 3 (13.6) |
| White | 10 (100.0) | 9 (75.0) | 19 (86.4) |
| Ethnicity, n (%) | |||
| Not Hispanic or Latino | 10 (100.0) | 12 (100.0) | 22 (100.0) |
| ECOG performance status 0, n (%) | 4 (40.0) | 2 (16.7) | 6 (27.3) |
| ECOG performance status 1, n (%) | 6 (60.0) | 10 (83.3) | 16 (72.7) |
| Median weight (range), kg | 77.3 (66.0–102.4) | 90.3 (75.3–106.1) | 86.5 (66.0–106.1) |
| Median body mass index (range), kg/m2 | 24.5 (21.7–34.8) | 28.2 (23.7–35.0) | 26.9 (21.7–35.0) |
| Gleason score 8–10, n (%) | 7 (70.0) | 8 (66.7) | 15 (68.2) |
| Median PSA (range), ng/mL | 57.1 (1.8–527.5) | 58.8 (1.9–585.0) | 57.9 (1.8–585.0) |
| Median hemoglobin (range), g/L | 130.0 (117.0–140.0) | 120.0 (98.0–148.0) | 125.0 (98.0–148.0) |
| Median alkaline phosphatase (range), U/L | 80.5 (45.0–547.0) | 112.0 (51.0–1432.0) | 90.5 (45.0–1432.0) |
| Prior opiate use, n (%) | 1 (10.0) | 7 (58.3) | 8 (36.4) |
| Prior therapy for localized disease, n (%) | |||
| Prostatectomy | 4 (40.0) | 3 (25.0) | 7 (31.8) |
| Transurethral resection of the prostate | 1 (10.0) | 1 (8.3) | 2 (9.1) |
| External beam radiotherapy | 9 (90.0) | 5 (41.7) | 14 (63.6) |
| Brachytherapy | 0 | 1 (8.3) | 1 (4.5) |
| Visceral disease at screening, n (%) | |||
| Lung | 0 | 2 (16.7) | 2 (9.1) |
| Liver | 0 | 2 (16.7) | 2 (9.1) |
| Median time from initial diagnosis (range), mo | 73.9 (15.2–209.0) | 45.7 (4.0–141.3) | 64.7 (4.0–209.0) |
| Median no. of prior systemic therapies (range)c | 3.5 (2–8) | 2 (1–4) | 2 (1–8) |
NOTE: Percentages are based on number of patients in the safety population.
MSKCC.
Virginia Oncology Associates.
Prior therapy data provided by the study sites.
Drug treatment and compliance
The median duration of treatment for the combination regimen was 3.9 months (range, 0–10.6), and median duration of post-docetaxel enzalutamide therapy was 5.6 months (range, 0.3–15.1). The median number of docetaxel cycles was 5.0 (range, 1.0–13.0). Median exposure to enzalutamide following cessation of docetaxel was 12.0 months (range, 0.2–17.2). Patients treated at Virginia Oncology Associates received more docetaxel (median of six vs. three cycles) and post-docetaxel enzalutamide (median of 13.6 vs. 5.9 months) than patients at MSKCC, a finding that may at least in part be explained by the demographic differences (prior section) showing patients treated at Virginia Oncology Associates were younger and had received less prior therapy than patients treated at MSKCC. Patients at Virginia Oncology Associates were also more likely to receive filgrastim (12/12) than patients at MSKCC (1/10), which may have also influenced the amount of study drug received.
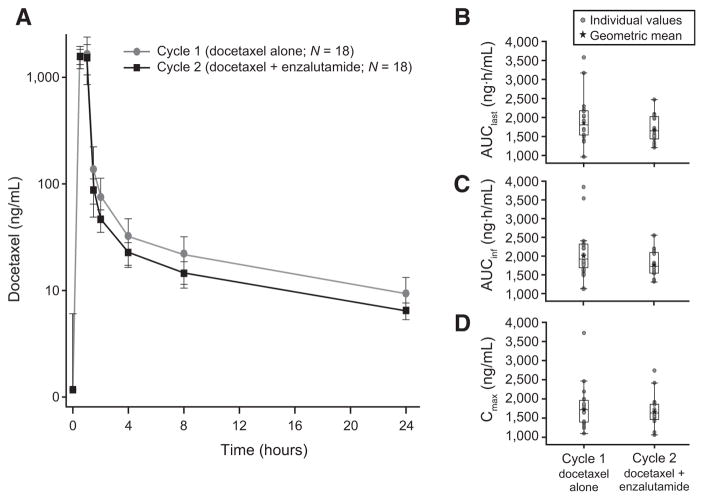
Pharmacokinetic parameters
Mean docetaxel PK parameters are shown in Table 2 and Fig. 1. The adjusted geometric mean ratios for docetaxel AUClast, AUCinf, and Cmax for cycle 2 relative to cycle 1 were 0.904 (90% CI, 0.782–1.04), 0.882 (90% CI, 0.767–1.02), and 0.963 (90% CI, 0.834–1.11), respectively. Thus, geometric mean docetaxel exposure (AUCinf) decreased by 11.8% and peak concentration (Cmax) decreased by 3.7% with concurrent enzalutamide and docetaxel administration versus docetaxel alone.
Table 2.
Plasma docetaxel PK parameters in cycles 1 and 2
| PK parameter | n | Adjusted geometric mean
|
Ratio (Test/reference) | 90% CI | |
|---|---|---|---|---|---|
| Cycle 2 (Test) | Cycle 1 (Reference) | ||||
| AUClast (ng·h/mL) | 18 | 1670 | 1850 | 0.904 | (0.782–1.04) |
| AUCinf (ng·h/mL) | 18 | 1770 | 2000 | 0.882 | (0.767–1.02) |
| Cmax (ng/mL) | 18 | 1660 | 1730 | 0.963 | (0.834–1.11) |
NOTE: Cycle 1, docetaxel alone; cycle 2, docetaxel plus enzalutamide.
Figure 1.
Individual and mean docetaxel PK by treatment cycle. A, mean ± SD plasma docetaxel concentration in cycle 1 (docetaxel alone) and cycle 2 (with enzalutamide administration). Insets show individual values and geometric mean for docetaxel (B) AUClast, (C) AUCinf, and (D) Cmax. Box plots indicate median and 25%/75% quartiles with whiskers to the last point within 1.5 times the interquartile range.
In treatment cycle 2, mean (standard deviation [SD]) predose Cmin concentration of enzalutamide was 10.6 (2.21) μg/mL, N-desmethyl enzalutamide was 7.79 (2.92) μg/mL, the sum of enzalutamide plus N-desmethyl enzalutamide was 18.3 (4.11) μg/mL, and the carboxylic acid metabolite was 3.70 (2.08) μg/mL. The mean enzalutamide concentration was similar to the mean steady-state Cmin value observed in patients with mCRPC in the phase III AFFIRM trial (11).
Safety
The safety analysis was conducted on the full patient population (N = 22), of whom 21 patients received both enzalutamide and docetaxel. The assessment of safety distinguished adverse events starting during the time patients received docetaxel and enzalutamide versus the time patients received post-docetaxel enzalutamide. As mentioned above, the median duration of combination therapy was 3.9 months, and the median duration of post-docetaxel enzalutamide was 5.6 months. Treatment-emergent adverse events reported in at least 10.0% of patients are shown in Table 3.
Table 3.
Treatment-emergent adverse events (reported in ≥10.0% of patients)
| Adverse event, n (%) | Combination therapya (n = 22)
|
Post-docetaxel enzalutamideb (n = 21)
|
||||
|---|---|---|---|---|---|---|
| All grades | Grade 3 | Grade 4 | All grades | Grade 3 | Grade 4 | |
| Blood and lymphatic system disorders | ||||||
| Neutropenia | 19 (86.4) | 2 (9.1) | 17 (77.3) | 1 (4.8) | 1 (4.8) | 0 |
| Febrile neutropenia | 4 (18.2) | 3 (13.6) | 1 (4.5) | 0 | 0 | 0 |
| Anemia | 4 (18.2) | 1 (4.5) | 0 | 1 (4.8) | 0 | 0 |
| General disorders and administration site conditions | ||||||
| Fatigue | 17 (77.3) | 0 | 0 | 4 (19.0) | 0 | 0 |
| Pain | 4 (18.2) | 0 | 0 | 0 | 0 | 0 |
| Asthenia | 3 (13.6) | 0 | 0 | 2 (9.5) | 0 | 0 |
| Nervous system disorders | ||||||
| Neuropathy peripheral | 9 (40.9) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Peripheral sensory neuropathy | 7 (31.8) | 1 (4.5) | 0 | 3 (14.3) | 0 | 0 |
| Dysgeusia | 5 (22.7) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Dizziness | 4 (18.2) | 0 | 0 | 0 | 0 | 0 |
| Peripheral motor neuropathy | 3 (13.6) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Headache | 3 (13.6) | 0 | 0 | 0 | 0 | 0 |
| Gastrointestinal disorders | ||||||
| Nausea | 8 (36.4) | 0 | 0 | 0 | 0 | 0 |
| Constipation | 7 (31.8) | 0 | 0 | 5 (23.8) | 0 | 0 |
| Diarrhea | 7 (31.8) | 0 | 0 | 0 | 0 | 0 |
| Dyspepsia | 4 (18.2) | 0 | 0 | 0 | 0 | 0 |
| Abdominal pain | 3 (13.6) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Stomatitis | 3 (13.6) | 0 | 0 | 0 | 0 | 0 |
| Metabolism and nutrition disorders | ||||||
| Decreased appetite | 6 (27.3) | 0 | 0 | 4 (19.0) | 0 | 0 |
| Dehydration | 3 (13.6) | 0 | 0 | 1 (4.8) | 1 (4.8) | 0 |
| Musculoskeletal and connective tissue disorders | ||||||
| Arthralgia | 6 (27.3) | 0 | 0 | 3 (14.3) | 1 (4.8) | 0 |
| Back pain | 6 (27.3) | 0 | 0 | 3 (14.3) | 0 | 0 |
| Musculoskeletal pain | 3 (13.6) | 0 | 0 | 4 (19.0) | 1 (4.8) | 0 |
| Musculoskeletal chest pain | 3 (13.6) | 0 | 0 | 2 (9.5) | 0 | 0 |
| Pain in extremity | 3 (13.6) | 0 | 0 | 0 | 0 | 0 |
| Flank pain | 3 (13.6) | 1 (4.5) | 0 | 1 (4.8) | 1 (4.8) | 0 |
| Respiratory, thoracic, and mediastinal disorders | ||||||
| Dyspnea | 6 (27.3) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Dyspnea exertional | 4 (18.2) | 0 | 0 | 0 | 0 | 0 |
| Skin and subcutaneous disorders | ||||||
| Alopecia | 6 (27.3) | 0 | 0 | 0 | 0 | 0 |
| Rash | 3 (13.6) | 0 | 0 | 2 (9.5) | 0 | 0 |
| Nail disorder | 3 (13.6) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Eye disorders | ||||||
| Lacrimation increased | 5 (22.7) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Investigations | ||||||
| White blood cell count decreased | 4 (18.2) | 3 (13.6) | 1 (4.5) | 1 (4.8) | 0 | 0 |
| Renal and urinary disorders | ||||||
| Pollakiuria | 3 (13.6) | 0 | 0 | 1 (4.8) | 0 | 0 |
| Psychiatric disorders | ||||||
| Insomnia | 3 (13.6) | 0 | 0 | 0 | 0 | 0 |
NOTE: Percentages are based on the number of patients in the safety population (N).
Starting the day of each docetaxel infusion to 30 days after the infusion.
From day 1 to 30 days after last enzalutamide dose, excluding the combination therapy window.
The most common any grade adverse events observed on the combination regimen (N = 22), regardless of causality and reported in five or more patients (22.7%), were neutropenia (86.4%), fatigue (77.3%), peripheral neuropathy (40.9%), nausea (36.4%), constipation (31.8%), diarrhea (31.8%), peripheral sensory neuropathy (31.8%), alopecia (27.3%), arthralgia (27.3%), back pain (27.3%), decreased appetite (27.3%), dyspnea (27.3%), dysgeusia (22.7%), and increased lacrimation (22.7%). In the post-docetaxel enzalutamide cycle (n = 21), the most common adverse events noted in three or more patients (≥14.3%) were constipation (23.8%), decreased appetite (19.0%), fatigue (19.0%), musculoskeletal pain (19.0%), arthralgia (14.3%), back pain (14.3%), and peripheral sensory neuropathy (14.3%).
Nearly all (95.5%) patients on the combination regimen reported at least one grade 3 or higher adverse event. The most common was neutropenia (19 [86.4%] patients). Other grade 3 or higher adverse events included febrile neutropenia and decreased white blood cell count (each reported in four [18.2%] patients), decreased blood phosphorus (two [9.1%] patients), and the following in one (4.5%) patient each: anemia, acute coronary syndrome, death, sepsis, ECG QT prolonged, flank pain, peripheral sensory neuropathy, and hematuria. Of the 19 patients reported to have a grade 3 or higher adverse event of neutropenia, 18 had their first grade 3 or higher neutropenia event during cycles 1 or 2 of docetaxel. Three of four patients with febrile neutropenia had these events during cycle 1 or 2 of docetaxel treatment.
Reasons for docetaxel discontinuations are listed in Supplementary Table S1; none were assessed by investigators as related to enzalutamide treatment. The most common reason for discontinuing docetaxel was peripheral neuropathy. One patient, who had grade 1 sensory neuropathy at baseline, discontinued docetaxel after two cycles after developing grade 3 sensory neuropathy. All other patients who discontinued docetaxel due to peripheral neuropathy received at least four cycles of docetaxel. Overall, of the 16 patients who reported any peripheral neuropathy with the combination, nine had their first occurrence of neuropathy after receiving at least four cycles of docetaxel.
Treatment-emergent adverse events led to temporary enzalutamide dose interruption in three of 22 (13.6%) patients receiving combination therapy (maculopapular rash, ECG QT prolonged, and febrile neutropenia) and in two of 21 (9.5%) patients receiving post-docetaxel enzalutamide (decreased appetite and pneumonia); however, no enzalutamide dose reductions were required in either group. Two of 22 patients (9.1%) permanently discontinued enzalutamide due to adverse events (one death due to unknown cause [described below], one acute coronary syndrome).
Eleven patients (50.0%) experienced one or more serious adverse event during the trial. Treatment-emergent serious adverse events were reported in 36.4% (during combination therapy) and 23.8% (during post-docetaxel enzalutamide therapy) of patients. During combination therapy, serious adverse events were reported for three patients with febrile neutropenia, two with acute coronary syndrome, and one each with pyrexia, sepsis, decreased white blood cell count, flank pain, hematuria, and maculopapular rash. One patient died on study due to an unknown cause (described below), and one died due to disease progression after discontinuing study treatment.
During post-docetaxel enzalutamide therapy, two patients (9.5%) were reported to have serious adverse events of atrial fibrillation, and one patient (4.8%) each had serious adverse events of asthenia, pyrexia, hepatic failure, pneumonia, sepsis, septic shock, fall, ECG QT prolonged, dehydration, cerebral hemorrhage, and deep vein thrombosis. All serious adverse events reported during post-docetaxel enzalutamide therapy were assessed as unrelated to enzalutamide.
The sole patient death on study occurred during the combination therapy cycle in a 77-year-old white male who had received bicalutamide, leuprolide, nilutamide, ketoconazole, abiraterone, and prednisone for prior treatment of prostate cancer. At study entry, the patient had metastases to the lymph nodes and two to four lesions on bone scan, with ongoing fatigue, sensory neuropathy, and bilateral hip pain, and an ECOG performance status of 0. On day 8, cycle 1 of docetaxel treatment and 6 days after initiation of enzalutamide therapy, the patient was discovered to have died due to an unknown cause. Autopsy was declined by the family. The investigator considered this death to be possibly related to the combination regimen of enzalutamide and docetaxel.
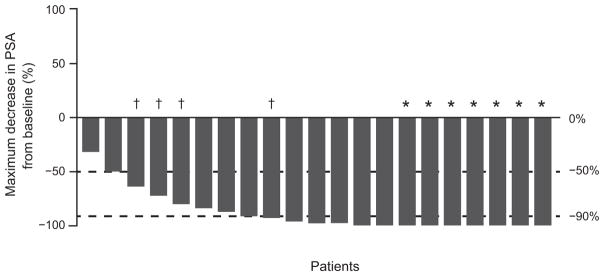
PSA assessments
At baseline, the median (SD) PSA in the mITT population (n = 20) was 57.9 μg/L (range, 1.8–585.0). Patients had a median percentage change from baseline to nadir of −96.8 (range, −100.0 to −31.4). The percentage change in PSA from baseline to nadir for all patients is shown in Fig. 2. A reduction of ≥50% from baseline in PSA was observed in 19 of 20 (95.0%) patients, with a median duration of 226 days. A ≥90% reduction occurred in 13 of 20 (65.0%) patients, with a median duration of 226 days.
Figure 2.
Percentage change in PSA from baseline to nadir. †, Patients had a ≥99.5% decrease in PSA. *, Patients had received prior abiraterone.
Discussion
The primary objectives of this phase Ib study were to assess the safety, tolerability, and PK of docetaxel when administered in combination with enzalutamide in men with advanced prostate cancer. The PK analyses showed no significant drug–drug interaction for the combination regimen. This contrasts with a previous clinical study in which enzalutamide reduced plasma exposure to orally-administered midazolam (a CYP3A4 substrate) by 86%, which led to the drug being classified as a strong inducer of CYP3A4 (11).
Docetaxel is also cleared by CYP3A4/5-dependent pathways (12, 13). However, because docetaxel is a high-extraction ratio drug and is administered intravenously, it was expected to be less susceptible to CYP3A4 enzyme induction effects. The finding that the geometric mean docetaxel exposure (AUCinf) decreased by 11.8% and peak concentrations (Cmax) by 3.7% when docetaxel and enzalutamide were given concomitantly confirms a modest effect of metabolism relative to single-agent therapy with docetaxel alone. This small effect of enzalutamide on docetaxel PK was expected based on PK principles and is not considered clinically meaningful.
The most common adverse events associated with the combination were those already identified with either single agent. Nearly all patients treated with the combination reported at least one grade 3 or higher adverse event, with events related to myelosuppression being the most common (neutropenia [86.4%], febrile neutropenia [18.2%], and decreased white blood cell count [18.2%]). All other grade 3 events were reported in two or fewer patients.
The incidence of grade 3 or higher neutropenia (86.4%) and febrile neutropenia (18.2%) in this study is higher than reported in the TAX 327 study (32% and 3%, respectively; ref.2). The reasons for this are unclear. It is possible that some of this was due to detection bias, as counts were checked on a weekly basis in this protocol, rather than every 3 weeks on the day of treatment as is standard practice, and therefore an excess degree of neutropenia could have been detected. Yet, a higher rate of neutropenic fever was clearly not only a laboratory detection issue. The PK analysis of this study does not demonstrate a significant drug–drug interaction for the combination regimen, but that does not rule out the possibility that the combination of docetaxel and enzalutamide is associated with more neutropenia than either drug alone. Physicians are cautioned that neutropenic fever can occur more commonly in patients receiving the combination of docetaxel plus enzalutamide. A larger randomized trial would be needed to better confirm whether the safety profile of enzalutamide plus docetaxel differs from that of docetaxel alone.
It should be noted that the median of 5.0 docetaxel cycles received in this study was lower than in the TAX 327 study (median of 9.5 cycles; ref.2), but it was comparable to the median number of docetaxel cycles received in other combination studies of docetaxel with noncytotoxic therapies such as dasatinib (six cycles; ref.14) and atrasentan (five cycles; ref.15). The reason for the higher median number of docetaxel cycles administered in the TAX 327 study as compared with the current study and other phase I–II studies is not clear, but in this study patients had the option of discontinuing docetaxel therapy after two cycles and continuing on enzalutamide monotherapy. Notably, enzalutamide was not available commercially or on other studies in the United States during the study enrollment period, and registration in this trial allowed for access to enzalutamide, providing that patients were willing to undergo two cycles of chemotherapy. It is not clear whether the relatively low number of docetaxel cycles received was due to toxicity of this regimen or patient/physician choice.
Treatment with enzalutamide and docetaxel resulted in PSA declines in almost all patients in this study. Of the 20 patients treated with docetaxel in the mITT population, 19 (95%) had a ≥50% reduction in PSA with a median duration of 226 days (approximately 7.4 months). The 95% PSA response rate (≥50% reduction in PSA) observed in this study was higher than the 45% PSA response rate reported in the TAX 327 study (1). The PSA response rate (≥50% reduction in PSA) with enzalutamide was 78% in the PREVAIL phase III trial of enzalutamide in patients with chemotherapy-naïve mCRPC (5).
These PSA data should be interpreted with caution due to the small sample size and the open-label, nonrandomized study design with no comparator. The study’s results do, however, suggest that enzalutamide and docetaxel may be coadministered safely at their standard doses and schedules in patients with mCRPC who are eligible for chemotherapy. However, clinicians should be attentive to the possibility of an increased rate of neutropenic fever. These data should prompt clinicians to consider carefully patient selection for this regimen and the use of growth factor support as primary prophylaxis particularly in patients who are frail or have prior extensive treatment histories that may compromise bone marrow reserve. The combination of docetaxel and enzalutamide may be an effective therapeutic option in mCRPC and warrants further study in a larger population with a particular focus on response and developing strict guidelines for prophylactic use of growth factor support. Future studies will also evaluate enzalutamide combined with other prostate cancer drugs and its use in earlier stages of disease.
Supplementary Material
Translational Relevance.
Docetaxel combined with prednisone was approved for treatment of metastatic castration-resistant prostate cancer (mCRPC) in 2004. Enzalutamide is an androgen receptor (AR) inhibitor that improves overall survival and radiographic progression-free survival in mCRPC both before and after docetaxel administration. Preclinical data suggest that docetaxel and enzalutamide inhibit AR translocation and signaling. As enzalutamide plus docetaxel may be a desirable combination therapy, we performed a phase Ib study to evaluate the safety, tolerability, and pharmacokinetics of docetaxel when administered with enzalutamide in docetaxel-naïve men with mCRPC. Small reductions in plasma exposure to docetaxel occurred with concurrent treatment, which were not clinically meaningful. The treatment was safe overall, but the rates of neutropenia and neutropenic fever were higher than expected. Prostate-specific antigen level decreases were seen in almost all patients. Further development of the combination of docetaxel and enzalutamide is planned.
Acknowledgments
Grant Support
This study was supported by the Medivation, Inc., and Astellas Pharma, Inc., the co-developers of enzalutamide.
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Disclosure of Potential Conflicts of Interest
M.J. Morris is a consultant/advisory board member for Astellas, Bayer, Millennium, Progenics, and Tokai. H.I. Scher reports receiving speakers bureau honoraria from Chagai Academy for Advanced Oncology, is a consultant/ advisory board member for Astellas, AstraZeneca, BIND Pharmaceuticals, Bristol-Myers Squibb, Celegene, Endocyte, Exelixis, Ferring Pharmaceuticals, Genentech, Janssen, Medivation, Novartis, Pfizer, Roche, Sanofi Aventis, Takeda Millennium, WCG Oncology and Ventana, and reports receiving commercial research grants from Mediavation. M.T. Fleming reports receiving speakers bureau honoraria from Medivation/Astellas. No potential conflicts of interest were disclosed by the other authors.
Authors’ Contributions
Conception and design: M.J. Morris, J.A. Gibbons, A.C. Peterson, T. Ouatas, M.T. Fleming
Development of methodology: M.J. Morris, J.A. Gibbons, A.C. Peterson, Z. Khondker, T. Ouatas, M.T. Fleming
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): M.J. Morris, D.E. Rathkopf, W. Novotny, H.I. Scher, M.T. Fleming
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): M.J. Morris, W. Novotny, J.A. Gibbons, A.C. Peterson, Z. Khondker, T. Ouatas, M.T. Fleming
Writing, review, and/or revision of the manuscript: M.J. Morris, D.E. Rathkopf, W. Novotny, J.A. Gibbons, A.C. Peterson, T. Ouatas, H.I. Scher, M.T. Fleming
Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): M.J. Morris, J.A. Gibbons, Z. Khondker, T. Ouatas, H.I. Scher
Study supervision: M.J. Morris, W. Novotny, A.C. Peterson, Z. Khondker, M.T. Fleming
References
- 1.TAXOTERE ® [package insert] Sanofi-Aventis U.S; Nov, 2014. [Accessed February 29, 2016]. Available from: http://products.sanofi.us/Taxotere/taxotere.html. [Google Scholar]
- 2.Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 3.Tran C, Ouk S, Clegg NJ, Chen Y, Watson PA, Arora V, et al. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science. 2009;324:787–90. doi: 10.1126/science.1168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scher HI, Beer TM, Higano CS, Anand A, Taplin ME, Efstathiou E, et al. Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1–2 study. Lancet. 2010;375:1437–46. doi: 10.1016/S0140-6736(10)60172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33. doi: 10.1056/NEJMoa1405095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 7.Zhu ML, Horbinski CM, Garzotto M, Qian DZ, Beer TM, Kyprianou N. Tubulin-targeting chemotherapy impairs androgen receptor activity in prostate cancer. Cancer Res. 2010;70:7992–8002. doi: 10.1158/0008-5472.CAN-10-0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darshan MS, Loftus MS, Thadani-Mulero M, Levy BP, Escuin D, Zhou XK, et al. Taxane-induced blockade to nuclear accumulation of the androgen receptor predicts clinical responses in metastatic prostate cancer. Cancer Res. 2011;71:6019–29. doi: 10.1158/0008-5472.CAN-11-1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thadani-Mulero M, Nanus DM, Giannakakou P. Androgen receptor on the move: boarding the microtubule expressway to the nucleus. Cancer Res. 2012;72:4611–5. doi: 10.1158/0008-5472.CAN-12-0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Leeuw R, Berman-Booty LD, Schiewer MJ, Ciment SJ, Den RB, Dicker AP, et al. Novel actions of next-generation taxanes benefit advanced stages of prostate cancer. Clin Cancer Res. 2015;21:795–807. doi: 10.1158/1078-0432.CCR-14-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibbons JA, Ouatas T, Krauwinkel W, Ohtsu Y, van der Walt JS, Beddo V, et al. Clinical pharmacokinetic studies of enzalutamide. Clin Pharmacokinet. 2015;54:1043–55. doi: 10.1007/s40262-015-0271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark SJ, Rivory LP. Clinical pharmacokinetics of docetaxel. Clin Pharmacokinet. 1999;36:99–114. doi: 10.2165/00003088-199936020-00002. [DOI] [PubMed] [Google Scholar]
- 13.Shou M, Martinet M, Korzekwa KR, Krausz KW, Gonzalez FJ, Gelboin HV. Role of human cytochrome P450 3A4 and 3A5 in the metabolism of taxotere and its derivatives: enzyme specificity, interindividual distribution and metabolic contribution in human liver. Pharmacogenetics. 1998;8:391–401. doi: 10.1097/00008571-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Araujo JC, Mathew P, Armstrong AJ, Braud EL, Posadas E, Lonberg M, et al. Dasatinib combined with docetaxel for castration-resistant prostate cancer: results from a phase 1–2 study. Cancer. 2012;118:63–71. doi: 10.1002/cncr.26204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong AJ, Creel P, Turnbull J, Moore C, Jaffe TA, Haley S, et al. A phase I-II study of docetaxel and atrasentan in men with castration-resistant metastatic prostate cancer. Clin Cancer Res. 2008;14:6270–6. doi: 10.1158/1078-0432.CCR-08-1085. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.