Abstract
We aimed to investigate whether the prognostic nutritional index (PNI), a combined nutritional-inflammatory score based on serum albumin levels and lymphocyte count, was associated with mortality in patients with acute ST-segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (pPCI). From September 2011 to November 2014, 309 consecutive patients with STEMI undergoing pPCI were prospectively enrolled. Patients with a combined score of albumin (g/L) + 5 × total lymphocyte count × 109/L ≥ 45 or <45 were assigned a PNI score of 0 or 1, respectively. Of the 309 STEMI patients, 24 (7.74%) died in the hospital, and 15 (4.83%) died during long-term follow-up (median follow-up time, 19.5 [3–36] months). Compared to patients with a PNI of 0, patients with a PNI of 1 had significantly higher in-hospital (14.2% vs. 3.7%; P < 0.001) and long-term follow-up (21.7% vs. 6.9%, P < 0.001) mortality rates. PNI (1/0, HR, 2.414; 95% CI, 1.016 to 5.736; P = 0.046) was a significant independent predictor of mortality in patients with STEMI undergoing pPCI. Moreover, cumulative survival was significantly lower for patients with a PNI of 1 compared to patients with a PNI of 0 (78.3% vs. 93.1%, log-rank P < 0.001). PNI appears useful for the risk stratification of STEMI patients undergoing pPCI.
Introduction
Despite recent advances in techniques and improved outcomes of percutaneous coronary intervention (PCI), patients with acute ST-segment elevation myocardial infarction (STEMI) are still at an increased risk of mortality even after timely revascularization1–4. Therefore, early risk stratification at the time of presentation is of clinical importance.
Malnutrition has been recognized as an independent risk factor for morbidity and mortality in patients with chronic heart failure (CHF)5, 6. Some single nutritional indices such as albumin have been shown to be closely associated with poor outcomes in patients with CHF7, 8. Additionally, to evaluate nutritional status, more complex indices, such as the prognostic nutritional index (PNI), have been developed and widely used9–13. The PNI is a combined nutritional-inflammatory score based on serum albumin levels and the lymphocyte count that reflects the immunological nutritional condition and that measures the risk of several types of cancer in patients14. This index is convenient to obtain since only simple blood biomarkers are required.
The prognostic influence of nutritional status in cardiovascular disease (CVD) is not very well understood. It seems that lower serum albumin levels are increased risk factors for coronary disease, which could, together with traditional risk factors, assist in confirming patients who are at risk of myocardial infarction (MI)8, 9. However, one study has shown that hypoalbuminemia was related to adverse events but not to mortality in patients with acute coronary syndrome. The impact of hypoalbuminemia on outcomes after STEMI has not been comprehensively investigated. Older patients may be especially vulnerable to haemodynamic changes, and we speculated that hypoalbuminemia and PNI may have markedly adverse effects on older patients with STEMI. Therefore, the aim of the present study was to examine whether the PNI on admission was associated with mortality in patients with acute STEMI undergoing pPCI.
Results
Between September of 2011 and November of 2014, we conducted a follow-up study at the Department of Cardiology, the First Affiliated Hospital of Xinjiang Medical University. A total of 324 consecutive patients who presented with acute STEMI within 12 hours of undergoing pPCI at our institution were enrolled. Among these patients, 15 patients were excluded from the final analysis according to our exclusion criteria. Thus, 309 patients were included in the final analysis; of these, 189 (61.2%) patients had a PNI of 0, and 120 (38.8%) patients had a PNI of 1on admission.
Patient baseline clinical characteristics by PNI score are shown in Table 1. Compared to patients with a PNI of 0, those with a PNI of 1 had an advanced age (P = 0.034), more often had a Killip class >2 (P = 0.004), had a higher GRACE score (P = 0.037), and had a lower LVEF (P = 0.002). Patient baseline biochemical characteristics by PNI score are shown in Table 2. Patients with a PNI of 1 had significantly lower blood albumin (P < 0.001), lower triglycerides (P < 0.001), lower total cholesterol (P = 0.014), lower haemoglobin levels (P < 0.001), and lower WBC counts (P = 0.025) compared with those with a PNI of 0.
Table 1.
Baseline clinical characteristics of patients with acute STEMI after pPCI by PNI score group.
| Variable | PNI = 0 (n = 189) | PNI = 1 (n = 120) | χ2/t | P |
|---|---|---|---|---|
| Age, years | 56 ± 12 | 62 ± 11 | −4.10 | 0.034 |
| Males, n (%) | 162 (85.7) | 88 (73.3) | 0.01 | 6.504 |
| Diabetes mellitus, n (%) | 46 (24.3) | 31 (25.8) | 0.03 | 0.872 |
| Hypertension, n (%) | 102 (54.0) | 51 (42.5) | 3.86 | 0.049 |
| Smoking, n (%) | 119 (63.0) | 64 (53.3) | 3.46 | 0.178 |
| Admission SBP, mmHg | 125 ± 19 | 120 ± 18 | 2.35 | 0.020 |
| Admission DBP, mmHg | 77 ± 14 | 73 ± 12 | 2.18 | 0.030 |
| Admission heart rate, beats/min | 79 ± 14 | 78 ± 13 | 0.69 | 0.490 |
| Killip class (class ≥2) | 23 (12.2) | 28 (23.3) | 13.16 | 0.004 |
| In-hospital medications | ||||
| Aspirin, n (%) | 189 (100) | 118 (98.3) | 1.11 | 0.292 |
| β-blockers, n (%) | 180 (95.2) | 115 (95.8) | 0.06 | 0.806 |
| ARB/ACEI, n (%) | 182 (96.3) | 112 (93.3) | 0.83 | 0.363 |
| CCB, n (%) | 83 (43.9) | 45 (37.5) | 0.99 | 0.319 |
| Tirofiban, n (%) | 184 (97.4) | 117 (97.5) | 0.006 | 0.937 |
| Medications at discharge | ||||
| Aspirin | 182 (96.3) | 116 (96.7) | 0.03 | 0.864 |
| Clopidogrel | 188 (99.5) | 119 (99.2) | 0.34 | 0.561 |
| ACEI/ARB | 155 (82.0) | 98 (81.7) | 0.01 | 0.939 |
| β-blockers | 170 (89.9) | 104 (86.6) | 4.56 | 0.033 |
| LVEF, % | 58.39 ± 6.29 | 55.95 ± 7.36 | 3.11 | 0.002 |
| Coronary artery disease, n (%) | ||||
| Left main | 13 (6.9) | 5 (4.2) | 0.55 | 0.458 |
| Left anterior descending | 146 (77.2) | 88 (73.3) | 0.42 | 0.518 |
| Left circumflex | 100 (52.9) | 61 (50.8) | 0.06 | 0.811 |
| Right coronary artery | 113 (59.8) | 76 (63.3) | 0.25 | 0.615 |
| Gensini score | 57.16 ± 34.50 | 58.51 ± 36.42 | 0.76 | 0.307 |
| GRACE score | 143 ± 25 | 149 ± 24 | 2.09 | 0.037 |
SBP, systolic blood pressure; DBP, diastolic blood pressure; ARB, angiotensin II receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; CCB, calcium-channel blocker; GRACE, the Global Registry of Acute Coronary Events; IABP, intra-aortic balloon pump counterpulsation; LVEF, left ventricular ejection fraction; PNI, prognostic nutritional index; STEMI, acute ST-segment elevation myocardial infarction.
Table 2.
Laboratory findings in STEMI patients after pPCI by PNI score group.
| Variable | PNI = 0 (n = 189) | PNI = 1 (n = 120) | χ2/t | P |
|---|---|---|---|---|
| WBC, ×109/L | 11.3 ± 3.64 | 10.3 ± 3.63 | 2.26 | 0.025 |
| Lymphocyte count, ×109/L | 2.34 ± 1.25 | 1.30 ± 0.57 | 8.58 | <0.001 |
| Neutrophil count, ×109/L | 8.03 ± 3.45 | 8.38 ± 3.75 | −0.84 | 0.40 |
| Mean platelet volume, ×1012/fL | 10.3 ± 1.2 | 10.6 ± 1.5 | −2.02 | 0.045 |
| RDW, % | 4.8 ± 0.56 | 4.4 ± 0.62 | −2.29 | 0.023 |
| Haemoglobin, g/L | 147 ± 17 | 133 ± 19 | 6.71 | <0.001 |
| Creatinine, μmol/L | 83.4 ± 42.09 | 85.5 ± 52.05 | −0.38 | 0.701 |
| Blood urea nitrogen, mmol/L | 5.2 ± 1.55 | 5.1 ± 2.33 | 0.36 | 0.722 |
| Triglycerides, mmol/L | 2.3 ± 1.78 | 1.4 ± 0.87 | 5.50 | <0.001 |
| Total cholesterol, mmol/L | 4.6 ± 1.01 | 4.3 ± 1.13 | 2.47 | 0.014 |
| Low-density lipoprotein cholesterol, mmol/L | 2.8 ± 0.80 | 2.8 ± 0.81 | 0.33 | 0.742 |
| Troponin T, ng/mL | 0.21 ± 0.66 | 0.23 ± 1.31 | −0.62 | 0.535 |
| CK, IU/L | 251 (99–910) | 418 (98–1495) | −0.99 | 0.319 |
| CK-MB, U/L | 28 (17–98) | 44 (19–144) | −1.19 | 0.233 |
| Serum albumin, g/dL | 40.8 ± 5.39 | 34.3 ± 4.66 | 10.10 | <0.001 |
| Urine protein positive, (%) | 33 (17.5) | 33 (27.5) | 4.40 | 0.036 |
WBC, white blood cell; RDW, red blood cell distribution; CK, creatinine kinase; CK-MB, creatinine kinase – myocardial band isoenzyme; PNI, prognostic nutritional index; STEMI, acute ST-segment elevation myocardial infarction.
Compared to PNI = 0 group, the PNI = 1 group had significantly higher in-hospital mortality (14.2% vs. 3.7%, P < 0.001; Fig. 1). Consistently, the PNI = 1 group showed significantly higher mortality (21.7% vs. 6.9%, P < 0.001) compared with the PNI = 0 group at long-term follow-up (median follow-up time, 19.5 [3–36] months).
Figure 1.
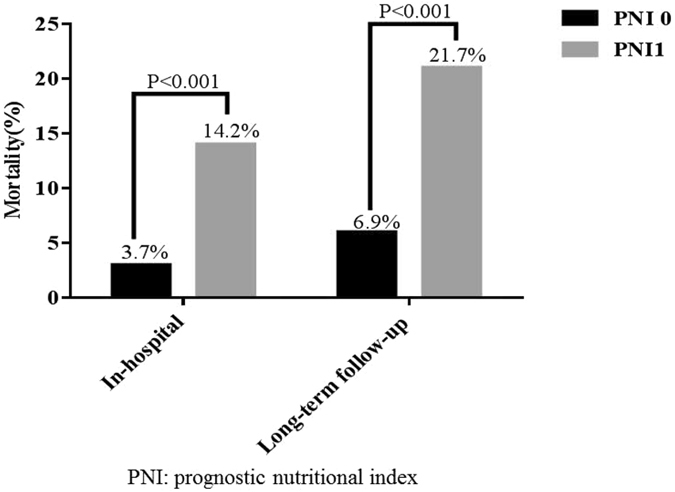
In-hospital and long-term follow-up mortality in the PNI = 0 and PNI = 1 groups of STEMI patients who underwent pPCI.
In univariate and multivariate analyses (Table 3), a greater PNI (1 vs. 0) on admission was a significant predictor of mortality (hazard ratio, 3.232 [95% confidence interval, 1.661–6.292], P = 0.001; and 2.414 [1.016–5.736], P = 0.046, respectively). Other multivariate independent predictors of mortality were age (hazard ratio, 1.064 [95% confidence interval, 1.027–1.102], P = 0.001), LVEF (hazard ratio, 0.931 [95% confidence interval, 0.890–0.974], P = 0.002), WBC count (hazard ratio, 1.203 [95% confidence interval, 1.118–1.294], P < 0.001) and GRACE score (hazard ratio, 1.038 [95% confidence interval, 1.002–1.074], P < 0.001). Moreover, cumulative survival was significantly lower in patients with a PNI of 1 relative to patients with a PNI of 0 (78.3% vs. 93.1%, respectively; log-rank P < 0.001) (Fig. 2).
Table 3.
Independent predictors of mortality in the Cox proportional hazard model.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| Age | 1.065 | 1.033–1.097 | <0.001 | 1.064 | 1.027–1.102 | 0.001 |
| AST | 1.002 | 1.000–1.004 | 0.020 | 1.002 | 0.997–1.006 | 0.408 |
| LDH | 1.001 | 1.000–1.002 | 0.002 | 1.000 | 0.998–1.002 | 0.953 |
| PNI (1 vs. 0) | 3.232 | 1.661–6.291 | 0.001 | 2.414 | 1.016–5.736 | 0.046 |
| Red blood count | 0.450 | 0.280–0.721 | 0.001 | 0.372 | 0.101–1.364 | 0.136 |
| Haemoglobin | 0.980 | 0.966–0.944 | 0.004 | 1.028 | 0.981–1.077 | 0.242 |
| Blood urea nitrogen | 1.215 | 1.066–1.385 | 0.003 | 0.980 | 0.817–1.175 | 0.828 |
| Creatinine | 1.005 | 1.002–1.008 | <0.001 | 1.005 | 0.999–1.012 | 0.104 |
| Triglycerides | 0.690 | 0.495–0.960 | 0.028 | 0.805 | 0.544–1.193 | 0.280 |
| TC | 0.708 | 0.509–0.986 | 0.041 | 0.856 | 0.569–1.289 | 0.457 |
| LVEF | 0.916 | 0.883–0.950 | <0.001 | 0.931 | 0.890–0.974 | 0.002 |
| Urine protein | 1.402 | 1.064–1.846 | 0.016 | 0.914 | 0.411–2.034 | 0.826 |
| Left main | 1.670 | 0.593–4.703 | 0.332 | 1.908 | 0.454–8.020 | 0.378 |
| WBC | 1.149 | 1.070–1.235 | <0.001 | 1.203 | 1.118–1.294 | <0.001 |
| Killip class ≥2 | 5.15 | 1.350–18.378 | 0.016 | 2.525 | 0.629–10.130 | 0.191 |
| Gensini score | 1.03 | 0.989–1.020 | 0.603 | 1.001 | 0.984–1.017 | 0.963 |
| GRACE | 1.014 | 1.011–1.037 | <0.001 | 1.038 | 1.002–1.074 | <0.001 |
AST, aspartate transaminase; LDH, lactate dehydrogenase; TC, total cholesterol; LVEF, left ventricular ejection fraction; WBC, white blood cell count; GRACE, Global Registry of Acute Coronary Events; PNI, prognostic nutritional index; HR, hazard ratio; CI, confidence interval.
Figure 2.
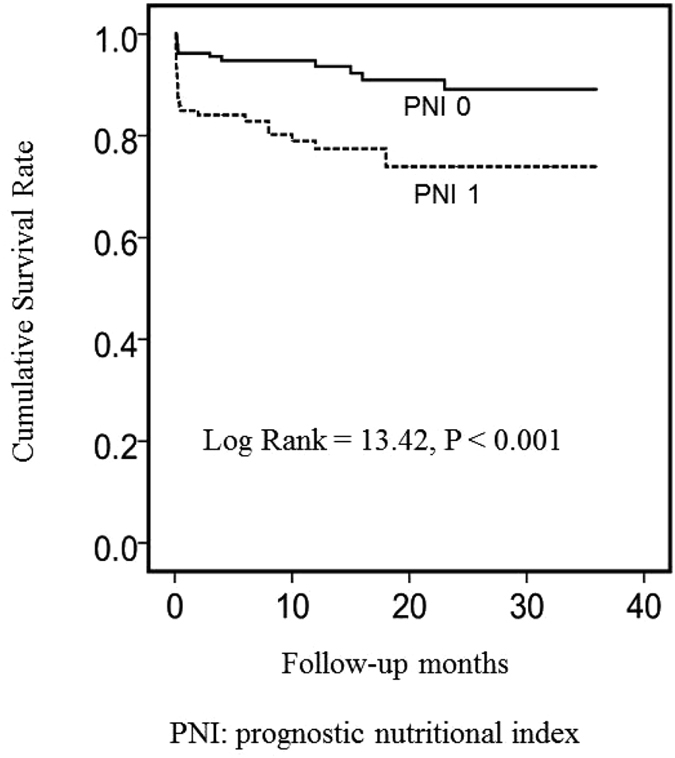
Kaplan–Meier survival analysis using the PNI score group of the STEMI patients.
As shown in Table 4, the PNI = 1 group had significantly higher rates of in-hospital all-cause mortality (14.2 vs. 3.7%) (P < 0.001 for all), of bleeding (6.7 vs. 3.7%), and of recurrent MI (5.0 vs. 2.1%); however, there was no significant difference between the two groups in terms of the rates of reinfarction or bleeding. At long-term follow-up (median follow-up time, 19.5 [3–36] months), the PNI = 1 group showed significantly higher rates of mortality (7.5 vs. 3.2%, P < 0.001) and had a lower frequency of cerebrovascular accidents (0.8 vs. 1.1%, P < 0.001), whereas there was no difference with respect to myocardial infarction re-interventionon percutaneous coronary intervention.
Table 4.
Major adverse cardiac events in STEMI patients after pPCI by PNI score group.
| PNI = 0 (n = 189) | PNI = 1 (n = 120) | P-value | |
|---|---|---|---|
| In-hospital complications | |||
| Bleeding | 7 (3.7) | 8 (6.7) | 0.363 |
| In-hospital mortality | 7 (3.7) | 17 (14.2) | <0.001 |
| Recurrent MI | 4 (2.1) | 6 (5.0) | 0.286 |
| MACE (follow-up) | |||
| MI | 8 (4.2) | 7 (5.8) | 0.714 |
| Death | 6 (3.2) | 9 (7.5) | <0.001 |
| CVA | 2 (1.1) | 1 (0.8) | <0.001 |
| Re-intervention PCI | 11 (5.8) | 6 (4.6) | 0.958 |
CVA, cerebrovascular accident; MACE, major adverse cardiac events; MI, myocardial infarction; PCI, percutaneous coronary intervention; PNI, prognostic nutritional index; STEMI, acute ST-segment elevation myocardial infarction.
Discussion
To the best of our knowledge, this is the first study to investigate the prognostic value of PNI, a combined nutritional-inflammatory score based on serum albumin levels and the lymphocyte count, in patients with STEMI undergoing pPCI. A greater PNI of 1 on admission was associated with higher in-hospital and long-term follow-up mortality in STEMI patients treated with pPCI. PNI was identified as a significant independent predictor of mortality in STEMI patients undergoing pPCI. Moreover, cumulative survival was significantly lower in patients with a PNI of 1 relative to patients with a PNI of 0. Thus, PNI on admission appears to be useful for risk stratification of STEMI patients undergoing pPCI.
The PNI combines the albumin level and the lymphocyte count into a single composite marker of nutrition, inflammation and immunity status10, 15. The PNI was initially designed to assess the immunological and nutritional aspects of patients who underwent gastrointestinal tract surgery and was predominantly an indicator of the nutritional status of any given patient16–18. Albumin is a widely used indicator for nutrition and has been shown to correlate with postoperative complications19, 20. However, there is increasing evidence that the serum albumin level decreases with the increasing severity of inflammation9, 21, 22. Albumin not only is the main determinant of plasma oncotic pressure but also transports numerous substances and participates in both acute and chronic inflammatory responses23, 24. Many studies have shown an elevation of inflammatory markers in myocardial infarction, and several inflammatory markers have been identified as useful predictors of clinical outcomes25, 26. Meanwhile, there is increasing evidence that hypoalbuminemia on admission is a strong independent predictor of long-term mortality and severe heart failure development in pPCI treated STEMI patients9. Moreover, hypoalbuminemia was significantly associated with in-hospital mortality in patients with STEMI who were ≥85 years of age27.
Atherosclerotic plaque rupture is an inflammatory process that is mediated by the complex interaction between neutrophil-mediated reactive immune responses and subsequent lymphocyte-mediated adaptive immune responses28–30. Procoagulants are secreted locally by the leukocytes, increasing oxidative and proteolytic damage31, 32. Lymphocytes also have an essential role in modulating the inflammatory response at different stages of the atherosclerotic process28. In the acute setting of coronary events, lymphocytopenia is a common finding during the stress response and is secondary to increased corticosteroid levels, whereas a greater lymphocyte count reflects a more appropriate immune response and a stable, quiescent inflammatory status33. In two previous studies, lymphocytopenia was independently associated with the occurrence of complications and death after acute myocardial infarction34, 35.
In our study, we found that PNI was an independent predictor of mortality in patients with STEMI undergoing pPCI. However, the pathophysiological mechanism of the association between the higher PNI and the poorer clinical outcome of STEMI patients who are treated with pPCI are not completely understood. Because PNI is calculated based on the serum albumin level and the total lymphocyte count in the peripheral blood, PNI may characterize both the nutritional and immunological status, which could affect the survival rate of cancer patients15, 36, 37. Several mechanisms may be responsible. First, increased inflammatory activity in the setting of STEMI may be the underlying mechanism for the association between a decreased serum albumin (SA) level and mortality after pPCI38. Additionally, SA is an important inhibitor of platelet aggregation that increases the production of the antiaggregatory prostaglandin D2 (PGD2) from cyclic endoperoxides39, 40. Furthermore, hypoalbuminemia may increase blood viscosity and disrupt endothelial function due to the increased concentrations of free lysophosphatidylcholine41. In addition, the lymphocyte count is an index of cell-mediated immunity. A low lymphocyte count may be associated with pre-existing immunosuppression, which could indicate an inadequate immunological reaction in the patient42. Therefore, in theory, combining serum albumin levels and the lymphocyte count to create the PNI may be able to estimate the nutritional, inflammatory and immunity statuses of STEMI patients. In the present study, the area under the ROC curve for the prediction of mortality using PNI exceeded the area under the ROC curve for the prediction of mortality using albumin levels and the lymphocyte counts separately, which indicates that the PNI provides a stronger predictive power of mortality than do its components.
The present study has several limitations. First, it is a single-centre study, and findings in the present study need to be confirmed and validated in larger populations. Second, inflammation-associated markers other than WBC counts were not analysed or compared with the PNI. Third, only baseline serum albumin levels and baseline lymphocyte counts were determined, and serial measurements of the latter PNI components may provide an additional prognostic value. Finally, future prospective studies are warranted to clarify the pathophysiologic roles of the PNI components.
Our study indicated that the PNI is a significant prognostic factor for STEMI patients undergoing pPCI. Proper assessments of the nutritional-inflammatory status of STEMI patients at the time of hospital admission can help to minimize (if not prevent) complications and readmission and mortality rates. The proof that the aggressive treatment of malnutrition, in addition to personalized dyslipidaemic therapy, in STEMI patients improves outcomes would be the most convincing evidence. Therefore, more comprehensive studies on the treatment of malnutrition and its effect on outcomes are needed.
Methods
Study design
This prospective cohort study complied with the Helsinki Declaration of 1975 based on its 1983 revision, and the Human Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University approved the study protocol. All patients provided written informed consent. The study inclusion criteria were as follows: presentation within the first 12 hours of the onset of chest pain and ST-segment elevation of at least 1 mm in two or more contiguous leads (2 mm for leads V1–V3) or presentation with a new-onset left bundle branch block. Patients with an active infection, a previous chronic inflammatory disease history, a known malignancy, an advanced-stage liver or renal disorder, or fibrinolytic administration in the previous 30 days were excluded from this study. PNI was assessed as a predictor of in-hospital and long-term follow-up mortality as the primary outcome.
Study subjects
From September 2011 to November 2014, a total of 324 consecutive patients who were hospitalized at the First Affiliated Hospital of Xinjiang Medical University for acute STEMI and who underwent pPCI within 12 hours of the diagnosis were screened for study enrolment. Of these patients, 15 patients were excluded: 3 patients had unavailable laboratory data, 10 patients were treated with urgent coronary artery bypass graft surgery due to failed pPCI or due to coronary anatomy that was not amenable to pPCI, 1 patient had severe renal failure, and 1 patient had a chronic infection. Consequently, a total of 309 patients were enrolled in this study.
Data collection and blood sampling
The baseline clinical and demographic characteristics of the patients were recorded from hospital files and computer records. Venous blood samples were collected using standardized EDTA blood tubes within 1 hour of admission. Albumin levels were measured using the photometric method (DC 800; Beckman Coulter, Dublin, Ireland). A haematology profile including the lymphocyte count, haemoglobin level and mean platelet volume (MPV) was determined using an automated haematology analysis system (LH750, Beckman Coulter Inc., Brea, CA, USA). An electrocardiogram (ECG) was immediately obtained on admission, 60 minutes after the procedure, and daily thereafter during the length of the hospital stay. Left ventricular ejection fraction (LVEF) was calculated using the biplane Simpson method within 12 hours of admission.
Coronary angiography and percutaneous coronary intervention
All patients received a 300 mg dose of chewable aspirin and a 300–600 mg loading dose of clopidogrel on admission. Prior to the procedure, patients also received 70 U/kg of standard intravenous heparin. The use of a glycoprotein IIb/IIIa inhibitor (tirofiban) was left to the discretion of the primary operator. All pPCI procedures were performed by experienced interventional cardiologists who used a transradial approach and drug-eluting stents. Serial monitoring of cardiac biomarkers was performed every eight hours starting 24 hours after the PCI and continuing until the patient was discharged. After the intervention, all patients received daily regimens of 100 mg of aspirin and 75 mg of clopidogrel. At the time of discharge, all patients were prescribed a daily aspirin regimen in perpetuity and a daily regimen of clopidogrel for at least 9–12 months.
Long-term follow-up
In-hospital clinical data were recorded from hospital files and computer records. The long-term follow-up (median: 19.5 months) data of patients were obtained from follow-up visits or in-hospital clinical records of re-admitted patients. In addition, all patients were contacted by telephone.
Definition of PNI
Baseline total lymphocyte counts and albumin levels were routinely measured on admission. The PNI cut-off score of 45 has been used in 3 recent oncological studies and has been confirmed as optimal15, 27, 33. Based on those results, we choose a score of 45 as our tangent point value. The PNI was calculated as described previously: albumin (g/L) + 5 × total lymphocyte count × 109/L scores that were ≥45 and scores that were <45 at admission were assigned PNI scores of 0 (n = 189) and 1 (n = 120), respectively.
Statistical analysis
Continuous variables are expressed as either the mean ± SD or the median with an interquartile range (25–75%). Parametric, non-parametric and categorical data were compared using one-way ANOVA, Kruskal-Wallis, and chi-square (χ2) tests, respectively. Kaplan-Meier curves were generated for each PNI group. Cox proportional hazard models were used to investigate whether PNI predicted mortality during the study period. Forty variables were tested as all-cause mortality predictors in the univariate analysis, and the 14 significant variables were included in the multivariate analysis. P < 0.05 was considered statistically significant. Data analysis was performed using the SPSS version 18.0 statistical software package (Chicago, IL, USA).
Acknowledgements
This work was supported by a grant from Xinjiang Uygur Autonomous Region Science and Technology Project (No. 2016E02072).
Author Contributions
Conceived and designed the study: Y.N.Y. and X.M.L.; Performed the experiments: Q.J.C. and H.J.Q.; Contributed tools for the methods and analysis: Y.T.M., D.Z.L., J.J.Z., Y.X. and L.L.; Analysed the data: D.Z.L., H.J.Q. and Q.J.C.; Statistical analyses: D.Z.L. and H.J.Q.; Writing of the manuscript: Q.J.C. and H.J.Q.; Preparation of tables and figures: Q.J.C. and H.J.Q. All authors have reviewed the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Qing-Jie Chen and Hui-Juan Qu contributed equally to this work.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 2.Pu J, et al. Insights into echo-attenuated plaques, echolucent plaques, and plaques with spotty calcification: novel findings from comparisons among intravascular ultrasound, near-infrared spectroscopy, and pathological histology in 2,294 human coronary artery segments. Journal of the American College of Cardiology. 2014;63:2220–2233. doi: 10.1016/j.jacc.2014.02.576. [DOI] [PubMed] [Google Scholar]
- 3.Moon J, et al. Serum transaminase determined in the emergency room predicts outcomes in patients with acute ST-segment elevation myocardial infarction who undergo primary percutaneous coronary intervention. International journal of cardiology. 2014;177:442–447. doi: 10.1016/j.ijcard.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 4.He B, et al. Influence of microvascular dysfunction on regional myocardial deformation post-acute myocardial infarction: insights from a novel angiographic index for assessing myocardial tissue-level reperfusion. Int J Cardiovasc Imaging. 2016;32:711–719. doi: 10.1007/s10554-015-0834-4. [DOI] [PubMed] [Google Scholar]
- 5.Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. Journal of the American College of Cardiology. 2004;43:1439–1444. doi: 10.1016/j.jacc.2003.11.039. [DOI] [PubMed] [Google Scholar]
- 6.Sargento L, Longo S, Lousada N, dos Reis RP. The importance of assessing nutritional status in elderly patients with heart failure. Current heart failure reports. 2014;11:220–226. doi: 10.1007/s11897-014-0189-5. [DOI] [PubMed] [Google Scholar]
- 7.Ueno T, et al. Albumin concentration determined by the modified bromocresol purple method is superior to that by the bromocresol green method for assessing nutritional status in malnourished patients with inflammation. Annals of clinical biochemistry. 2013;50:576–584. doi: 10.1177/0004563213480137. [DOI] [PubMed] [Google Scholar]
- 8.Sujino Y, et al. Impact of hypoalbuminemia, frailty, and body mass index on early prognosis in older patients (>/= 85 years) with ST-elevation myocardial infarction. Journal of cardiology. 2015;66:263–268. doi: 10.1016/j.jjcc.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Oduncu V, et al. The prognostic value of serum albumin levels on admission in patients with acute ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coronary artery disease. 2013;24:88–94. doi: 10.1097/MCA.0b013e32835c46fd. [DOI] [PubMed] [Google Scholar]
- 10.Nochioka K, et al. Prognostic impact of nutritional status in asymptomatic patients with cardiac diseases: a report from the CHART-2 Study. Circulation journal: official journal of the Japanese Circulation Society. 2013;77:2318–2326. doi: 10.1253/circj.CJ-13-0127. [DOI] [PubMed] [Google Scholar]
- 11.Nakagomi A, et al. Nutritional Status is Associated with Inflammation and Predicts a Poor Outcome in Patients with Chronic Heart Failure. Journal of atherosclerosis and thrombosis. 2016;23:713–727. doi: 10.5551/jat.31526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fukushima K, et al. The nutritional index ‘CONUT’ is useful for predicting long-term prognosis of patients with end-stage liver diseases. The Tohoku journal of experimental medicine. 2011;224:215–219. doi: 10.1620/tjem.224.215. [DOI] [PubMed] [Google Scholar]
- 13.Iseki Y, et al. Impact of the Preoperative Controlling Nutritional Status (CONUT) Score on the Survival after Curative Surgery for Colorectal Cancer. PloS one. 2015;10:e0132488. doi: 10.1371/journal.pone.0132488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kos FT, et al. Assessment of Prognostic Value of “Neutrophil to Lymphocyte Ratio” and “Prognostic Nutritional Index” as a Sytemic Inflammatory Marker in Non-small Cell Lung Cancer. Asian Pacific journal of cancer prevention: APJCP. 2015;16:3997–4002. doi: 10.7314/APJCP.2015.16.9.3997. [DOI] [PubMed] [Google Scholar]
- 15.Chan AW, et al. Prognostic Nutritional Index (PNI) Predicts Tumor Recurrence of Very Early/Early Stage Hepatocellular Carcinoma After Surgical Resection. Annals of surgical oncology. 2015;22:4138–4148. doi: 10.1245/s10434-015-4516-1. [DOI] [PubMed] [Google Scholar]
- 16.Onodera T, Goseki N, Kosaki G. [Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients] Nihon Geka Gakkai zasshi. 1984;85:1001–1005. [PubMed] [Google Scholar]
- 17.Nozoe T, et al. Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma. Surgery today. 2010;40:440–443. doi: 10.1007/s00595-009-4065-y. [DOI] [PubMed] [Google Scholar]
- 18.Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. American journal of surgery. 1980;139:160–167. doi: 10.1016/0002-9610(80)90246-9. [DOI] [PubMed] [Google Scholar]
- 19.Relles DM, et al. Serum blood urea nitrogen and serum albumin on the first postoperative day predict pancreatic fistula and major complications after pancreaticoduodenectomy. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2013;17:326–331. doi: 10.1007/s11605-012-2093-1. [DOI] [PubMed] [Google Scholar]
- 20.Wysocki WM, et al. Preoperative radiotherapy does not alter pre- and early postoperative serum C-reactive protein and albumin concentrations in colorectal cancer patients. Contemporary oncology. 2013;17:161–164. doi: 10.5114/wo.2013.34620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurtul A, et al. Serum albumin levels on admission are associated with angiographic no-reflow after primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction. Angiology. 2015;66:278–285. doi: 10.1177/0003319714526035. [DOI] [PubMed] [Google Scholar]
- 22.Ishida S, et al. Serum albumin levels correlate with inflammation rather than nutrition supply in burns patients: a retrospective study. The journal of medical investigation: JMI. 2014;61:361–368. doi: 10.2152/jmi.61.361. [DOI] [PubMed] [Google Scholar]
- 23.Chojkier M. Inhibition of albumin synthesis in chronic diseases: molecular mechanisms. Journal of clinical gastroenterology. 2005;39:S143–146. doi: 10.1097/01.mcg.0000155514.17715.39. [DOI] [PubMed] [Google Scholar]
- 24.Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Seminars in dialysis. 2004;17:432–437. doi: 10.1111/j.0894-0959.2004.17603.x. [DOI] [PubMed] [Google Scholar]
- 25.Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA: the journal of the American Medical Association. 1998;279:1477–1482. doi: 10.1001/jama.279.18.1477. [DOI] [PubMed] [Google Scholar]
- 26.Neumann FJ, et al. Cardiac release of cytokines and inflammatory responses in acute myocardial infarction. Circulation. 1995;92:748–755. doi: 10.1161/01.CIR.92.4.748. [DOI] [PubMed] [Google Scholar]
- 27.Mohri Y, et al. Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World journal of surgery. 2013;37:2688–2692. doi: 10.1007/s00268-013-2156-9. [DOI] [PubMed] [Google Scholar]
- 28.Kurtul A, et al. Increased neutrophil-to-lymphocyte ratio predicts persistent coronary no-flow after wire insertion in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Clinics. 2015;70:34–40. doi: 10.6061/clinics/2015(01)07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pu, J. et al. In vivo characterization of coronary plaques: novel findings from comparing greyscale and virtual histology intravascular ultrasound and near-infrared spectroscopy. European Heart Journal33, doi:10.1093/eurheartj/ehr387 (2012). [DOI] [PubMed]
- 30.Wu XF, et al. Level of pregnancy-associated plasma protein-A correlates with coronary thin-cap fibroatheroma burden in patients with coronary artery disease: novel findings from 3-vessel virtual histology intravascular ultrasound assessment. Medicine (Baltimore) 2016;95:e2563. doi: 10.1097/MD.0000000000002563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ducloux D, Challier B, Saas P, Tiberghien P, Chalopin JM. CD4 cell lymphopenia and atherosclerosis in renal transplant recipients. Journal of the American Society of Nephrology: JASN. 2003;14:767–772. doi: 10.1097/01.ASN.0000048718.43419.44. [DOI] [PubMed] [Google Scholar]
- 32.He B, et al. The nuclear melatonin receptor RORα is a novel endogenous defender against myocardial ischemia/reperfusion injury. Journal of Pineal Research. 2016;60:313–326. doi: 10.1111/jpi.12312. [DOI] [PubMed] [Google Scholar]
- 33.Onsrud M, Thorsby E. Influence of in vivo hydrocortisone on some human blood lymphocyte subpopulations. I. Effect on natural killer cell activity. Scandinavian journal of immunology. 1981;13:573–579. doi: 10.1111/j.1365-3083.1981.tb00171.x. [DOI] [PubMed] [Google Scholar]
- 34.Widmer, A. et al. Mechanical complications after myocardial infarction reliably predicted using C-reactive protein levels and lymphocytopenia. Cardiology99, 25–31, doi:68448 (2003). [DOI] [PubMed]
- 35.Arbel Y, et al. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography. Atherosclerosis. 2012;225:456–460. doi: 10.1016/j.atherosclerosis.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 36.Pinato DJ, North BV, Sharma R. A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI) British journal of cancer. 2012;106:1439–1445. doi: 10.1038/bjc.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang Y, et al. Prognostic significance of preoperative prognostic nutritional index in colorectal cancer: results from a retrospective cohort study and a meta-analysis. Oncotarget. 2016 doi: 10.18632/oncotarget.10148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Djousse L, Rothman KJ, Cupples LA, Levy D, Ellison RC. Serum albumin and risk of myocardial infarction and all-cause mortality in the Framingham Offspring Study. Circulation. 2002;106:2919–2924. doi: 10.1161/01.CIR.0000042673.07632.76. [DOI] [PubMed] [Google Scholar]
- 39.Gresele P, Deckmyn H, Huybrechts E, Vermylen J. Serum albumin enhances the impairment of platelet aggregation with thromboxane synthase inhibition by increasing the formation of prostaglandin D2. Biochemical pharmacology. 1984;33:2083–2088. doi: 10.1016/0006-2952(84)90577-X. [DOI] [PubMed] [Google Scholar]
- 40.Maalej N, Albrecht R, Loscalzo J, Folts JD. The potent platelet inhibitory effects of S-nitrosated albumin coating of artificial surfaces. Journal of the American College of Cardiology. 1999;33:1408–1414. doi: 10.1016/S0735-1097(98)00687-1. [DOI] [PubMed] [Google Scholar]
- 41.Joles JA, Willekes-Koolschijn N, Koomans HA. Hypoalbuminemia causes high blood viscosity by increasing red cell lysophosphatidylcholine. Kidney international. 1997;52:761–770. doi: 10.1038/ki.1997.393. [DOI] [PubMed] [Google Scholar]
- 42.Zhang S, et al. Neutrophil count improves the GRACE risk score prediction of clinical outcomes in patients with ST-elevation myocardial infarction. Atherosclerosis. 2015;241:723–728. doi: 10.1016/j.atherosclerosis.2015.06.035. [DOI] [PubMed] [Google Scholar]


