Abstract
Purpose
Evidence suggests that radiotherapy may not have substantial benefits for older women with early-stage breast cancer, yet more than 75% of patients opt for this treatment. Given that this is a preference-sensitive decision, the utilization pattern suggests the decision-making might not be shared appropriately. The objectives of this study were to identify the information older women with early-stage breast cancer need when making radiotherapy decisions, and whom patients identify as the main decision-maker.
Method
We surveyed (through face-to-face, phone, or mail) women aged 65 and older who received lumpectomy and were considering or receiving adjuvant radiotherapy for early-stage breast cancer. The survey instrument was constructed with input from patient and professional advisory committees, including breast cancer survivors, advocates of breast cancer care and aging, clinicians, and researchers. Participants rated the importance (on a 4-point scale) of 24 statements describing the benefits, side effects, impact on daily life, and other issues of radiotherapy in relation to radiotherapy decision-making. Participants also designated who was considered the key decision-maker.
Results
The response rate was 56.4% (93/165). Mean age was 72.5 years, ranging from 65 to 93 years. More than 96% of participants indicated they were the main decision-maker on receiving radiotherapy. There was wide variation in information needs regarding radiotherapy decision-making. Participants rated a mean of 18 (range: 3–24) items as “essential.” Participants rated items related to benefits highest, followed by side effects. Participants who were older than 75 rated 13.9 questions as essential; whereas participants who were 74 or younger rated 18.7 as essential (p-value=.018).
Conclusions
Older women desire information and have more agency and input in the decision-making process than prior literature would suggest. The variation in information needs indicates that future decision support tools should provide options to select what information would be of interest to the participants.
INTRODUCTION
Breast cancer is one of the most common malignant tumors in women, and about half of all breast cancers occur in patients after age 65.1 While adjuvant radiotherapy (RT) after breast-conserving surgery (BCS) is considered the standard of care,2 RT does not improve longevity for many older breast cancer patients.3–5 The National Comprehensive Cancer Network guidelines suggest that adjuvant RT after BCS may be omitted for breast cancer patients who are older, have limited life expectancy due to comorbidities, or have favorable tumor characteristics.6 This is largely based on the PRIME II and Cancer and Leukemia Group B 9343 (C9343) trials, which have shown that RT leads to a small improvement in loco-regional recurrence but does not improve overall or disease-free survival for older patients with favorable tumor features.3,4 However, despite these data, approximately 75% of patients who could safely omit RT still received such treatment.7 On one hand, some patients may overestimate the benefits of RT, as the risk for development of treatment-related complications is not trivial.8,9 On the other hand, some patients who may substantially benefit from RT omit this therapy. Both situations suggest that the current model of physician-patient communication might be ineffective in helping older women fully comprehend the risks and benefits of breast radiation.
Little is known about how older women make their RT decisions. Existing literature suggests that older people are more likely to be passive decision-makers;10–12 that is, they are more likely than younger population to accept their doctors’ recommendations without actively participating in the decision making process. If physicians are the main decision makers for older women, then interventions designed to reduce utilization of RT should focus on the physicians. Such interventions might concentrate on educating physicians about the minimal benefit of RT in this setting, or on overcoming the inherent intervention bias13 to which physicians are vulnerable. Alternatively, if older women are the main decision-makers, then efforts should be expended to engage patients and their families in the shared decision-making conversation so that patient preference can be the driving force behind the ultimate therapeutic decision. Indeed, evidence suggests that shared decision-making can lead to better quality of care, increased patient satisfaction, and a range of cognitive, affective, behavioral, and health-status benefits.14–16 In order to facilitate such shared decision-making, it is important to know the information needs of women during this decision process, and also to understand who and what helps influence this decision.
The objectives of this study were to identify 1) the information necessary for older women with early stage breast cancer to facilitate their RT decision, 2) the role of family, friends, or providers in the decision-making process, 3) the main decision-maker in this process, and 4) the magnitude of the perceived benefit of RT which is required to receive this treatment. This information is required to inform interventions to facilitate shared decision-making related to adjuvant RT among older women. We also examined whether the information needs were correlated with various demographic factors such as age, race/ethnicity, education, tumor characteristics, and participants’ plans to receive or forgo RT. Our research could better identify patient’s views if patients are properly informed and educate physicians on what patients want to know.
METHODS
Questionnaire Development
To assess patients’ information needs regarding RT decision-making, a survey instrument was constructed with input from patient and professional advisory committees. Our patient advisory committee consisted of 13 members, including breast cancer survivors (n=6) and community members who are advocates for aging (n=4) or breast cancer care (n=7; four are also breast cancer survivors). We also organized a professional advisory committee, which included a radiation oncologist, a medical oncologist, a surgical oncologist, a geriatric oncologist, and the remaining research team members. Through collaborative discussions with the patient and professional advisory committees, we developed a list of potential informational needs surrounding the decision to receive breast radiation (Appendix Table 1). The final questionnaire was divided into four domains as follows: (1) benefits of RT (3 questions); (2) side effects of RT (7 questions); (3) impact of daily life while receiving RT (7 questions); and (4) additional information needs surrounding RT decision (7 questions). We used four response categories to explore the importance of information—essential, desired, neutral (not important), or avoidable (don’t want to know)—following prior research that has examined information needs among prostate cancer patients.17 We also included an open-ended question to identify any additional information participants felt was important for making this treatment decision.
Participants and Procedures
Patients, recruited from five radiation oncology clinics, were women aged at least 65 years, diagnosed with stage I/II breast cancer, received BCS, and were considering or receiving adjuvant RT. The recruitment period was from May 2015 to August 2016, and all consecutively scheduled consults were screened for eligibility. Patients were then screened by their physicians for willingness to participate, as well as any emotional or cognitive impairment that would interfere with their ability to participate. Written consent was obtained from all patients prior to enrollment in the study. Patients completed the survey either independently or with help from a research assistant. Patients were also allowed to take the survey home to complete and return it via mail or at their next follow-up appointment. In order to understand the information needs of women who elected to forgo RT, we also identified eligible patients who had breast cancer diagnosed in 2014 at our institution and did not receive RT. This group of participants was asked to return the questionnaire via mail. The Human Investigation Committee of authors’ institution approved this study.
Each participant indicated whether other people helped or would help her make the decision to undergo RT; and if so, who these people were. Participants then indicated who the main decision maker was in terms of their RT decision. We asked participants to rate the items in the survey by importance (on four response categories described above) in making their RT decision. We also asked how significant the benefit of radiation needed to be for them to decide to receive RT (see footnotes of Figure 1). Participants also indicated whether they planned to receive RT (or whether they did receive RT for participants who were diagnosed in 2014).
Figure 1. Impact of the Incremental Benefit of radiotherapy (RT) for RT Decision-Making*.
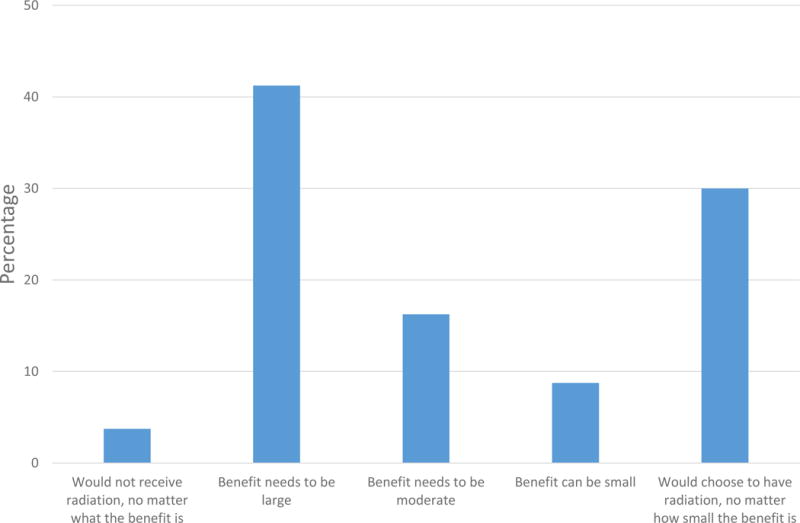
* The questionnaire stated that RT can prevent cancer recurrence, but may have some negative effects.
We then asked “Thinking about what is important to you, how significant would the benefit of radiation need to be for you to decide to receive radiation therapy?” 13 participants who had missing value, or responded as “don’t know/unsure” or “refuse to answer” were excluded in this figure.
Demographic information was collected on age, race/ethnicity, marital status, education, income, insurance, and financial status. We collected information about their tumor characteristics and medical conditions, including disease stage, tumor size, tumor grade, surgical margin (positive, close <2mm, and negative), estrogen receptor (ER) status, lymph node involvement status, and other comorbidities from the medical records.
Statistical Analyses
Descriptive statistics were performed for continuous variables using means and standard deviations, and categorical measures using frequency counts and percentages. We summarized a count variable for the number of questions that each participant rated as essential information. Using a two-sample two-sided t test, we examined the relationship with patient and tumor characteristics, as well as participant’s plan whether or not to receive RT. Fishers exact test was used for comparisons of frequencies. All analyses were performed using SAS Version 9.3 (SAS Institute, Cary, NC), and a two-tailed p<.05 was used to define statistical significance.
Results
Participants
Of the 121 eligible patients who were approached in the radiation oncology clinic, 83 patients completed the survey (a response rate of 68.6%). Additionally, of the 44 surveys that were mailed to patients who had received BCS in 2014 without subsequent RT, 10 were returned (a response rate of 22.7%). Our combined response rate was 56.4%. The mean age of the 93 participants was 72.5 (ranging from 65 to 93; Table 1). The majority were non-Hispanic whites (87.5%), were living with others (58.4%), had higher than secondary school education (67.4%), and had Medicare and supplement insurance or private insurance coverage (83.5%). Only one participant indicated no insurance coverage, and 24.2% of participants indicated that they ‘make ends meet’ with some or great difficulty. Approximately 83.9% of participants had stage I breast cancer and 94.6% had ER-positive breast cancer. More than one-third of participants had restrictions in physical ability, and 52.7% of participants had other comorbid conditions, including chronic lung disease (22.6%), other cancer (19.4%), diabetes (16.1%), or heart disease (16.1%). Among the 83 participants recruited from radiation oncology clinics at the time of making RT decisions, 6 patients (7.2%) decided not to receive RT. Overall, 16 participants did not receive RT. Among them, 14 participants (87.5%) had radiation oncologist visit(s).
Table 1.
Patient characteristics
| Characteristics | Number (percentage)* |
|---|---|
| Age, years: Mean (range) | 72.5 (65–93) |
| Race (missing value=2) | |
| White | 79 (87.8%) |
| Black | 7 (7.8%) |
| Others | 4 (4.4%) |
| Hispanic (missing value=3) | |
| Yes | 3 (3.4%) |
| No | 86 (96.6%) |
| Marital status (missing value=1) | |
| Married/living together | 52 (56.5%) |
| Divorced/separated | 14 (15.2%) |
| Never married/never lived together | 6 (6.5%) |
| Widowed | 20 (21.7%) |
| Education (missing value=1) | |
| High school or less | 30 (32.6%) |
| Post-secondary | 62 (67.4%) |
| Income (missing value=3) | |
| Less than $49,999 | 28 (31.1%) |
| $50,000 to $99,999 | 24 (26.7%) |
| $100,000 to $149,999 | 9 (10%) |
| $150,000 and above | 13 (14.4%) |
| Refuse to answer | 16 (17.8%) |
| How easily can you “make ends meet” (missing value=2) | |
| With no difficulty | 44 (48.4%) |
| With minimal difficulty | 25 (27.5%) |
| With some difficulty | 17 (18.7%) |
| With great difficulty | 5 (5.5%) |
| Health insurance (missing value=2) | |
| Private insurance | 6 (6.6%) |
| Medicare alone | 10 (11.0%) |
| Medicare with supplemental insurance | 70 (76.9%) |
| Medicaid or another government assistance plan | 4 (4.4%) |
| No insurance coverage | 1 (1.1%) |
| Breast cancer stage | |
| Stage I | 78 (83.7%) |
| Stage II | 15 (16.1%) |
| Breast cancer grade | |
| 1 | 34 (36.6%) |
| 2 | 50 (53.8%) |
| 3 | 9 (9.7%) |
| Tumor size | |
| 2cm or less | 82 (88.2%) |
| >2cm | 11 (11.8%) |
| ER status | |
| Positive | 88 (94.6%) |
| Negative | 5 (5.4%) |
| HER2 status | |
| Positive | 2 (2.2%) |
| Equivocal | 8 (8.6%) |
| Negative | 82 (88.2%) |
| Unknown | 1 (1.1%) |
| Lymph node involvement | |
| Yes | 8 (8.6%) |
| No | 83 (89.2%) |
| No lymph node examination | 2 (2.2%) |
Decision-Making Roles
All except two participants (96.8%) indicated that they were the main decision-maker regarding RT treatment. Sixty-six participants (71.0%) indicated that other people participated in the RT decision. The most commonly cited individuals cited as being involved in decision-making included: doctors (71.2%), other family members (50.0%), their spouse (45.5%), friends (15.2%), and nurses (1.5%).
How Significant the Benefit of RT Needed to Be to Receive RT
In weighing the risks and benefits of RT, 41.3% of the 80 participants who provided quantifiable responses to this question indicated that the benefit of RT would need to be large for them to decide to receive RT (Figure 1). It should be noted that the interpretation of “large” by the respondents was a subjective value. Only 3.3% indicated that they would refuse RT, no matter what the benefit. In contrast, 30.0% indicated that they would choose to receive RT, no matter how small the treatment benefit.
Information Needed for Decision Making
Participants rated a mean of 17.6 (of 24) questions as essential for decision making (ranging from 0 to 24; standard deviation [SD] = 6.7). Participants rated items related to treatment benefits highest, followed by side effects. Approximately 91.3% of participants rated information about chances of survival and receipt of radiation as essential, and 88.0% of participants rated information regarding risks of recurrence with vs. without RT as essential. We reported the top 12 items in Table 2 (detailed results could be found in Appendix Table 2). While all except one participant had insurance coverage, 57.1% of participants rated information on out-of-pocket cost as essential.
Table 2.
The top 12 items ordered by percent essential for radiotherapy (RT) decision making in the survey
| Domain | Item | Percent essential | |||
|---|---|---|---|---|---|
| RT benefit | Benefits of RT | 92.4 | |||
| RT benefit | Chance that I will survive breast cancer with and without RT | 91.3 | |||
| RT benefit | Chances the cancer will come back with and without RT | 88.0 | |||
| Daily life | Be able to continue my normal schedule of activities during RT | 82.6 | |||
| Side effect | Increased risk of heart disease caused by RT | 82.4 | |||
| Side effect | Risk that RT will increase risks of other types of cancer | 78.3 | |||
| Other | What to do if the cancer comes back with or without RT | 78.3 | |||
| Other | How long do I have to make my decision | 78.0 | |||
| Side effect | Risk of lung disease cause by RT | 77.2 | |||
| Side effect | Risk of feeling tiredness | 76.1 | |||
| Daily life | How many weeks will it take to finish my RT | 76.1 | |||
| Other | My quality of life after treatment | 76.1 | |||
Associations with Importance Ratings
In bivariate analyses, the number of items which patients rated as essential was correlated with age and patient’s plan to receive or forgo RT. Participants who were older than 75 rated 13.9 (SD = 8.5) questions as essential; whereas participants who were 74 or younger rated 18.7 (SD = 5.6) as essential (p-value = .018 for two-sample t-test). Similarly, participants who planned to receive RT rated 18.8 (SD = 5.2) questions as essential, compared to 13.9 (SD = 9.7) questions among those who did not include RT in their treatment plan (p-value = .068). Participants who were undecided about receipt of RT rated 17.6 (SD = 5.9) questions as essential. The number of items that patients rated as essential was not correlated with race, education, income, stage, or comorbidity.
Younger participants were more likely to want information regarding treatment benefits, compared with older participants (Figure 2 and Appendix Table 2). Among participants who were 74 or younger, 97.1% rated information regarding chances of survival and receipt of radiation as essential, whereas 72.7% of participants who were older than 75 rated it as essential (p-value<.001). Similarly, 92.9% of participants who were 74 or younger rated information regarding cancer recurrence as essential, whereas 72.7% of participants who were older than 75 rated it as essential (p-value=.020). Only the item regarding ease of transport to the radiation center was rated lower by younger (60.9%) vs older (73.7%), but the result was statistically insignificant (p-value=.421).
Figure 2.
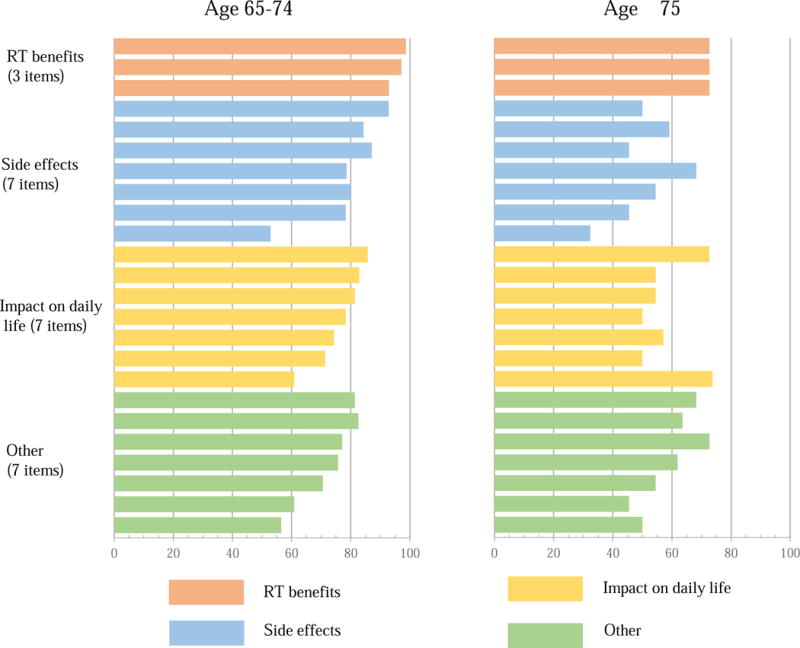
Questions rated as essential for radiotherapy decision making, grouped by the domain, and appearing vertically in the same order as listed in Appendix Table 1 (top bar question 1, bottom bar question 24)
Open-Ended Items
Seven participants indicated an interest in receiving additional information not listed in the survey. Two participants wanted information to support their family. Another patient requested greater clarification about what would be discussed during the consult visit, and requested a list of questions to be asked by patients during the visit. Other women wanted additional information regarding side effects of surgery (such as lymphedema), hormone therapy (weight gain and bone density) or chemotherapy (neuropathy). Separate from informational needs, another patient indicated that care coordination between health care providers was a priority for her.
Discussion
In this study, we found that almost all older women with early-stage breast cancer considered themselves the main decision-maker regarding receipt of RT. This finding is substantially different from prior literature: Two decades ago, one Canadian study showed that, approximately 52% breast cancer patients who were 70 or older preferred an active or collaborative role in decision making; and 48% of them preferred a passive role.12 While this preference may differ genuinely along national or cultural lines, or merely reflect a difference in survey methods or context, we hypothesize that the recent emphasis on shared-decision making processes may be the main driver, encouraging patient autonomy and involvement. Our results indicate that physicians should engage older patients in the decision process, as this is consistent with their perceived role. This is particularly important given that participants indicated that they received more assistance from doctors than from others (such as family members or friends) in making treatment decisions. It is not clear from our work which physicians (e.g. surgical oncology, medical oncology, radiation oncology, or primary care) were most relied upon, however.
Our findings build upon previous work in important ways. First, we identified two mechanisms that could explain why the majority of older women with breast cancer receive RT: misinterpretation of perceived risk and intervention bias. Overestimation of risk by participants is suggested by this work, given that a substantial number of participants choosing RT indicated that the benefit of RT must be large in order to receive treatment. This suggests that the relative term “large” can be interpreted variably, or perhaps that there is a numeracy issue at play, where the “large” relative risk reduction receives greater weight than the small absolute risk reduction. Therefore, providing accurate risk estimates to place these potential risks and benefits of treatment in context within their individual values may help reduce decisional conflict,18 and ensure that the true value of the risk reduction offered by RT is understood. Additionally, 30% of our population stated they would receive RT no matter how small the benefit, reflecting an intervention bias on the part of the patient. Fears of cancer may compound this bias, and outweigh the potential side effects and treatment burden, leading to overtreatment.19,20 Future research examining why these patients opt for treatment despite a small absolute benefit could advance our knowledge on decision-making processes.
Second, our findings on patient information needs could be integrated into a decision support tool to help patient-physician communications. Using focus groups and one patient interview, prior research has demonstrated that older women with early-stage breast cancer have individual information needs that are not fully met,21 yet little is known about the details of these needs. Our patient and professional advisory committees helped identify 24 salient items; and these items were rated as essential among the majority of our participants, ranging from 48.9% to 92.4%. Participants in our survey further identified two important items: coordination between providers and support for family members. These concepts will be integrated into the development of a decision tool. In a few cases, information contained in the survey prompted patients to seek clarification from their physicians, which further demonstrates the value of a structured approach to information provision.
Overall, participants rated items related to the benefits of RT highest, followed by side effects and the impact on daily life when receiving RT. Items related to the disruption in daily life RT can cause and cost information were considered less important than longer-term side effects such as heart damage or another cancer. Plausible explanations included that participants were retired, and almost all had insurance coverage. Furthermore, consistent with prior literature,22 women with breast cancer want a lot of information, but information needs vary. The variation in questions that might be considered as important for treatment decision-making has also been observed among patients with prostate cancer.17 To ensure an adequate shared decision-making process, these findings highlight the importance of individualized information provision.17,23 Future decision support tools should provide adequate options for patients to select which information is of interest.
We found that most demographics were not associated with information needs, except that participants who were older or elected to forgo RT tended to have fewer information needs. Younger participants were more likely to want information regarding survival benefits and risks of cancer recurrence than older participants, potentially reflecting that older women recognized potential competing mortalities or viewed quality of life as more important than maximal risk reduction. We acknowledge that participants who were older were more likely to elect to forgo RT. For instance, two older participants decided to not receive RT because one wanted to avoid burden to her family members, and another one thought she would die of other causes. Because of the small sample size, we were unable to determine the independent association attributed to age and RT decision separately. Future research is needed to address this question. Additionally, comparisons between young and old populations regarding their information needs are of great interest.
Our study has several limitations. The sample size was small, and overall participation rate was 56.4%. Therefore, there could be a non-response bias. Additionally, participation was limited to patients who visited an academic cancer center in the northeast; thus, results might not be applicable to the general population. For instance, while our sample varied by income and education, most participants were non-Hispanic whites. Information needs may vary along racial, cultural, or socioeconomic lines, and our population may not adequately reflect this diversity. Lastly, we recruited patients through the clinics of radiation oncologists; therefore, these women were at least considering treatment. Although almost every patient in our practice who receives BCS is referred to a radiation oncologist, those who elect to forgo RT may skip the consultation. While we did reach out to patients who did not receive RT via our survey, the response rate was low. These participants may also have recall bias, because the decision-making process took place 1 year prior to the survey. We acknowledge that our results were more representative of patients who opted for RT, however, this is consistent with other series of women in this population.7
In conclusion, older women desire information and have more agency and input in the decision-making process than anticipated. There is wide variation in information needs for RT decision-making. While almost all participants sought to understand the benefits of RT, a substantial proportion of them rated other aspects of treatment as essential, which include side effects and impact on daily life activities. A decision tool to help women prioritize their values and healthcare priorities is needed in this population.
Supplementary Material
Summary.
To understand information needs for radiotherapy decision-making, we surveyed 93 older women (≥65y/o) with early-stage breast cancer. Approximately 97% of participants indicated they were the main decision-maker on receiving radiotherapy. Wide variation in information needs exists: Participants rated a mean of 18 (range: 3–24) items as “essential.” Participants rated items related to benefits highest, followed by side effects. Younger participants (65–74 y/o) rated 18.7 as essential; whereas older participants rated 13.9 questions as essential (p-value=.018).
Acknowledgments
Funding: This study was supported by grant 1K01HS023900-01 from the Agency for Healthcare Research and Quality (Dr. Wang), and by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR060231-05 (Dr. Fraenkel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mandelblatt J. To screen or not to screen older women for breast cancer: a new twist on an old question or will we ever invest in getting the answers? Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007 Jul 20;25(21):2991–2992. doi: 10.1200/JCO.2007.11.9560. [DOI] [PubMed] [Google Scholar]
- 2.Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011 Nov 12;378(9804):1707–1716. doi: 10.1016/S0140-6736(11)61629-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kunkler IH, Williams LJ, Jack WJ, Cameron DA, Dixon JM. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. The Lancet Oncology. 2015 Mar;16(3):266–273. doi: 10.1016/S1470-2045(14)71221-5. [DOI] [PubMed] [Google Scholar]
- 4.Hughes KS, Schnaper LA, Berry D, et al. Lumpectomy plus tamoxifen with or without irradiation in women 70 years of age or older with early breast cancer. The New England journal of medicine. 2004 Sep 2;351(10):971–977. doi: 10.1056/NEJMoa040587. [DOI] [PubMed] [Google Scholar]
- 5.Hughes KS, Schnaper LA, Bellon JR, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2013 Jul 1;31(19):2382–2387. doi: 10.1200/JCO.2012.45.2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson RW, Allred DC, Anderson BO, et al. Breast cancer. Clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network : JNCCN. 2009 Feb;7(2):122–192. doi: 10.6004/jnccn.2009.0012. [DOI] [PubMed] [Google Scholar]
- 7.Soulos PR, Yu JB, Roberts KB, et al. Assessing the impact of a cooperative group trial on breast cancer care in the medicare population. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 May 10;30(14):1601–1607. doi: 10.1200/JCO.2011.39.4890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robb C, Haley WE, Balducci L, et al. Impact of breast cancer survivorship on quality of life in older women. Critical reviews in oncology/hematology. 2007 Apr;62(1):84–91. doi: 10.1016/j.critrevonc.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Gagliardi G, Constine LS, Moiseenko V, et al. Radiation dose-volume effects in the heart. International journal of radiation oncology, biology, physics. 2010 Mar 1;76(3 Suppl):S77–85. doi: 10.1016/j.ijrobp.2009.04.093. [DOI] [PubMed] [Google Scholar]
- 10.Hanson JL. Shared decision making: have we missed the obvious? Archives of internal medicine. 2008 Jul 14;168(13):1368–1370. doi: 10.1001/archinte.168.13.1368. [DOI] [PubMed] [Google Scholar]
- 11.Swenson SL, Buell S, Zettler P, White M, Ruston DC, Lo B. Patient-centered communication: do patients really prefer it? Journal of general internal medicine. 2004 Nov;19(11):1069–1079. doi: 10.1111/j.1525-1497.2004.30384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997 May 14;277(18):1485–1492. [PubMed] [Google Scholar]
- 13.Foy AJ, Filippone EJ. The case for intervention bias in the practice of medicine. The Yale journal of biology and medicine. 2013 Jun;86(2):271–280. [PMC free article] [PubMed] [Google Scholar]
- 14.Crawford MJ, Rutter D, Manley C, et al. Systematic review of involving patients in the planning and development of health care. BMJ. 2002 Nov 30;325(7375):1263. doi: 10.1136/bmj.325.7375.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kinnersley P, Edwards A, Hood K, et al. Interventions before consultations for helping patients address their information needs. The Cochrane database of systematic reviews. 2007;(3):CD004565. doi: 10.1002/14651858.CD004565.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease. The Cochrane database of systematic reviews. 2005;(4):CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 17.Feldman-Stewart D, Brundage MD, Hayter C, et al. What questions do patients with curable prostate cancer want answered? Medical decision making : an international journal of the Society for Medical Decision Making. 2000 Jan-Mar;20(1):7–19. doi: 10.1177/0272989X0002000102. [DOI] [PubMed] [Google Scholar]
- 18.Sherman KA, Shaw LK, Winch CJ, et al. Reducing Decisional Conflict and Enhancing Satisfaction with Information among Women Considering Breast Reconstruction following Mastectomy: Results from the BRECONDA Randomized Controlled Trial. Plastic and reconstructive surgery. 2016 Oct;138(4):592e–602e. doi: 10.1097/PRS.0000000000002538. [DOI] [PubMed] [Google Scholar]
- 19.Katz SJ, Morrow M. Contralateral prophylactic mastectomy for breast cancer: addressing peace of mind. JAMA. 2013 Aug 28;310(8):793–794. doi: 10.1001/jama.2013.101055. [DOI] [PubMed] [Google Scholar]
- 20.Bhatt JR, Klotz L. Overtreatment in cancer - is it a problem? Expert opinion on pharmacotherapy. 2016;17(1):1–5. doi: 10.1517/14656566.2016.1115481. [DOI] [PubMed] [Google Scholar]
- 21.Wong JJ, D’Alimonte L, Angus J, Paszat L, Soren B, Szumacher E. What do older patients with early breast cancer want to know while undergoing adjuvant radiotherapy? J Cancer Educ. 2011 Jun;26(2):254–261. doi: 10.1007/s13187-010-0188-5. [DOI] [PubMed] [Google Scholar]
- 22.Feldman-Stewart D, Madarnas Y, Mates M, et al. Information needs of post-menopausal women with hormone receptor positive early-stage breast cancer considering adjuvant endocrine therapy. Patient Educ Couns. 2013 Oct;93(1):114–121. doi: 10.1016/j.pec.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 23.Ruesch P, Schaffert R, Fischer S, et al. Information needs of early-stage prostate cancer patients: within- and between-group agreement of patients and health professionals. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2014 Apr;22(4):999–1007. doi: 10.1007/s00520-013-2052-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


