Abstract
Objectives. To measure the level of burnout among pharmacy practice faculty members at US colleges and schools of pharmacy and to identify factors associated with burnout.
Methods. Using a cross-sectional, electronic, anonymous survey-design, we measured faculty burnout (n=2318) at US colleges and schools of pharmacy using the Maslach Burnout Inventory-Educators Survey (MBI-ES), which measures burnout dimensions: emotional exhaustion, depersonalization, and personal accomplishment. We assessed MBI-ES scores, demographics and possible predictors of burnout.
Results. The response rate was 32.7% (n=758). Emotional exhaustion was identified in 41.3% and was higher in women, assistant professors, and those without a hobby. Participants without a mentor had higher scores of depersonalization. Those with children ages 1-12 years had higher emotional exhaustion and depersonalization compared to those with older children.
Conclusion. Pharmacy practice faculty members at US colleges and schools of pharmacy are suffering from burnout, exhibited mainly through emotional exhaustion.
Keywords: burnout, pharmacy practice faculty, stress
INTRODUCTION
Burnout is a pathological syndrome in which emotional depletion and maladaptive detachment develop secondary to chronic occupational stress.1 It may be associated with a decline in mental and physical health, as well as work performance. Additionally, burnout has been associated with conditions such as depression, suicide, and substance abuse.
The Maslach Burnout Inventory (MBI) measures the three dimensions of burnout (emotional exhaustion, depersonalization and cynicism, feelings of inefficacy) and is the gold standard for assessing burnout in medical research.1-5 This model defines “emotional exhaustion” as the stress component of burnout, in which an individual feels depleted of one’s emotional and physical resources without any source of replenishment. “Depersonalization” represents the interpersonal dimension of burnout, where an individual displays a distant attitude toward work and colleagues and is presumed to be a direct response to exhaustion. “Inefficacy” measured by perception of personal accomplishment, represents the self-evaluation aspect of burnout and refers to the belief that one is incompetent and lacks productivity at work.3,4 Of the three versions of the MBI Survey, the MBI-Educators Survey (MBI-ES) is designed for individuals working in education.3,6 A high subscore in emotional exhaustion or depersonalization is suggestive of clinically significant burnout.7
Burnout is a serious issue affecting individuals working in the health profession and higher education fields.8-15 To our knowledge, there is limited recent evidence for the systematic assessment of burnout among pharmacy practice faculty in the United States with very little published in academic pharmacy since the early 1990s.9,10,16,17 Assessing burnout among this population is important to identify associated factors and to develop strategies that can help reduce or prevent burnout. We aimed to assess the prevalence of burnout among pharmacy practice faculty using the MBI-ES and to identify predictive factors contributing to burnout.
METHODS
In August 2014, we measured burnout in pharmacy practice faculty members at US colleges and schools of pharmacy using a cross-sectional, voluntary, anonymous survey-design.6
We emailed a link to the MBI-ES with supplemental demographic questions to individuals listed on the 2014 American Association of Colleges of Pharmacy (AACP) pharmacy practice roster at the lecturer/instructor, assistant, associate, and full professor levels at US colleges and schools of pharmacy. Along with the survey, we also provided information on the research scope. Completion of the survey served as consent. A raffle for two $100 gift cards was utilized as incentive for participation. Participants were able to submit an email address for the raffle drawing that was not linked to survey results. Non-responders were emailed two weeks after baseline. Faculty whose emails were not returned to the investigators as “undeliverable” were considered to have received the survey. Faculty who did not respond to at least one question on the MBI-ES (items 1-22) were excluded from analysis.
The MBI-ES questions were divided into each subscale (Emotional Exhaustion=EE, Depersonalization=DP, Personal Accomplishment=PA). The average rating of each subscale was calculated by dividing the total score by the number of completed items. The EE subscale contained nine items, the DP subscale had five items, and the PA subscale had eight items. In EE and DP, low scores were seen as favorable, but in PA, low scores were seen as unfavorable. Scoring on the MBI-ES subscales are as follows: EE as 0-16 (low), 17-26 (moderate) and 27 or higher (high); DP as 0-6 (low), 7-12 (moderate) and 13 or higher (high); and PA as 0-30 (low), 31-36 (moderate) and 37 or higher (high).
De-identified data were collected via Qualtrics version 60949 (Provo, Utah) and analyzed with IBM SPSS Statistics, Version 22.0 (Armonk, NY). No personal identifiers were linked to survey results to ensure privacy. Data were password-protected and maintained by the investigators. Descriptive statistics (mean, median, standard deviations, range were used to evaluate the primary outcome. Student t-tests, chi-square and ANOVA were used to analyze associations between MBI scores and predictive factors (eg, gender, hobbies, mentor, children, marital status, academic rank) associated with faculty burnout. The study was approved by the Midwestern University and UCSD Institutional Review Boards.
RESULTS
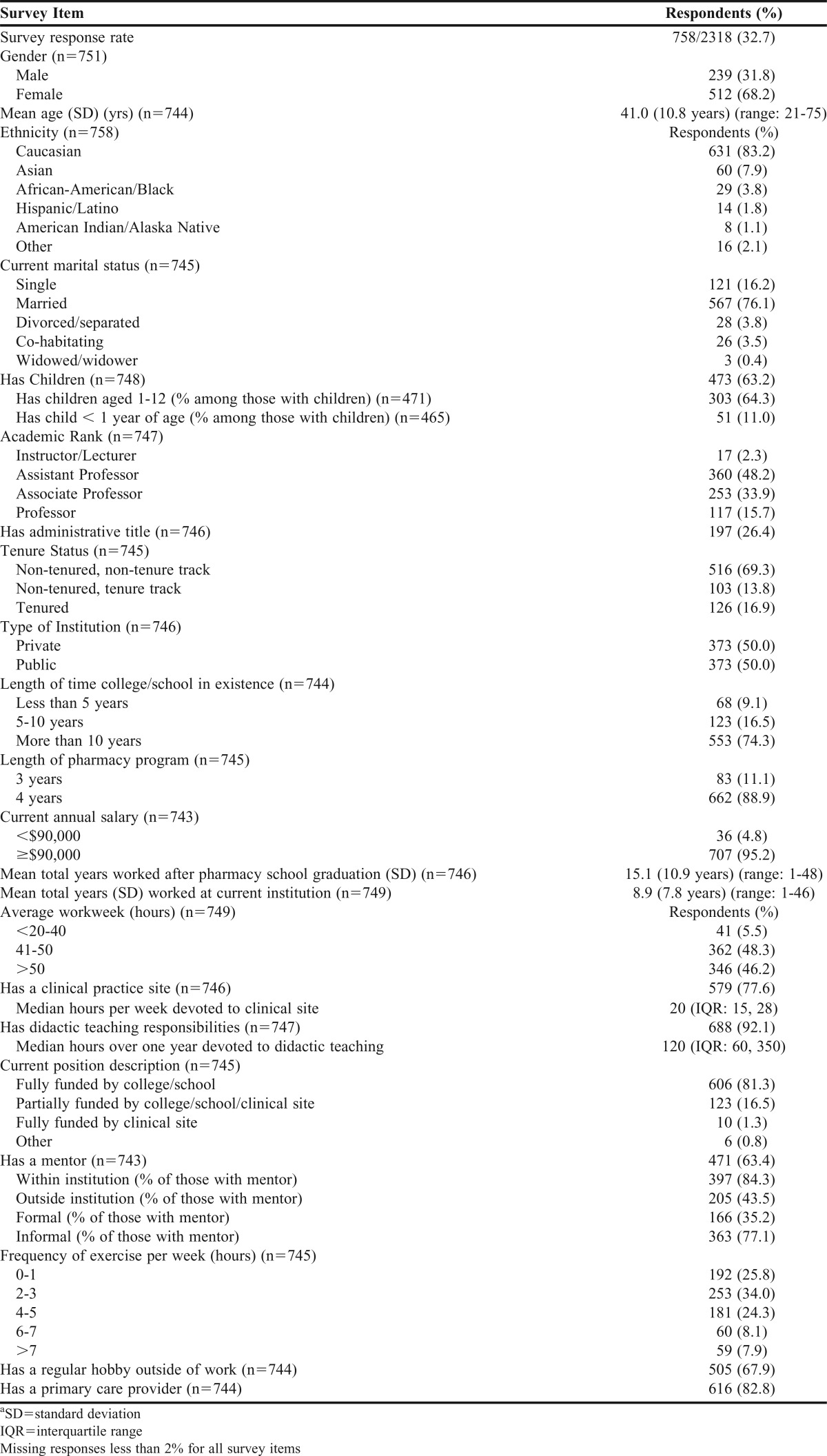
Of the 2318 subjects, 758 responded to the survey request (32.7% response rate) (Table 1). Majority of respondents were female, Caucasian, married, had children, and were in non-tenure tracks. Most respondents were assistant or associate professors (>80% combined). Equal numbers were at public and private institutions, and most respondents were at institutions that were established more than 10 years. More than 60% of respondents reported having a mentor; of those who had a mentor, majority had informal relationships.
Table 1.
Demographics of Respondentsa
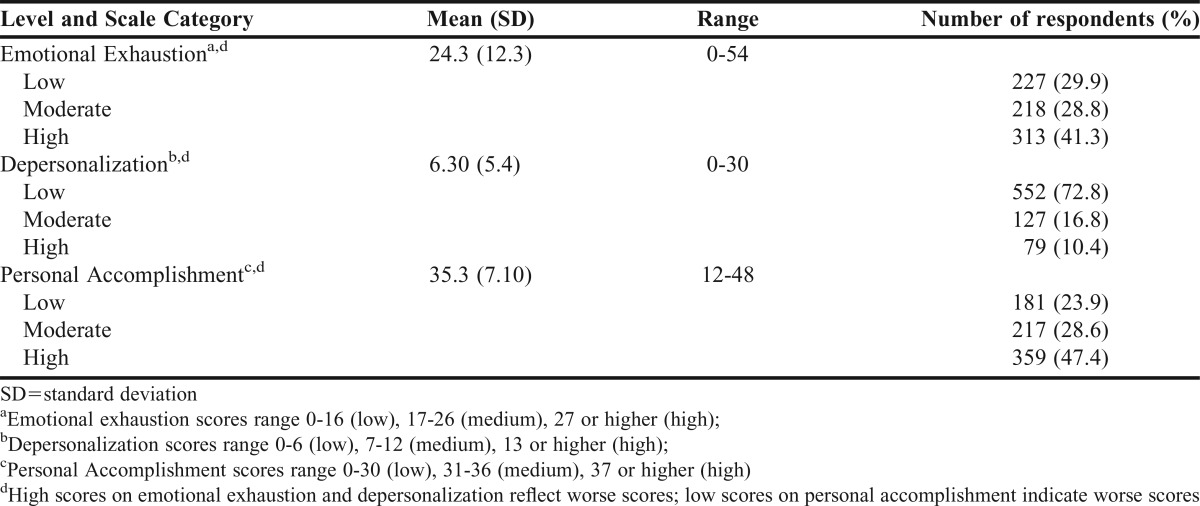
Among the respondents, the mean scores (± standard deviation) on the MBI-ES for EE, DP and PA are displayed in Table 2. More than 40% of faculty had scores considered “high” for EE. Only about 10% of faculty had “high” scores on the DP subscale while about 24% of faculty had “low” scores on the PA subscale.
Table 2.
Respondent Overall MBI Scores and Domain Scoresa-d
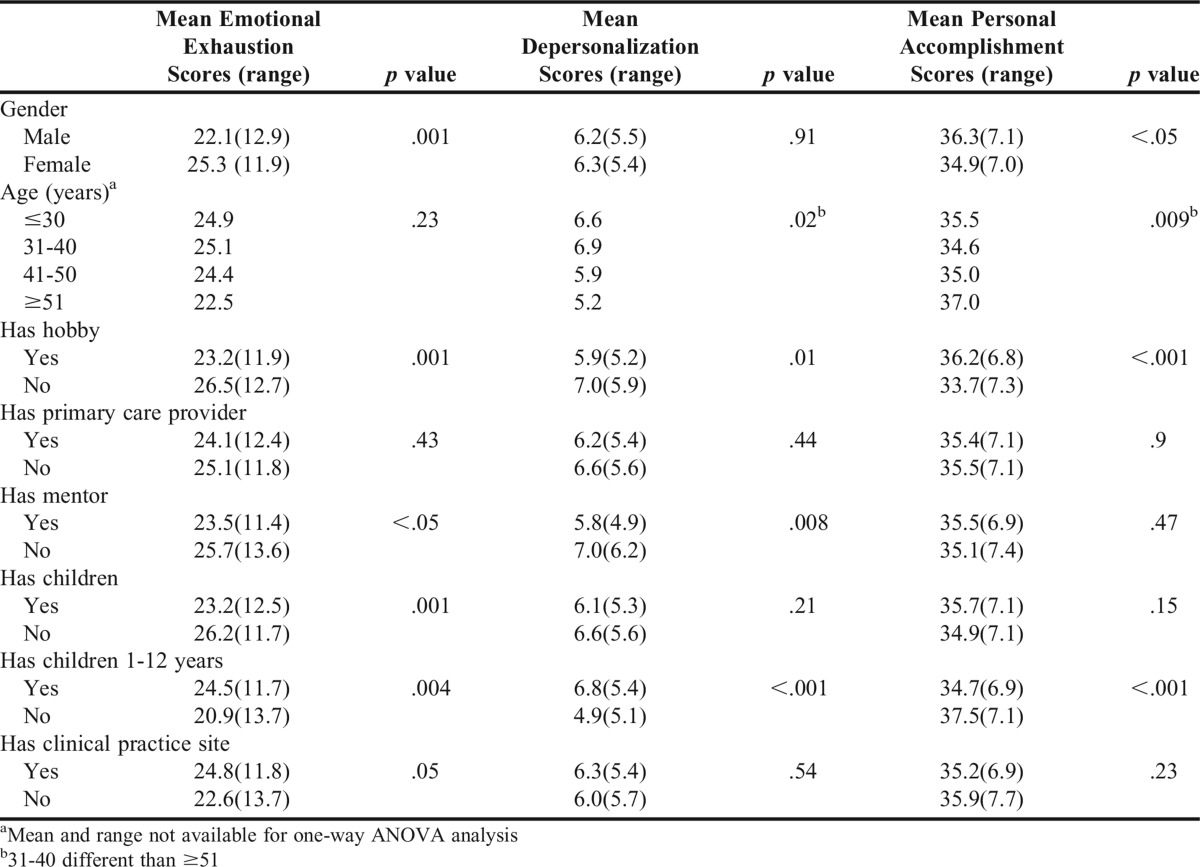
Mean scores on the MBI subscales were analyzed for potential predictive characteristics (Table 3). Women had significantly higher EE and lower PA scores compared with men. Those without a hobby had significantly higher EE and DP scores and lower PA scores. Those without a mentor had significantly higher EE scores and DP scores. Having children produced varying results in that those with children had lower levels of EE compared with those without children. However, those with young children (ages 1-12) had higher EE and DP and lower PA scores compared with those without young children.
Table 3.
Predictive Characteristics for Domains of Burnout
Scores on EE, DP and PA differed based on academic rank (df=3, p<.05 for all scores). In post-hoc analysis using Bonferroni correction (significance at 0.125 level), assistant professors had 5.1 mean higher scores (p=.001) and associate professors had 3.8 mean higher scores on EE (p=.03) compared with full professors. On DP scores, assistant professors had 1.7 mean higher scores (p=.02) compared with full professors. For PA scores, associate professors had 2.3 mean lower scores (p=.02) compared with full professors. We also found a negative correlation between total years worked after pharmacy graduation to average EE and DP scores (p<.001 for both) and a positive correlation with PA scores (p<.001).
Faculty working in newer colleges/schools were associated with worse scores on DP and PA. Those who worked at colleges/schools established fewer than five years had higher DP scores than faculty at schools established 5-10 years (p=.02) and more than 10 years (p=.008). Faculty at colleges/schools established fewer than five years had lower DP scores than those at schools established 5-10 years. (p=.03).
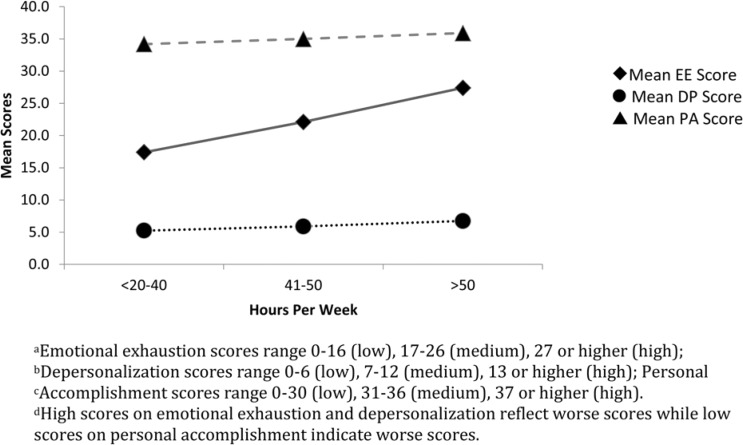
Figure 1 shows the EE, DP, and PA scores depending on the reported average workweek. In a one-way ANOVA analysis, EE scores were significantly associated (p<.001) with increased workweek hours. In post-hoc analysis using Bonferroni correction (df=2, significance at p<.02), those who worked >50 hours per week had higher EE scores compared to those who worked <20-40 hours per week (p<.001) and those who worked 41-50 hours per week (p<.001).
Figure 1.
Level of MBI-ES Domain Scoresa-d vs. Mean Workweek Hours
Faculty with administrative titles did not have significantly worse scores on EE, DP or PA than those without administrative roles. Having a primary care provider was not predictive of worse EE, DP or PA scores. Tenure status also did not significantly affect the EE, DP or PA scores.
DISCUSSION
Our study demographics with high percentage of women, assistant professors and Caucasians are representative of the pharmacy practice faculty in the US.18 In addition, we had equal numbers of private and public institutions represented, also resembling the AACP membership.19 The age distribution in our sample was also representative of pharmacy practice faculty with 40.4% of faculty in the 30-39 age range, followed by 21.4% in the 40-49 year age group and 20.7% in the greater than 50 year age group.18
In one of the earliest studies conducted on pharmacy faculty burnout, Jackson and colleagues reported that 16.4% of faculty had high EE, 16.8% had high DP and 35.8% had low PA scores.10 In our study, the rate of burnout more than doubled, with 41.3% of participants reporting high EE scores. In addition, mean EE scores were higher than those reported in the Jackson and colleagues’ study (24.3 vs. 18.8); but similar for DP (6.3 vs. 6.5) and PA (35.3 vs. 36.3) scores. In the normative data from the MBI developers, the mean EE, DP and PA scores among teachers were 21.3, 11 and 33.5, respectively.6 Pharmacy faculty in our study had higher EE scores and lower DP scores. The PA scores were similar to the normative group.7
These differences could be due to the fact that our study only included pharmacy practice faculty compared to all pharmacy faculty surveyed in the previous study. We also used the MBI Educators Survey (MBI-ES) (survey used “student” instead of “recipient”) although it is uncertain which version was used in the Jackson and colleagues study. Pharmacy practice faculty are heavily involved in clinical activities (77.6% in our sample) which could add to increased stress and burnout. The normative samples reported mean scores (SD) for pharmacists licensed in the US for EE, DP and PA were 21.1±11.7, 8.0±6.0 and 34.2±8.1, respectively.12 Our study found worse mean scores in all sub-domains. Burnout has been extensively studied among health care providers; in a national survey of US physicians, 37.9% reported high EE scores.1,8,9,13,20-23 Our sample of pharmacy faculty differed from physicians on the DP and PA scores; 10.4% of pharmacy faculty had high DP scores compared to 29.4% of physicians and 24% of pharmacy faculty had low PA scores compared to 12.4% of physicians reporting low PA scores. These differences could be due to different job expectations and motivations between pharmacy faculty and physicians. For example, PA is less related to EE and more related to control, freedom, and autonomy in the workplace.16 Physicians may have more autonomy in their clinical practice whereas pharmacy practice faculty may be limited in their job responsibilities and in their clinical practice. A similar pattern was seen among nurses where job demands had the most significant impact on EE.13
Compared to the previous study and demographic norms for the MBI subscales, EE scores were higher for both men and women pharmacy faculty in our study.6 Between genders, it is not surprising the women had higher EE, which is consistent with previous studies and the continuing role conflicts that may exist for women in the workplace and home.17,24-26
The mean EE scores for the age groups ≤30, 31-40, 41-50 and ≥51 in our study were consistently higher than demographic norms (23.9, 22.3, 20.2 and 18, respectively) and the previous pharmacy faculty study (22.4, 21.5, 18.6, 14.7, 14.4; age groups ranged from 20-29, 30-39, 40-49, 50-59 and >60). The notable difference between our study and the previous Jackson study is that our study showed similar EE scores across the age groups instead of declining as age increased.10
In our study, we found that age was not predictive of higher EE scores although those in the assistant professor rank were significantly higher on EE scores. Age may not be directly related to higher EE scores due to the wide age range among junior faculty. Among pharmacy faculty, rank may be more predictive of burnout and EE than age. Another study also found that there was little difference between those in different academic ranks and work and non-work role conflicts.26
The mean DP scores for the age groups were lower than the demographic norms (9.4, 8.3, 6.7, 5.3). The PA scores for the age groups in our study were similar to the demographic norms (35.9, 37.3, 38.2, 38.4) and previous pharmacy faculty study (36.1, 35.2, 37.2, 37, 36.8).
The mean EE scores for single, married, and divorced/separated in our study were higher than in the Jackson study (23.9 (single), 18.1 (married), 20 (divorced) and 13.3 (separated)) and higher than the normative samples (24.3 (single), 20 (married), 22.3 (divorced) and 23 (other)).7,10 The higher scores for single and divorced/separated faculty were attributed possibly due to younger faculty being non-tenured, having lower salaries and having less social support to discuss job-related issues.10,26 Non-work influences (eg, marital status, number of children), work influences (eg, time spent at work, academic rank), and gender may contribute to role conflict that ultimately determines overall life satisfaction.26 The mean DP scores were lower in our study compared to the demographic norms for single, married and divorced. The mean PA scores in our study were lower than the demographic norms for the same marital statuses.
Having young children was associated with higher EE scores; inability to achieve work-life balance has been identified previously as a contributor to EE.16,25,27 Again, among pharmacy faculty, simply having children may not be as impactful as having young children with respect to EE. Having dependent children may also depend on marital status; single faculty with children had lower overall life satisfaction when compared to married faculty with children, married faculty without children and single faculty without children.26 Considering the demographic characteristics of pharmacy faculty workforce in the US (young, women, junior rank) and the additive contribution of each factor to burnout, there is a need for intervention.
Emotional exhaustion has been identified as a core feature of burnout.5,28-30 The high percentage of pharmacy faculty with significant EE found in our study is concerning. Emotional exhaustion is also most responsive to the organizational environment such as role conflict, role ambiguity, participation in decision-making, reward systems and social support networks.31-38 In our study, assistant professors had the highest EE scores compared to other ranks, which was consistent with the Jackson study and others.10,14,25 This may be associated with real or perceived inability to participate in decision-making, potential lack of social support as new faculty members and concerns about promotion and academic success. Improvements in faculty governance structure, clear role-delineations and reward systems can be made in colleges and schools of pharmacy to potentially reduce EE and burnout among faculty.
Mentoring is defined as a “symbiotic relationship between the mentor and mentee.”39 We found those with a mentor had lower scores on DP; social support and professional engagement have been shown to be negatively related to depersonalization and positively associated with personal accomplishment.40 While a formal mentoring process increases the probability a mentee will receive some kind of mentorship at the initial phase, informal mentoring cannot be ignored. Since most of our respondents had informal mentor-mentee relationships, our study suggests that any type of social support can decrease feelings of DP and increase feelings of PA.41 We did not investigate whether faculty had more than one mentor and the extent or effectiveness of those relationships. Regardless of the nature of mentoring, it has been documented that mentoring can lead to job satisfaction and increased productivity.41-43 Supporting and implementing mentoring objectives for each faculty member have been shown to be critical to increase faculty retention.41
Most faculty reported working more than 40 hours per week, similar to previous reports.26 In our study, the number of hours worked correlated linearly with increasing EE scores which contrasted with the previous study. This difference could be due to possibly increasing demands of pharmacy practice faculty and increased expectations within the academic and clinical settings. Time spent at work has been shown to correlate with positive role conflict and negative overall life satisfaction among pharmacy faculty.26 Those who reported working more than 48 hours reported doing work-related activities during the evening or weekend/vacation time, spending less time with their family and their job making it difficult for them to be the parent or spouse that they want to be.26
Having a primary care provider did not have any correlation with burnout; however, a recent study showed that anxiety and major depressive disorders were reported by 8.8% and 5.8% of respondents.44 In addition, 15.5% of respondents reported recent binge alcohol use (five or more drinks on same occasion) and 3.7% reported heavy alcohol use (five or more drinks on same occasion on five or more days within a month). Assuming that these voluntary figures are underestimations, pharmacy faculty may be at similar risk of mental health and substance use disorders as the general population.44-46 Minimal exercise among pharmacy faculty was also confirmed in this study; previously, majority of faculty reported exercising less than 150 minutes per week and spending a significant part of their day in a sedentary environment.45
Top five stressors identified among pharmacy faculty are lack of time to perform well, interruptions by students/faculty, handling paperwork, lack of time to meet deadlines, and keeping up with new developments in the profession.10 Modification of the workload may help reduce burnout especially among junior faculty.10 Flexible work schedules may also be beneficial; annual evaluation of workload is essential since more work hours may be associated with burnout. Mentoring programs should be encouraged especially for junior faculty; however, peer support at all ranks is equally important to promote collegiality and social networks. Establishing clear lines of authority and responsibility, engaging faculty in decision making, and encouraging development of mentor relationships may also help to reduce burnout.37 Staff development and counseling, job restructuring, management development and program goals, methods and traditions are also potential strategies to reduce professional burnout.47 Self-care (achieving a work-life balance) and finding mentors/role models were provided as guidance/advice for young women considering careers in academic pharmacy.48 Based upon the results of the Wolfgang study, it is suggested that deans and department chairs can help faculty set realistic goals, use time management training programs for faculty who have difficulty in this area, and focus attention on high risk groups such as younger faculty, non-administrative and non-tenured faculty.49 Other strategies offered have included mandatory time off, job sharing and incorporating stress-reduction education programs and wellness activities into the workday to reduce sedentary time.45
Limitations to our study include a relatively low response rate of 32.7%; however, this is the largest study to date evaluating burnout among pharmacy practice faculty in the US and also matches response rates in similar studies among other health professions’ faculty.8-10 In addition, the demographics of our responders are representative of the pharmacy practice faculty in the US similar to the demographics characterized by AACP.18,19 As with any survey study, response bias could have occurred and results may be reflective of individuals interested in participating rather than the entire population. It is unknown if non-responders were suffering from burnout and therefore had no time or interest to participate. Conversely, those not suffering from burnout could have chosen not to participate due to disinterest. Our results are also limited to those faculty listed on the AACP roster and this may have excluded other potential participants. In addition, the survey timing may have influenced faculty responses. The survey was administered in the summer when many faculty are on vacation or have lighter teaching loads. In fact, the rate of burnout reported may have been lower during this time and the results may be an underestimation.
CONCLUSION
Pharmacy practice faculty members at US colleges and schools of pharmacy are suffering from burnout, mainly through emotional exhaustion that is higher than demographic norms. Groups that are at higher risk of emotional exhaustion include women, assistant professors, those with young children, and those who work high number of hours per week. Those with a mentor had lower levels of depersonalization. Programs and resources are needed to assist deans and department chairs at US colleges and schools of pharmacy to reduce or prevent burnout among faculty, especially in high-risk groups. Further research may be conducted to assess whether the impact of faculty burnout has an effect on measurable outcomes, such as depression, substance abuse, and suicidality/violence. Ultimately, the goal is to increase awareness of faculty burnout, prevent or manage burnout among faculty, and improve faculty job satisfaction and retention.
ACKNOWLEDGMENTS
We would like to thank the Department of Pharmacy Practice, College of Pharmacy-Glendale, Midwestern University for financially supporting this project.
REFERENCES
- 1.Thomas NK. Resident burnout. JAMA. 2004;292:2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 2. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. In: Evaluating Stress: A Book of Resources. Lanham, MD: Rowman & Littlefield Publishers.; 1997:191–218.
- 3.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Ann Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 4.Montero-Marin J, Araya R, Blazquez BO, et al. Understanding burnout according to individual differences: ongoing explanatory power evaluation of two models for measuring burnout types. BMC Public Health. 2012;12:922. doi: 10.1186/1471-2458-12-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maslach C. Understanding burnout: work and family issues. In: Halpern DF, Murphy SE, eds. From Work-Family Balance to Work-Family Interaction: Changing the Metaphor. Hillsdale, NJ: Lawrence Erlbaum; 2005:99–214.
- 6.Maslach burnout inventory (MBI) Mind Garden. http://www.mindgarden.com/products/mbi.htm Accessed January 13, 2015.
- 7. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd Ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
- 8.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 10.Jackson R, Barnett C, Stajich G, Murphy J. An analysis of burnout among school of pharmacy faculty. Am J Pharm Educ. 1993;57(1):9–17. [Google Scholar]
- 11.Lahoz MR, Mason HL. Maslach burnout inventory: factor structures and norms for USA pharmacists. Psychol Rep. 1989;64(3 Pt 2):1059–1063. doi: 10.2466/pr0.1989.64.3c.1059. [DOI] [PubMed] [Google Scholar]
- 12.Gupchup G, Lively B, Holidaygoodman M, et al. Maslach burnout inventory – factor structures for pharmacists in health maintenance organizations and comparison with normative data for USA pharmacists. Psychol Rep. 1994;74(3):891–895. doi: 10.2466/pr0.1994.74.3.891. [DOI] [PubMed] [Google Scholar]
- 13.Jourdain G, Chenevert D. Job demands-resources, burnout and intention to leave the nursing profession: A questionnaire survey. Int J Nurs Stud. 2010;47:709–722. doi: 10.1016/j.ijnurstu.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Tijdink JK, Vergouwen AC, Smulders YM. Emotional exhaustion and burnout among medical professors; a nationwide survey. BMC Med Educ. 2014;14(1):183. doi: 10.1186/1472-6920-14-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Melendez WA, de Guzman RM. Burnout: the new academic disease. ASHE-ERIC higher education research report no. 9, 1983. Association for the Study of Higher Education; Eric Clearinghouse on Higher Education, Washington, DC.
- 16.Keeton K, Fenner DE, Johnson TR, Hayward RA. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol. 2007;109(4):949–955. doi: 10.1097/01.AOG.0000258299.45979.37. [DOI] [PubMed] [Google Scholar]
- 17.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among american surgeons: a comparison by sex. Arch Surg. 2011;146(2):211–217. doi: 10.1001/archsurg.2010.310. [DOI] [PubMed] [Google Scholar]
- 18.American Association of Colleges of Pharmacy. 2014-15 Profile of Pharmacy Faculty. http://www.aacp.org/resources/research/institutionalresearch/documents/ppf1415-final.Pdf. Accessed November 15, 2015.
- 19.American Association of Colleges of Pharmacy. Academic pharmacy’s vital statistics. http://aacp.org/about/pages/vitalstats.aspx. Accessed December 11, 2015.
- 20.Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Med Care. 2004;42(2 Suppl):1157–1166. doi: 10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alacacioglu A, Yavuzsen T, Dirioz M, Oztop I, Yilmaz U. Burnout in nurses and physicians working at an oncology department. Psychooncology. 2009;18(5):543–548. doi: 10.1002/pon.1432. [DOI] [PubMed] [Google Scholar]
- 22.Roth M, Morrone K, Moody K, et al. Career burnout among pediatric oncologists. Pediatr Blood Cancer. 2011;57(7):1168–1173. doi: 10.1002/pbc.23121. [DOI] [PubMed] [Google Scholar]
- 23.Kimo Takayesu J, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emer Med. 2014;21(9):1031–1035. doi: 10.1111/acem.12464. [DOI] [PubMed] [Google Scholar]
- 24.Gunasingam N, Burns K, Edwards J, Dinh M, Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J. 2015;91(1074):182–187. doi: 10.1136/postgradmedj-2014-132847. [DOI] [PubMed] [Google Scholar]
- 25.Dyrbye LN, West CP, Satele D, Sloan JA, Shanafelt TD. Work/home conflict and burnout among academic internal medicine physicians. Arch Intern Med. 2011;171(13):1207–1209. doi: 10.1001/archinternmed.2011.289. [DOI] [PubMed] [Google Scholar]
- 26.Nair K, Gaither C. Effects of work, non work, and role conflict on the overall life satisfaction of pharmacy faculty. Am J Pharm Educ. 1999;63(1):1–11. [Google Scholar]
- 27.Lowenstein SR, Fernandez G, Crane LA. Medical school faculty discontent: prevalence and predictors of intent to leave academic careers. BMC Med Educ. 2007;7:37. doi: 10.1186/1472-6920-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schaufeli W, Taris T. The conceptualization and measurement of burnout: common ground and worlds apart. Work & Stress. 2005;19(3):256–262. [Google Scholar]
- 29. Shirom A. Job-related burnout: a review. In: Handbook of Occupational Health Psychology. Washington, DC: American Psychological Association; 2003:245–265.
- 30.Brenninkmeijer V, Vanyperen N. How to conduct research on burnout: advantages and disadvantages of a unidimensional approach in burnout research. Occup Environ Med. 2003;60(Suppl 1):i16–i20. doi: 10.1136/oem.60.suppl_1.i16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson MBG, Iwanicki EF. Teacher motivation and its relationship to burnout. Educ Adm Quar. 1984;20(2):109–132. [Google Scholar]
- 32.Byrne BM. Burnout – testing for the validity, replication, and invariance of causal-structure across elementary, intermediate, and secondary teachers. Amer Ed Res J. 1994;31(3):645–673. [Google Scholar]
- 33.Crane SJ, Iwanicki EF. Perceived role conflict, role ambiguity, and burnout among special education teachers. Remedial Special Educ. 1986;7(2):24–31. [Google Scholar]
- 34. Farber BA, Wechsler LD. Crisis in Education: Stress and Burnout in the American Teacher. San Francisco, CA: Jossey-Bass; 1991.
- 35. Hubert JA, Gable RK, Iwanicki EF. The relationship of teacher stress to school organizational health. In: Advances in Research and Theories of School Management and Policy. Greenwich, CT.: JAI Press; 1990:185–207.
- 36.Schwab RL, Iwanicki EF. Perceived role conflict, role ambiguity, and teacher burnout. Educ Adm Quar. 1982;18(1):60–74. [Google Scholar]
- 37.Schwab RL, Jackson SE, Schuler RS. Educator burnout: sources and consequences. Educ Res Quar. 1986;10(3):14–30. [Google Scholar]
- 38.Gaither CA, Nadkarni A, Mott DA, et al. Should I stay or should I go? The influence of individual and organizational factors on pharmacists’ future work plans. J Am Pharm Assoc (2003) 2007;47(2):165–173. doi: 10.1331/6J64-7101-5470-62GW. [DOI] [PubMed] [Google Scholar]
- 39.Haines S. The mentor-protege relationship. Am J Pharm Educ. 2003;67(3):Article 82. [Google Scholar]
- 40.Schaufeli WB, Salanova M, Gonzalez-Roma V, Bakker AB. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. J Happiness Stud. 2002;3(1):71–92. [Google Scholar]
- 41.Fuller K, Maniscalco-Feichtl M, Droege M. The role of the mentor in retaining junior pharmacy faculty members. Am J Pharm Educ. 2008;72(2):Article 41. doi: 10.5688/aj720241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carter O, Nathisuwan S, Stoddard GJ, Munger MA. Faculty turnover within academic pharmacy departments. Ann Pharmacother. 2003;37(2):197–201. doi: 10.1177/106002800303700206. [DOI] [PubMed] [Google Scholar]
- 43.Roch GR. Much ado about mentors. Harv Bus Rev. 1979;57(1):14–20. [PubMed] [Google Scholar]
- 44.Kenna G, Wood MD. Substance use by pharmacy and nursing practitioners and students in a northeastern state. Am J Health Syst Pharm. 2004;61(9):921–930. doi: 10.1093/ajhp/61.9.921. [DOI] [PubMed] [Google Scholar]
- 45.Lindfelt TA, Ip EJ, Barnett MJ. Survey of career satisfaction, lifestyle, and stress levels among pharmacy school faculty. Am J Health Syst Pharm. 2015;72(18):1573–1578. doi: 10.2146/ajhp140654. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the national comorbidity survey replication (NSC-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 47. Cherniss C. Professional Burnout in Human Service Organizations. New York, NY: Praeger Publishers; 1980.
- 48.Chisholm-Burns MA, Spivey CA, Billheimer D, et al. Multi-institutional study of women and underrepresented minority faculty members in academic pharmacy. Am J Pharm Educ. 2012;76(1):7. doi: 10.5688/ajpe7617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolfgang AP, Ortmeier BG. Career commitment, career plans, and job-related stress – a follow-up-study of pharmacy students as pharmacists. Am J Pharm Educ. 1993;57(1):25–28. [Google Scholar]